Abstract
Background & objectives:
Scrub typhus is one of the differential diagnoses of haemorrhagic fevers especially if associated with jaundice and/or renal failure. Goa State in the western region of India has been witnessing increased incidence of such fevers, therefore, the present study was undertaken to identify whether scrub typhus is the aetiological agent.
Methods:
Adult patients presenting with undiagnosed febrile illness between June 2009 to October 2010, were evaluated. Testing was done using a commercial ELISA kit for specific IgM antibodies against Orientia tsutsugamushi.
Results:
Of the 44 patients included in the study, 15 (34%) were found to be positive for IGM antibodies against O. tsutsugamushi. The cases were seen mainly in the months between July to November. The common symptoms noted were fever, myalgias, gastrointestinal complaints, followed by breathlessness, rash and jaundice. The pathognomonic features such as eschar and lymphadenopathy were seen only in two patients. Nearly two third of the patients had leukocytosis (67%) and low serum albumin (60%). The most common complication noticed was hepatitis (80%) followed by acute respiratory distress syndrome (ARDS) (60%), thrombocytopenia (40%) and acute renal failure (33%). Five patients died in the course of illness.
Interpretation & conclusions:
Our results showed that scrub typhus should be considered in the differential diagnosis of acute febrile illness associated with gastrointestinal symptoms, rash, myalgia, including those with organ dysfunctions such as hepatorenal syndrome, coagulopathy or ARDS. Empirical treatment with doxycycline or macrolides may be given in cases with strong suspicion of scrub typhus.
Keywords: Eschar, hepatorenal syndrome, ictero-haemorrhagic fever, Orientia tsutsugamushi
Scrub typhus is a rickettsial disease caused by the organism Orientia tsutsugamushi. The organism is transmitted through the bite of larval forms (chiggers) of trombiculid mites1. It presents as either a non-specific febrile illness with constitutional symptoms such as fever, rash, myalgias and headache or with organ dysfunctions involving organs such as kidney (acute renal failure, ARF), liver (hepatitis), lungs (acute respiratory distress syndrome, ARDS), central nervous system (meningitis), or with circulatory collapse with haemorrhagic features1,2. Scrub typhus is one of the differential diagnoses (in addition to leptospirosis, malaria or dengue fever) in patients with haemorrhagic fever especially if associated with jaundice and/or renal failure2.
Scrub typhus is widespread in the so called “tsutsugamushi triangle” which includes Japan, Taiwan, China and South Korea on the north, India and Nepal on the west and Australia and Indonesia on the south3. In India, epidemics of scrub typhus have been reported from north, east and south India4–11. Although the disease is endemic in our country, it is grossly underdiagnosed owing to the non-specific clinical presentation, lack of access to the specific diagnostic facilities in most areas, and low index of suspicion by the clinicians12.
Goa is a costal State located in the western region of India, along the Western Ghats. There has been an increased incidence of ictero-haemorrhagic fevers or fever with hepatorenal syndrome presenting to our institution in the recent past. After ruling out complicated malaria, leptospirosis and dengue fever, many of these cases remained undiagnosed. As the prevalence of scrub typhus has been reported in neighbouring States4–7 and the existence of trombiculid mites is reported from Western Ghats13, the present study was undertaken to assess the aetiological agent in these fever cases in Goa.
Material & Methods
Goa Medical College is a tertiary care teaching institution in the State of Goa where this study was conducted. All consecutive adult patients presenting with febrile illness from June 2009 to October 2010 were evaluated. Other likely diagnoses such as malaria, leptospirosis, dengue fever, viral pharyngitis, enteric fever, urinary tract infection were ruled out by history, clinical examination and appropriate laboratory investigations. The patients were subjected to a battery of investigations such as urine analysis, complete blood count, platelet count, renal function tests and liver function tests, smear for malarial parasite, rapid antigen test for malaria, serology for leptospirosis and dengue haemorrhagic fever, blood widal and culture. The patients were subjected to further investigations such as bleeding and clotting time, prothrombin time / International normalized ratio (INR), activated partial thromboplastin time, fibrin degradation products, chest X-ray, abdominal ultrasonography, wherever necessary. Blood samples (5 ml) were collected and serum preserved at -70°C from patients who remained febrile and no aetiological diagnosis could be made. These samples were subjected, retrospectively, in batches, to testing for specific IgM antibodies against O. tsutsugamushi using a commercial ELISA kit (InBiOS International Inc. USA). The kit uses O. tsutsugamushi derived recombinant antigen mix. The test was performed as per manufacturer's instructions. The study protocol was approved by institutional Ethics Committee and informed consent was obtained from the patients.
The patients having of IgM antibodies against O. tsutsugamushi in their serum samples were diagnosed as having scrub typhus. Various complications such as acute renal failure, hepatitis, ARDS, disseminated intravascular coagulation, pancreatitis, meningitis, myocariditis, etc. were noted.
The following criteria (based on standard definitions given in Harrison's Principals of Internal Medicine) were used to diagnose above complications:
(i) Acute renal failure was defined as urine output less than 400 ml/24 h or serum creatinine >1.6 mg% failing to improve after adequate rehydration. (ii) Patients who had elevation of serum bilirubin > 3 mg% and/or elevation of serum transaminases >3 times the upper limit of normal were labelled as having hepatitis. (iii) Acute onset of non cardiogenic pulmonary oedema manifesting with bilateral alveolar or interstitial infiltrates on chest radiograph and PaO2/FIO2<200 mm Hg on arterial blood gas analysis confirmed the presence of ARDS. (iv) Disseminated intravascular coagulation (DIC) was defined as clinical manifestations of bleeding along with thrombocytopenia and elevated coagulation profile (raised fibrin degradation products, prolonged prothrombin time/INR, activate partial thromboplastin time, aPTT). (v) Pancreatitis was defined as acute onset of clinical signs such as abdominal pain, vomiting, guarding/ tenderness associated with elevation of serum amylase/ lipase >3 times upper limit of normal. (vi) Myocarditis was defined as presence of systolic global left ventricular wall motion abnormalities on 2D echocardiography along with ECG changes and clinical findings consistent with left ventricular dysfunction in a previously normal individual. (vii) Systolic blood pressure of <90 mm Hg for at least 1 h despite adequate fluid resuscitation was labelled as shock. (viii) Meningitis was defined as presence of altered sensorium and signs of meningeal irritation associated with elevated proteins and neutrophilic cytology on CSF analysis.
The patients who were serologically diagnosed of having scrub typhus or those with strong clinical suspicion of scrub typhus, were given doxycycline in the dosage of 100 mg twice a day for 10 days. All other supportive measures such as haemodialysis, ventillatory support, transfusion of blood components, inotropic support were given as per the indications.
Results
A total of 44 consecutive patients with undiagnosed fever were included in the study and 15 (34%) showed presence of IgM antibody against scrub typhus. Four of these 15 patients were referred from the neighbouring States of Maharashtra and Karnataka while the remaining 11 patients were the native residents of Goa State. Ten were females; the youngest patient was 22 yr old while the oldest was aged 65 yr. The cases were seen mainly in the months between July to November.
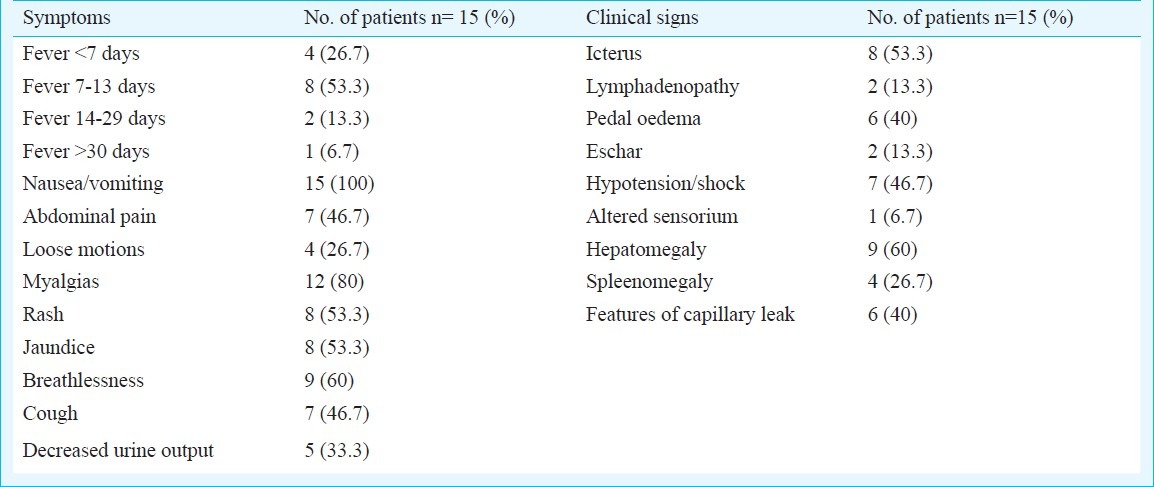
The common symptoms noted were fever, myalgias, nausea and vomiting, followed by breathlessness, gastrointestinal complaints such as abdominal pain and loose motions, rash and jaundice. The commonest signs seen were hepatomegaly (60%) and icterus (53%). Nearly half of patients (40%) had signs suggestive of capillary leak syndrome in the form of generalized anasarca, pedal oedema, hypotension and low serum albumin. The pathognomonic features such as eschar and lymphadenopathy were rare in the present study; only two patients had the presence of eschar with lymphadenopathy (Table I).
Table I.
Clinical features of the patients included in the study
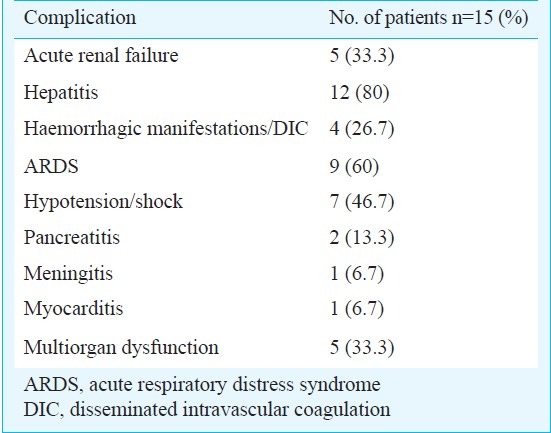
Among the laboratory parameters, leukocytosis (66.7%), raised transaminases (80%) (mean SGOT(aspartate transaminase)/SGPT (alanine transaminase) were 264/139.6 IU/l) and alkaline phosphatase (60%) patients (mean 188.2 IU/l) and low serum albumin (60%) were main laboratory findings noted (Table II). Hepatitis (80%), ARDS (60%), thrombocytopenia (40%) and acute renal failure (33%) were main complications noted in the study (Table III). Five patients presented with multiorgan dysfunction and died in the hospital; the remaining ten patients were discharged on recovery. In the present study, nine patients were treated with doxycycline empirically in the dosage of 100 mg twice a day for 10 days on the clinical suspicion of scrub typhus, seven patients responded promptly to treatment while the remaining two presented to hospital late with dysfunction of multiple organs and died. Three of total five patients, who died, could not receive doxycycline or macrolides.
Table II.
Laboratory investigations and results in the patients
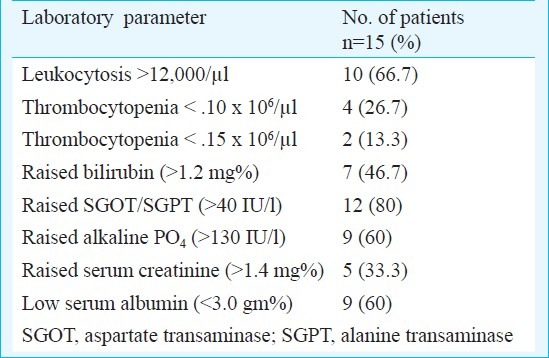
Table III.
Complications of scrub typhus in the patients
Discussion
There have been reports of the outbreaks of scrub typhus from various parts of the country in the recent past with serological evidence of widespread prevalence of spotted fevers and scrub typhus in the neighbouring States4,5,7–11. Thus, there was a strong possibility of presence of rickettsial diseases in Goa also but it had not been documented yet. Eleven out of 15 serologically confirmed cases in the present study were the natives of Goa. This proves the existence of the disease in the State.
In the present study most of the cases were seen during the months of July to November. Such post monsoon surge is reported earlier also5–7,9,11. This is because, during the months of August to October, farmers are involved in the harvesting activity in the fields, where they are exposed to the bites of larval mites. Further, in the immediate post monsoon period (September to early months of the next year), there is growth of secondary scrub vegetation, which is the habitat for trombiculid mites (mite islands)13.
The disease presents as an acute febrile illness with non-specific signs and symptoms1. In our study, the commonest presentation seen was that of fever with myalgias (80%) or with rash (54%). Another important finding was predominance of gastrointestinal signs and symptoms such as nausea and vomiting, abdominal pain, and loose motions. This finding assumes importance, as there is limited available information on the relationship between scrub typhus and gastrointestinal dysfunction14. Since clinical presentation of fever with rash/ myalgia occurs in many other febrile illnesses like dengue fever or leptospirosis, presence of gastrointestinal complaints could be used as a differentiating feature for suspecting scrub typhus.
A necrotic eschar at the inoculating site of the mite is pathognomonic of scrub typhus1,3, however, it is rarely seen in south East Asia and Indian subcontinent5,7,11. In our series, eschar was seen in only two patients. Though lymphadenopathy is common in scrub typhus8,15, it was rare in present study.
Another important finding noted was the occurrence of capillary leak. O. tsutsugamushi infects vascular endothelium leading to vasculitis and organ dysfunction2. Vascular injury to capillary endothelium may be the causative factor for capillary leak. However, this finding needs to be validated in a large number of patients.
Similar to many other case series5,7,14, most patients had elevation of serum transaminases, even without any other evidence of multiorgan dysfunction. Other laboratory findings noted were leukocytosis, thrombocytopenia, and low serum albumin. While low serum albumin and leucocytosis are thought to be associated with severe scrub typhus16,17, these findings need to validated in a large sample.
The mainstay of diagnosis in scrub typhus is serology18. The gold standard serological tests are immunoflorescence antibody test or indirect immunoperoxidase assay18 but are out of reach in our country owing to high costs. The cheapest test currently available and used extensively in our country4,6,7,8,11 is Weil- Felix test which is highly specific, but lacks sensitivity12,15. In the present study, we used ELISA testing for IgM antibodies against O. tsutsugamushi for diagnosis. This test has shown good sensitivity and specificity4,12,18 and has been adequately validated5.
Complications in scrub typhus develop after first week of illness1 and are directly related to the blood load of O. tsutsugamushi19,20. In the present study, the most common organ dysfunction was hepatitis followed by ARDS, circulatory collapse and acute renal failure. The present case series is about patients presenting at our centre which is a tertiary referral centre where patients are referred from peripheral primary care or district level for complications. This referral bias has led to high complication rate in this study. Two patients had acute pancreatitis which has not been reported earlier. In our study, five patients succumbed to disease (mortality rate 33.5%). This is relatively higher as compared to other studies5,7,17. All patients who died had presented with multiorgan dysfunction; of these, three had not received tetracyclines or macrolides. In other two patients, doxycycline was initiated late (second week of illness).
In conclusion, our study showed that scrub typhus should be considered in the differential diagnosis of acute febrile illness associated with gastrointestinal symptoms, rash, myalgias, including those with organ dysfunctions such as hepatorenal syndrome, coagulopathy or ARDS. Though eschar is pathognomonic of the disease, it may not be commonly seen, and its absence does not rule out scrub typhus. Delay in treatment may lead to complications and higher mortality. As patients respond to doxycycline or macrolides, empirical treatment with these antibiotics may be given in cases where there is a strong suspicion of scrub typhus.
References
- 1.Mahajan SK. Scrub typhus. J Assoc Physicians India. 2005;53:954–8. [PubMed] [Google Scholar]
- 2.Kothari VM, Karnad DR, Bichile LS. Tropical infections in the ICU. J Assoc Physicians India. 2006;54:291–8. [PubMed] [Google Scholar]
- 3.Chogle AR. Diagnosis and treatment of scrub typhus - the Indian scenario. J Assoc Physicians India. 2010;58:11–2. [PubMed] [Google Scholar]
- 4.Mathai E, Lloyd G, Cherian T, Abraham OC, Cherian AM. Serological evidence for the continued presence of human rickettsioses in southern India. Ann Trop Med Parasitol. 2001;95:395–8. doi: 10.1080/00034980120065804. [DOI] [PubMed] [Google Scholar]
- 5.Varghese GM, Abraham OC, Mathai D, Thomas K, Aaron R, Kavitha ML, et al. Scrub typhus among hospitalised patients with febrile illness in South India: magnitude and clinical predictors. J Infect. 2006;52:56–60. doi: 10.1016/j.jinf.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Kamarasu K, Malathi M, Rajagopal V, Subramani K, Jagadeeshramasamy D, Mathai E. Serological evidence for wide distribution of spotted fevers and typhus fever in Tamil Nadu. Indian J Med Res. 2007;126:128–30. [PubMed] [Google Scholar]
- 7.Vivekanandan M, Mani A, Priya YS, Singh AP, Jayakumar S, Purty S. Outbreak of scrub typhus in Pondicherry. J Assoc Physicians India. 2010;58:24–8. [PubMed] [Google Scholar]
- 8.Mahajan SK, Rolain JM, Sankhyan N, Kaushal RK, Raoult D. Pediatric scrub typhus in Indian Himalayas. Indian J Pediatr. 2008;75:947–9. doi: 10.1007/s12098-008-0198-z. [DOI] [PubMed] [Google Scholar]
- 9.Somashekar HR, Moses PD, Pavithran S, Mathew LG, Agarwal I, Rolain JM, et al. Magnitude and features of scrub typhus and spotted fever in children in India. J Trop Pediatr. 2006;52:228–9. doi: 10.1093/tropej/fmi096. [DOI] [PubMed] [Google Scholar]
- 10.Ittyachen AM. Emerging infections in Kerala: a case of scrub typhus. Natl Med J India. 2009;22:333–4. [PubMed] [Google Scholar]
- 11.Sharma A, Mahajan S, Gupta ML, Kanga A, Sharma V. Investigation of an outbreak of scrub typhus in the himalayan region of India. Jpn J Infect Dis. 2005;58:208–10. [PubMed] [Google Scholar]
- 12.Batra HV. Spotted fevers and typhus fever in Tamil Nadu. Indian J Med Res. 2007;126:101–3. [PubMed] [Google Scholar]
- 13.Tilak R. Ticks and mites. In: Bhalwar RV, editor. Textbook on public health and community medicine. 1st ed. Pune: Department of Community Medicine, AFMC, Pune; 2009. pp. 955–9. [Google Scholar]
- 14.Aung-Thu, Supanaranond W, Phumiratanaprapin W, Phonrat B, Chinprasatsak S, Ratanajaratroj N. Gastrointestinal manifestations of septic patients with scrub typhus in Maharat Nakhon Ratchasima Hospital. Southeast Asian J Trop Med Public Health. 2004;35:845–51. [PubMed] [Google Scholar]
- 15.Mahajan SK, Kashyap R, Kanga A, Sharma V, Prasher BS, Pal LS. Relevance of Weil -Felix test in diagnosis of scrub typhus in India. J Asssoc Physicians India. 2006;54:619–21. [PubMed] [Google Scholar]
- 16.Kim DM, Kim SW, Choi SH, Yun NR. Clinical and laboratory findings associated with severe scrub typhus. BMC Infect Dis. 2010;10:108. doi: 10.1186/1471-2334-10-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee CS, Hwang JH, Lee HB, Kwon KS. Risk factors leading to fatal outcome in scrub typhus patients. Am J Trop Med Hyg. 2009;81:484–8. [PubMed] [Google Scholar]
- 18.Koh GC, Maude RJ, Paris DH, Newton PN, Blacksell SD. Diagnosis of scrub typhus. Am J Trop Med Hyg. 2010;82:368–70. doi: 10.4269/ajtmh.2010.09-0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sonthayanon P, Chierakul W, Wuthiekanun V, Phimda K, Pukrittayakamee S, Day NP, et al. Association of high Orientia tsutsugamushi DNA loads with disease of greater severity in adults with scrub typhus. J Clin Microbiol. 2009;47:430–4. doi: 10.1128/JCM.01927-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim DM, Kang DW, Kim JO, Chung JH, Kim HL, Park CY, et al. Acute renal failure due to acute tubular necrosis caused by direct invasion of Orientia tsutsugamushi. J Clin Microbiol. 2008;46:1548–50. doi: 10.1128/JCM.01040-07. [DOI] [PMC free article] [PubMed] [Google Scholar]


