Abstract
Background:
Family violence, including child abuse, neglect, and domestic violence, is a public health problem. The aim of this study was to provide data on prevalence and factors of Orofacial lesions relating child abuse in Iran to lend evidence to support preventing child abuse.
Materials and Methods:
The overall approach was a case-note review of children having child abuse note, recording by personnel of social services. Research ethical approval was sought from the Central social service organization. This study was conducted in Isfahan, Iran (2011).
Result:
The mean age of children, when abuse had been occurred was 8 years (SD = 1.68), and there were approximately an equal number of boys and girls. Children had a high physical experience (66.1%).Of these children, at least 60% sustained trauma to the face and mouth. Emotional abuse was 77.1%, neglect was 64.1%, and lower experience of sexual abuse which was 4.1%. There was a strong relationship between gender and abuser which shows girls have been affected by stepfathers (P = 0.001).
Conclusion:
Preliminary data suggest that there are strong evidence regarding the incidence of child abuse relating orofacial lesions which dentists should be aware of them. Future trials may draw on these useful baseline data to help their study design.
Keywords: Child abuse, child neglect, Iran, orofacial lesions
INTRODUCTION
Child abuse is defined as any physical or emotional injury which causes harm or substantive risk of harm to the child's health or welfare. It includes sexual abuse, neglect, or being physically dependent upon an addictive drug at birth.[1] Types of child abuse, include physical abuse, emotional abuse and neglect, healthcare neglect (medical and dental), physical neglect, sexual abuse,[2] failure to thrive, safety neglect, intentional poisoning, and Munchausen Syndrome by proxy (fabricated or induced illness by parent). Factors contributing to abuse include stress[3–5] (e.g. life crises such as unemployment or homelessness), lack of a support network, substance/alcohol abuse, learned behavior (many abusers were previously victims), and other forms of family violence in the home such as spousal or elderly abuse.[6–9] Craniofacial, head, face, and neck injuries happen in more than half of the cases of child abuse.[9] Although the oral cavity is a frequent point of sexual abuse in children, obvious oral injuries or infections are rare.[10]
The American Academy of Pediatric Dentistry defined dental neglect as the willful failure of a parent or guardian to seek and follow through with treatment necessary to ensure a level of oral health essential for adequate function and freedom from pain and infection. Indeed, many dentists who regularly treat children assert that management of dental neglect is part of daily practice.[11] However, based on the literature, dentists feel unprepared to play a child protection role and are unsure what to do if they suspect that a child has been maltreated.[12–15] The aim of this study was to provide data on prevalence and factors of orofacial lesions relating child abuse in Iran to lend evidence to support preventing child abuse.
MATERIALS AND METHODS
The overall approach was a case-note review of children with child abuse history recording by personnel of social services. The social emergency services are legally eligible to separate the victims of child abuse from their families as well as interview the children and their families in order to solve their problems. Research ethical approval was sought from the Central social service organization as well as ethics committee of Isfahan University of Medical Sciences. This study was conducted in Isfahan, Iran.
Participants
For study inclusion, participating children had to have identifiable records of abuse during 2007-2011. Inclusion criteria for children dictated that they had been exposed to at least one child abuse event during this period. Children with incomplete records or missing clinical details were excluded from the study sample. The data collected retrospectively for each child, from their existing records, were as follows:
Type of abuse: physical, sexual
Patient characteristics: Age, gender
Data analysis
Descriptive statistics were used to describe child-related sociodemographic and clinical data. Type of child abuse, gender, age, and the type of abuser was described using appropriate measures of spread. Exploratory analyses including bivariate analyses and correlation were used to analyze the relationship of different variables such as child gender, age, abuse experience, abuse type as well as abuser type.
Reliability of data collection and entry were determined by recollecting 10% of the sample. All statistical tests were repeated using these data and found the same relationships between variables as identified for the original data set.
RESULTS
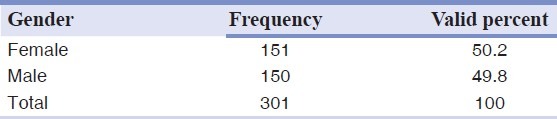
Data were obtained for 301 children from social services records. There was an equal gender distribution amongst children gender.
Patient details
The mean age of children when abuse had been occurred was 8 years (SD = 1.68) which was categorized to seven age groups [Table 1], and there were approximately an equal number of boys and girls [Table 2]. Children had a high physical experience (66.1%); of these children, at least 69% sustained trauma to the face and mouth. Emotional abuse was 77.1%, neglect was 64.1%, and lower experience of sexual abuse which was 4.1%.
Table 1.
Age of children having child abuse records categorized to seven age groups
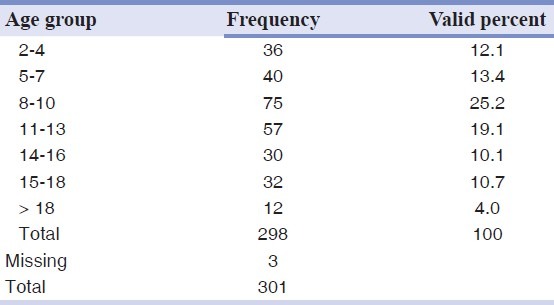
Table 2.
The gender distribution of children having child abuse records during 2007-2011
Outcomes
Exploratory bivariate analyses revealed a significant relationship between the frequency of abuse with gender and age, P = 0.008 and 0.015, respectively. Having problem such as being a mental retired and hyperactive child shows significant relationship with gender, P = 0.03 and 0.02, respectively, which was in the favor of males. There was a strong relationship between gender and abuser which shows girls have been affected by stepfathers, P = 0.001. There was also strong relationship between age of child and age of abuser, P = 0.001. However, there were no significant differences regarding age of abuser and gender of the child.
DISCUSSION
Key findings
The main purpose of this study was to obtain preliminary data to provide data on child abuse-related Orofacial lesions in order to lend evidence to prevent child abuse. This was considered important as there is a paucity of current data on the incidence of child abuse in all over the world and there is recognized need to evaluate the evidence to support dentists in different aspects of service provision.
Results of previous studies show that trauma to the head and associated areas occurs in approximately 50% of the cases of physically abused children and soft tissue injuries — most frequently bruises — are the most common injury to head and face.[15] These results are compatible with the results of our study. These findings make it obvious that dentists are in a position to detect child abuse.
The British study by Skinner and Castle (1967) documented the injuries to 78 abused children requiring medical attention[16]; of these children, at least 34 (43.5%) sustained trauma to the face and mouth. This may be an underestimate since some of the bruises were reported without noting the region. The majority of the injuries were bruises, but they also included lacerations, bites, and abrasions which support the results of our study. However, in our study, 60% of children had trauma to the face and head which was a higher prevalence.
National figures in USA indicate that as many as 1 million children are abused and/or neglected annually and of these about 1000 die each year.[17] If we assume that half of these cases involve trauma to the head, as is indicated in the literature, our profession is definitely in a position to detect and assist substantial numbers of victim-abused children. In this way, we can help to refer them to social security agencies and prevent further continuing trauma to the children by bringing help to these troubled families. The majority of victim-abused cases in our study were lower than ten years old. This group are growing and developing in sociobehavioral and physical aspects. Stress and trauma of them permanently impacted any aspects of their future life, especially in girls. The cost of orofacial trauma makes heavy burden on social security agencies and their families.
CONCLUSION
This is the first study in Iran to provide data for the evaluation of orofacial lesions relating child abuse. Preliminary data suggest that there are strong evidence regarding the incidence of child abuse relating orofacial lesions which dentists should be aware of them. Future trials may draw based on these useful baseline data to help their study design.
ACKNOWLEDGMENT
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. There was no particular conflict of interest with any organization.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Needleman HL. Orofacial trauma in child abuse: Types, prevalence, management, and the dental profession's involvement. Pediatr Dent. 1986;8:71–80. [PubMed] [Google Scholar]
- 2.Baetz K, Sledziewski W, Margetts D, Koren L, Levy M, Pepper R. Recognition and management of the battered child syndrome. J Dent Assoc S Afr. 1977;32:13–8. [PubMed] [Google Scholar]
- 3.Becker DB, Needleman HL, Kotelchuck M. Child abuse and dentistry: Orofacial trauma and its recognition by dentists. J Am Dent Assoc. 1978;97:24–8. doi: 10.14219/jada.archive.1978.0447. [DOI] [PubMed] [Google Scholar]
- 4.Cameron JM, Johnson HR, Camps FE. The battered child syndrome. Med Sci Law. 1966;6:2–21. doi: 10.1177/002580246600600102. [DOI] [PubMed] [Google Scholar]
- 5.Jessee SA. Physical manifestations of child abuse to the head, face and mouth: A hospital survey. ASDC J Dent Child. 1995;62:245–9. [PubMed] [Google Scholar]
- 6.Jessee SA, Rieger M. A study of age-related variables among physically abused children. ASDC J Dent Child. 1996;63:275–80. [PubMed] [Google Scholar]
- 7.Malecz RE. Child abuse, its relationship to pedodontics: A survey. ASDCJ Dent Child. 1979;46:193–4. [PubMed] [Google Scholar]
- 8.O’Neill JA, Jr, Meacham WF, Griffin JP, Sawyers JL. Patterns of injury in the battered child syndrome. J Trauma. 1973;13:332–9. doi: 10.1097/00005373-197304000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Skinner AE, Castle RL. 78 battered children: A retrospective study. London, England: National Society for the Prevention of Cruelty to Children; 1969. [Google Scholar]
- 10.Tate RJ. Facial injuries associated with the battered child syndrome. Br J Oral Surg. 1971;9:41–5. doi: 10.1016/s0007-117x(71)80007-0. [DOI] [PubMed] [Google Scholar]
- 11.Kittle PE, Richardson DS, Parker JW. Two child abuse/child neglect examinations for the dentist. J Dent Child. 1981;48:175–80. [PubMed] [Google Scholar]
- 12.Harris JC, Elcock C, Sidebotham PD, Welbury RR. Safeguarding children in dentistry: 2. Do paediatric dentists neglect child dental neglect? Br Dent J. 2009;206:465–70. doi: 10.1038/sj.bdj.2009.356. [DOI] [PubMed] [Google Scholar]
- 13.Lazenbatt A, Freeman R. Recognizing and reporting child physical abuse: A survey of primary healthcare professionals. J Adv Nurs. 2006;56:227–36. doi: 10.1111/j.1365-2648.2006.04030.x. [DOI] [PubMed] [Google Scholar]
- 14.Welbury RR, MacAskill SG, Murphy JM. General dental practitioners’ perception of their role within child protection: A qualitative study. Eur J Paediatr Dent. 2003;4:89–95. [PubMed] [Google Scholar]
- 15.Cairns AM, Mok JY, Welbury RR. The dental practitioner and child protection in Scotland. Br Dent J. 2005;199:517–20. doi: 10.1038/sj.bdj.4812809. [DOI] [PubMed] [Google Scholar]
- 16.Tymiak R. Dentists-face to face with a battered child. Ill Dent J. 1978;47:484–7. [PubMed] [Google Scholar]
- 17.J Dent Child. Vol. 46. Washington: U.S. Department of Health and Human Services; 1979. National study of the incidence and severity of child abuse and neglect: Executive summary; pp. 193–4. [Google Scholar]


