Abstract
Background:
The optimal position of the condyle in glenoid fossa is a fundamental question in dentistry. There is no quantitative standard for the optimal position of mandibular condyle in the glenoid fossa in our population. The purpose of this study is to assess the position of the condyle by cone beam computed tomography (CBCT) images in patient with normal function of temporomandibular joint (TMJ).
Materials and Methods:
In this cross-sectional study, CBCT images of 40 class I skeletal patients (15 males and 25 females) without history of TMJ disorders were selected. Next, the anterior, superior and posterior joint spaces (Ajs, Sjs, Pjs) were measured on the two true central sagittal slices. Then medial (M) and lateral (L) joint spaces on true coronal view were measured in the right and left sides, separately. After that, P/A ratio, S/A ratio and M/L ratio were calculated. Finally, a paired t-test and independent samples t-test were employed for analysis.
Results:
The centric position of the condyle in glenoid fossa was more common (92.5%) than other positions. Significant differences in Ajs, Sjs, Pjs, Mjs and Ljs values between two sides were observed (P ≤ 0.05). Additionally, Sjs showed statistically significant differences between the sexes (P = 0.05). P/A ratio and S/A ratio had significant differences between two sides but not between those sexes.
Conclusion:
The assessment of joint spaces in right and left sides should be done independently. Overall, the measured joint spaces except Sjs are not different in two sexes. The data from this study could be a useful and comparable reference for the clinical assessment of condylar position in patients with normal functional joints.
Keywords: Cone beam CT, mandibular condyle, temporomandibular joint
INTRODUCTION
The ideal position of the condyle in the glenoid fossa of the temporomandibular joint (TMJ) is one of the most hot topics found in dentistry with a lot of fundamental questions.[1–6] Although, the occlusion of the patient can be observed directly in the mouth, condylar position in the fossa is unapproachable to the naked eye.[7] Thus, the optimal condylar position in the glenoid fossa can be determined by the dimension of the joint space. The joint space is a total term radiographically that uses for description of the radiolucent zone that places between condylar and temporal parts.[8] Conventional radiographs cannot show anatomical relationships exactly, as a result, modern imaging modalities such as MRI and CT are now being used more frequently for radiographic TMJ examination.[9]
Magnetic Resonance Imaging (MRI) is considered as one of the most useful tools that show disc displacement.[10–12] Unfortunately MRI gives a little information of the bone TMJ structures.[13] Incesu et al.[14] classified the degree of anterior disc displacement by MRI technique in patients with TMJ dysfunction (TMD).
Computed tomography (CT) provides images of the bony components of TMJ. CT has the advantage of presentation of the three-dimensional details of bone structure.[15] Yamada et al. showed the slope of eminence decreased with an increase in the severity of the condylar bone change in the CT images.[16]
Cone-beam computed tomography (CBCT) is a newer technique producing reconstructed images of high diagnostic quality using lower radiation doses and higher resolution than normal CT. This technique provides images that are obtained in planes parallel or perpendicular to the long axis of the condyle instead of the true anatomic coronal and sagittal planes. Thus, high quality images of the bony components on all planes will be produced.[9] CBCT technique allows the measurement of the position of condyle in the glenoid fossa with high accuracy.[13]
In order that there is no quantitative standard for the optimal position of mandibular condyle in the glenoid fossa in our population and due to the ability of CBCT technique in measuring the TMJ position with high accuracy, the purpose of this study is to assess quantitatively and qualitatively position of the condyle by CBCT images in people with normal function of TMJ.
MATERIALS AND METHODS
This cross-sectional study carried out with CBCT images of 40 patients (15 males and 25 females between 12-59 years of age with an average age of 33.7 years) without any history of temporomandibular joint disorders, but with class I skeletal category. Their CBCT images were taken based on many reasons except TMJ disorder. In this study, the normal function or absence of TMJ disorders was described as following: lack of history of pain, the joint sound, the clenching, and without limitation in the range of motion and posterior bite collapse.
We originally obtained the approval of the ethical board of the institutional ethics committee of the Guilan University of Medical Sciences Research Foundation in Rasht, Iran, before conducting this investigation (Ethics Approval Number 10229) to ensure our compliance with the recommendations of the Declaration of Helsinki and Tokyo for humans. Accordingly, our protocol complied with these guidelines. Moreover, we obtained written consent of the participating patients to use their volumetric data of CBCT images for this study.
CBCT images for all patients were obtained in an upright position using a new tom VG CBCT (QR SRL Company, Verona, Italy) device in full zoom mode. The patients were instructed to look into their eyes in a front mirror to obtain a natural head position.
At first, on axial slices, the cut that showed the largest medio-lateral dimension of condylar heads was selected. Sometimes, this selected slice was different for assessment of right (RT) and left (LT) sides. Next, true sagittal images with 2 mm thickness and interval distance on medio-lateral axis of condyle, as well as true coronal view with the same thickness and interval distance on anterior posterior axis of the condyle were reconstructed. Then, two true central sagittal images with 2 mm thickness and interval distance were chosen. After that, anterior, superior and posterior joint spaces were measured on these reconstructed sagittal images. Initially, a horizontal line on uppermost area of glenoid fossa was drawn and the intersection of this line with glenoid fossa was selected as superior reference point (S). Sequentially, this point was connected to the most prominent points on anterior (A) and posterior (P) aspects of the condyle. Finally, the perpendicular distance from A and P tangent points to glenoid fossa were measured as anterior and posterior joint spaces (Ajs, Pjs). Therefore, the right distance between S point and superior prominent point of condylar head was considered as superior joint space (Sjs) [Figure 1]. It is worth mentioning that this pattern of measurement was adopted from Ideka and Kawamura's study.[13] To enclose, the mean of the mentioned measurements on two central cuts was regarded as the final Ajs, Sjs and Pjs.
Figure 1.
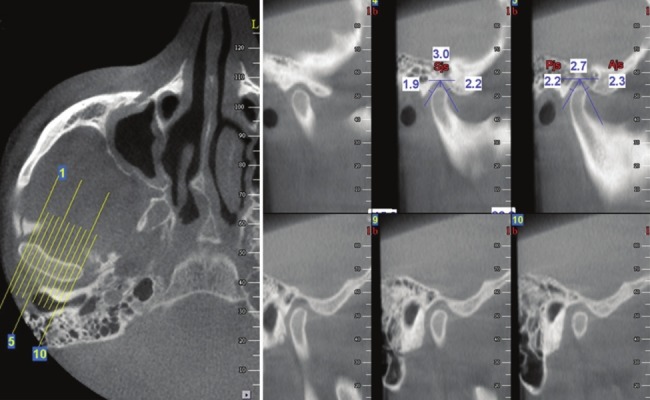
The method of the measurements of the superior, anterior and posterior joint spaces
For measuring the medial and lateral joint spaces on true coronal view, from deepest point of glenoid fossa, two tangent lines on medial and lateral slopes of glenoid fossa were drawn. A perpendicular line from the most prominent points on medial (M) and lateral (L) poles of each condylar head was connected to the tangent lines drawn on medial and lateral slopes of the glenoid fossa. The obtained distances were regarded as medial joint space (Mjs) and lateral joint space (Ljs) [Figure 2]. All of the measurements were conducted twice with 1 week interval. The mean of twice measurements was considered as the amount of joint space. In true sagittal view, the position of condyle in glenoid fossa as being centric or eccentric (anterior or posterior position) has been assessed.
Figure 2.
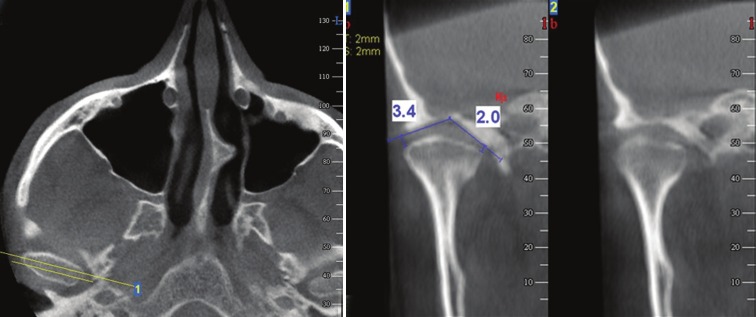
The method of measurement of the medial and lateral joint spaces
The mean values for all of measurements on right and left sides were considered as the total measurements. Based on the given total measurements, P/A ratio, S/A ratio and M/L ratio were calculated. Normal distribution of data was checked with one-sample kolmogorov-smirnov test. Finally, to compare these values, a “paired t-test” for the right and left sides was used and to determine the significant differences between female and male, an “independent-samples t-test”, was employed. Significance was established at P ≤ 0.05. It is required to state that all of the measurements were made with 0.1 mm accuracy.
RESULTS
In this cross-sectional study, CBCT images of 40 patients with class I skeletal category (15 males and 25 females between 12 - 59 years of age with an average age of 33.7 years) without any history of temporomandibular joint disorders were assessed.
The centric position of the condyle in the glenoid fossa was more common (92.5%) than other positions such as anterior (5%) and posterior (2.5%) positions.
Mean values (SD) of Ajs, Sjs, Pjs, Mjs and Ljs in right and left sides were presented in Table 1. Significant differences between the values of Ajs, Sjs, Pjs, Mjs and Ljs in right and left sides were observed.
Table 1.
The mean values of joint spaces in right and left sides
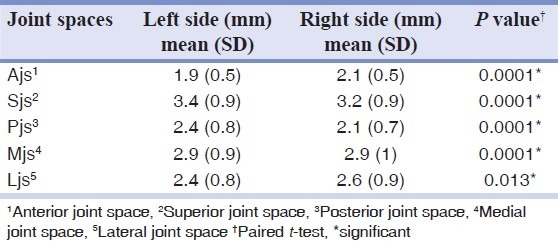
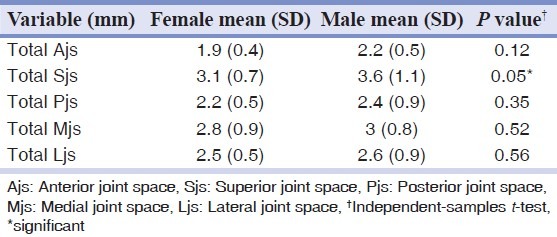
Table 2 shows comparing between female and male subjects about the values of total joint spaces.
Table 2.
Statistical data for the subjects by sex
The mean differences between the right and left anterior joint space was reported 0.2 mm ± 0.7. This quantity was 0.2 mm ± 0.4 for superior and 0.2 mm ± 1.2 for lateral joint spaces. The mean difference of posterior joint space in right and left sides was 0.3 mm ± 1.1.
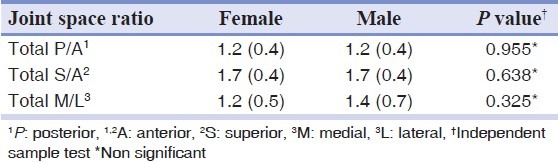
Tables 3 and 4 reveal comparing between the joint space ratios between two sides and sexes. Statistical analysis indicated no significant differences in the P/A ratio, S/A ratio and M/L ratio between the sexes [Table 4].
Table 3.
Comparing of the joint spaces ratios between two sides
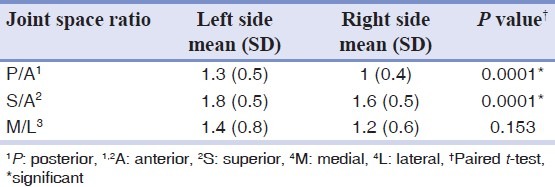
Table 4.
Comparing of the joint spaces ratios between sexes
DISCUSSION
Temporomandibular joint is a unique joint. Moreover, TMJ is a rather difficult area for radiological investigation because there is no possibility for accurate evaluation of this position in conventional radiographs. Thus, more advanced techniques are needed to show anatomical relationships accurately.[8]
The recently developed CBCT method by providing the possibility of three-dimensional imaging from TMJ area produces reconstructed images with high diagnostic quality.[9,17] In this study, we used CBCT method for the evaluation of the joint spaces. Lascala et al.,[18] Soumalainen et al.[19] and Kobayashi et al.[20] confirmed the accuracy of our selective method for linear measurements. Furthermore, Lascala et al.[18] reported that CBCT image underestimates real distances between the different points on skull base and is reliable for linear evaluation measurements of other structures. Soumalainen et al.[19] showed that the error of the linear measurement by using CBCT technique is less than multislice CT. Kobayashi et al.[20] found that the measurement error was significantly less with CBCT technique than the spiral CT. Moreover, CBCT allows accurate morphologic assessment of the bony structures of TMJ.[13,21]
In our study, the value of Sjs was the greatest in both sexes, followed by Mjs, Ljs, Pjs and Ajs. Without considering the values of Mjs and Ljs values, this result is in agreement with the results of Ikeda et al.[13] and Kinniburgh et al.[22] studies but, it is incompatible with the findings of Hansson et al.[23] Generally, the outcome values of our study are more than Ikeda et al.[13] and less than Kinniburgh et al.[22] studies. Hansson et al.[23] directly measured disc thickness in autopsy materials and found that the thickness of the posterior and anterior bands were more than intermediate zone. In addition, the significant difference in the thickness of intermediate joint space can be due to ignoring the thickness of the soft tissues covering the fossa, the tissue shrinkage and muscle spasm after the death in Hansson et al.[23] study.
In this study, only Sjs showed statistically significant difference between the sexes. This finding is in agreement with the results of Kinniburgh et al.[22] study and is incompatible with the results of Ikeda et al. study.[13] Ikeda et al.[13] observed no significant difference in the values of joint space between the sexes.
In our study, P/A ratio, S/A ratio and M/L ratio were 1.2, 1.7 and 1.3, respectively. Whereas Ikeda et al. 13 reported the values of P/A ratio and S/A ratio 1.6 and 1.9, respectively. These ratios in both sexes in Kinniburgh et al.[22] study are more than those in our study, except S/A ratio in female subjects that was equal with our findings.
Burke et al.[24] found no correlation between facial morphology and anterior-posterior position of the condyle in glenoid fossa. They found that the differences were observed in the vertical plane and the Sjs in the long face patients were less than short face patients. Katsavrias et al.[25] reported that the class III group had closer vertical relationship between the condyle and the roof of the fossa, indicating that Sjs is smaller while, in the present study, we found that Sjs was the largest space in class I skeletal category.
A wide variation in the posterior position of the condyle within the mandibular fossa in asymptomatic volunteers was reported.[26,27] In the present study, the centric position of the condyle in the glenoid fossa was more common than other position. Alexander et al.[28] reported posterior position of the condyle in glenoid fossa in the half of the anteriorly displaced disc on a symptom-free population. Incesu et al.[14] reported the posterior position of condyle as the most common position in patients with temporomandibular joint disorder. The results of Wiese et al.[29] study were similar to our results, that the condyle was positioned centrally in most TMJs.
Cohlmia et al.[30] and Seren et al.[31] stated that there was a smaller Ajs in the class III patients than class I, perhaps indicating a more anterior position of the condyle was a more frequent position in the class III patients.
Gateno et al.[32] used linear measurements of both horizontal and vertical distances by using the geometric centers of the condylar head and the glenoid fossa and also anteroposterior joint space ratio for evaluation of the condylar position space ratio. They found that the condyles in the patient with anterior disc displacement were situated more posterior and superior in the fossa than normal group.
CONCLUSION
In our study, the centric position of the condyle in the glenoid fossa is the most common position in the skeletal class I subjects with normal TMJ. The evaluation of joint spaces should be done independently in right and left sides. Overall, there were no differences between the values of joint spaces and joint space ratios. Therefore, the data collected in this study would be a helpful reference for clinical assessment of condylar position in subjects with normal functional joints.
ACKNOWLEDGEMENT
We are grateful to Mr. Ezzati for his assistance in editing the text.
Footnotes
Source of Support: This study was approved by oral and maxillofacial developmental research center of Dental school, Guilan university of medical sciences. The ethical approval was done by the ethical board of the institutional ethics committee of the Guilan University of Medical Sciences, Rasht, Iran.
Conflict of Interest: None declared.
REFERENCES
- 1.Gelb H. The optimum temporomandibular joint condyle position in clinical practice. Int J Periodontics Restorative Dent. 1985;4:34–61. [PubMed] [Google Scholar]
- 2.Carlton KL, Nanda RS. Prospective study of post treatment changes in the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2002;122:486–90. doi: 10.1067/mod.2002.128863. [DOI] [PubMed] [Google Scholar]
- 3.Kikuchi K, Takeuchi S, Tanaka E, Shibaguchi T, Tanne K. Association between condylar position, joint morphology and craniofacial morphology in orthodontic patients without TMJ disorders. J Oral Rehabil. 2003;30:1070–5. doi: 10.1046/j.1365-2842.2003.01194.x. [DOI] [PubMed] [Google Scholar]
- 4.Vitral RW, Telles Cde S, Fraga MR, deOliveira RS, Tanaka OM. Computed tomography evaluation of TMJ alterations in patients with class II division 1 subdivision malocclusions: Condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2004;126:48–52. doi: 10.1016/j.ajodo.2003.06.012. [DOI] [PubMed] [Google Scholar]
- 5.Gössi DB, Gallo LM, Bahr E, Palla S. Dynamic intra-articular space variation in clicking temporomandibular joints. J Dent Res. 2004;83:480–4. doi: 10.1177/154405910408300609. [DOI] [PubMed] [Google Scholar]
- 6.Cordray FE. Three dimentional analysis of model articulated in the seated condylar position from a deprogrammed asymptomatic population: A prospective study. Part 1. Am J Orthod Dentofacial Orthop. 2006;129:619–30. doi: 10.1016/j.ajodo.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Weinberg LA. The role of stress, occlusion and condyle position in TMJ dysfunction-pain. J Prosthet Dent. 1983;49:532–45. doi: 10.1016/0022-3913(83)90318-9. [DOI] [PubMed] [Google Scholar]
- 8.White SC, Pharoah MJ. 5th ed. Los Angeles: Mosby; 2009. Oral radiology principles and interpretation; p. 475. [Google Scholar]
- 9.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004;33:196–201. doi: 10.1259/dmfr/27403192. [DOI] [PubMed] [Google Scholar]
- 10.Kircos LT, Ortendahl DA, Mark AS, Arakawa M. Magnetic resonance imaging of the TMJ disc in asymptomatic volunteers. J Oral Maxillofac Surg. 1987;45:852–4. doi: 10.1016/0278-2391(87)90235-7. [DOI] [PubMed] [Google Scholar]
- 11.Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence of temporomandibular joint disc displacement in patients and symptom-free volunteers. Am J Orthod Dentofacial Orthop. 1996;109:249–62. doi: 10.1016/s0889-5406(96)70148-8. [DOI] [PubMed] [Google Scholar]
- 12.Ribeiro RF, Tallents RH, Katzberg RW, Murphy WC, Moss ME, Magalhaes AC, et al. The prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6-12 years. J Orofac Pain. 1997;11:37–47. [PubMed] [Google Scholar]
- 13.Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:495–501. doi: 10.1016/j.ajodo.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Incesu L, Taşkaya-Yilmaz N, Oğütcen-Toller M, Uzun E. Relationship of condylar position to dics position and morphology. Eur J Radiol. 2004;51:269–73. doi: 10.1016/S0720-048X(03)00218-3. [DOI] [PubMed] [Google Scholar]
- 15.Hayashi T, Ito J, Koyama J, Hinoki A, Kobayashi F, Torikai Y, et al. Detectability of anterior displacement of the articular disc in the temporomandibular joint on helical computed tomography: The value of open mouth position. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:106–11. doi: 10.1016/s1079-2104(99)70202-7. [DOI] [PubMed] [Google Scholar]
- 16.Yamada K, Tsuruta A, Hanada K, Hayashi T. Morphology of the articular eminence in temporomandibular joints and condyle bone change. J Oral Rehabil. 2004;31:438–44. doi: 10.1111/j.1365-2842.2004.01255.x. [DOI] [PubMed] [Google Scholar]
- 17.Palomo JM, Kau CH, Palomo LB, Hans MG. Three-dimentional cone beam computerized tomography in dentistry. Dent Today. 2006;25:130,132–5. [PubMed] [Google Scholar]
- 18.Lascala CA, Panella J, Marques MM. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom) Dentomaxillofac Radiol. 2004;33:291–4. doi: 10.1259/dmfr/25500850. [DOI] [PubMed] [Google Scholar]
- 19.Suomalainen A, Vehmas T, Kortesniemi M, Robinson S, Peltola J. Accuracy of linear measurements using dental cone beam and conventional multislice computed tomography. Dentomaxillofac Radiol. 2008;37:10–7. doi: 10.1259/dmfr/14140281. [DOI] [PubMed] [Google Scholar]
- 20.Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using limited cone beam computerized tomography. Int J Oral Maxillofac Implants. 2004;19:228–31. [PubMed] [Google Scholar]
- 21.Honda K, Arai Y, Kashima M, Takano Y, Sawada K, Ejima K, et al. Evaluation of the usefulness of the limited cone-beam CT(3DX) in the assessment of the thickness of the roof of the glenoid fossa of the temporomandibular joint. Dentomaxillofac Radiol. 2004;33:391–5. doi: 10.1259/dmfr/54316470. [DOI] [PubMed] [Google Scholar]
- 22.Kinniburgh RD, Major PW, Nebbe B, West K, Glover KE. Osseous morphology and spatial relationships of the temporomandibular joint: Comparisons of normal and anterior disc positions. Angle Orthod. 2000;70:70–80. doi: 10.1043/0003-3219(2000)070<0070:OMASRO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Hansson T, Oberg T, Carlsson GE, Kopp S. Thickness of the soft tissue layers and the articular disk in the temporomandibular joint. Acta Odontol Scand. 1977;35:77–83. doi: 10.3109/00016357709055993. [DOI] [PubMed] [Google Scholar]
- 24.Burke G, Major P, Glover K, Prasad N. Correlation between condylar characteristics and facial morphology in class II preadolescent patients. Am J Orthod dentofacial Orthop. 1998;114:328–36. doi: 10.1016/s0889-5406(98)70216-1. [DOI] [PubMed] [Google Scholar]
- 25.Katsavrias EG, Halazonetis DJ. Condyle and fossa shape in class II and class III skeletal patterns: A morphometric tomographic study. Am J Orthod Dentofacial Orthop. 2005;128:337–46. doi: 10.1016/j.ajodo.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 26.Blaschke D, Chase DC. Differences in TMJ condyle temporal relationships in normal men and women. J Dent Res. 1984;63:266–72. [Google Scholar]
- 27.Madsen B. Normal variation in anatomy, condylar movement and arthrosis frequency of the temporomandibular joint. Acta Radiol Diagn (Stockh) 1966;4:273–88. doi: 10.1177/028418516600400305. [DOI] [PubMed] [Google Scholar]
- 28.Alexander SR, Moor RN, DuBois LM. Mandibular condyle position: Comparison of articular mounting and magnetic resonance imaging. Am J Orthod Dentofacial Orthop. 1993;104:230–9. doi: 10.1016/S0889-5406(05)81724-X. [DOI] [PubMed] [Google Scholar]
- 29.Wiese M, Wenzel A, Hintze H, Petersson A, Knutsson K, Bakke M, et al. Osseous changes and condylar position in TMJ tomograms: Impact of RDC/TMD clinical diagnosis on agreement between expected and actual finding. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:52–63. doi: 10.1016/j.tripleo.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 30.Cohlmia JT, Ghosh J, Sinha PK, Nanda RS, Currier GF. Tomographic assessment of temporomandibular joints in patients with malocclusion. Angle Orthod. 1996;66:27–35. doi: 10.1043/0003-3219(1996)066<0027:TAOTJI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Seren E, Akan H, Toller MO, Akyar S. An evaluation of the condylar position of the temporomandibular joint by computerized tomography in class III malocclusions: A preliminary study. Am J Orthod Dentofacial Orthop. 1994;105:483–8. doi: 10.1016/S0889-5406(94)70009-5. [DOI] [PubMed] [Google Scholar]
- 32.Gateno J, Anderson PB, Xia JJ, Horg JC, Teichgraeber JF, Liebschner MA. A comparative assessment of mandibular condylar position in patients with anterior disc displacement of the temporomandibular joint. J Oral Maxillofac surg. 2004;62:39–43. doi: 10.1016/j.joms.2003.05.006. [DOI] [PubMed] [Google Scholar]


