Abstract
Background:
Blood pressure (BP) recording is the most commonly measured clinical parameter. Standing mercury sphygmomanometer is the most widely used equipment to record this. However, recording by sphygmomanometer is subject to observer and instrumental error. The different sources of equipment error are faulty manometer tube calibration, baseline deviations and improper arm bladder cuff dimensions. This is further compounded by a high prevalence of arm bladder miss-cuffing in the target population.
Objectives:
The study was designed to assess the presence of equipment malcalibrations, cuff miss-matching and their effect on BP recording.
Materials and Methods:
A cross-sectional check of all operational sphygmomanometers in a health university was carried out for the length of the manometer tube, deviation of resting mercury column from “0” level, the width and length of arm bladder cuff and extent of bladder cuff-mismatch with respect to outpatient attending population.
Results:
From the total of 50 apparatus selected, 39 (78%) were from hospital setups and 11 (22%) from pre-clinical departments. A manometer height deficit of 13 mm was recorded in 36 (92.23%) of the equipment in hospital and 11 (100%) from pre-clinical departments. Instruments from both settings showed significant deviation from recommended dimensions in cuff bladder length, width and length to width ratio (P < 0.001). Significant number of apparatus from hospital setups showed presence of mercury manometer baseline deviation either below or above 0 mmHg at the resting state (χ2 = 5.61, D. F. = 1, P = 0.02). Positive corelationship was observed between manometer height deficit, baseline deviation and width of arm cuff bladder (Pearson correlation, P < 0.05). Bladder cuff mismatching in response to the target population was found at 48.52% for males and 36.76% for females. The cumulative effect of these factors can lead to an error in the range of 10-12 mmHg.
Conclusion:
Faulty equipments and prevalent arm bladder cuff-mismatching can be important barriers to accurate BP measurement.
Keywords: Blood pressure, instrument error, miss-cuffing
Introduction
Hypertension is a frequent condition seen in clinical practice. The prevalence of hypertension is on an up spiral at a global level. One in every fourth adult has hypertension in India,(1,2) Pooling of epidemiologic studies shows that it is present in 25% of the urban and 10% of the rural Indian subjects.(3) The consequences of hypertension are numerous and involve multiple organ systems. Medical treatment when required is usually life long.
Levelling an individual hypertensive requires accurate recording of his blood pressure (BP). The most commonly used technique to measure BP in routine conditions is by indirect measurement. The equipment used universally for this purpose is a mercury gravity sphygmomanometer and a stethoscope. The sphygmomanometer comprises a manometer (mercury or aneroid) tube with a calibrated scale for measuring pressure, a mercury reservoir with valve and an inflation system. The latter consists of an inflatable bladder encased in a non-distensible cuff that can be securely wrapped around the limb, an inflation bulb for manual inflation of the bladder in the cuff and tubing connecting both the manometer and the inflation bulb to the bladder. This complexity of the equipment opens the gate for error. When less than ideal quality control relating to equipment selection, calibration, repair and production of component is observed, this fairly reliable machine can produce alarming fallacious results.
Surveys from health care settings demonstrate that 18% to more than 50% of mercury sphygmomanometers record maintenance defects, including resting manometer tube baseline deviation, which accounts for BP deviation in the range of 5-12 mmHg.(4) Employing an arm bladder cuff whose dimensions are less than the minimum recommended 1:1.8 for width to length can lead to overestimation of BP by 7 mm systolic and 4.3 mm diastolic.(5) Deviation from the recommended arm cuff size of 40% (0.4) in reference to the arm circumference is another common source of equipment error. Use of bladder cuff with cuff width:arm circumference (CW: AC) in the range of 0.34 and 0.5 can either overestimate or underestimate the BP recording by another 5 mmHg. For the same degree of mismatch, the error is greater when the cuff width is narrower rather than larger.(6) These equipment fallacies put tighter can contribute to inappropriate estimation of BP by over 20 mm systolic and 10 mm diastolic.
These observations prompted us to carry out a hospital-based point prevalence survey for the mentioned parameters in an Indian set-up in lieu of paucity of such studies.
Research question
How frequent are the issues of malcalibration and miss-cuffing in a tertiary health care organization and what is its impact on BP recording?
Hypothesis
The interplay of factors like malcalibration and miss-cuffing may act as a significant barrier to accurate BP recording.
Objectives
To measure the deficit in height of mercury manometer tubes from the proclaimed 300 mm marking and associate it with BP recording variation.
To study the presence of baseline deviation of resting sphygmomanometer tubes in routine use and try to associate its impact on BP recording.
To study the bladder cuff length, width and length to width ratio and its deviation from the recommended standard.
To study the appropriateness of bladder cuffs in use with reference to population need and estimate prevalence of miss-cuffing.
To evaluate the interrelationships of these variables with each other and predict their combined impact on BP recording.
Materials and Methods
Place of study
This cross-sectional study was carried out in a rural health university situated in the state of Maharashtra in India, catering to a rural and semi-urban population in excess of 5, 00,000 from three adjourning districts, namely Ahmednagar, Nasik and Aurangabad. This university has six constituent institutes like a medical college with specialty and superspeciality facilities, a dental college, a nursing college, a physiotherapy college, a center for biotechnology and a center for social medicine with undergraduate and post-graduate teaching training activities. The areas selected for the study purpose were the medical and dental college hospital out patient departments (OPD), wards, casualty and basic science departments.
Sample size
Fifty functioning manual sphygmomanometers were selected for the study purpose.
Inclusion criteria
Sphygmomanometers in regular use in the hospital wards, outpatient departments (both medical and dental), casualty and medical college basic science departments were selected.
Exclusion criteria
Broken instruments, instruments with any gross defect and those with leaking valves and other defect were left out.
Equipments used to record study parameters
Digital vernier caliper (Aerospace) with a resolution of 0.01 mm.
Standardized measuring tape with accuracy up to 0.1 cm.
Measuring scale with accuracy up to 1 mm.
Parameters measured
The height of the calibration on the manometer tube and baseline deviation of the mercury column from the 0 mm level at resting state when the manometer tube is in functional position (standing position) was measured with a digital caliper.
The length and width of the arm bladder cuff was measured with the help of a measuring scale, and the correctness of the recording was checked by a digital vernier caliper.
Mid-arm circumference (MAC) of OPD attending individuals was measured by a measuring tape.
The manufacturer as well as the standardization marks of each instrument were also noted.
Sampling of participants for study of arm cuff adequacy
The study universe was outpatient-attending adult patients in the age group of 13-60 years over 1 weeks time. From them, a sample of 10% sex-stratified population was selected by the systematic sampling technique. This accounted for 168 participants whose MAC of non-dominant extended and relaxed arm was measured to the nearest half centimeter using a measuring tape.
Statistical analysis
Distribution of equipment at different locations, presence of cuff mismatching and baseline deviation was expressed in percentage. Chi-square test (χ2) was used to measure the significance of difference between the mercury column height and mercury column baseline deviation, mercury column baseline deviation and location of equipments and arm cuff bladder length and width versus location of equipment. Pearson correlation, proximity similarity matrix for distances correlation, was used to estimate the corelationship between the different study variables, namely bladder length to width ratio, baseline deviation of mercury column from resting 0 mm level and manometer column height. ANOVA test was employed to establish co-relationships of study variables and limit confounding. A P value of < 0.05 was taken up to establish significance. Coded data was analyzed by SPSS 11.
Results
The distribution of the studied equipments showed that 20 (40%) were from the outpatient department, 17 (34%) from the clinical wards, 11 (22%) from pre-clinical departments and two (4%) from the casualty.
The markings on the manometer tubes were from 0 mm to 300 mm. But, on actual measurement, the readings were found to be deficient. In the hospital setting, 36 (92.23%) and in the medical college setting, 11 (100%) of the instruments recorded a tube length of 287 mm. None of the studied equipments recorded the actual 300 mm length. The mean measurement of the calibrated manometer tube was 287.1 mm. This accounted to an actual deficit of 12.9 mm (300-287.1 mm). Arithmetic conversion to this deficit for the corresponding scales of 120 mm and 80 mm was found to be 5.12 mm and 3.44 mm, respectively. This deficit can result in overestimating BP by 5.12 mmHg systolic and of 3.44 Hg diastolic in a normotensive (BP 120/80 mmHg.) individual. The details of manometer height measurement are expressed in Figure 1.
Figure 1.
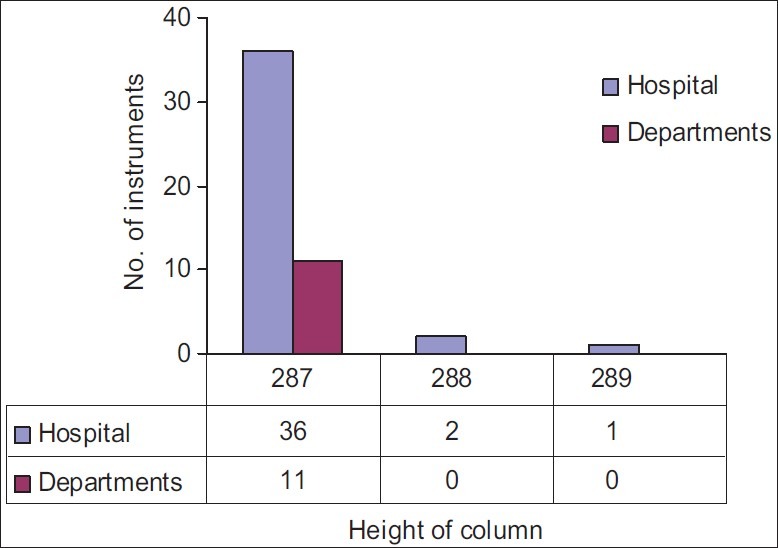
Recording of manometer height (in mm) at different study set-ups (hospital and pre-clinical department)
Baseline deviation of resting mercury column from the 0 mm Hg mark in standing position was recorded by a digital vernier caliper. Twenty (40%) of the studied equipments showed baseline deviation, of which 12 (26%) had positive and eight (16%) had negative deviation. Their corresponding mean values were 2.92 mm and-2.50 mm, respectively. The range of deviation varied from +12 mm to-5 mm, with standard error 0.32 and variance 5.13.
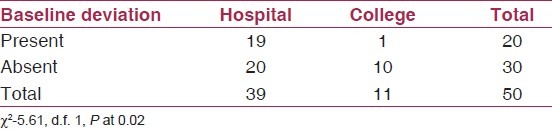
Equipments from hospital settings (OPDs, wards and casualty) and basic sciences set-ups showed significant variations. Equipments from the hospital set-up were found to have a significant baseline deviation (Chi-square (χ2) value of 5.61, for degree of freedom 1, P < 0.05). The detailed comparison of equipments from hospitals and medical college basic sciences departments is presented in Table 1.
Table 1.
Comparison of mercury column baseline deviation of the manometer tube at resting state at hospital and basic sciences (college) set-ups
In all locations except the pediatric ward, small-sized adult cuff with a recommended dimension of 220 mm × 120 mm was found to be in use. These cuffs were supposed to record the ideal bladder length to width ratio of 2:1.
In our study, the length of the bladder cuffs varied from 188 mm to 224 mm, with a mean of 216.4 mm, and width from 120 mm to 128 mm, with a mean of 124.5 mm. Bladder length/width ratio ranged from 1.5 to 1.8, with the mean at 1.7 and 95% confidence at 1.6-1.8. The descriptive statistics of major study variables are presented in Table 2.
Table 2.
Descriptive findings of major study variables
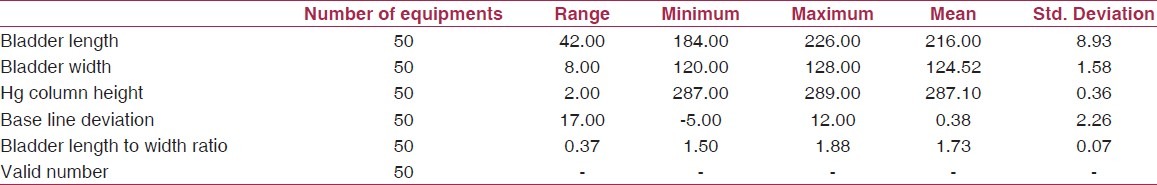
On analysis of equipments at different locations with respect to bladder length to width ratio, it was observed that in hospital OPDs, of 20 equipments studied, only four (20%) had a bladder cuff length to width ratio of the recommended value (≥1.8). The remaining 16 (80%) had a substandard ratio (<1.8). The corresponding Figures for the equipments at hospital wards were two (11.7%) and 15 (88.3%). The recording of equipments at the medical college basic sciences departmental level was even worse. There, all the equipment studied had a cuff length to width ratio <1.8.
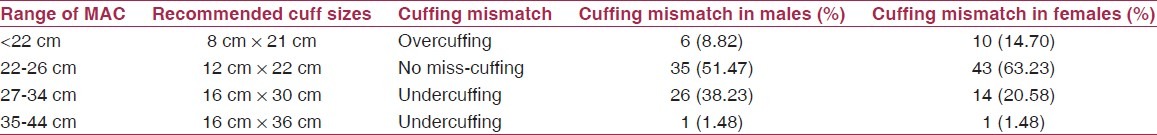
Small-sized adult cuff was the only arm cuff in use to measure BP in the adult population in the study set-up. We decided to find out the adequacy of this cuff in reference to the target population. For this purpose, the MAC of 136 randomly selected adults in the age group of 13-60 was taken. It was noticed that the cuff in routine use (adult small size, i.e. 220/120 mm) was found inadequate in 33 (48.52%) males and 25 (36.76%) females. Table 3 provides the detailed break-ups of the pilot population's MAC and the expected cuff size along with the extent of mismatching (miss-cuffing).
Table 3.
Cuff mismatch in the target population
A significant corelationship was noticed between major study variables like baseline deviation, manometer column height and cuff bladder length to width ratio (Pearson correlation, proximity similarity matrix for distances correlation). This is given in Table 4.
Table 4.
Measures of similarity between variables by Pearson correlation (distances)

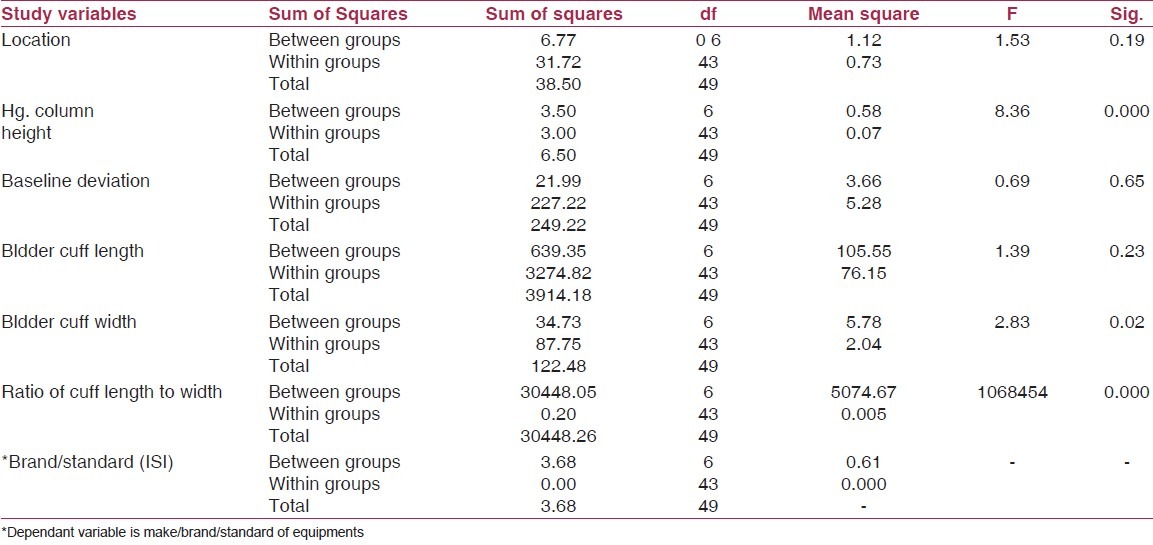
Association of study variables to each other and to that of the equipments in general were tested by the ANOVA test. It was observed that the study variables were consistently deviant irrespective of the make or brand of equipments examined. Therefore, we decided to keep the make or brand of the equipment as the dependent variable for multivariate analysis. After taking care of confounders at the analysis stage, a strong association was observed among arm cuff bladder width, deficit in Hg manometer and bladder cuff length to width ratio. These observations are reported in Table 5.
Table 5.
ANOVA test for study variable demonstrating existence of relationship between them
Discussion
The highest attainable standard of health is one of the fundamental rights of every human being.(3) This fundamental right is seriously threatened by cardiovascular diseases that are estimated to be the largest cause of death and disability in India.(7)
Blood pressure measurement is an essential screening exercise for detection of cardio vascular diseases (CVD) risks. Sphygmomanometers used for BP recording are one of the most commonly used diagnostic instruments. However, the detection of hypertension by sphygmomanometer is not free from errors. A steady error of 5 mmHg can double or halve the number of patients diagnosed with hypertension.(8) Studies suggest that an error of ≥3 mmHg can result in clinically significant under-and overdetection of hypertensive conditions.(7–10)
One of the important causes for errors in BP measurement by sphygmomanometer is malcalibrated instruments. The calibration defects can arise from deficit in the mercury manometer height, presence of baseline deviation and disproportion in the arm bladder cuff. This problem can be compounded by existence of miss-cuffing with respect to the target population.
The presence of height deficit in the calibrated mercury manometer tube is ill conceived. The recorded 12.9 mm mean deficit of our study on logical mathematical language can account for an increased BP recording of 5.12 mm systolic and 3.44 mm diastolic in a normotensive individual. This fallacy was recorded in 100% of the equipments studied.
Studies found that 18% to more than 50% of the instruments tested were exhibiting clinically significant errors, of which 10-39% recorded baseline deviation at ≥5 mmHg.(5–7) In our study, 40% of the sphygmomanometers had baseline deviation, and the mean deviation was in excess of 2.5 mmHg. Presence of baseline deviation was more prevalent in demand locations like OPDs and wards (Chi-square (χ2) value of 5.61, for degree of freedom 1, P < 0.05). This may be due to the greater wear and tear of equipments in demand locations. Therefore, the need for frequent check and standardization in these set-ups cannot be understated.
The accuracy of BP measurement is also dependant on the adequacy of the bladder cuffs. The recommended “ideal cuff” should have a bladder length that is 80% and a width that is at least 40% of the arm circumference, i.e., “Length to Width” ratio of at least 2:1.(8–10) Thus, the cuff size is required to vary with the patient profile. Manning et al. in their study demonstrated that the cuff length width ratio mismatch can lead to an increase of 8.5 mm Hg systolic and 4.6 mm Hg diastolic, with a wide individual variance.(4–8,11,12)
The cuff width to length ratio for over 80% of the equipments in our study was found to be less than 1:1.8. Any measurement by these equipments can lead to an overestimation of BP by 7 mm systolic and 4.3 mm diastolic.(5)
The use of a too-small cuff (undercuffing) on large arm incorrectly diagnose one with high blood pressure, resulting in erroneous medication.(13–15) On the other hand, someone's high blood pressure goes undiagnosed because of the use of a too-large cuff (overcuffing) on a small arm. This leads to lack of treatment, which can damage the blood vessels, resulting in stroke and heart attack.(16–18) Therefore, using the wrong cuff size (miss-cuffing) means that any readings you get are inaccurate.
The extent of miss-cuffing in our study was 36.76% for males and 48.58% for females. This observation was similar to that of Manning and Kuchirka and others, where the proper cuff size was used only in 69% of the measurements taken by the nurses and 63% by the house staff.(17–19)
Using a small cuff on a larger arm is the most common cause of error.(4–8,16) We recorded a prevalence of undercuffing of22.06% in females and 39.71% in males, which matched with that of Maxwell (Lancet, 1982), where 37% i.e. more than one-third of obese hypertensive were incorrectly diagnosed and actually had normal blood pressure, because of undercuffing.(16) Numerous other studies since then have confirmed that using a too-small cuff significantly overestimates blood pressure in “obese” people (sometimes called “Spurious Hypertension”). The extent of error due to undercuffing had shown an average error of 8.5 mm Hg systolic and 4.6 mm Hg diastolic.,(15,20) Unfortunately, in many situations, only one cuff size (small adult) is available, as was the case in our study.(20–22)
The issue of overcuffing is also equally alarming. Recent studies showed that a “standard” cuff often underestimates BP in very lean people. Thus, many skinny folks may be told that they have normal blood pressure when in fact they have hypertension.,(20,23–26) A large bladder cuff may lead to falsely low reading in the range of 10 mm to 30 mm of Hg.(6) The prevalence of overcuffing in our study was 8.82% for males and 14.70% for females. Thus, correct cuff size is an important issue for people of all sizes.
A combined presence of these factors can further complicate the issue. Such fallacies may jointly lead to error, ranging from 9 mm to 12 mm Hg for systolic and 6 mm to 8 mm Hg for diastolic BP (i.e. 4.3-5.2 for Hg column deficit, -2.3 to 3 for baseline deviation and 4.6-8.5 for bladder undercuffing).
Furthermore, the association of cuff length to width ratio to that of the baseline deviation and Hg.mercury manometer height in the present study might compound the quantum of error. The accuracy of BP recording from these apparatus then becomes highly questionable.
Conclusions
Issues relating to malcalibration and miss-cuffing and its impact on BP recording is a subject of study for over the last four decades. An unnoticed item that we hope was projected for the first time in our study is the issue of undercalibration of manometer tube. This deficit is projected to overestimate BP by 5.12 mm of Hg systolic and 3.44 mm of Hg diastolic in a normal individual. This grey area has future potential for research. Comparison of intra-arterial (direct) and auscultatory (indirect) readings demonstrates that the auscultatory method overestimated the systolic and diastolic blood pressures.(27) Future research may find an answer to this, and the mercury column height deficit may be a contributing factor in this regard.
It is essential that we choose a correct cuff size relative to the patient's arm profile. Using an inappropriate cuff can significantly distort BP readings. The miss-cuffing issue can be addressed by providing alternate cuffs at the end-user level. This may be achieved through an aggressive marketing strategy. The equipment manufacturers should pack the instrument with at least five standard cuffs, i.e., three adult sizes with dimensions of 22 cm × 12 cm, 16 cm × 30 cm and 16 cm × 36 cm and two pediatric sizes like child and neonate cuffs. There has to be increased signage in place on the arm cuff unit with respect to its dimension and locating the center. This forced marketing strategy can ensure the cuff availability to all concerned and increase their use.
We tried to limit bias by blinding the observer to the study outcome, requiting committed and competent observer and using standardized equipments.
It could have been prudent to enhance the study result by a comparative design where all factors influencing BP recording should have been discussed threadbare. The multivariate analysis effects could have been more useful if the extent of errors were linked to the cumulative effort on BP recording. Such an analysis by future researchers can add strength to our observations.
Recommendations
End users of sphygmomanometers, like practitioners and hospitals, should check for proper standardization. Equipments once commissioned for use need to be calibrated at regular intervals to prevent the occurrence of erroneous readings.
Physicians and other health care provider's myths and misconceptions relating to cuffing issues can be addressed by continuing and sustained medical education and clinical orientation training.
Most importantly, public awareness should increase so that they demand for proper and accurate instruments and correct recordings of BP. It is them who are at the receiving end anyway.
Acknowledgments
We thank the medical superintendent, the matron of the hospital and all heads of the Departments who encouraged and supported our study. Our heartfelt thanks to Dr. S. N. Jain, Professor of Microbiology because it is he who implanted the seed for this research.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Whitworth JA World Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–92. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–8. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 3.An epidemiological approach to describing risk associated with blood pressure levels. Final report of the working group on risk and high blood pressure. Hypertension. 1985;7:641–51. [PubMed] [Google Scholar]
- 4.Mion D, Pierin AM. How accurate are sphygmomanometers? J. Hum Hypertension. 1998;12:245–8. doi: 10.1038/sj.jhh.1000589. [DOI] [PubMed] [Google Scholar]
- 5.Markandu ND, Whither F, Amild A, Carney C. The mercury sphygmomanometer should be abandoned before it is prescribed. J Hum Hypertension. 2000;14:31–6. doi: 10.1038/sj.jhh.1000932. [DOI] [PubMed] [Google Scholar]
- 6.Kidney Disease Outcomes Quality Initiative (K/DOQI). K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43:S1–290. [PubMed] [Google Scholar]
- 7.Nicholas WC, Watson RL, Barnes TY, Goodnow C, Russell E. Does blood pressure cuff size make a difference in blood pressure reading? J Miss State Med Assoc. 1985;26:31–4. [PubMed] [Google Scholar]
- 8.Iyriboz Y, Hearon CM, Edwards K. Agreement between large and small cuffs in sphygmomanometry: A quantitative assessment. J Clin Monit. 1994;10:127–33. doi: 10.1007/BF02886825. [DOI] [PubMed] [Google Scholar]
- 9.Geddes LA, Whistler SJ. The error in indirect blood pressue measurement with the incorrect size cuff. Am Heart J. 1978;96:4–8. doi: 10.1016/0002-8703(78)90119-9. [DOI] [PubMed] [Google Scholar]
- 10.O’Brien E. Will mercury manometers soon be obsolete? J Hum Hypertens. 1995;9:933–4. [PubMed] [Google Scholar]
- 11.Joffres MR, Hamet P, Rabkin SW, Gelskey D, Hogan K, Fodor G. Prevalence, control and awareness of high blood pressure among Canadian adults. Canadian Heart Health Surveys Research Group. CMAJ. 1992;146:1997–2005. [PMC free article] [PubMed] [Google Scholar]
- 12.Turner MJ, Baker AB, Kam PC. Effects of systematic errors in blood pressure measurements on the diagnosis of hypertension. Blood pressure Monit. 2004;9:249–53. doi: 10.1097/00126097-200410000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Rouse A, Marshall T. The extent and implications of sphygmomanometer calibration error in primary care. J Hum Hypertens. 2001;15:587–91. doi: 10.1038/sj.jhh.1001241. [DOI] [PubMed] [Google Scholar]
- 14.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142–61. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 15.Manning DM, Kuchirka C, Kaminski J. Miscuffing: Inappropriate blood pressure cuff application. Circulation. 1983;68:763–6. doi: 10.1161/01.cir.68.4.763. [DOI] [PubMed] [Google Scholar]
- 16.Fonseca-Reyes S, de Alba-García JG, Parra-Carrillo JZ, Paczka-Zapata JA. Effect of standard cuff on blood pressure readings in patients with obese arms. How frequent are arms of a ‘large circumference’? Blood Press Monit. 2003;8:101–6. doi: 10.1097/00126097-200306000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Linfors EW, Feussner JR, Blessing CL, Starmer CF, Neelon FA, McKee PA. Spurious hypertension in the obese patient. Effect of sphygmomanometer cuff size on prevalence of hypertension. Arch Intern Med. 1984;144:1482–5. [PubMed] [Google Scholar]
- 18.Elliott KE, McCall KL, Fike DS, Polk J, Raehl C. Assessment of manual blood pressure and heart rate measurement skills of pharmacy students: a follow-up investigation. Am J Pharm Educ. 2008;72:60. doi: 10.5688/aj720360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manning DM, Kuchirka C, Kaminski J. Miscuffing: Inappropriate blood pressure cuff application. Circulation. 1983;68:763–6. doi: 10.1161/01.cir.68.4.763. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien E, Pickering T, Asmar R, Myers M, Parati G, Staessen J, et al. Working group on blood pressure monitering of the european society of hypertension international protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2002;7:3–17. doi: 10.1097/00126097-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Iyriboz Y, Hearon CM, Edwards K. Agreement between large and small cuffs in sphygmomanometry: A quantitative assessment. J Clin Monit. 1994;10:127–33. doi: 10.1007/BF02886825. [DOI] [PubMed] [Google Scholar]
- 22.Maxwell MH, Waks AU, Schroth PC, Karam M, Dornfeld LP. Error in blood-pressure measurement due to incorrect cuff size in obese patients. Lancet. 1982;2:33–6. doi: 10.1016/s0140-6736(82)91163-1. [DOI] [PubMed] [Google Scholar]
- 23.Blood pressure monitors. Consumer Reports. 1992;5:295–9. [PubMed] [Google Scholar]
- 24.Russell AE, Wing LM, Smith SA, Aylward PE, McRitchie RJ, Hassam RM, et al. Optimal size of cuff bladder for indirect measurement of arterial pressure in adults. J Hypertens. 1989;7:607–13. doi: 10.1097/00004872-198908000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40:795–6. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- 26.Oliveira SM, Arcuri EA, Santos JL. Cuff width influence on blood pressure measurement during the pregnant-puerperal cycle. J Adv Nurs. 2002;38:180–9. doi: 10.1046/j.1365-2648.2002.02162.x. [DOI] [PubMed] [Google Scholar]
- 27.Chyun DA. A comparison of intra-arterial and auscultatory blood pressure readings. Heart Lung. 1985;14:223–8. [PubMed] [Google Scholar]


