Abstract
It is widely recognized that sleep is important for children's health and well-being and that short sleep duration is associated with a wide range of negative health outcomes. Recently, there has been much interest in whether or not there are sufficient data to support the specific recommendations made for how much sleep children need. In this article we explore concepts related to children's sleep need, discuss the theory, rationale, and empirical evidence for contemporary sleep recommendations, and outline future research directions for sleep recommendations. If sleep is to be treated as a therapeutic intervention, then consensus guidelines, statements, and evidence-based best-practice documents are needed to underpin sleep recommendations for children.
Citation:
Matricciani L; Blunden S; Rigney G; Williams MT; Olds TS. Children's sleep needs: is there sufficient evidence to recommend optimal sleep for children? SLEEP 2013;36(4):527-534.
Keywords: Adolescents, children, need, recommendations, sleep
INTRODUCTION
Concerns that children are “in need of more sleep” and that children are “chronically sleep deprived” are contemporary concerns in our society.1–9 Such concerns, however, are not new. As our recent historical review10 reports, concerns that children are not getting enough sleep have persisted for the past century, with sleep recommendations consistently exceeding actual sleep time by approximately 37 min, due to declines in both actual and recommended sleep over time. It seems that children have always “needed” extra sleep, no matter how much sleep they were actually getting. Our review raised the issue of whether or not there was sufficient high level, low risk of bias data to support specific sleep recommendations and attracted the interest of various paediatric sleep experts11–13 and institutions.14
Sleep is undoubtedly important for the health and well-being of children. Prospective and cross-sectional studies show that short sleep duration is associated with a wide range of negative physical, social, emotional, and cognitive outcomes including poor concentration,15,16 impaired academic achievement,15,17,18 an increased risk of obesity,19,20 depression,21 suicide ideation, and injuries.22–24 A number of experimental studies have also shown that negative cognitive behavioral outcomes arise when sleep is restricted but improve when sleep is extended in both children and adolescents.25–28 There is also convincing evidence that children are sleeping less than they used to. A recent meta-analysis29 covering 690,747 children from 20 different countries found that children's sleep has decreased by 0.75 min per year over the past century, with the rate of change being greatest on school days, for older children, and for boys.
Although these studies suggest sleep duration is important, none of these observations alone provides irrefutable evidence that children need a specific amount of sleep (e.g., 9.5 hours or 8.5-9.5 hours a night). Although secular declines in sleep are concerning given the negative outcomes associated with short sleep, declines may perhaps suggest that children can simply “cope” with less sleep now than they did 100 years ago. If children could indeed do better with more sleep than they are currently getting, just how much more is optimal?
The aim of this article is to discuss the theory, rationale, and empirical evidence for contemporary sleep recommendations, explore the concept of “optimal sleep,” and discuss future research directions for sleep recommendations.
SLEEP RECOMMENDATIONS
Sleep recommendations for children date as far back as 189710 and play an important role in informing public policies, guidelines, interventions, and perhaps most importantly, informing parents and children of healthy sleep behaviors. Sleep recommendations are widely used in academic, clinical, and popular media contexts. Two normative cross-sectional studies30,31 have used specific sleep recommendations as a benchmark to assess whether children are getting sufficient (and therefore healthy) amounts of sleep. The results of such studies have led to concerns that children are sleep deprived and that public health interventions are needed.7,32,33 Some of the interventions that have been proposed to ensure adequate sleep among children and adolescents include delaying school start times and implementing education programs in schools regarding the importance of sleep. If sleep recommendations are to help us interpret normative sleep values and drive public policies and interventions, sleep recommendations must be informed by a comprehensive review of evidence and based on the best available evidence.
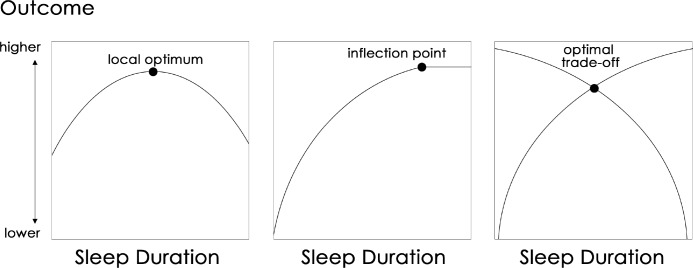
Currently there are several competing sets of sleep guidelines, which can recommend widely divergent sleep durations (Table 1). Among school-aged children, for example, recommendations can differ by as much as 1.75 hours per night, equivalent to more than 1.5 standard deviations in this age group. It appears that, of these, the most commonly cited recommendations are those of the US National Sleep Foundation (NSF). However, to date, the publicly available information from all these recommending bodies does not consistently include references from which the specific sleep durations recommended were derived for children of different age groups, nor do there appear to be any details to indicate how these recommendations were developed. Of the references cited,34–38 none are able to provide strong supporting evidence for the specific hour-based sleep recommendations made for children and adolescents of different age groups. This is not to say that these sleep recommendations have not been based on research or consensus evidence, but rather the derivation or data supporting the recommendations are not provided. We have extensively searched the websites/literature for such evidence and have not been able to locate any sources of evidence and/ or consensus statements describing the process used to develop recommendations.
Table 1.
Sleep recommendations issued by contemporary recommending bodies
Turner et al.,39 in a recent review that examined how clinical practice guidelines were developed, identified 14 key elements required in the development process. These included the establishment of a multidisciplinary guideline development group, involvement of consumers, identification of clinical questions or problems, systematic searches for and appraisal of research evidence, a process for drafting recommendations, consultation with others beyond the guideline development group, and ongoing review and updating of the clinical practice guidelines. It is not clear whether these processes underpin any or all of the currently available sleep recommendations.
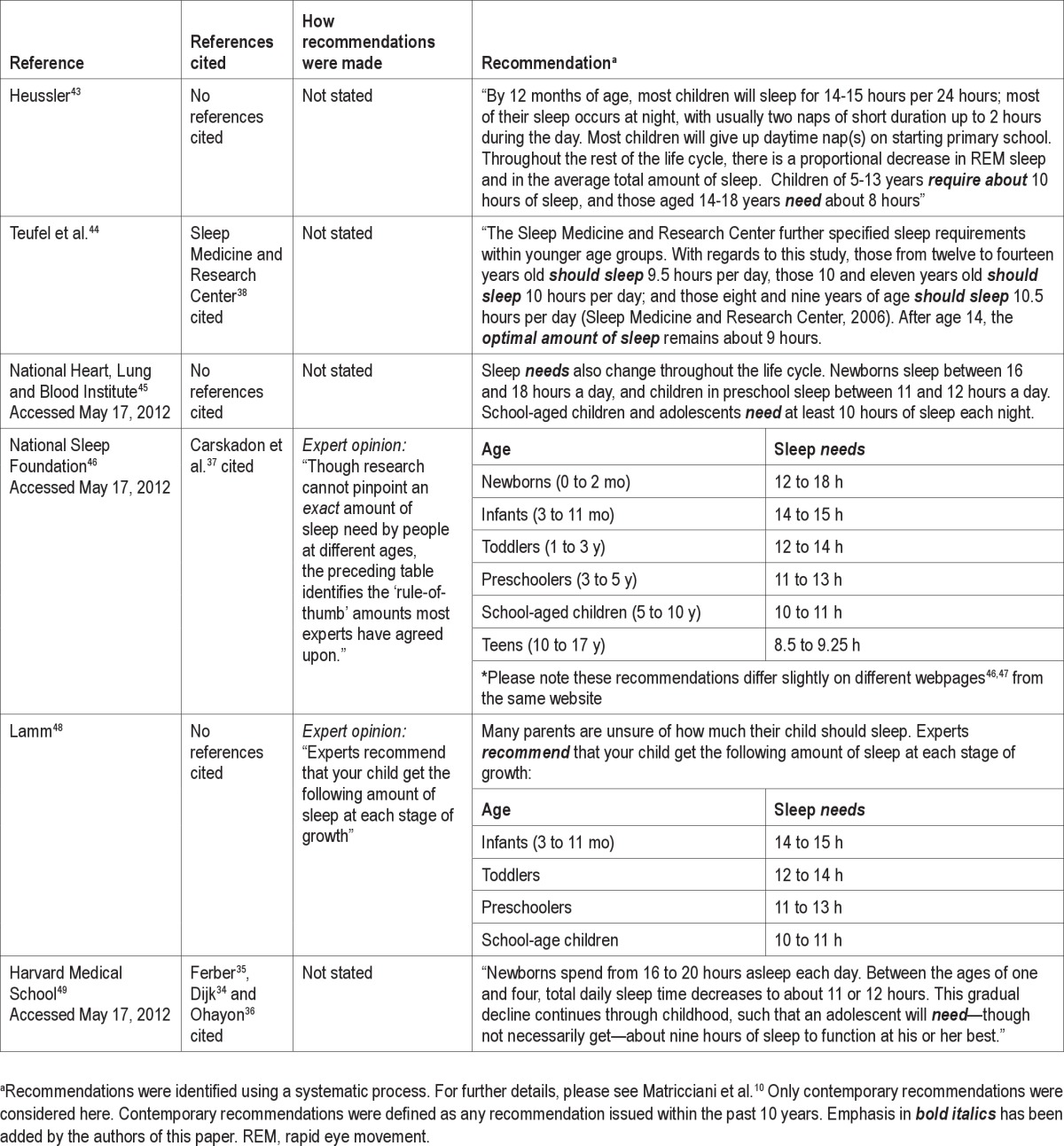
As shown in Table 1, sleep recommendations appear to have been developed by consensus of a group of experts, presumably based on a combination of research evidence and clinical experience. Although this is a good step toward informing sleep recommendations, this approach cannot ensure guidelines are based on the “best available evidence.” When considering the hierarchy of evidence for questions of intervention (Figure 1), it becomes clear that efforts to support contemporary sleep recommendations with high level, low risk of bias evidence are needed. Ideally, the next logical steps are to progress from anecdotal experience, move on from observational and quasi-experimental studies, and to conduct high level, low risk of bias studies, such as well-designed randomized controlled trials, for which few currently exist in the area of sleep needs for children. At the same time, there is also a need to review, synthesize, and appraise the existing body of evidence in an attempt to gain a better understanding of children's sleep needs and to better inform contemporary sleep recommendations.
Figure 1.
Schematic diagram of hierarchy of evidence, adapted from Jackson et al.,40 the National Collaborating Centre for Methods and Tools,41 and National Institute for Clinical Excellence.42 Although there is no universally accepted hierarchy of evidence, for questions of intervention efficacy, there is general agreement that experimental randomized controlled trial research designs are stronger than quasi-experimental studies (case-control and cohort studies), which are stronger than observational studies (uncontrolled case studies and cross-sectional studies) and expert opinion and anecdotal experience. Within each of the levels of evidence, available evidence can be further ranked as ‘limited’, ‘moderate’ or ‘strong’ depending on whether or not a systematic review or meta-analysis has been conducted with studies where the risk of methodological bias is low. Key: Strong: Supporting evidence from at least one published systematic review or meta-analysis with an appropriate target population and a low risk of bias. Moderate: Supporting evidence from at least one published systematic review or meta-analysis with an appropriate target population and a moderate to high risk of bias. Low: No supporting evidence from any published systematic review or meta-analysis.
CAN WE DEFINE OPTIMAL SLEEP?
Sleep recommendations aim to reflect children's “sleep need” or “optimal sleep” duration. Although the term “optimal sleep” is widely used in the literature, it has been operationalized in a number of different ways. Ferrara and De Gennaro50 define optimal sleep as “the daily amount of sleep that allows a subject to be fully awake (i.e., not sleepy) and able to sustain normal levels of performance during the daytime” whereas Engle-Friedman et al.51 define optimal sleep as “the amount of sleep required to feel refreshed in the morning.” Other studies52,53 with impressive circularity define optimal sleep as the amount recommended by authorizing bodies. These definitions, however, may be considered inadequate. As Horne54,55 suggests, feelings of sleepiness do not necessarily indicate a need for more sleep nor does feeling refreshed immediately after awakening in the morning.
Although sleep duration is a necessary component of “optimal sleep,” we acknowledge that other factors such as sleep quality, timing, architecture, consistency, and continuity also play an important role. Indeed, it has recently been shown that sleep timing may be even more important than sleep duration in predicting children's physical activity and body mass status.56 Nevertheless, sleep recommendations are issued to help guide optimal sleep on the basis of duration.
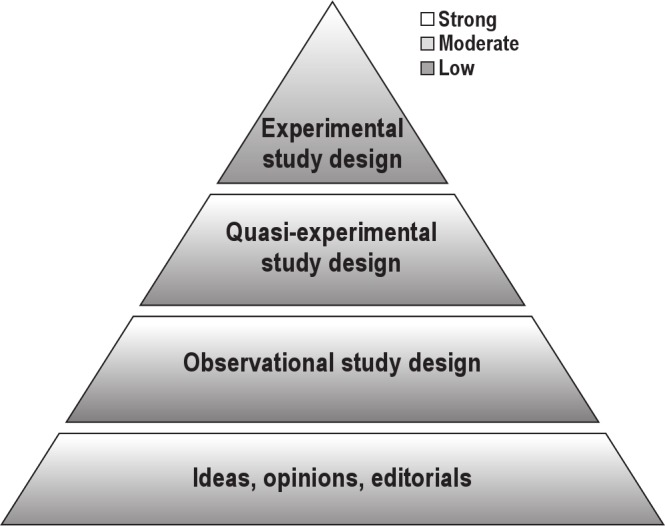
We conceptualize “optimal sleep” as the amount of sleep required to optimize some desirable outcome, such as academic performance, or aspects of mental or physical health. The notion of optimal sleep therefore reflects dose-response relationships. If there is an optimal amount of sleep, and sleep recommendations capture this optimum, then dose-response relationships should show an inverted U pattern, with a peak (the optimal outcome) close to the recommended sleep durations, or at least will have a clear deflection point showing a zone of diminished returns. Alternatively, dose-response relationships may show monotonically increasing benefits for one outcome coupled with monotonically increasing deficits for another, so that the recommendation represents an optimal tradeoff. It is inconceivable that recommendations should be issued for an optimal drug dosage, for example, without such consideration of dose-response relationships (Figure 2).
Figure 2.
Models of dose-response curves from which an optimal dosage can be determined. The left panel shows an inverted U pattern, where there is a clear local optimum. The middle panel shows a deflection point beyond which there is no further gain. The right panel shows two outcomes with opposite dose-response relationships, so that the optimum is a tradeoff.
WHAT KINDS OF STUDIES COULD INFORM CHILDREN'S SLEEP NEED?
There are four main ways in which we could gain insight into children's sleep needs and in turn, sleep recommendations. The simplest is to see how much children are sleeping, observe that they are sleepy or report wanting more sleep or feeling sleepy, and add on “a bit” of extra sleep time. This appears to have been the method adopted for most of the 20th century. However, this method is problematic because we are unable to determine whether the extra sleep recommended will produce any improvements, or if so, exactly how much extra sleep will produce optimal results. Furthermore, because sleep is an appetitive behavior, wanting more sleep and/or feeling sleepy may not necessarily indicate a need for more sleep54,57 but may indicate a choice for more sleep. This method is analogous to seeing how much children eat, observing that they often say they are hungry, and deciding that they need to eat “a bit more.”
A second method is to use unconstrained sleeping, that is, letting healthy children sleep for as long as they feel necessary, and assuming that this represents optimal sleep. The seminal study of this kind was conducted by Carskadon et al.,37,58 and is the most often cited source of evidence for sleep recommendations in North America. This longitudinal study consisted of a small sample (n = 19) of North American children initially age 10-12 years who enrolled to take part in the study in the 1970s. These children stayed at the Stanford University sleep camp for three days each year for 5-6 years, during which time their sleep was monitored. The investigators on this study reported that when adolescents were allowed to control the amount of sleep they obtained between 10:00 and 08:00, all children slept approximately 9 hours, regardless of their age. During the 1970s this innovative study was a large and singlehanded move toward understanding children's sleep needs; however, the very small and selective nature of the sample, its cultural homogeneity, the 35 years that have elapsed between that study and currently, and the ecologically abnormal context of the summer camp limits the inferences that can be drawn from this study. Furthermore, the study design does not allow inferences to be made concerning sleep duration and health outcomes; that is, would these children have performed better (or worse) with less or more sleep than they chose. Given these considerations, perhaps the least plausible conclusion from this study is that optimal sleep does not change with age among adolescents.
A third method is to examine cross-sectional data and derive dose-response relationships (Figure 2). Like all cross-sectional studies, we cannot infer causation, but such data are at least suggestive and may be the best available evidence currently. This approach has most commonly been used in relation to the link between sleep and obesity in children and adolescents. To our knowledge, with a single exception,59 none of the studies investigating associations between sleep duration and health outcomes finds an inverted U relationship, a clear deflection point, or concurrently increasing benefits and deficits. The risk of being overweight or obese, for example, consistently decreases as sleep duration increases. In some cases, the highest sleep category is equivalent to or less than the recommended duration.60,61 In those studies where the highest sleep category is greater than recommended, optimal sleep in relation to minimizing obesity risk is greater than recommended.62–66
A more recent study59 explored the relationship between sleep and student performance for children age 10-19 years, with a focus on estimating the optimal hours of sleep to maximize test score performance on a select group of neurocognitive measures. Using the Panel Study of Income Dynamics dataset, this study did in fact find an inverted U relationship between sleep duration and standardized academic test scores, with optimal hours of sleep for the optimal test performance on those selected tests being approximately 1 hour less than the recommended 9.25 hours and decreasing with age. Interestingly, and in contrast to the studies by Carskadon et al.,37,58 this study found that optimal sleep decreased with age.
The fourth method that could determine children's sleep needs is sleep extension/restriction interventions that monitor relevant outcome variables. The changes in outcomes can be plotted against the various titrations of sleep to generate dose-response relationships. This is a solid and appropriate methodology, but such studies are relatively rare in children in ecologically valid contexts.
Unfortunately, most studies using this methodology have only considered two sleep durations, so an optimum cannot be determined.26–28,67–70 The available studies have used very small, mainly North American samples, and have examined a small range of acute outcome variables, typically neurobehavioral functioning. In most cases, sleep has been restricted to levels far below the NSF recommendations (Figure 3). These studies are fairly consistent in finding only modest deficits in neurobehavioral function, motor performance, and mood, even with very large sleep restrictions (mean effect size typically < 0.2). More critically, only one finds optimal performance to coincide with the most commonly cited recommendations, those of the NSF (Figure 3). The only study reporting on three sleep durations25 failed to find a local optimum. Although these studies do suggest that children will do somewhat better with more sleep, they do not provide confirmation of the specific NSF sleep guidelines.
Figure 3.
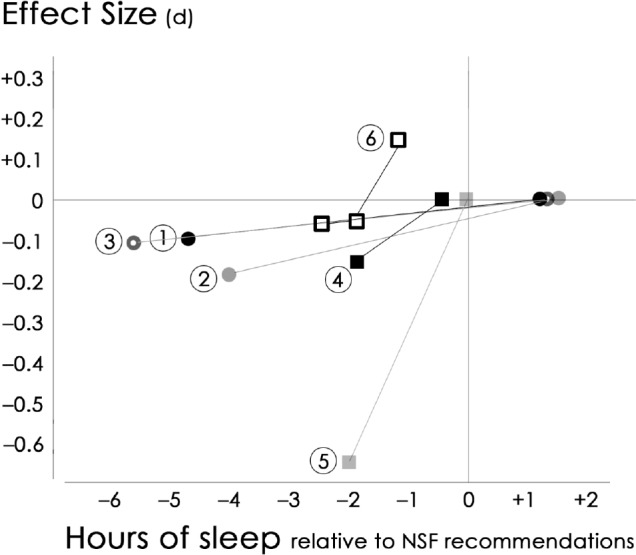
Mean effect size changes (relative to best performance) after sleep restriction/extension in six studies. The horizontal axis shows the hours of sleep relative to National Sleep Foundation (NSF) recommendations; the vertical axis shows the mean effect size difference in outcomes. 1, Carskadon et al., 198167; 2, Randazzo et al., 199826; 3, Fallone et al., 200127; 4, Gruber et al., 201168; 5, Berger et al., 201169; 6, Sadeh et al., 2003.25
CURRENT EVIDENCE BASE FOR SLEEP RECOMMENDATIONS
Although there are a number of ways in which we could gain insight into how much sleep children need, there are no studies, to our knowledge, that currently exist that directly align with contemporary sleep recommendations for children. Although sleep extension/restriction studies and dose-response relationships established from cross-sectional studies exist, the results of these studies do not provide a consistent evidence base for any of the specific hour-based sleep recommendations issued. Indeed, the results of these studies either fail to show an ‘optimum’ or else indicate an optimum that differs from values recommended.
Furthermore, as noted in our recent historical review,10 the publicly available information provided by recommending bodies does not report the basis or the consensus process from which the guidelines are derived to support each of the recommendations made for children of different ages. It has been argued that “current sleep recommendations are founded on solid science and decades of observation and research”71 and that “current expert recommendations for the sleep needs of children may not be perfect or immutable, but they are based on sound and rigorous science”71 but despite these assertions, several authors have recognized that the ideal sleep duration still remains unknown.46,53,72 Although these explanations may well be true, the difficulty remains for anyone outside the recommending body (general public, clinicians, researchers, etc.) to know which research is included or excluded and the consensus process by which the recommendations are derived.
Our conception of optimal sleep raises a number of questions. The first is whether there is a generalized optimum, or whether there are different optima for different outcomes. The second relates to interindividual variability, which can be so great that generalized recommendations may not be of much practical use. The third relates to intraindividual variability; that is, whether behavioral adaptations and environmental contexts can alter sleep requirements. If adaptability is high, then any given child (or adult) may cope equally well with a wide range of habitual sleep durations.
Generalized Optimum Versus Different Optima for Different Outcomes
Current sleep recommendations tend to suggest a “generalized optimum” exists. That is, a certain amount of sleep will optimize all physical, cognitive, and behavioral outcomes. However, it is possible that different optima exist for different health outcomes. With physical activity, for example, there is evidence that dose-response curves differ according to the outcome, such as psychologic versus physical health,73 and indeed according to the nature of the activity.74,75 Similarly, Eide and Showalter's data59 suggest that different cognitive tasks require different optimal sleep needs. It may indeed be that optimal sleep durations are different for different physical, cognitive, and behavioral outcomes.
Alternatively, it may be that different sleep durations and patterns are associated with differences in sleep architecture, which in turn influence various physical, cognitive, and behavioral outcomes differently. Accordingly, further polysomnography studies are also needed to better understand how sleep duration and timing influence sleep architecture and whether sleep architecture is associated with different physical, cognitive and behavioural outcomes.
Interindividual Variability
Alongside most sleep recommendations is a statement suggesting that “sleep needs may vary among children.”45,46 The standard deviation for school day sleep is approximately 60 minutes, and approximately 90 minutes for weekend sleep.76 It is possible that we will see similar variability in optimal sleep.
Interestingly, children from different parts of the world have radically different habitual sleep durations. At any given age, children from Asia sleep 60-120 minutes less each day than children from Europe, and 40-60 minutes less each day than children from the United States76 (Figure 4). Either there are genetic differences in sleep needs, or sleep needs can be modified by sociocultural context, or Asian children are catastrophically sleep deprived. Interestingly, when self-reported sleep needs are compared, children from Asian countries not only sleep less than children other countries, but also report needing less sleep.77–81 This brings into question the idea of a generalized biological optimum. Further research is needed to better understand the biological and nonbiological factors contributing to differences in sleep duration across demographic groups.
Figure 4.
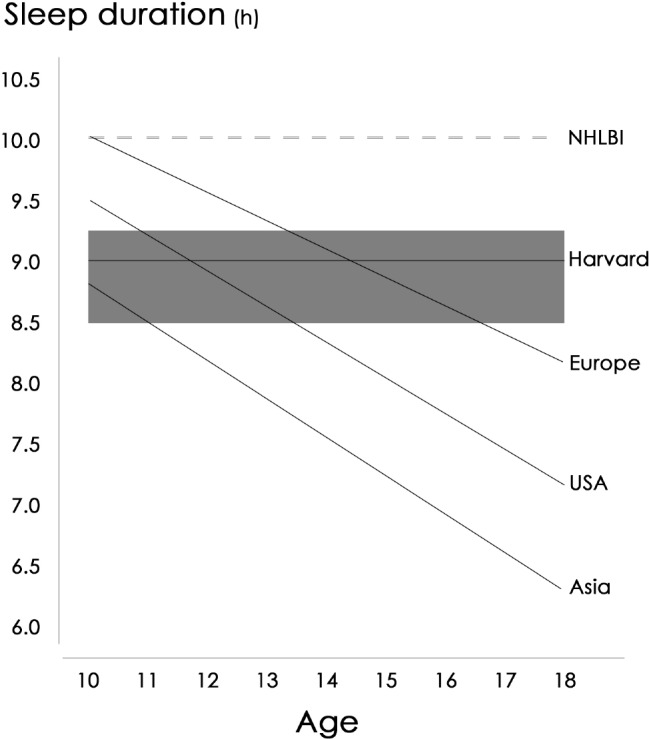
Mean sleep durations in adolescents age 9-18 y in Europe (Belgium, Finland, France, Germany, Hungary, the Netherlands, Norway, Spain, Sweden, Switzerland, the United Kingdom), the United States and Asia (China, India, Japan, Korea) (from Olds et al.76). The solid horizontal line and gray area represent the National Sleep Foundation (NSF) guidelines,46,47 the dotted line the National Heart, Lung and Blood Institute (NHLBI) guidelines,45 and the straight horizontal line represents guidelines from Harvard.49 As shown, the NSF,46,47 which cites the study by Carskadon et al.,37 recommend children age 9-18 y get 8.5-9.25 h of sleep; the NHLBI,45 which does not provide any references, recommend 10 h of sleep; and Harvard,49 who cite Ferber,35 Dijk et al.,34 and Ohayon et al.,36 recommends 9 h of sleep.
Intraindividual Variability
It is also possible, though rarely stated, that there may be intraindividual variability, depending, for example, on the amount of physical activity in which the child has participated, or the timing of growth and maturation. Can behavioral adaptations, such as diet, physical activity, external stimuli, and sleep patterns, alter sleep requirements? To answer this question, studies are needed to quantify the change in sleep duration associated with various increments and decrements of potentially modifying factors of sleep (e.g., light exposure and physical activity). Such studies would assist the interpretation of sleep restriction studies conducted in an ecologically valid setting.
CONCLUSION
As van Vugt82 explains, “people worry whether they get sufficient sleep, especially if they sleep less than the magic number,” and although recommending bodies45,46 do acknowledge that there is in fact no so-called magic number and that sleep needs may vary from person to person, a number is nevertheless provided. We conclude that there is currently insufficient high level, low risk of bias data to support specific sleep recommendations for children. Current sleep recommendations appear to be based largely on expert opinion and there do not appear to be any publicly available consensus statements outlining how recommendations were formulated or any strong sources of evidence that align with contemporary recommendations.
If sleep is to be treated as a therapeutic intervention, then consensus guidelines, statements, and evidence-based best-practice documents are needed to underpin sleep recommendations for children. In no other therapeutic arena would health professionals be content to adopt recommendations where the information from which the recommendations are derived is not explicit or provided in an easily accessed format.
This article, which explores concepts concerning children's sleep need, discusses the theory, rationale, and empirical evidence for contemporary sleep recommendations that will hopefully drive future research. There are many challenges associated with conducting studies that aim to determine children's sleep needs and there is universally good will and altruism to gain a greater understanding of children's sleep needs. Further efforts that build on past research are now needed for recommendations to be reconsidered and reevaluated. Ideally, the next steps to ensure sleep recommendations are evidence-based will involve a rigorous guideline development process with experts in the field and a comprehensive systematic review of the evidence with the aim of developing a consensus paper outlining the current best available evidence.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
Footnotes
A commentary on this article appears in this issue on page 461.
REFERENCES
- 1.Kotagal S, Pianosi P. Sleep disorders in children and adolescents. Br Med J. 2006;332:828–32. doi: 10.1136/bmj.332.7545.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loessl B, Valerius G, Kopasz M, Hornyak M, Riemann D, Voderholzer U. Are adolescents chronically sleep-deprived? An investigation of sleep habits of adolescents in the Southwest of Germany. Child Care Health Devel. 2008;34:549–56. doi: 10.1111/j.1365-2214.2008.00845.x. [DOI] [PubMed] [Google Scholar]
- 3.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91:881–4. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carskadon M. Patterns of sleepiness in adolescents. Paediatrician. 1990;17:5–12. [PubMed] [Google Scholar]
- 5.Fredriksen K, Rhodes J, Reddy R, Way N. Sleepless in Chicago: tracking the effects of adolescent sleep loss during the middle school years. Child Devel. 2004;75:84–95. doi: 10.1111/j.1467-8624.2004.00655.x. [DOI] [PubMed] [Google Scholar]
- 6.Spilsbury J, Drotar D, Rosen C, Redline S. The Cleveland Adolescent Sleepiness Questionnaire: a new measure to assess excessive daytime sleepiness in adolescents. J Clin Sleep Med. 2007;3:603–12. [PMC free article] [PubMed] [Google Scholar]
- 7.Walsh J, Dement W, Dinge D. Sleep medicine, public policy, and public health. In: Kryger M, Roth T, Dement W, editors. Principles and practice of sleep medicine. Philadelphia: Elsevier; 2005. pp. 648–56. [Google Scholar]
- 8.Yu Y, Lu B, Wang B, et al. Short sleep duration and adiposity in Chinese adolescents. Sleep. 2007;30:1688–97. doi: 10.1093/sleep/30.12.1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Honda M, Genba M, Kawakami J, Nishizono-Maher A. A sleep and lifestyle survey of Japanese high school boys: factors associated with frequent exposure to bright nocturnal light. Sleep Biol Rhythms. 2008;6:110–19. [Google Scholar]
- 10.Matricciani L, Olds T, Blunden S, Rigney G, Williams M. Never enough sleep: a brief history of sleep recommendations for children. Pediatrics. 2012;129:548–56. doi: 10.1542/peds.2011-2039. [DOI] [PubMed] [Google Scholar]
- 11.Owens J, Wise M, Akanli L, et al. A letter to the editor in defense of sleep recommendations. Pediatrics. 2012;129:987–8. doi: 10.1542/peds.2012-0755A. [DOI] [PubMed] [Google Scholar]
- 12.Feinberg I, Campbell I. Sleep recommendations for children: a need for more data. Pediatrics. 2012;129:989. doi: 10.1542/peds.2012-0755C. [DOI] [PubMed] [Google Scholar]
- 13.Buckhalt J. Sleep recommendations. Pediatrics. 2012;129:991. doi: 10.1542/peds.2012-0755E. [DOI] [PubMed] [Google Scholar]
- 14.AAP Executive Committee. AAP Executive Committee Response. Pediatrics. 2012 [Google Scholar]
- 15.Wolfson A, Carskadon M. Sleep schedules and daytime functioning in adolescents. Child Devel. 1998;69:875–87. [PubMed] [Google Scholar]
- 16.Steenari M, Vuontela V, Paavonen J, Carlson S, Fjällberg M, Aronen E. Working memory and sleep in 6-to 13-year-old schoolchildren. J Am Acad Child Adolesc Psychiatry. 2003;42:85–92. doi: 10.1097/00004583-200301000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Gruber R, Laviolette R, Deluca P, Monson E, Cornish K, Carrier J. Short sleep duration is associated with poor performance on IQ measures in healthy school-age children. Sleep Med. 2010;11:289–94. doi: 10.1016/j.sleep.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Blunden S, Chervin R. Sleep problems are associated with poor outcomes in remedial teaching programs. J Paediatr Child Health. 2007;44:237–42. doi: 10.1111/j.1440-1754.2007.01237.x. [DOI] [PubMed] [Google Scholar]
- 19.Cappuccio F, Taggart F, Kandala N, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel S, Hu F. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin J, Tung H, Hsieh Y, Lin F. Interactive effects of delayed bedtime and family-associated factors on depression in elementary school children. Res Devel Dis. 2011;32:2036–44. doi: 10.1016/j.ridd.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Koulouglioti C, Cole R, Kitzman H. Inadequate sleep and unintentional injuries in young children. Public Health Nursing. 2008;25:106–14. doi: 10.1111/j.1525-1446.2008.00687.x. [DOI] [PubMed] [Google Scholar]
- 23.Lam L, Yang L. Short duration of sleep and unintentional injuries among adolescents in China. Am J Epidemiol. 2007;166:1053–8. doi: 10.1093/aje/kwm175. [DOI] [PubMed] [Google Scholar]
- 24.Li Y, Jin H, Owens J, Hu C. The association between sleep and injury among school-aged children in rural China: a case-control study. Sleep Med. 2008;9:142–8. doi: 10.1016/j.sleep.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 25.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Devel. 2003;74:444–55. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 26.Randazzo A, Muehlbach M, Schweitzer P, Walsh J. Cognitive function following acute sleep restriction in children ages 10-14. Sleep. 1998;21:861–8. [PubMed] [Google Scholar]
- 27.Fallone G, Acebo C, Arnedt T, Carskadon M, Seifer R. Effects of acute sleep restriction on behavior, sustained attention, and response inhibition in children. Percept Mot Skills. 2001;93:213–29. doi: 10.2466/pms.2001.93.1.213. [DOI] [PubMed] [Google Scholar]
- 28.Beebe D, Rose D, Amin R. Attention, learning, and arousal of experimentally sleep-restricted adolescents in a simulated classroom. J Adolesc Health. 2010;47:523–5. doi: 10.1016/j.jadohealth.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matricciani L, Olds T, Petkov J. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. 2012;16:203–11. doi: 10.1016/j.smrv.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Spilsbury J, Storfer-Isser A, Drotar D, et al. Sleep behavior in an urban US sample of school-aged children. Arch Pediatr Adolesc Med. 2004;158:988–94. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- 31.Dorofaeff T, Denny S. Sleep and adolescence. Do New Zealand teenagers get enough? J Paediatr Child Health. 2006;42:515–20. doi: 10.1111/j.1440-1754.2006.00914.x. [DOI] [PubMed] [Google Scholar]
- 32.Chung K, Cheung M. Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep. 2008;31:185–94. doi: 10.1093/sleep/31.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holden C. Wake-up call for sleep research. Science. 1998;259:305. doi: 10.1126/science.8420000. [DOI] [PubMed] [Google Scholar]
- 34.Dijk D, Duffy J, Czeisler C. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiol Int. 2000;17:285–311. doi: 10.1081/cbi-100101049. [DOI] [PubMed] [Google Scholar]
- 35.Ferber R. Sleep, sleeplessness, and sleep disruptions in infants and young children. Ann Clin Res. 1985;17:227–34. [PubMed] [Google Scholar]
- 36.Ohayon M, Carskadon M, Guilleminault C, Vitiello M. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 37.Carskadon M, Harvey K, Duke P, Anders T, Litt I, Dement W. Pubertal changes in daytime sleepiness. Sleep. 1980;2:453–60. doi: 10.1093/sleep/2.4.453. [DOI] [PubMed] [Google Scholar]
- 38.Sleep Medicine and Research Center. Sleep requirements. [Accessed April 3, 2006]. Available at http://www.stjohnsmercy.org/services/sleepmedicine/
- 39.Turner T, Misso M, Harris C, Green S. Development of evidence-based clinical practice guidelines (CPGs): comparing approaches. Implement Sci. 2008;3:1–8. doi: 10.1186/1748-5908-3-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jackson S, Fazal N, Giesbrecht N. A hierarchy of evidence: which intervention has the strongest evidence of effectiveness? [Accessed June 1, 2012]. Available at: http://cbpp-pcpe.phac-aspc.gc.ca/pubs/hierachy_of_evidence.pdfaccessed.
- 41.Ciliska D, Thomas H, Buffet C. ‘An introduction to evidence-based public health and a compendium of critical appraisal tools for public health practice’ from National Collaborating Centre for Methods and Tools (NCCMT) 2008. [Accessed May 31, 2012]. Available at http://www.nccmt.ca/pubs/2008_07_IntroEIPH_compendiumENG.pdf.
- 42.Weightman A, Ellis S, Cullum A, Sander L, Turley R. Grading evidence and recommendations for public health interventions: developing and piloting a framework. 2005. [Accessed May 31, 2012]. Available at: http://www.nice.org.uk/niceMedia/docs/grading_evidence.pdf.
- 43.Heussler H. Common causes of sleep disruption and daytime sleepiness: childhood sleep disorders II. Med J Aust. 2005;182:484–9. doi: 10.5694/j.1326-5377.2005.tb06793.x. [DOI] [PubMed] [Google Scholar]
- 44.Teufel J, Brown S, Birch D. Sleep among early adolescent students. Am J Health Studies. 2007;22:10–17. [Google Scholar]
- 45.National Heart LaBI. Your Guide to Healthy Sleep. US Department of Health and Human Services; [Accessed May 17, 2012]. Available at: www.nhlbi.nih.gov/health/public/sleep/healthy_sleep.pdf. [Google Scholar]
- 46.National Sleep Foundation [NSF] How Much Sleep Do We Really Need? [Accessed May 17, 2012]. Available at: www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need.
- 47.National Sleep Foundation [NSF] Children and Sleep. [Accessed May 17, 2012]. Available at: http://www.sleepfoundation.org/article/sleep-topics/children-and-sleep.
- 48.Lamm C. Sleep and children. American Academy of Sleep Medicine Education Committee; [Accessed May 17, 2012]. Available at: www.sleepeducation.com/Topic.aspx?id=8. [Google Scholar]
- 49.Harvard Medical School. Changes in sleep with age. [Accessed May 17, 2012]. Available at: http://healthysleep.med.harvard.edu/healthy/science/variations/changes-in-sleep-with-age.
- 50.Ferrara M, De Gennaro L. How much sleep do we need? Sleep Med Rev. 2001;5:155–79. doi: 10.1053/smrv.2000.0138. [DOI] [PubMed] [Google Scholar]
- 51.Engle-Friedman M, Palencar V, Riela S. Sleep and effort in adolescent athletes. J Child Health Care. 2010;14:131–41. doi: 10.1177/1367493510362129. [DOI] [PubMed] [Google Scholar]
- 52.Jin Q, Shi Q. A comparison of the number of hours of sleep in high school students who took advanced placement and/or college courses and those who did not. J Sch Nurs. 2008;24:417–24. doi: 10.1177/1059840508326747. [DOI] [PubMed] [Google Scholar]
- 53.Eaton D, McKnight-Eily L, Lowry R, Perry G, Presley-Cantrell L, Croft J. Prevalence of insufficient, borderline, and optimal hours of sleep among high school students - United States 2008. J Adolesc Health. 2010;46:399–401. doi: 10.1016/j.jadohealth.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 54.Horne J. Sleepfaring: a journey through the science of sleep. New York: Oxford University Press; 2007. [Google Scholar]
- 55.Horne J. Sleepiness as a need for sleep: when is enough, enough? Neurosci Biobehav Rev. 2010;34:108–18. doi: 10.1016/j.neubiorev.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 56.Olds T, Maher C, Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. 2011;34:1299–307. doi: 10.5665/SLEEP.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harrison Y, Horne J. Should we be taking more sleep? Sleep. 1995;18:901–7. [PubMed] [Google Scholar]
- 58.Carskadon M. California: Stanford University; 1979. Determinants of daytime sleepiness: adolescent development, extension and restriction of nocturnal sleep. [Google Scholar]
- 59.Eide E, Showalter M. Sleep and student achievement. East Econ J. 2012:1–13. [Google Scholar]
- 60.Seicean A, Redline S, Seicean S, et al. Association between short sleeping hours and overweight in adolescents: results from a US suburban high school survey. Sleep Breath. 2007;11:285–93. doi: 10.1007/s11325-007-0108-z. [DOI] [PubMed] [Google Scholar]
- 61.Sekine M, Yamagami T, Handa K, et al. A dose-response relationship between short sleeping hours and childhood obesity: results of the Toyama Birth Cohort Study. Child Care Health Devel. 2002;28:163–70. doi: 10.1046/j.1365-2214.2002.00260.x. [DOI] [PubMed] [Google Scholar]
- 62.Snell E, Adam E, Duncan G. Sleep and the body mass index and over-weight status of children and adolescents. Child Devel. 2007;78:309–23. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 63.von Kries R, Toschke A, Wurmser H, Sauerwald T, Koletzko B. Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep-a cross-sectional study. Int J Obesity. 2002;26:710–6. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 64.Padez C, Mourao I, Moreira P, Rosado V. Prevalence and risk factors for overweight and obesity in Portuguese children. Acta Pædiatr. 2005;94:1550–7. doi: 10.1080/08035250510042924. [DOI] [PubMed] [Google Scholar]
- 65.Reilly J, Armstrong J, Dorosty A, et al. Early life risk factors for obesity in childhood: cohort study. Br Med J. 2005;330:1357–63. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chaput J, Brunet M, Tremblay A. Relationship between short sleeping hours and childhood overweight/obesity: results from the ‘Québec en Forme’ Project. Int J Obesity. 2006;30:1080–5. doi: 10.1038/sj.ijo.0803291. [DOI] [PubMed] [Google Scholar]
- 67.Carskadon M, Harvey K, Dement W. Acute restriction of nocturnal sleep in children. Percept Mot Skills. 1981;53:103–12. [Google Scholar]
- 68.Gruber R, Wiebe S, Montecalvo L, Brunetti B, Amsel R, Carrier J. Impact of sleep restriction on neurobehavioral functioning of children with attention deficit hyperactivity disorder. Sleep. 2011;34:315–23. doi: 10.1093/sleep/34.3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Berger R, Miller A, Seifer R, Cares S, Lebourgeois M. Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. J Sleep Res. 2012;21:235–46. doi: 10.1111/j.1365-2869.2011.00962.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Copes J, Rosentzweig K. The effects of sleep deprivation upon motor performance of ninth-grade students. J Sports Med. 1972;12:47–56. [PubMed] [Google Scholar]
- 71.Carskadon M, Owens J. Sleep guidance for kids and teens is based on sound science. Huffpost. 2012 [Google Scholar]
- 72.Lumeng J. Future directions for research on sleep durations in pediatric populations. Sleep. 2010;33:1281–2. doi: 10.1093/sleep/33.10.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Oja P. Dose response between total volume of physical activity and health and fitness. MedSci Sports Exerc. 2001;33:s428–37. doi: 10.1097/00005768-200106001-00011. [DOI] [PubMed] [Google Scholar]
- 74.Harvey S, Hotopf M, Øverland S, Mykletun A. Physical activity and common mental disorders. Br J Psychiatry. 2010;197:357–64. doi: 10.1192/bjp.bp.109.075176. [DOI] [PubMed] [Google Scholar]
- 75.Cerin E, Leslie E, Sugiyama T, Owen N. Associations of multiple physical activity domains with mental well-being. J Ment Health Phys Act. 2009;2:55–64. [Google Scholar]
- 76.Olds T, Blunden S, Forchino F, Petkov J. The relationships between sex, age, geography and time in bed in adolescents: a meta-analysis of data from 23 countries. Sleep Med Rev. 2010;14:371–8. doi: 10.1016/j.smrv.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 77.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–9. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 78.Yang C, Kim J, Patel S, Lee J. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics. 2005;115:250–6. doi: 10.1542/peds.2004-0815G. [DOI] [PubMed] [Google Scholar]
- 79.Takemura T, Funaki K, Kanbayashi T, et al. Sleep habits of students attending elementary schools, and junior and senior high schools in Akita prefecture. Psychiatry Clin Neurosci. 2002;56:241–2. doi: 10.1046/j.1440-1819.2002.01013.x. [DOI] [PubMed] [Google Scholar]
- 80.Mercer P, Merritt S, Cowell J. Differences in reported sleep need among adolescents. J Adolesc Health. 1998;23:259–63. doi: 10.1016/s1054-139x(98)00037-8. [DOI] [PubMed] [Google Scholar]
- 81.Tonetti L, Fabbri M, Natale V. Sex differences in sleep-time preference, and sleep need: a cross-sectional survey among Italian pre-adolescents adolescents, and adults. Chronobiol Int. 2008;25:745–59. doi: 10.1080/07420520802394191. [DOI] [PubMed] [Google Scholar]
- 82.van Vugt H. Sleep in context. In: Westerink J, Ouwerkerk M, Krans M, editors. Sensing emotions: the impact of context on experience measurements. New York: Springer; 2011. [Google Scholar]