Abstract
Background:
Several studies have hypothesized that periodontal diseases may increase the risk of preeclampsia. The purpose of this study was to compare periodontal parameters in preeclamptic and normotensive pregnant women 48 hours after delivery.
Materials and Methods:
A case-control study was carried out on 26 pure preeclamptic women and 25 women with normal pregnancy. The participants did not have any systemic disease that may affect both preeclampsia and periodontal conditions. Clinical parameters measured in case and control groups include attachment loss, gingival bleeding index, and plaque index. These indices were measured in all teeth except the third molars. The data from each subject were reported in mean and finally the average amount of each group was compared to others and analyzed using SPSS software, t-test, and Mann-Whitney test.
Results:
Mean of gestational age at delivery in preeclamptic and normotensive groups was respectively 33.2 ± 3.89 weeks and 36.5 ± 3.08 weeks. A significant difference was observed in preeclamptic women compared to controls (P = 0.01). There were no statistical differences between groups with regard to mean clinical attachment loss (P = 0.16), mean gingival bleeding (P = 0.89), and mean plaque (P = 0.95) indices.
Conclusion:
The present study showed that maternal periodontal diseases during pregnancy are not associated with preeclampsia.
Keywords: Periodontal index, preeclampsia, pregnancy outcome
INTRODUCTION
Periodontal disease is one of the most common chronic disorders of infectious origin in human beings, with a reported prevalence varying between 10 and 60% in adults.[1–4] The past 5 years have witnessed an increase in research evidence suggesting association between periodontal disease and increased risk of systemic disease such as atherosclerosis, myocardial infarction, stroke, diabetes mellitus, and adverse pregnancy outcomes.[5–8]
Adverse pregnancy outcomes that have been linked to periodontal disease include preterm birth, low birth weight, miscarriage or early pregnancy loss, and preeclampsia. Preeclampsia and preterm births are major causes of maternal and prenatal morbidity and mortality.[9,10] The specific etiologies and pathogeneses of these outcomes are still unclear. Periodontal disease as an independent risk factor for adverse pregnancy outcomes would be of great public health importance and is preventable and at the same time curable.[11]
Preeclampsia was defined by the American Congress of Obstetricians and Gynecologists criteria as blood pressure >140/90 mmHg and > or = 1+ proteinuria on a catheterized urine specimen.[12]
Lohsoonthorn, et al.[13] in a case-control study after periodontal examination 48 hours of delivery concluded that there is not meaningful difference in periodontal parameters between preeclamptic and normotensive women, whereas Nabet, et al.[12] demonstrated significant relationship between generalized periodontitis and preterm labor induced by preeclampsia.
In the present study, we evaluated periodontal parameters in women with preeclampsia and normal pregnant women.
MATERIALS AND METHODS
Study population
In our case-control study, 51 pregnant women (26 pure preeclampsia and 25 normotensive pregnant women) who were admitted to the Department of Obstetrics and Gynecology, Isfahan University of Medical Science, Isfahan, Iran were selected. Preeclampsia has been defined by the American Congress of Obstetricians and Gynecologists criteria as blood pressure >140/90 mmHg and > or = 1+ proteinuria on a catheterized urine specimen.
The age of participants ranged from 17 to 45 years. The inclusion criterion was the presence of chronic periodontitis (presence of clinical attachment loss).Women were excluded if they had chronic hypertension, diabetes, urinary infection, cardiac disease, rupture of membrane, any medical conditions requiring antibiotics or were alcohol consumers or smokers. All subjects were provided with written informed consent.
Data collection
Data about maternal age, gestational age at delivery, and number of pregnancies were collected. Periodontal condition was evaluated 48 hours after delivery in all teeth except the third molars utilizing following indices:
1-CAL (clinical attachment loss)[14]
2-GBI (gingival bleeding index [Ainamoand Bay])[15]
3-PI (plaque index [Silness and Löe])[16]
For this purpose, we used disposable mirror, strilled explorer 17-23, and pressure sensitive probe O’Mishigan for each participant.
Measurement method
Level of attachment is the distance between the base of the pocket and a fixed point on the crown, such as the cementoenamel junction (CEJ).[14] In this study, the distance between CEJ and the bottom of pocket was measured in buccal, lingual, mesial, and distal surfaces of each tooth except the third molars and was registered in a chart in millimeter. Finally, all data were collected then divided into their numbers and a mean was registered for the whole mouth.
GBI was used to evaluate the severity of gingival inflammation at four gingival units of each tooth except the third molars. To evaluate GBI, the probe is placed 1 mm in the gingival sulcus moving along the soft tissue of the pocket. After 10 seconds, we recorded any occurred bleeding. Finally, the number of bleeding areas was divided by the number of the total examined regions and then multiplied into 100, and the result was expressed as percentage.[15]
For measurement of plaque index, the teeth (except the third molars) were evaluated by an explorer 17-23 along the gingival margin in 4 sites: Buccal, lingual, mesial, and distal. If there was no plaque at the gingival margin, the score was recorded as 1, score 2 indicates a thin layer of plaque, score 3 is due to moderate layer of plaque, and if an excessive accumulation of plaque is at the gingival margin the score is 4.[16] So, for each tooth, 4 scores existed and their average was recorded for the whole mouth. The data in each sample were expressed in mean and the average of each index was compared in both groups.
Statistical analysis
First, the characteristics of case and control women were compared, and then the distribution of periodontal status was assessed in both groups. Data were analyzed using SPSS software, t-test, and Mann-Whitney test. The P value greater than 0.05 was considered to be significant.
RESULTS
Mean of maternal age in case group (women with preeclampsia) was 28.5 ± 4.5 years and 27.8 ± 5.6 years in control group, so there was no significant difference between them (P = 0.64) [Table 1].
Table 1.
Mean of maternal age, gestational age at delivery, and number of pregnancies in case and control groups
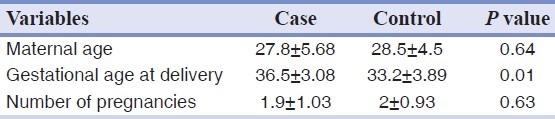
Gestational age at delivery was 33.2 ± 3.89 weeks in case group and 36.5 ± 3.02 weeks in control group, so significant difference was observed between two groups (P = 0.01) [Table 1].
The mean number of pregnancies did not differ significantly between case and control groups (P = 0.63), as they were 1.9 ± 1.03 in control group and 2 ± 0.93 in case group [Table 1].
Mean of GBI in case and control groups was 9.8 ± 14.44 and 7.6 ± 6.71, respectively. No clinically meaningful differences were observed between case and control groups with regard to GBI (P = 0.89) [Table 2].
Table 2.
Mean of CAL, GBI, and PI in case and control groups
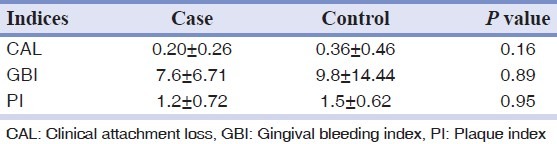
The difference between the average of PI was not statistically significant (P = 0.95), as it was 1.5 ± 0.62 in case group vs 1.2 ± 0.72 in control group [Table 2].
Mean of clinical attachment loss was not significantly different between two groups (P = 0.16), being 0.36 ± 0.46 mm in case vs. 0.20 ± 0.26 mm in control [Table 2].
DISCUSSION
The aim of this study was to evaluate the association between periodontal disease and preeclampsia. Data about the maternal age, gestational age at delivery, and frequency of pregnancies were collected and then compared to each others in both groups. Statistical analysis showed that except the gestational age at delivery, P = 0.01. There were no significant correlation between these items in two groups (P > 0.05). Of course, we should notice to this point that the determinant treatment for preeclampsia is rapid termination of pregnancy because of the probability of seizure and prenatal and maternal morbidity.[8]
Periodontal indices including CAL, GBI, and PI were measured in both groups and were then compared between case and control groups. Since periodontal infection causes transient and low-grade bacteremias and endotoxemias in the body, promotes systemic inflammatory and immune responses, and also the circulating CRP (C-reactive protein) level is elevated in both periodontal disease and adverse pregnancy outcomes,[17,18] so at first we hypothesized that preeclampsia is associated with periodontal disease, but based on this study the difference in the mean of indices was not statistically significant (P > 0.05). The association between periodontal inflammation and preeclampsia has been evaluated in several studies. In 2009, Srinivas, et al.[19] demonstrated in an extensive multi-centered cohort study no significant relation between periodontal disease and pregnancy complications (preterm birth, preeclampsia, infant's death or low birth weight), that was consistent with the results of our study.
In 2009, Lohsoonthorn, et al.[13] in a case-control study on the normotensive and preeclamptic pregnant women 48 hours of delivery reported no significant difference between rate of periodontal disease between two groups. This study also expressed that with increasing the severity of periodontal disease, the risk of preeclampsia does not increase.[13] In contrast, in 2008, Baggs and Ruma[18] concluded in a cohort study after detecting periodontal condition and the level of CRP in serum (before the 26th week until delivery) in pregnant women that maternal periodontal disease with systemic inflammation is associated with an increased risk for preeclampsia.[20]
However, we evaluated periodontal conditions in a time frame of 48 hours after delivery using clinical indices and we did not evaluate the laboratory parameters; and this maybe a cause to the controversy. In another study, in 2007, Canaki, et al.[21] indicated that presence and severity of periodontal disease seems to increase the risk of not only the occurrence but also the severity of preeclampsia. In this study, (IL) 1-beta, PGE2 levels and TNF alpha were evaluated in both gingival crevicular fluid and serum, but our study only evaluated clinical periodontal parameters.
In another study performed by Shetty, et al.[22] in 2010, after oral health examination on 130 pregnant women at recruitment and 48 hours of delivery, he demonstrated that periodontitis at both times may be associated with an increased risk of preeclampsia. Khader, et al.[23] showed no significant relationship between the number of filled surfaces, missing teeth and also periodontal parameters, and occurrence of preeclampsia. A randomized controlled trial in pregnant women with periodontitis found that treatment of periodontitis (compared with no treatment) before 21 weeks of gestation did not reduce preterm birth; it did not reduce the preeclampsia rate either, but that rate was low.[24]
From above, it seems that various studies about the association between periodontal disease and preeclampsia show conflicting reports due to different reasons. One of them is the heterogenicity nature of preeclampsia and periodontal disease. Since various factors are included in the etiology of preeclampsia and periodontal disease, it is very difficult to evaluate just one reason cross-sectionally in a way that the confounding factors become eliminated. It seems that use of diagnostic laboratory tests accompanying paraclinical indices for detecting the inflammatory factors in gingival crevicular fluid and serum will be more reliable.
Extensive cohort studies in which priority and delay between the cause and effect are determined can decrease the confounding effects, and the results get closer to the reality.
CONCLUSION
Based on this study, there is no significant association between periodontal disease and preeclampsia in pregnant women.
Footnotes
Source of Support: This report is based on a thesis which was submitted to the School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran, in partial fulfillment of the requirements for the DMD degree. The study was approved by the Medical Ethics and Research Office at the Isfahan University of Medical Sciences and financially supported by this University
Conflict of Interest: None declared
REFERENCES
- 1.Papapanou PN. Periodontal diseases: Epidemiology. Ann Periodontol. 1996;1:1–36. doi: 10.1902/annals.1996.1.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Albandar JM, Rams TE. Global epidemiology of periodontal diseases: An overview. Periodontol 2000. 2002;29:7–10. doi: 10.1034/j.1600-0757.2002.290101.x. [DOI] [PubMed] [Google Scholar]
- 3.Albandar JM. Periodontal diseases in North America. Periodontol 2000. 2002;29:31–69. doi: 10.1034/j.1600-0757.2002.290103.x. [DOI] [PubMed] [Google Scholar]
- 4.Offenbacher S, Lieff S, Boggess KA, Murtha AP, Madianos PN, Champagne CM, et al. Maternal periodontitis and prematurity. Part I: Obstetric outcome of prematurity and growth restriction. Ann Periodontol. 2001;6:164–74. doi: 10.1902/annals.2001.6.1.164. [DOI] [PubMed] [Google Scholar]
- 5.Chopra R, Patil SR, Mathur S. Comparison of cardiovascular disease risk in two main forms of periodontitis. Dent Res J (Isfahan) 2012;9:74–9. doi: 10.4103/1735-3327.92953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia RI, Henshaw MM, Krall EA. Relationship between periodontal disease and systemic health. Periodontol 2000. 2001;25:21–36. doi: 10.1034/j.1600-0757.2001.22250103.x. [DOI] [PubMed] [Google Scholar]
- 7.Champagne CM, Madianos PN, Lieff S, Murtha AP, Beck JD, Offenbacher S. Periodontal medicine: Emerging concepts in pregnancy outcomes. J IntAcadPeriodontol. 2000;2:9–13. [PubMed] [Google Scholar]
- 8.Paquette DW. The periodontal infection-systemic disease link: A review of the truth or myth. J Int Acad Periodontol. 2002;4:101–9. [PubMed] [Google Scholar]
- 9.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 10.Shennan AH. Recent developments in obstetrics. BMJ. 2003;327:604–18. doi: 10.1136/bmj.327.7415.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiong X, Buekens P, Fraser WD, Beck J, Offenbacher S. Periodontal disease and adverse pregnancy outcomes: A systematic review. BJOG. 2006;113:135–43. doi: 10.1111/j.1471-0528.2005.00827.x. [DOI] [PubMed] [Google Scholar]
- 12.Nabet C, Lelong N, Colombier ML, Sixou M, Musset AM, Goffinet F, et al. Maternal periodontitis and the causes of preterm birth: The case-control Epipap study. J Clin Periodontol. 2010;37:37–45. doi: 10.1111/j.1600-051X.2009.01503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lohsoonthorn V, Kungsadalpipob K, Chanchareonsook P, Limpongsanurak S, Vanichjakvong O, Sutdhibhisal S, et al. Maternal periodontal disease and risk of preeclampsia: A case-control study. Am J Hypertens. 2009;22:457–63. doi: 10.1038/ajh.2008.365. [DOI] [PubMed] [Google Scholar]
- 14.Carranza FA, Takei HH. Diagnosis, prognosis and treatment plan. In: Newman MG, Takei HH, editors. 10th ed. St Louis: Saunder Elsevier; 2006. p. 553. [Google Scholar]
- 15.Ainamo J, Bay I. Problems and proposal for recording gingivitis and plaque. Int Dent J. 1975;25:229–35. [PubMed] [Google Scholar]
- 16.Silness J, Löe H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 17.Sharma A, Ramesh A, Thomas B. Evaluation of plasma C-reactive protein levels in pregnant women with and without periodontal disease: A comparative study. J Indian Soc Periodontol. 2009;13:145–9. doi: 10.4103/0972-124X.60227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hradecky L, Subrt I, Ulcova-Gallovaz Z. Urgent termination of pregnancy in preeclampsia and panel of antiphospholipid antibodies. Am J Reprod Immunol. 2009;62:412–7. doi: 10.1111/j.1600-0897.2009.00759.x. [DOI] [PubMed] [Google Scholar]
- 19.Srinivas SK, Sammel MD, Stamilio DM, Clothier B, Jeffcoat MK, Parry S, et al. Periodontal disease and adverse pregnancy outcomes: Is there an association? Am J Obstet Gynecol. 2009;200:497.e1–8. doi: 10.1016/j.ajog.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Ruma M, Boggess K, Moss K, Jared H, Murtha A, Beck J, et al. Maternal periodontal disease, systemic inflammation, and risk for preeclampsia. Am J Obstet Gynecol. 2008;198:389.e1–5. doi: 10.1016/j.ajog.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Canakci V, Canakci CF, Yildirim A, Ingec M, Eltas A, Erturk A. Periodontal disease increases the risk of severe pre-eclampsia among pregnant women. J Clin Periodontol. 2007;34:639–45. doi: 10.1111/j.1600-051X.2007.01105.x. [DOI] [PubMed] [Google Scholar]
- 22.Shetty M, Shetty PK, Ramesh A, Thomas B, Prabhu S, Rao A. Periodontal disease in pregnancy is a risk factor for preeclampsia. Acta Obstet Gynecol Scand. 2010;89:718–21. doi: 10.3109/00016341003623738. [DOI] [PubMed] [Google Scholar]
- 23.Khader YS, Jibreal M, Al-Omiri M, Amarin Z. Lack of association between periodontal parameters and preeclampsia. J Periodontol. 2006;77:1681–7. doi: 10.1902/jop.2006.050463. [DOI] [PubMed] [Google Scholar]
- 24.Michalowicz BS, Hodges JS, Diangelis AJ, Lupo VR, Novak MJ, Ferguson JE, et al. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355:1885–94. doi: 10.1056/NEJMoa062249. [DOI] [PubMed] [Google Scholar]


