Abstract
Background & objectives:
Prevention of parent-to-child transmission (PPTCT) services are an integral part of National AIDS Control Programme and their critical appraisal is necessary for improving quality care. The present study was conducted to evaluate the performance of PPTCT services in West Bengal during April, 2008 - March 2009 and April 2009 - March 2010 and identify gaps in service delivery for making suitable recommendations.
Methods:
Data were collected from the Computerized Management Information System and validated by cross-checking records at each district. Focus group discussions (FGDs) were conducted among programme managers, counsellors and antenatal women attending the Integrated Counselling and Testing Centres. Performance indicators and outcomes of FGDs were analyzed.
Results:
The proportion of antenatal women tested declined in 2009-2010 from 2008-2009 (64.3 to 63.8%). Proportions of counseled cases also declined (72.5 vs. 68.4%). HIV positivity rates among those tested were 0.13 and 0.14 per cent, respectively in two years. Proportion of mother-baby pairs receiving nevirapine prophylaxis was increased by 5 per cent. Medical colleges, and category A districts having high HIV prevalence provided better services. Follow up services of HIV-exposed birth cohorts were grossly unsatisfactory.
Interpretation & conclusions:
Gaps were identified at each step of service delivery for which capacity building, improvement of infrastructure including laboratory services and ensuring emergency labour room testing up to the sub-district level were imperative. Outsourcing follow up services to other community based organizations may also be considered.
Keywords: Antenatal, HIV, nevirapine prophylaxis, PPTCT
Prevention of mother-to-child transmission (PMTCT) of HIV has been at the forefront of global HIV prevention activities since 1998, following the success of the short-course zidovudine and single-dose nevirapine clinical trials1. These drugs offered the promise of a relatively simple, low-cost intervention that could substantially reduce the risk of HIV transmission from mother to baby. Several antiretroviral regimens are recommended in resource constrained settings, although nevirapine (either alone or with other drugs) is usually favoured because it is cheap, easy to administer, rapidly absorbed, and has a long half life1. Significant progress in the area of PMTCT has been made during the past several years. In 2008, 45 per cent of the estimated HIV-infected pregnant women in low- and middle-income countries received at least some antiretroviral (ARV) drugs to prevent HIV transmission to their child, this percentage was 35 per cent in 20072.
In India, adult HIV prevalence among women was estimated to be 0.25 per cent (range 0.18-0.39%) in 2006, while that among men was 0.44 per cent (range 0.30-0.68%). Of the 2.47 (range 2.0-3.1) million people living with HIV/AIDS (PLHA) in 2006, 89 per cent were adults in the 15-49 yr age group, 7 per cent were over 49 yr of age and 4 per cent were children3. In India, perinatal transmission accounts for around 3 per cent of the total HIV infections in the country. This route of transmission is called parent-to-child transmission to emphasize the role of fathers in both transmission of the virus and management and care of the mothers and their children4,5. Majority of the HIV infections among children are the result of parent-to-child transmission and this can be prevented through an effective package of PPTCT (Prevention of Parent to Child Transmission) services integrated with the existing reproductive and child health (RCH) services6. During 2007-2008, NACP III (National AIDS Control Programme Phase III: 2007-2012) renamed voluntary counselling and testing centres as Integrated Counselling and Testing Centres (ICTC). PPTCT services are now being provided at ICTC-Ante-Natal Care (ANC) units, separated from ICTC for general public, at the medical colleges and up to the district hospital level due to huge load. The PPTCT programme involves counselling and testing of pregnant women, detection of HIV-positive pregnant women, and the administration of prophylactic nevirapine to these women and their infants, to prevent the mother-to-child transmission of HIV5. At sub-divisional, State-general and rural hospitals, PPTCT services are delivered as an integrated function of ICTC for general public. In April - December 2009, among 44 lakh pregnant women who have been tested for HIV under the PPTCT programme, about 0.34 per cent were detected HIV positive. Those who are HIV positive, are given a single dose of nevirapine prophylaxis at the time of labour and newborn is also given a single dose of nevirapine within 72 h of birth. During this period, 9, 398 mother-baby pairs received nevirapine prophylaxis to prevent the mother-to-child transmission of HIV4.
In West Bengal with an estimated 0.4 per cent prevalence of HIV infection among pregnant women, there will be around 6400 HIV infected pregnant women a year. PPTCT units were established in the medical colleges in the State in January 2004 and thereafter covering district, sub-district and State general hospitals in the subsequent years. Till the end of December 2009, PPTCT services were available in around 121 ICTCs including medical colleges, district, sub-divisional, State general hospitals as well as in private and other set-ups7–9.
Based on the HIV surveillance data, epidemiological profile, risk and vulnerability, National AIDS Control Organization (NACO) has classified 611 districts of India into categories A, B, C and D, with category A having the highest prevalence and category D having the lowest. The planning of HIV related services has also been graded as per categorization of districts10. West Bengal has got no category D district.
In this context, the present study was undertaken to assess the current scenario of the PPTCT services provided across the State of West Bengal in India with the following specific objectives: (i) to evaluate the performance of PPTCT service delivery in West Bengal during April, 2008 - March 2009 and April 2009 - March 2010; and (ii) to identify gaps in delivery of PPTCT services and to make suitable recommendations.
Material & Methods
The study was undertaken by the Department of Community Medicine, of Calcutta National Medical College & Hospital, Kolkata in close collaboration with West Bengal State AIDS Prevention and Control Society. The study period was seven months (June 2010 - December 2010), and both quantitative and qualitative methods were adopted. The survey visits were made by the researchers themselves. The principal investigator visited most of the districts of West Bengal accompanied by the other researchers as per their convenience. Relevant data were collected from the CMIS (Computerized Management Information System) programme installed nation-wide at all State AIDS Control Society (SACS) for monitoring and evaluation of NACP-III. Data were validated and all discrepancies were resolved by cross-checking with the district level data management system. Due to time constraint single visits were made to the ICTCs where PPTCT services were provided in each district including medical colleges, district and sub-divisional hospitals, State general and rural hospitals. During these visits data were re-validated by reviewing the reports and registers.
Focus group discussions (FGDs) with a pre-designed checklist were conducted among the following three groups at ICTC-ANC sites of all medical colleges and 10 poorly performing districts (based on percentage of antenatal women tested for HIV less than 70% during 2009-2010): (i) District level nodal officers for NACP and the Medical Officers of ICTCs; (ii) PPTCT counsellors and the laboratory technicians; and (iii) Antenatal women attending the ICTCs.
The main purpose of the FGDs was to identify the gaps in provision of services related to PPTCT and to find out possible solutions, taking feedbacks from service providers and beneficiaries. A checklist was prepared with experts in accordance with Operational Guidelines for Integrated Counselling and Testing Centres, NACO (2007)11. The checklist was standardized with inputs from public health experts and pre-tested to reduce inter-observer variations.
For heath functionaries a group of 4-5 members was formed and in case of antenatal women groups of 6-8 were selected after obtaining their informed consent and assuring strict confidentiality. The topics of discussion with health personnel mainly centered around the reasons for non-attendance of antenatal women at the ICTCs for counselling and testing, difficulties faced in providing services to directly-in-labour cases, training status and needs of the service providers, reasons behind non-coverage of a large number of mother-baby pairs with nevirapine prophylaxis, difficulties faced in tracking HIV-positive pregnant women who were lost to follow up before or after delivery and possible solutions to the problem.
The topics discussed with the groups of HIV-positive antenatal women were mainly regarding the convenience of location and timings of ICTCs and laboratories, whether test results were received on the same day of counselling, whether they had understood the implications of a positive test result, whether they had been informed about “window period”, their intention of having delivery done at the same institute, whether the counsellors kept in touch with them periodically, their opinion regarding paying them home visit by a health staff or by NGO workers or a member of the positive people network, and whether they have understood the importance of nevirapine prophylaxis and that of regular follow up of HIV exposed babies (babies born to HIV positive mothers) and getting them tested for HIV at the end of 18 months. The discussions were recorded verbatim.
Relevant variables used as performance indicators of PPTCT services are described below:11
Number (%) of newly registered antenatal cases: This included all new antenatal cases registered for the first time at any of the ICTCs that provided PPTCT services during any time of the antenatal period and also those cases who were registered for the first time at the time of admission during labour (otherwise referred to as ‘directly-in-labour’ cases).
Number (%) of newly registered antenatal cases provided counselling: This included those newly registered antenatal cases who were provided with counselling.
Number (%) of newly registered antenatal cases tested for HIV: This included those newly registered antenatal cases who were tested for HIV.
Number (%) of newly registered antenatal cases who were found HIV positive: This included those antenatal cases who were found HIV positive out of those tested for HIV.
Number of live births to antenatal cases who were found HIV positive: This included live births during the study period (2008-2009 and 2009-2010) to HIV positive pregnant women.
Number (%) of mother and baby pairs provided with prophylactic treatment: This included pairs of HIV positive mothers and their exposed babies who were provided single dose nevirapine as prophylaxis out of the total number of HIV positive mothers. It may be noted that some HIV positive mothers who were registered earlier than the study period delivered during the study period. At the same time, some pregnant women who were newly registered during antenatal visits were yet to deliver.
HIV-exposed live birth cohort analysis: This included the outcome of HIV positive deliveries during 2005, 2006 and 2007. These babies supposed to be followed up at regular intervals were traced at 18 months and those found alive were tested for HIV with rapid test kits available at the ICTCs.
Data analysis: Data were analyzed using simple statistical proportions with SPSS 10.0 for Windows (Chicago, USA). Relevant performance indicators for evaluation of PPTCT service delivery were laid down in simple tabular form. Analysis for identification of gaps was done by considering both performance indicators and outcome of focus group discussions. Issues related to the topic of discussions and emerging themes were scrutinized and checked for general consensus between the three groups and data triangulation.
Results
Overall, the number of newly registered antenatal cases was 3,45,460 and 4,22,416 in 2008-2009 and 2009-2010, respectively. However, the proportions of counselled cases have declined from 2008-2009 to 2009-2010 (72.5 vs. 68.4%) (Table I). Further analysis revealed that category-wise, in 2008-2009, both A and C had more or less similar proportion of cases counselled 78.5 (97,043/1,23,545) and 72.3% (1,22,031/1,68,892), respectively, but the proportion was much lower in category B districts [58.9% (31,216/53,023)]. The proportion declined further in 2009-2010 in category B [57.2% (37,255/65,085)]. However, the most dramatic decrease by a staggering 8.8 per cent was observed in category C in 2009-2010. According to types of institution, medical colleges with their upgraded infrastructure have shown the highest proportion in comparison to other two types in both years, though suffered from slight decline 87.1% (97,237/1,11,694) to 86.8% (1,04,783/1,20,768). Institutions classified as “others” showed a further decline from an already poor proportion 57.8% (1, 26,587/2, 19,161) from 63.5% (95,821/1,50,984). Increase in client load and lack of infrastructure may be the reasons behind such decline. Overall, the percentage of antenatal women tested out of the total registered has been reduced in two successive years (64.3 to 63.8%) (Table I). Category-wise, although a satisfactory increase of about 7 per cent has been observed in category A districts, categories B and C showed further poor performance (decline of about 1.3% and 3.7%, respectively) (Table II). Institution-wise, again, the medical colleges performed much better in this aspect Above 80% in both years, (93,141/1,11,694 in 2008-2009 and 97,867/1,20,768 in 2009-2010) though there had been a decline of 2.4 per cent whereas district hospitals and ‘others’ have marginally improved their performances, 1.7 and 2.5 per cent respectively (data not shown). The percentage of antenatal women found positive out of the total tested remained almost the same in two successive years in West Bengal. In 2008-2009, out of 2,22,230 tested, 291 (0.13%) was diagnosed positive whereas in 2009-2010, 375 out of 2,69,471 (0.14%) were found positive (Table I). According to category of districts, categories A districts have a reassuring proportion similar to State averages in both years. However, category B districts have shown an increase in proportion of about 0.06 per cent. Category C districts have positivity rates below that of the State averages in both years as expected (Table II).
Table I.
Summary of performance of PPTCT service delivery in West Bengal during 2008-2009 and 2009-2010

Table II.
District-wise performance of PPTCT service delivery in West Bengal during 2008-2009 and 2009-2010
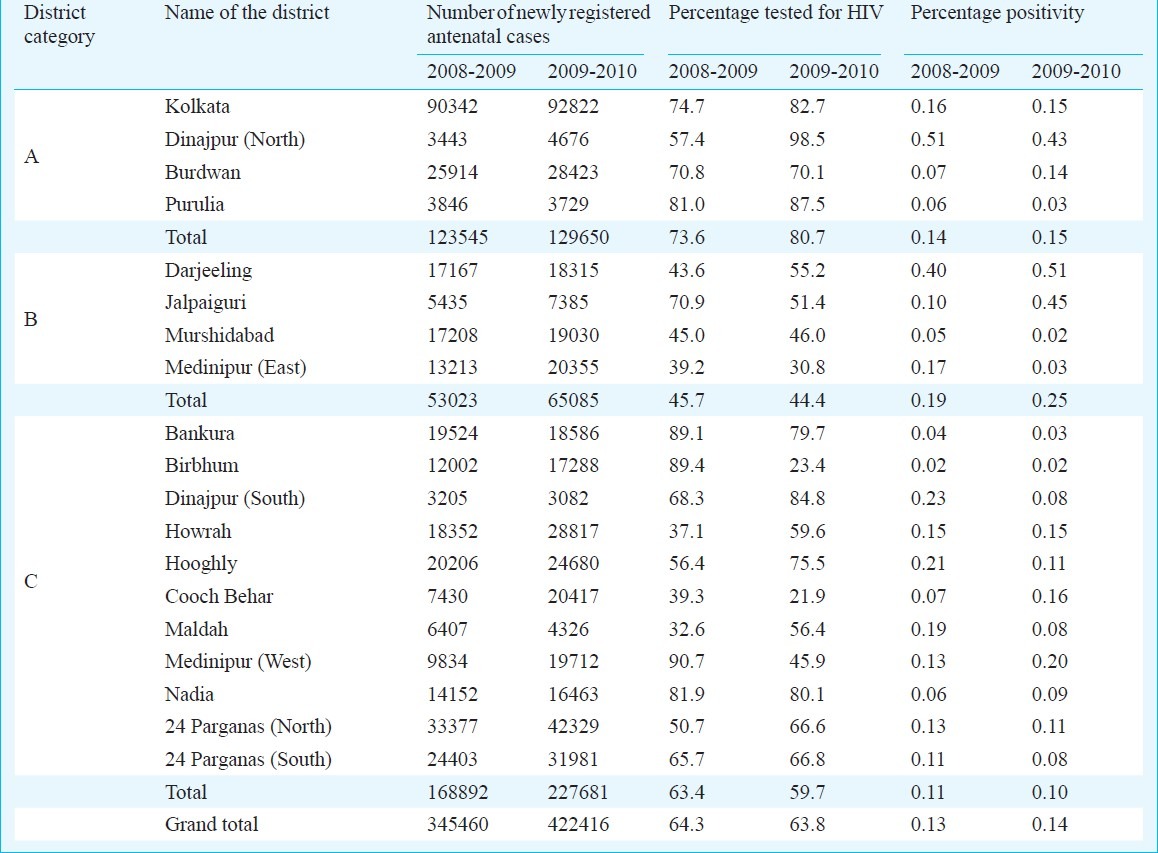
Institution wise, all types of institution have shown proportions more or less similar to the state average (between 0.13-0.14%) (data not shown). District-wise observations from 2008-2009 and 2009-2010 revealed that some districts differed considerably from other ones belonging to the same category. In category A, North Dinajpur had high positivity rate in both the years (0.51 and 0.45%) and an increase in uptake of HIV testing (from 57.4 to 98.5%). Purulia, although classified into category A, showed a further decline in an already low positivity rate (from 0.06 to 0.03%). In category B, Jalpaiguri showed an increase in positivity rate (from 0.10 to 0.45%) in spite of a decreased uptake of testing (from 70.9 to 51.4%). Somewhat similar results were observed in some of the category C districts. Cooch Behar showed a high rise in positivity (from 0.07 to 0.16%) despite a decrease in testing (from 39.3 to 21.9%). Medinipur (West) also showed an increase in positivity rate (from 0.13 to 0.20%) in spite of a sharp fall in uptake of testing (from 90.7 to 45.9%) (Table II).
Although there was an increase in the proportion of mother-baby pair who received nevirapine out of the HIV positive mothers by 5 per cent in two consecutive years, the absolute proportions (44.3 and 49.3%) were grossly dissatisfactory being not even half of the total seropositives (Table I). Category A districts with more than 60 per cent coverage in both years, showed a modest increase by about 8 per cent. But it was category C that had significantly improved their coverage by about 11 per cent. On the other hand, category B showed further decline from an already poor coverage by about 11 per cent (Table III). It was observed that the average for a particular category was sometimes distorted by outliers making the proper interpretation difficult. In category A, better nevirapine coverage was reflected just because of the results of Kolkata, owing to the better performance of the five medical colleges in this district, whereas the performance was poor in the remaining districts (Table III). In general, medical college hospitals with their adequate infrastructure and manpower have quite obviously excelled in providing nevirapine prophylaxis, though there has been an alarming decrease in the coverage in medical colleges by about 8 per cent from 2008-2009 to 2009-2010 so that proportion has decreased to below 80 per cent [74.5% (102/137)]. On the other hand, district hospitals and other hospitals succeeded in achieving an increase in coverage by about 20 per cent [from 39.4% (26/66) to 59.1% (39/66)] and 21 per cent [from 4.7% (5/106) to 25.6 per cent (44/172)] respectively (data not shown).
Table III.
District-wise coverage of mother-baby pairs with nevirapine prophylaxis in West Bengal during 2008-2009 and 2009-2010

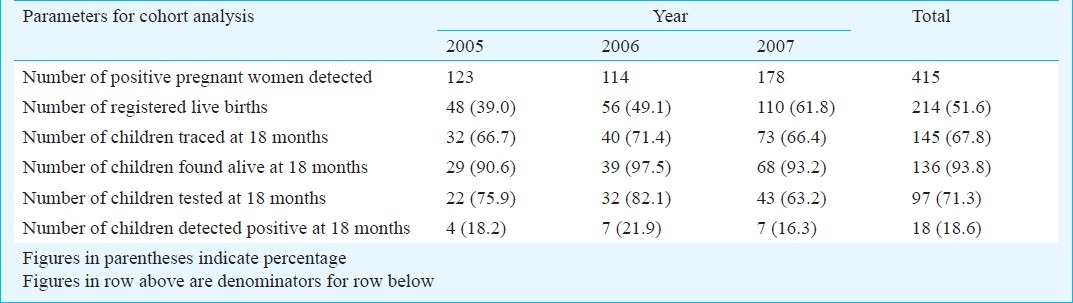
HIV exposed children born during 2005, 2006 and 2007 were followed up to 18 months of age and tested for HIV status. There were 214 registered live births out of 415 positive pregnancies (51.6%). Unfortunately only 145 (67.8%) of the registered live births could be traced at 18 months. Again 71.3 per cent (97/136) of those found alive could be tested. About 18.6 per cent of those tested (18/97) were found to be HIV positive. It is thus evident that the follow up system is still at its incipient stage (Table IV).
Table IV.
Birth cohort analysis for PPTCT programme (2005-2007) in West Bengal
By analyzing these performance indicators, as well as physical verification of the sites and situation and outcomes of the focus group discussions, a number of themes related to PPTCT service delivery and the related gaps were identified (Box).
Box.
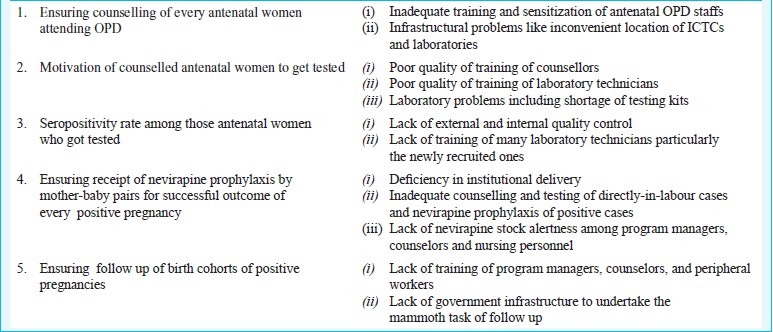
Themes releted to PPTCT service delivery
Discussion
There is a step-wise approach in service delivery of PPTCT programme beginning with registration and counselling and every step is crucial to reduce perinatal transmission of HIV. The present study revealed that the proportion of antenatal women tested declined in 2009-2010 from 2008-2009. Proportions of counselled clients also declined. HIV positivity rates among those tested were 0.13 and 0.14 per cent, respectively in two years. However, a wide variation was observed between the different districts. The increased uptake of HIV testing in North Dinajpur in category A could be partly contributed to the high HIV prevalence in Islampur sub-divisional area which lies very close to northern part of Bihar and also shares an international border with Bangladesh with high rate of in-migration. All types of high-risk group (HRG) populations namely injection drug users (IDU), sex workers, truckers and migrant labourers could be found here in a large number. The other reason for high testing uptake might be the special drive made by the administration during 2009-2010 coordinating the activities of the ICTCs, ART (anti-retroviral therapy) center and targeted intervention (TI) projects and strengthening the existing link-worker scheme for tracking the HIV positives. Purulia, being a category A district, had only two ICTCs, one at the district hospital and another at a near-by sub-divisional hospital, covering only a small part of the total population in this district. This might be one of the reasons behind its low positivity rate in two successive years. Short supply of testing kits and selective counselling of the high risk groups and their partners led to high positivity rate despite decreased uptake in testing in districts like Jalpaiguri, Cooch Behar and Medinipur (West). In a cohort analysis on PPTCT service utilization in Gujarat during 2005 to 2008, it was found that around 72.1 per cent of the antenatal clients out of those newly registered received pre-test counselling, with some districts showing significant gap between registration and counselling12.
Challenges are being faced in implementation of PPTCT services across the world. Inadequate counselling services delivered to clients were found to affect service utilization in Nyanza Provincial Hospital in Kenya, as was indicated by long waiting times, short post-test counselling duration, lack of disclosure of positive HIV status, and lack of follow up counselling for HIV-positive clients13. Study in Vietnam showed only 44 per cent of the women had received minimal PMTCT services and 42 per cent women received no counselling14.
The present study showed that the HIV-positivity rate almost remained the same in the two years (0.13 and 0.14%). In a study Kumar et al15 among 750 PPTCT sites from 27 States of India, reported HIV prevalence 0.68 per cent, much higher than that of the present study14. The possible reason is that overall HIV prevalence of West Bengal is <0.5 per cent3. The present study showed a wide variation in the testing uptake between districts, even within the same category. The study from Gujarat12 revealed that only 60.1 per cent of all registered antenatal cases were tested for HIV, with inter-district variations particularly in Rajkot and Surat. The reasons cited were poor quality of counselling and inadequate testing facilities and referral services12. In a cross-sectional sample of 400 recently pregnant women from rural Maharashtra, India, only 3.3 per cent of women received antenatal HIV testing. Women who did not receive HIV testing, compared with women who did, were 95 per cent less likely to have received antenatal HIV counselling and 80 per cent less aware of an existing HIV testing facility15.
Coverage of mother-baby pairs with nevirapine prophylaxis had remained a daunting challenge, particularly in rural areas. The present study showed that although this had increased by 5 per cent in two successive years, it was still grossly unsatisfactory. In a sub-district level hospital in Tamil Nadu, India, of the 7866 pregnant women who accessed the PMTCT services, group counselling was provided to all, 0.77 per cent test positive and 83 per cent received nevirapine, proportions much higher than that of the present study16. Mother-baby pair coverage, as shown in Gujarat study was found to be only 56.1 per cent, but definitely higher than that in the present study12. Somewhat similar results were obtained from the other parts of world as well. In spite of high levels of awareness of trained staffs, nevirapine uptake varied in a clinic in South Africa, with an average of 56 per cent17.
The present study revealed a dismal performance in the follow up of HIV exposed babies (babies born to HIV positive mothers). Only 67.8 per cent of the registered live births could be traced at 18 months, and 71.3 per cent of those found alive could be tested of whom 18.6 per cent were found to be HIV positive. Tracking of HIV exposed babies is the most crucial and most difficult part of PPTCT service delivery as the ultimate success of the programme depends upon the HIV test results in these exposed babies.
In conclusion, analyzing the performance indicators, as well as physical verification of the sites and situation and outcomes of the focus group discussions, wide gaps were observed between different steps of service delivery which varied across different levels of institutions and different categories of districts as well leading to poor performance indicators. Appropriate interventions need to be taken by the authorities to fill these gaps, such as capacity building, training of laboratory staff, promotion of institutional deliveries, ensuring emerging labour room testing and outsourcing of follow up services to other community based organizations.
Acknowledgment
Authors thank to Dr Kaninika Mitra, Health & HIV Specialist, UNICEF Office for West Bengal, for her useful suggestions regarding the study design and analysis, and acknowledge the core support from the West Bengal State AIDS Prevention and Control Society. Authors also thank to all the district programme managers, hospital administrators and ICTC counsellors for their cooperation and participation during our visits to the districts.
References
- 1.Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants in resource-limited settings. Geneva: WHO; 2006. [accessed on November 15, 2010]. World Health Organization. Available from: http://www.who.int/hiv/pub/mtct/guidelines/en/ [Google Scholar]
- 2.Towards universal access: scaling up priority HIV/AIDS interventions in the health sector. Progress report 2009. Geneva: World Health Organization; 2009. [accessed on November 17, 2010]. WHO, UNAIDS, UNICEF. Available from: http://www.who.int/entity/hiv/pub/tuapr_2009_en.pdf . [Google Scholar]
- 3.Pandey A, Reddy DCS, Ghys PD, Thomas M, Sahu D, Bhattacharya M, et al. Improved estimates of India's HIV burden in 2006. Indian J Med Res. 2009;129:50–8. [PubMed] [Google Scholar]
- 4.Government of India. Ministry of Health & Family Welfare. Department of AIDS Control. National AIDS Control Organization. Annual Report 2009-10. [accessed on November 17, 2010]. Available from: http://www.nacoonline.org/upload/AR202009-10/NACO_AR_English corrected.pdf .
- 5.Government of India. Ministry of Health & Family Welfare. Department of AIDS Control. National AIDS Control Organization. Annual Report 2008-09. [accessed on December 17, 2010]. Available from: http://www.nacoonline.org/upload/publication/Annual_Report_NACO_2008-09.pdf .
- 6.Prevention of parent to child transmission (PPTTC) of HIV India. Sensitization training curriculum presentation manual. New Delhi: NACO; 2004. Government of India. Ministry of Health & Family Welfare. National AIDS Control Organization (NACO) pp. 41–56. [Google Scholar]
- 7.Annual Report 2009-10. West Bengal State AIDS Prevention & Control Society. Department of Health & Family Welfare. Government of West Bengal. [accessed on December 22, 2010]. Available from: http://www.wbhealth.gov.in/wbsapcs/report/AnnualReport09-10Final.pdf .
- 8.Annual Report 2008-09. West Bengal State AIDS Prevention & Control Society. Department of Health & Family Welfare. Government of West Bengal. [accessed on December 22, 2010]. Available from: http://www.wbhealth.gov.in/wbsapcs/report/AnnualReport2008-2009.zip .
- 9.Programme Implementation Plan for the State of West Bengal. National AIDS Control Programme Phase III 2007-12. West Bengal State AIDS Prevention & Control Society. [accessed on December 22, 2010]. Available from: NACP III_PIP_WB.pdf_ param_page_id=5¶m_link_id=4 .
- 10.Government of India. Ministry of Health & Family Welfare. Department of AIDS Control. National AIDS Control Organization. Prioritization of Districts For Programme Implementation: Categorization of Districts based on HIV Sentinel Surveillance 2004, 2005 and 2006_Detailed List. [accessed on December 25, 2010]. Available from: District_Categorisation_for Priority_Attention.pdf .
- 11.Operational guidelines for integrated counseling and testing centres. New Delhi: National AIDS Control Organization; 2007. Government of India. Ministry of Health & Family Welfare; p. 34. [Google Scholar]
- 12.Joshi U, Kadri A, Bhojiya S. Prevention of parent to child transmission services and interventions - coverage and utilization: A cohort analysis in Gujarat, India. Indian J Transm Dis. 2010;31:92–8. doi: 10.4103/2589-0557.74983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moth IA, Ayayo ABCO, Kaseje DO. Assessment of utilisation of PMTCT services at Nyanza Provincial Hospital, Kenya. SAHARA J. 2005;2:244–50. doi: 10.1080/17290376.2005.9724847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar R, Virdi NK, Lakshmi PVM, Garg R, Bhattacharya M, Khera A. Utility of Prevention of Parent-to-Child Transmission (PPTCT) Programme data for HIV surveillance in general population. Indian J Med Res. 2010;132:256–59. [PubMed] [Google Scholar]
- 15.Sinha G, Dyalchand A, Khale M, Kulkarni G, Vasudevan S, Bollinger RC. Low Utilization of HIV testing during pregnancy: What are the barriers to HIV testing for women in rural India? J Acquir Immune Defic Syndr. 2008;47:248–52. [PubMed] [Google Scholar]
- 16.Parameshwari S, Jacob MS, Vijayakumari JJ, Shalini D, Sushi MK, Sivakumar MR. A Program on Prevention of Mother to Child Transmission of HIV at Government Hospital, Tiruchengode Taluk, Namakkal District. Indian J Commun Med. 2009;34:261–3. doi: 10.4103/0970-0218.55298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rispel LC, Peltzer K, Phaswana-Mafuya N, Metcalf CA, Treger L. Assessing missed opportunities for the prevention of mother-to-child HIV transmission in an Eastern Cape local service area. S Afr Med J. 2009;99:174–9. [PubMed] [Google Scholar]


