Abstract
Eosinophilic granuloma is a rare disease which is difficult to diagnose clinically and radiographically. Localized Langerhans’ cell histiocytosis, previously known as eosinophilic granuloma, mainly affects the skull, mandible, vertebrae, pelvis and ribs in children and the long bones of adults. We present a case report of a female who developed pain and swelling over the left mandibular region, and was later diagnosed as eosinophilic granuloma, which after administration of intralesional corticosteroid with surgical enucleation showed positive response. This disease is of importance to dental professionals because early clinical signs can occur in the jaw and can cause extensive destruction of the periodontal tissues and bone. The purpose of this case report is to describe a case of eosinophilic granuloma with emphasis on conservative approach for the treatment and the radiographic changes observed during and after the treatment.
Keywords: Adrenal cortex hormones, eosinophilic granuloma, Langerhans’ cell histiocytosis
INTRODUCTION
Eosinophilic granuloma (EG) is a benign lytic lesion of bone characterized by increased histiocytes. It is classified with Hand-Schüller-Christian and Letterer-Siwe diseases as a member of the reticuloendothelial disorder group, Langerhans’ Cell Histiocytosis (LCH). In 1953, Lichtenstein grouped this disease under the name histiocytosis X.[1] The “X” referred to the fact that the etiology was unknown. However, in 1987, the term “Langerhans’ Cell Histiocytosis” (LCH) was introduced by the “Writing Group of the Histiocyte Society”.[2] Eosinophilic granuloma is the most common benign lesion and accounts for 50-60% of all cases of this disease.[3,4] It can affect almost any bone and commonly involves the mandible when the jaws are affected.[5–7]
Eosinophilic granuloma has been treated with surgery, radiotherapy, chemotherapy and intralesional steroid injections.[5,8,9] Recurrence rate in multifocal eosinophilic granuloma is high. Most of the authors advised mandibular resection for recurrent lesions. In the present case, after the first recurrence, systemic and intralesional corticosteroids with surgical curettage were given to the patient. The clinical and radiographical changes observed during two years of duration are reported in the present paper with special emphasis on intralesional corticosteroids in the management of eosinophilic granuloma.
CASE REPORT
A 51-year-old female referred to our department with the complaint of pain and swelling in the left mandibular region since two years. During systemic history, patient revealed low back pain, hypertension and diabetic mellitus Type 2 since 10-11 years. She underwent surgery of the maxillary sinus region which as per her previous records was treated with FESS (functional endoscopic sinus surgery), left conchaplasty with widening of maxillary sinus. The biopsied tissue of the ophthalmic and maxillary region showed inflammatory cells and was not suggestive of any malignancy. During course of time patient underwent root canal treatments of mandibular molars, premolars and incisors for her dental pain. However, the pain did not subside and patient referred to our department. On examination pain was mild, dull, and localized in nature. The family history of the patient was not contributory. Physical examination showed facial asymmetry attributable to diffuse swelling of the left mandibular region. Mouth opening and sensation over the distribution of the left inferior alveolar nerve was normal. Intraorally, the alveolar ridge posterior to the right first molar was covered with intact, normal-appearing mucosa. No teeth showed mobility or pain on percussion. There was no cervical or axillary lymphadenopathy. A two-year-old panoramic radiograph [Figure 1] showed an ill-defined osteolytic lesion in the left posterior mandibular body, with involvement of the apices of both the first molar and the second molar and in the anterior part of the mandible involving the incisors and premolars of the left side of the mandible. However, a recent panoramic radiograph showed massive increase of erosion in the posterior and anterior part of the mandible [Figure 2].
Figure 1.

Old orthopantomogram depicting osteolytic lesions in the left mandibular posterior and anterior part in the year 2007
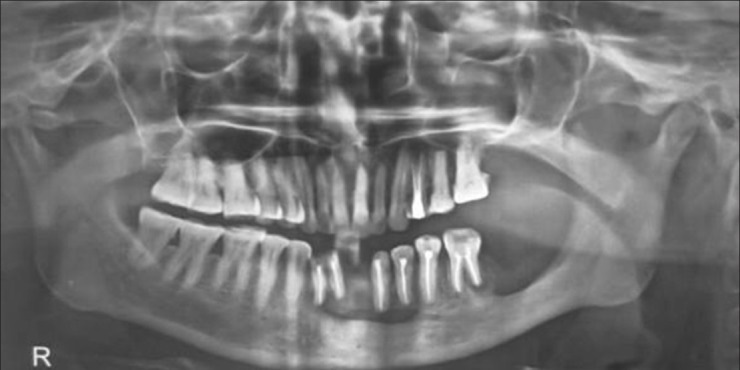
Figure 2.

Orthopantomogram showing increase in the radiolucency and the size of the lesions after two years (2009)
Because the clinical and radiographic findings led to suspicion of a malignancy, surgical intervention with biopsy of the lesion was planned and performed. The specimen, which was friable and resembled granulation tissue, showed a proliferation of histiocytic cells and an infiltration of eosinophils and neutrophils on microscopic examination. Soft-tissue fragments permeated by hematopoietic cells and predominantly mononuclear cells with clefted nuclei and granular cytoplasm were seen admixed with eosinophils, neutrophils and lymphocytes [Figure 3]. Immunohistochemical staining showed that the histiocytic cells were positive for the CD 68, CD1a, S-100 protein [Figures 4–6], and Myeloperoxidaes were positive in the surrounding granulocytes. The CD 45 was also positive in lymphocytes [Figure 6].
Figure 3.
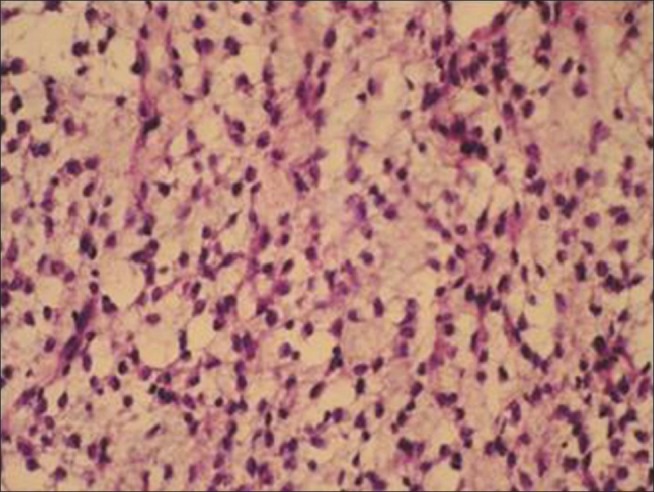
Histopathological picture showing predominantly mononuclear cells with clefted nuclei and granular cytoplasm admixed with eosinophils, neutrophils and lymphocytes
Figure 4.
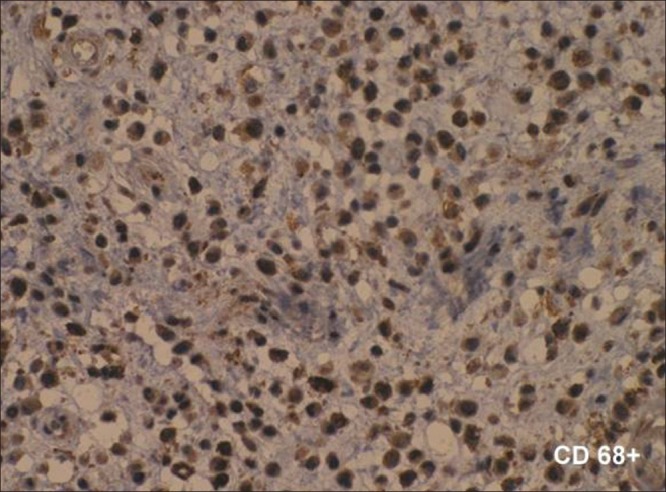
Immunohistochemistry showing that histiocytic cells were positive for the CD 68
Figure 6.
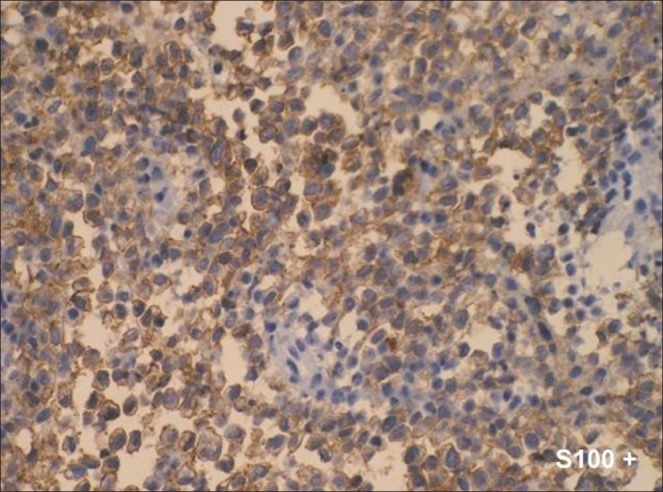
Immunohistochemistry showing that histiocytic cells were positive for the S-100 protein
Figure 5.
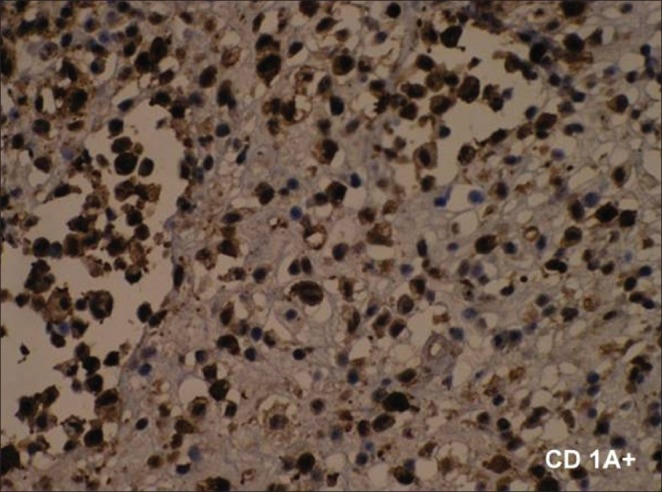
Immunohistochemistry showing that histiocytic cells were positive for the CD 1A
These features were consistent with a diagnosis of eosinophilic granuloma. To evaluate the possibility of systemic histiocytosis X, a radiographic skeletal survey and a visceral ultrasound was performed. These examinations detected no other lesions except a few changes in sacroiliac joint. The results of laboratory tests, consisting of blood and serum biochemical studies, were within normal ranges except there was a significant increase in ESR observed. A chest radiograph did not show any significant abnormality. Consequently, the mandibular lesion was diagnosed as eosinophilic granuloma. After three weeks of surgery the mandibular swelling decreased rapidly, and there was marked improvement in the facial asymmetry. Patient reported again after one year to us with a pain in the right mandibular posterior region. Computed tomography (CT) scans showed a destructive bony lesion extending from the mesial side of the right first premolar to the distal side of the second premolar [Figure 7]. A separate well-defined new radiolucent lesion was observed distal to the left mandibular first molar [Figure 8].
Figure 7.

Computed tomography scan
Figure 8.

A separate well-defined new radiolucent lesion observed distal to the left mandibular first molar
Second surgery with curettage of the lesion was done along with biweekly intralesional 40 mg injections of methylprednisolone in the posterior lesion for the next eight weeks. The patient was also given systemic steroid Defcort 6 mg (Deflazacortil, Mehius India) per day for 30 days in a tapering manner along with surgical curettage. The patient was evaluated after every six months for the next two years. Patient was free of symptoms and signs and her radiographs revealed healed lesions in the anterior and posterior part of the mandible [Figure 9].
Figure 9.
Post-treatment orthopantomogram showing complete bone formation distal to the left mandibular first molar
DISCUSSION
Eosinophilic granuloma, known as benign localized LCH, represents the most common form of this disease and presents single or multiple skeletal lesions. Solitary lesions are more common than multiple lesions. When multiple lesions occur, the new osseous lesions appear within 1-2 years, and the condition is still classified as eosinophilic granuloma. Radiologically this lesion is characterized by destructive lytic bone lesion, edges of which may be bevelled, scalloped or confluent (geographic), or show a “button sequestrum”.[10,11]
Choosing the treatment option for eosinophilic granuloma is highly debatable. Treatment of eosinophilic granuloma is important because local expansion can cause destruction of the bone and sometimes fracture of the jaw.[12,13] Eosinophilic granuloma has been conventionally treated with surgery, radiotherapy, chemotherapy, and steroid injections, alone or in combination.[3,7,8] However, a few reports have described spontaneous resolution after biopsy.[14] The major drug modalities available and which have shown good results include methyl prednisolone, 2-Chlorodeoxyadenosine,[15] etoposide, 2-deoxycoformin,[16] vinblastine,[17] mercaptopurine, methotrexate, interferon and interleukin. Comparing the two different trials conducted by Histiocyte Society and “DAL/HX 83”, the later showed a better response rate and mortality in which six weeks’ initial treatment with methylprednisone, vinblastin and etoposide was given followed by mercaptopurine, vinblastin and prednisolone for one year.[18] In addition to many therapeutic combinations including surgery, chemotherapy and radiation, new therapeutic strategies are represented by monoclonal CD-1a-antibody-therapy[19] and gene transfer into hemopoietic progenitor cells.[19,20]
Curettage of the lesion has been suggested but complete removal of the lesion is not necessary in most cases. Intralesional corticosteroids were used along with the surgical curettage because of the fact that surgical curettage alone showed recurrence of the lesion as well as appearance of new lesion [Figure 8]. The role of corticosteroids in the treatment of eosinophilic granuloma is well documented.[4,20,21] Methylprednisolone is an effective immunosuppressive and anti-inflammatory agent when administered systemically and is effective in bone cysts as it destroys granulomatous tissue and induces osteogenesis.[3] Harris and Woo reviewed a series of seven patients with LCH of the orbit. Two patients were treated with biopsy and low-dose radiation and five patients had subtotal curettage at the time of biopsy; four of five received simultaneous intralesional corticosteroid injection, no local recurrence or additional focus was noted in follow-up periods of 1 to 17 years.[22]
In our case when the patient was evaluated after one year of surgery, a new lesion was seen as on radiograph [Figure 8]. After discussion it was decided to give biweekly intralesional injection of methylprednisolone 40 mg and systemic steroid Defcort 6 mg (Deflazacortil, Mehius India) per day for 30 days in a tapering manner along with surgical curettage. Accessible lesions are best managed by curettage[11,23–26] which can be done intraorally. When these lesions are not accessible by curettage or if the operation will result in a gross disfigurement, low-dose radiation of 6-10 Gy or chemotherapy can be used.[5,25] The recurrence rate of eosinophillic granuloma ranges from 1-25%, depending on the treatment protocol and the location of the lesion.[5,7] Postovsky[27] recommends mandibulectomy in case of recurrence.
There are a variety of therapeutic approaches to multifocal eosinophillic granuloma. Taking into account a propensity to spontaneous healing of some of these lesions, it may be prudent to leave them without any therapeutic intervention, if the lesions do not pose a direct danger to the functioning of adjacent structures or cause major cosmetic defects.[26,27] In the present case, the patient was symptomatic with regard to the multiple, small lesions in her mandible. Therefore a “wait and watch” strategy could not be applied for these lesions. According to the literature, there are only two reports associated with spontaneous remission of Langerhans’ cell histiocytosis after biopsy.[6,27] In the present case, the patient was followed up clinically and radiographically for two years. After three weeks of intralesional methylprednisone injection and systemic corticosteroid with surgical curettage, remissions associated with clinical and radiographic improvement have occurred in the jaws.
CONCLUSION
Eosinophilic granuloma often presents with a wide range of clinical symptoms and sometimes with an unpredictable clinical course requiring multiple surgical as well as non-surgical interventions. We provide additional and independent evidence of the efficacy of intralesional and systemic corticosteroids in the management of recurrent polyostotic eosinophilic granuloma of the mandible. This method is also minimally invasive and relatively inexpensive, although some adverse effects are possible. Further studies are required to evaluate the safety and efficacy of this treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Lichtenstein L. Histiocytosis X. Integration of Eosinophilic granuloma of bone, Letterer-Siwe disease, and Schüller-Christian disease as related manifestations of a single oncologic entity. AMA Arch Pathol. 1953;56:84–102. [PubMed] [Google Scholar]
- 2.Chu T, D’Angio GJ, Favara BE, Ladisch S, Nesbit M, Pritchard J. Histiocytosis syndromes in children. Lancet. 1987;2:41–2. doi: 10.1016/s0140-6736(87)93074-1. [DOI] [PubMed] [Google Scholar]
- 3.Cohen M, Zornoza J, Cangir A, Murray JA, Wallace S. Direct injection of methylprednisolone sodium succinate in the treatment of solitary eosinophilic granuloma of bone. Radiology. 1980;136:289–93. doi: 10.1148/radiology.136.2.7403498. [DOI] [PubMed] [Google Scholar]
- 4.Lee R, Jones, Toth Bela B, Cangir Ayten. Treatment for Solitary Eosinophilic Granuloma of the Mandible by Steroid Injection. Report of a Case. J Oral Maxillofac Surg. 1989;47:306–9. doi: 10.1016/0278-2391(89)90238-3. [DOI] [PubMed] [Google Scholar]
- 5.Ardekian L, Peled M, Rosen D, Rachmiel A, Abu el-Naaj I, Laufer D. Clinical and radiographic features of eosinophilic granuloma in the jaws. Review of 41 lesions treated by surgery and low-dose radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:238–42. doi: 10.1016/s1079-2104(99)70279-9. [DOI] [PubMed] [Google Scholar]
- 6.Gnanasekhar JD, Ahmad MS, Reddy RR. Multifocal Langerhans cell histiocytosis of the jaws: A case report. Quintessence Int. 1991;22:559–64. [PubMed] [Google Scholar]
- 7.Hartman KS, Histiocytosis X. A review of 114 cases with oral involvement. Oral Surg Oral Med Oral Pathol. 1980;49:38–54. doi: 10.1016/0030-4220(80)90030-4. [DOI] [PubMed] [Google Scholar]
- 8.Roychoudhury A, Shah N, Parkash H, Mukhopadhyay S, Chopra P. Eosinophilic granuloma of the jaws. Br J Oral Maxillofac Surg. 1998;36:380–3. doi: 10.1016/s0266-4356(98)90651-9. [DOI] [PubMed] [Google Scholar]
- 9.Sartoris DJ, Parker BR. Histiocytosis X: Rate and pattern of resolution of osseous lesions. Radiology. 1984;152:679–84. doi: 10.1148/radiology.152.3.6611563. [DOI] [PubMed] [Google Scholar]
- 10.Hicks J, Flaitz CM. Langerhans cell histiocytosis: Current insights in a molecular age with emphasis on clinical oral and maxillofacial pathology practice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:S42–66. doi: 10.1016/j.tripleo.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 11.Artzi Z, Grosky M, Raviv M. Periodontal manifestations of adult onset of histiocytosis X. J Periodontol. 1989;60:57–66. doi: 10.1902/jop.1989.60.1.57. [DOI] [PubMed] [Google Scholar]
- 12.Holzhauer AM, Abdelsayed RA, Sutley SH. Eosinophilic granuloma: A case report with pathologic fracture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:756–9. doi: 10.1016/s1079-2104(99)70176-9. [DOI] [PubMed] [Google Scholar]
- 13.Watzke IM, Millesi W, Kermer C, Gisslinger H. Multifocal eosinophilic granuloma of the jaws: Long-term follow-up of a novel intraosseous corticoid treatment for recalcitrant lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:317–22. doi: 10.1067/moe.2000.107535. [DOI] [PubMed] [Google Scholar]
- 14.Tomono Namai, Hiroshi Yusa, Hiroshi Yoshida. Spontaneous Remission of a Solitary Eosinophilic Granuloma of the Mandible after Biopsy: A Case Report. J Oral Maxillofac Surg. 2001;59:1485–7. doi: 10.1053/joms.2001.28290. [DOI] [PubMed] [Google Scholar]
- 15.Dhall G, Finlay JL, Dunkel IJ, Ettinger LJ, Kellie SJ, Allen JC, et al. Analysis of Outcome for Patients with Mass Lesions of the Central Nervous System due to Langerhans Cell Histiocytosis with 2-Chlorodeoxyadenosine. Pediatr Blood Cancer. 2008;50:72–9. doi: 10.1002/pbc.21225. [DOI] [PubMed] [Google Scholar]
- 16.McCowage GB, Frush DP, Kurtzberg J. Successful treatment of two children with Langerhans’ cell histiocytosis with 20-deoxycoformycin. J Pediatr Hematol Oncol. 1996;18:154–8. doi: 10.1097/00043426-199605000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Jones B, Kung F, Chevalier L. Chemotherapy of reticuloendotheliosis. Comparison of methotrexate plus prednisolone vs. vincristine plus prednisolone. Cancer. 1974;34:1011–7. doi: 10.1002/1097-0142(197410)34:4<1011::aid-cncr2820340408>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 18.Eckardt A, Schultze A. Maxillofacial manifestations of Langerhans cell histiocytosis: A clinical and therapeutic analysis of 10 patients. Oral Oncol. 2003;39:687–94. doi: 10.1016/s1368-8375(03)00080-0. [DOI] [PubMed] [Google Scholar]
- 19.Kelly KM, Pritchard J. Monoclonal antibody therapy in Langerhans cell histiocytosis-feasible and reasonable? Br J Cancer. 1994;70:54–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Brenner M. Current status of gene transfer into hematopoietic progenitor cells: Application to langerhans cell histiocytosis. Br J Cancer. 1994;70:56–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Scaglietti Marchetti PG, Bartolozzi P. The effects of methylprednisolone acetate in the treatment of bone cysts. J Bone Joint Surg. 1979;61:200–4. doi: 10.1302/0301-620X.61B2.438272. [DOI] [PubMed] [Google Scholar]
- 22.Harris GJ, Woo KI. Eosinophilic granuloma of the orbit: A paradox of aggressive destruction responsive to minimal intervention. Trans Am Ophthalmol Soc. 2003;101:93–103. [PMC free article] [PubMed] [Google Scholar]
- 23.Giona F, Caruso R, Testi AM, Moleti ML, Malagnino F, Martelli M, et al. Langerhans’ cell histiocytosis in adults: A clinical and therapeutic analysis of 11 patients from a single institution. Cancer. 1997;80:1786–91. [PubMed] [Google Scholar]
- 24.Domboski ML. Eosinophilic granuloma of bone manifesting mandibular involvement. Oral Surg Oral Med Oral Pathol. 1980;50:116–23. doi: 10.1016/0030-4220(80)90196-6. [DOI] [PubMed] [Google Scholar]
- 25.Storrs J. Bilateral eosinophilic granuloma of the mandible. Oral Surg Oral Med Oral Pathol. 1976;41:93–100. doi: 10.1016/0030-4220(76)90256-5. [DOI] [PubMed] [Google Scholar]
- 26.Postovsky S, Daitzchman M, Dale A, Ellasid R, Arush MW. Unusual presentation of mastoid eosinophilic granuloma in a young patient. Pediatr Hematol Oncol. 2001;18:283–9. doi: 10.1080/088800101750238603. [DOI] [PubMed] [Google Scholar]
- 27.Namai T, Yusa H, Yoshida H. Spontaneous remission of a solitary eosinophilic granuloma of the mandible after biopy: A case report. J Oral Maxillofac Surg. 2001;59:1485–7. doi: 10.1053/joms.2001.28290. [DOI] [PubMed] [Google Scholar]


