Abstract
Background:
This study was to evaluate the effects of calcium hydroxide premedication on the marginal adaptation of the calcium-enriched mixture (CEM) cement as an apical plug.
Materials and Methods:
In this in vitro study, forty single rooted teeth were prepared and apical portion of the roots were immersed in sulfuric acid to produce open apices. The teeth were divided into 2 experimental groups. In medicated group, calcium hydroxide was placed in all canals for 1 week and in non-medicated group no dressing was used. Then, a 4-mm apical plug of CEM cement was placed in canals; each root was prepared for observation using scanning electron microscope and the maximum distance between CEM cement and surrounding dentin was measured. The data were analyzed by t-test, and significance level was set at α = 0.05.
Results:
The mean width of gap in medicated and non-medicated groups was 158/1 μm and 147/1 μm, respectively. There was no significant difference between the two groups (P > 0.05).
Conclusion:
Calcium hydroxide premedication had no adverse effect on the marginal adaptation of CEM cement apical plug.
Keywords: Apical plug, calcium-enriched mixture cement, calcium hydroxide, marginal adaptation, scanning electron microscopy
INTRODUCTION
Root canal therapy of immature teeth poses a special challenge for the clinician. Due to absence of apical constriction or apical stop, it is difficult to limit the obturation process within the root canal space.
Apexification (a method including long term application of calcium hydroxide to induce apical closure),[1] has several disadvantages. This treatment requires multiple appointments during an extended period. Susceptibility to fracture, coronal microleakage and aesthetic concerns during this extended treatment period are additional negative points.[2]
Placement of artificial apical barriers has been considered as an alternative to traditional calcium hydroxide apexification.[3,4] The material has been widely employed as artificial apical barrier is mineral trioxide aggregate (MTA).[5] MTA can be placed in one visit,[6,7] and induce hard tissue formation.[8–10] It is biocompatible,[11–14] and has good sealing and antimicrobial properties.[14–16] Although, MTA has poor handling characteristics[17] and a long setting time.[18]
Calcium-enriched mixture (CEM) cement has been developed with clinical applications similar to those of MTA. MTA and CEM cement showed similar favorable biologic responses in repair of furcal perforation,[19] pulp cap[20] and pulpotomy treatment.[21] CEM cement has appropriate handling characteristics[22] and exhibited similar sealing properties to MTA when used as root-end filling material.[23] Asgary, et al. compared the response of periradicular tissues to MTA and CEM cement as root-end fillings and concluded that CEM cement and MTA were associated with regenerative periapical tissue response when used as root-end filling biomaterials.[24]
Usually, one or two visits of calcium hydroxide therapy are performed before application of apical barrier, in order to disinfect the root canal system of teeth with nonvital pulps.[5] However, complete removal of calcium hydroxide from the dentinal walls is reportedly impossible.[25,26]
The purpose of this study was to evaluate the effects of residual calcium hydroxide on the marginal adaptation of the CEM apical barrier.
MATERIALS AND METHODS
Forty extracted human single-root teeth were selected for this in vitro study. The teeth were clinically examined to be free of caries, cracks, restoration, and calcification. The teeth were placed in 5.25% sodium hypochlorite (NaOCl) for 5 h. Thereafter, they were rinsed and stored in saline solution. Clinical crowns were removed from the cement-enamel junction with a high-speed diamond bur (D and Z Germany) under excess water to create a standardized root length of 14 mm.
The root canals were instrumented using K-files (Dentsply Maillefer, Tulsa, USA) up to master apical file # 45 and gates-glidden drills ≠ 1−4 (Dentsply, Maillefer, Tulsa, OK) in a step back manner. Then the access opening was sealed with coltozol (Coltene, Altstatten, Switzerland) and sulfuric acid was used to produce apical resorption. Briefly, the roots were drowned in melted rose wax (Cavex Holland, Netherlands) up to 3 mm from the anatomic apex. The waxed teeth were immersed in 20% sulfuric acid for 4 days. After that, the teeth were rinsed with a saline solution, the wax was removed with a scalpel (Supa, Tehran, Iran), and temporary filling was removed from the access opening.[27]
The teeth were randomly divided into two experimental groups (n = 20). In medicated group (n = 20), calcium hydroxide (pure calcium hydroxide mixed with distilled water) (cina bartar, Tehran, Iran) was placed in root canals using a lentulo spiral (Moyco Union Brach, York, PA) and a radiograph was taken to ensure complete coverage of the canal. After 1 week, the medicament was removed using 0.5% NaOCl irrigation and stainless steel hand files (Dentsply, Maillefer, Tulsa, USA). In non-medicated group (n = 20), no medication was placed into the canals. Small sponges were placed at the external portion of root apices. After that, the roots were placed in the putty molding blocks. The CEM cement was mixed according to the manufacturer's instructions and using MTA carrier, CEM cement was placed in the root canals. A hand condenser was used to condense the material. This process was continued until 4 mm apical plugs were formed at the root apices. Radiographs were taken to ensure proper placement and thickness of the CEM cement plugs. All specimens were stored at 37°C and 100% humidity for 7 days.
The roots were sectioned perpendicular to its long axis at 5 mm of the anatomic root apex using a high-speed diamond saw (D and Z Germany). The specimens were mounted on aluminum stubs, sputter-coated with gold and assessed from the top at a *300 magnification under scanning electron microscopy (Vega II XMU, Tescan, Czech Republic). Marginal adaptation evaluated at the root apices only, and width of largest gap (maximum distance between CEM cement and surrounding dentin) in each specimen was scored and recorded [Figures 1a and b].
Figure 1.
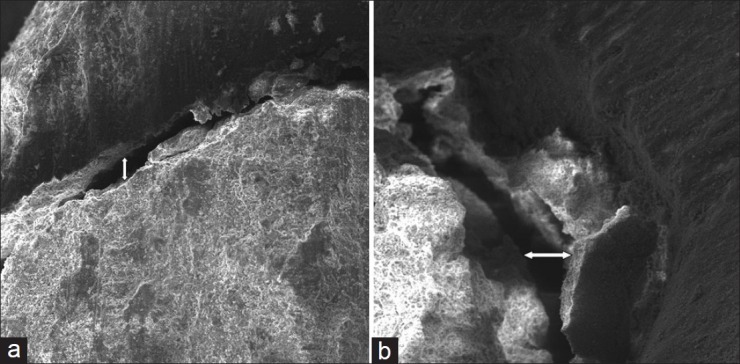
(a and b) scanning electron microscope (SEM) micrograph. A gap between the calcium-enriched mixture cement plug and dentinal wall at the root end can be observed in the (a) medicated group (with prior calcium hydroxide dressing and the (b) non-medicated group (without prior calcium hydroxide dressing)
The Kolmogorof-Smirnov test was used to confirm normal distribution of the data. The results were analyzed by t-test, and significance level was set at α = 0.05.
RESULTS
The scanning electron microscope (SEM) observation of root ends revealed gaps between CEM cement and the dentinal walls in all cases. Variations were observed in theses specimens in the width of gaps. The average gap width in medicated and non-medicated groups was 158/1 ± 67.1 μm and 147/1 ± 34/8 μm, respectively. No significant difference was observed between two experimental groups (P> 0.05).
DISCUSSION
Several studies have shown that MTA has good marginal adaptation in comparison of other root-end filling materials and the gap size is smaller in MTA root-end filled teeth.[28–32] Marginal adaptation of CEM cement has not been evaluated. The mean gap size in premedicated and non-premedicated root canals was 158.1 μm and 147.1 μm, respectively. These sizes are greater than those observed by Torabinejad, et al. (2.68 μm),[28] Bidar, et al. (14.8 μm)[31] and Xavier, et al. (1.051 and 0.812 μm)[32] in evaluation of marginal adaptation of MTA. This difference can be related to several factors. First, in these studies, MTA was placed retrogradely in the root canals and the root-end and marginal adaptation were assessed but in the present study, CEM cement was placed in root canals orthogradely (as an apical plug). Second, the method of measuring the gaps is different; Torabinejad, et al. and Bidar, et al. used longitudinally sections to measure gap widths between MTA and the root canal walls. Xavier, et al. used transverse sections to evaluate the marginal adaptation of MTA as a root-end filling material. Here, the gaps between CEM cement and the root canal walls at the root apices was evaluated, without performing sectioning at the CEM cement and dentinal wall interface. Finally, in this study sulfuric acid was used to produce open apex teeth. Sulfuric acid resorbs the root apex in a disordered manner, producing irregularities at the root end that may hinder adaptation of CEM cement to the dentinal walls and thereby increase the gap size. The size of gaps in this study is comparable with those was observed for marginal adaptation of MTA by same method (70.2 μm and 130.0 μm in premedicated and non-premedicated root canals, respectively).[33]
The present study showed that medication with calcium hydroxide had no adverse effect on marginal adaptation of the CEM cement plug. Hachmeister, et al.[34] also found that calcium hydroxide therapy for one week did not affect the sealing ability of MTA in 70 days. Porkaew, et al.[35] found decreased dye leakage in canals obturated with gutta-percha following premedication with calcium hydroxide. Bidar, et al.[33] also found that premedication with calcium hydroxide improved marginal adaptation of MTA.
CONCLUSION
According to the results of this study, calcium hydroxide medication had no effect on the marginal adaptation of CEM cement as an apical plug. Because the apical plug technique eliminates the lengthy apexification procedure, in vivo studies focused on the success rate of CEM cement apical plug are warranted.
ACKNOWLEDGMENT
This article is based on postgraduate thesis of Dr. Gharagozlo (no. 380). This study was also supported by Vice Chancellor for Research of Mashhad University of Medical Sciences.
Footnotes
Source of Support: This study was also supported by vice chancellor for research of Mashhad University of Medical Science
Conflict of Interest: None declared
REFERENCES
- 1.Steiner JC, Dow PR, Cathey GM. Inducing root end closure of nonvital permanent teeth. J Dent Child. 1968;35:47–54. [PubMed] [Google Scholar]
- 2.Holden DT, Schwartz SA, Kirkpatrick TC, Schindler WG. Clinical outcomes of artificial root-end barriers with mineral trioxide aggregate in teeth with immature apices. J Endod. 2008;34:812–7. doi: 10.1016/j.joen.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Coviello J, Brilliant JD. A preliminary clinical study on the use of tricalcium phosphate as an apical barrier. J Endod. 1979;5:6–13. doi: 10.1016/S0099-2399(79)80141-7. [DOI] [PubMed] [Google Scholar]
- 4.Brandell DW, Torabinejad M, Bakland LK, Lessard GM. Demineralized dentin, hydroxyapatite and dentin chips as apical plug. Endod Dent Traumatol. 1986;2:210–4. doi: 10.1111/j.1600-9657.1986.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 5.Shabahang S, Torabinejad M. Treatment of teeth with open apices using mineral trioxide aggregate. Pract Periodontics Aesthet Dent. 2000;12:315–20. quiz 322. [PubMed] [Google Scholar]
- 6.Steining TH, Regan JD, Gutmann U. The use and predictable placement of mineral trioxide aggregate in one visit apexification cases. Aust Endod J. 2003;29:34–42. doi: 10.1111/j.1747-4477.2003.tb00496.x. [DOI] [PubMed] [Google Scholar]
- 7.Parirokh M, Torabinejad M. Mineral trioxide aggregate: A comprehensive literature review—Part III: Clinical applications, drawbacks, andmechanism of action. J Endod. 2010;36:400–13. doi: 10.1016/j.joen.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Apaydin E, Shabahang S, Torabinejad M. Hard-tissue healing after application of fresh or set MTA as root-end-filling material. J Endod. 2004;30:21–4. doi: 10.1097/00004770-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Shabahang S, Torabinejad M, Boyne PP, Abedi HR, McMillan P. A comparative study of root-end induction using osteogenic protein-1, calcium hydroxide and mineral trioxide aggregate in dogs. J Endod. 1999;25:1–5. doi: 10.1016/S0099-2399(99)80388-4. [DOI] [PubMed] [Google Scholar]
- 10.Eskandarizadeh A, Parirokh M, Eslami B, Asgary S, Eghbal MJ. A comparative study between mineral trioxide aggregate and calcium hydroxide as pulp capping agent in dog's teeth. Dent Res J (Isfahan) 2005;2:1–10. [Google Scholar]
- 11.Aminozarbian MG, Barati M, Salehi I, Mousavi SB. Biocompatibility of mineral trioxide aggregate and three new endodontic cements: An animal study. Dent Res J (Isfahan) 2012;9:54–9. doi: 10.4103/1735-3327.92944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jabbarifar E, Razavi SM, Ahmadi N. Histopathologic Responses of dog's dental pulp to mineral trioxide aggregate, bio active glass, formocresol, hydroxyapatite. Dent Res J (Isfahan) 2007;4:83–7. [Google Scholar]
- 13.Torabinejad M, Ford TR, Abedi HR, Kariyawasam SP, Tang HM. Tissue reaction to implanted root-end filling materials in the tibia and mandible of guinea pigs. J Endod. 1998;24:468–71. doi: 10.1016/s0099-2399(98)80048-4. [DOI] [PubMed] [Google Scholar]
- 14.Parirokh M, Torabinejad M. Mineral trioxide aggregate: A comprehensive literature Review—Part II: Leakage and biocompatibility investigations. J Endod. 2010;36:190–202. doi: 10.1016/j.joen.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 15.AL-Heizami K, Naghshbandi J, Oglesby S, Simon JH, Rotestein I. Human saliva penetration of root canals obturated with two types of mineral trioxide aggregate cements. J Endod. 2005;31:453–6. doi: 10.1097/01.don.0000145429.04231.e2. [DOI] [PubMed] [Google Scholar]
- 16.Saatchi M, Hosseini HS, Farhad AR, Narimany T. The effect of various concentrations of iodine potassium iodide on the antimicrobial properties of mineral trioxide aggregate - A pilot study. Dent Traumatol. 2012 doi: 10.1111/j.1600-9657.2012.01119.x. [DOI] [PubMed] [Google Scholar]
- 17.Chng HK, Islam I, Yap AU, Tong YW, Koh ET. Properties of a new root-end filling material. J Endod. 2005;31:665–8. doi: 10.1097/01.don.0000157993.89164.be. [DOI] [PubMed] [Google Scholar]
- 18.Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995;21:349–53. doi: 10.1016/S0099-2399(06)80967-2. [DOI] [PubMed] [Google Scholar]
- 19.Sameei M, Eghbal MJ, Parirokh M, Abbas FM, Asgary S. Repair of furcal perforation using a new endodontic cement. Clin Oral Invest. 2010;14:653–8. doi: 10.1007/s00784-009-0351-8. [DOI] [PubMed] [Google Scholar]
- 20.Asgary S, Eghbal MJ, Parirokh M, Ghanavati F, Rahimi H. A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:609–14. doi: 10.1016/j.tripleo.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Tabarsi B, Parirokh M, Eghbal MJ, Haghdoost AA, Torabzadeh H, Asgary S. A comparative study of dental pulp response to several pulpotomy agents. Int Endod J. 2010;43:565–71. doi: 10.1111/j.1365-2591.2010.01711.x. [DOI] [PubMed] [Google Scholar]
- 22.Asgary S, Eghbal MJ, Parirokh M. Sealing ability of a novel endodontic cement as a root-end filling material. J Biomed Mater Res A. 2008;87:706–9. doi: 10.1002/jbm.a.31678. [DOI] [PubMed] [Google Scholar]
- 23.Asgary S, Eghbal MJ, Parirokh M, Torabzadeh H. Sealing ability of three commercial mineral trioxide aggregates and an experimental root-end filling material. Iran Endod J. 2006;1:101–5. [PMC free article] [PubMed] [Google Scholar]
- 24.Asgary S, Eghbal MJ, Ehsani S. Periradicular regeneration after endodontic surgery with calcium-enriched mixture cement in dogs. J Endod. 2010;36:837–41. doi: 10.1016/j.joen.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Kenee DM, Allemang JD, Johnson JD, Hellstein J, Nichol BK. Aquantitative assessment of efficacy of various calcium hydroxide removal techniques. J Endod. 2006;32:563–5. doi: 10.1016/j.joen.2005.10.065. [DOI] [PubMed] [Google Scholar]
- 26.Van der Sluis LW, Wu MK, Wesselink PR. The evaluation of removal of calcium hydroxide paste from an artificial standardized groove in the apical root canal using different irrigation methodologies. Int Endod J. 2007;40:52–7. doi: 10.1111/j.1365-2591.2006.01182.x. [DOI] [PubMed] [Google Scholar]
- 27.Ghoddusi J, Asgary S, Parirokh M, Eghbal MJ. Simulated root resorption: A new study model. Iran Endod J. 2008;2:152–5. [PMC free article] [PubMed] [Google Scholar]
- 28.Torabinejad M, Smith PW, Kettering JD, Pitt Ford TR. Comparative investigation of marginal adaptation of mineral trioxide aggregate and other commonly used root end filling materials. J Endod. 1995;21:295–9. doi: 10.1016/S0099-2399(06)81004-6. [DOI] [PubMed] [Google Scholar]
- 29.Gondim E, Jr, Kim S, de Souza-Filho FJ. An investigation of microleakage from root-end fillings in ultrasonic retrograde cavities with or without finishing: A quantitative analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:755–60. doi: 10.1016/j.tripleo.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 30.Shipper G, Grossman ES, Botha AJ, Cleaton-Jones PE. Marginal adaptation of mineral trioxide aggregate (MTA) compared with amalgam as a root-end filling material: A low-vacuum (LV) versus high-vacuum (HV) SEM study. Int Endod J. 2004;37:325–36. doi: 10.1111/j.0143-2885.2004.00806.x. [DOI] [PubMed] [Google Scholar]
- 31.Bidar M, Moradi S, Jafarzadeh H, Bidad S. Comparative SEM study of the marginal adaptation of white and grey MTA and Portland cement. Aust Endod J. 2007;33:2–6. doi: 10.1111/j.1747-4477.2007.00053.x. [DOI] [PubMed] [Google Scholar]
- 32.Xavier CB, Weismann R, de Oliveira MG, Demarco FF, Pozza DH. Root-end filling materials: Apical microleakage and marginal adaptation. J Endod. 2005;31:539–42. doi: 10.1097/01.don.0000152297.10249.5a. [DOI] [PubMed] [Google Scholar]
- 33.Bidar M, Disfani R, Gharagozloo S, Khoynezhad S, Rouhani A. Medication with calcium hydroxide improved marginal adaptation of mineral trioxide aggregate apical barrier. J Endod. 2010;36:1679–82. doi: 10.1016/j.joen.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 34.Hachmeister DR, Schindler WG, Walker WA, Thomas DD. The sealing ability and retention characteristics of mineral trioxide aggregate in a model of apexification. J Endod. 2002;28:386–90. doi: 10.1097/00004770-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 35.Porkaew P, Retief H, Barfield RD, Laceficld WR, Soong S. Effect of calcium hydroxide paste as an intracanal medicament of apical seal. J Endod. 1990;16:369–74. doi: 10.1016/S0099-2399(06)81908-4. [DOI] [PubMed] [Google Scholar]


