Abstract
Mycoplasma genitalium is a member of genital mycoplasmas, which is emerging as an important causative agent of sexually transmitted infections both in males and females. The advent of polymerase chain reaction and other molecular methods have made studies on M. genitalium more feasible, which is otherwise a difficult organism to isolate. Besides Chlamydia trachomatis, M. genitalium is now an important and established cause of non gonococcal urethritis (NGU) in men, more so in persistent and recurrent NGU. Multiple studies have also shown a positive association of M. genitalium with mucopurulent cervicitis and vaginal discharge in females as well. The evidences for M. genitalium pelvic inflammatory diseases and infertility are quite convincing and indicate that this organism has potential to cause ascending infection. Lack of clear association with M. genitalium has been reported for bacterial vaginosis and adverse pregnancy outcomes. Diagnosis of M. genitalium infections is performed exclusively using nucleic acid amplification tests (NAATs), owing to poor or slow growth of bacterium in culture. Although there are no guidelines available regarding treatment, macrolide group of antimicrobials appear to be more effective than tetracyclines. The present review provides an overview of the epidemiology, pathogenesis, clinical presentation and management of sexually transmitted infections due to M. genitalium.
Keywords: Emerging infection, Mycoplasma genitalium, non-gonococcal urethritis, sexually transmitted diseases
Introduction
According to the WHO there are an estimated 448 million new cases of sexually transmitted infections (STIs) which are acquired worldwide annually1. If diagnosed in time, these infections can be treated easily with minimal morbidity as well as decreased economic burden. Mycoplasma genitalium is an emerging cause of STIs and has been implicated in urogenital infections of men and women around the world. More than 25 years after its initial isolation from men with non-gonococcal urethritis (NGU)2, M. genitalium is now recognized as an important aetiologic agent of acute and persistent male NGU and is responsible for approximately 20-35 per cent of non-chlamydial NGU cases3,4. The role of this organism in male urogenital disease was a significant advancement in our knowledge of STIs, but its role in the inflammatory reproductive tract diseases of women is still not very clear5.
The risk factors for M. genitalium infection are typical as for any STI. Researchers in various study groups of women and men aged 21-23 yr identified behavioural risk factors for M. genitalium infection6: higher number of partners, younger age during first intercourse, having a partner with infection symptoms, coinfection with other sexually transmitted pathogens like Chlamydia trachomatis6. Manhart et al7 showed that the prevalence of M. genitalium increased by 10 per cent for every additional sexual partner. Asymptomatic carrier state7 is also a serious epidemiological problem because of transmission to sexual partners and may be vertical transmission from mother to the newborn. Some investigators have reported infection as common as chlamydial infection and trichomoniasis, and more common than gonorrhoea8,9.
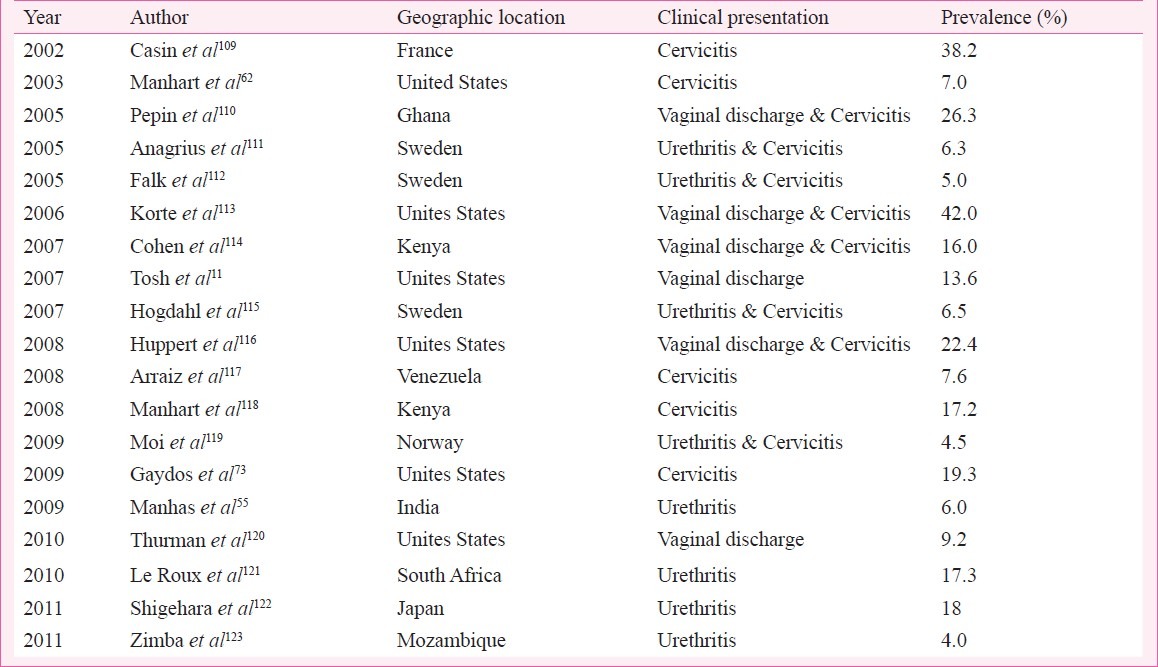
In studies conducted in Denmark, the prevalence of infection was 2.3 and 1.1 per cent in women and men, respectively9. Takahashi et al10 demonstrated the positivity rate of M. genitalium DNA in urine from asymptomatic healthy young Japanese men as 1 per cent; among female students in Japan the prevalence of M. genitalium was 2.8 per cent6. Tosh et al showed high prevalence rate of 13.6 per cent in young (14-17 yr of age) sexually active women who tested positive for M. genitalium11. Among women and men reporting to an STD clinic in Seattle, M. genitalium was detected in 14 and 9 per cent cases, respectively12. Table gives a chronological account of important studies reporting geographic prevalence of M. genitalium.
Table.
Chronological account of important representative studies reporting geographic prevalence of M. genitalium
Taxanomy and general characteristics
Mycoplasma (Latin: fungus form) belongs to class Mollicutes (Latin: soft skin). Despite the lack of a cell wall, many taxonomists have classified Mycoplasma and relatives in the phylum Firmicutes, consisting of low G+C Gram-positive bacteria such as Clostridium, Lactobacillus, and Streptococcus based on 16S rRNA gene analysis. The order Mycoplasmatales contains a single family, Mycoplasmataceae, comprising two genera: Mycoplasma and Ureaplasma. These are amongst the smallest free living microorganisms capable of self-replication. M. genitalium is one out of the so far 15 named mycoplasma species of human origin13. In 1981, two mycoplasma strains, G-37 and M-30 were first isolated from two men with nongonococcal urethritis (NGU)2,14. Later in 1983 these were named as M. genitalium, the twelfth mycoplasma species recovered from humans15.
The genus Mycoplasma contains very small bacteria, with sizes ranging from 0.2 to 0.7 μm. The shape depends on the particular mycoplasma species which may vary from spherical, filamentous or flask/pear-like. M. genitalium is a motile flask-shaped mycoplasma with terminal tip-like structure which assists in attachment to various surfaces and provides gliding motility. It does not have a peptidoglycan cell wall and, therefore, lacks cell surface markers. The absence of a cell wall also means that this bacterium has less osmotic stability in the host environment. Lack of a cell wall is responsible for a negative Gram stain reaction and non-susceptibility to β-lactam antibiotics that inhibit bacterial cell wall synthesis16. As M. genitalium is too small to be visible singly under a light microscope, the first detailed study of its structure was conducted under a transmission electron microscope (TEM)16. These organisms are difficult to culture and it may take from a few weeks to a few months before a culture shows visible growth. The mycoplasmas penetrate the surface of the agar and grow in the underlying medium through deposition of manganese dioxide (MnO2). The colonies appear brown and have a typical “fried egg” appearance (size: 200-400 μm): a dense, dark, granulated nucleus, bordered by a thin, light zone2,17.
GENOME
In 1995 M. genitalium complete genome sequence was published making it the second bacterium after Haemophilus influenzae to have its genome fully sequenced18. It is the species with the smallest genome of all mycoplasmas studied so far with a genome of only 580 kb. Although most mycoplasma genomes have a low guanine plus cytosine (G+C) content, with the range of 24-33 per cent G+C, the M. genitalium genome has a comparatively higher G+C content of 32 per cent18. The small genome of M. genitalium made it the organism of choice in ‘The Minimal Genome Project’, a study to find the smallest set of genetic material necessary to sustain life19.
PATHOGENESIS
The pathogenesis of M. pneumoniae has been studied extensively and due to the close genetic resemblance, certain features in the pathogenesis of M. pneumoniae can be applied to M. genitalium. Though M. pneumoniae is primarily found in the respiratory tract, and M. genitalium in the urogenital tract, both organisms have been shown to cross tissue barriers. M. genitalium has been shown to attach to different cell types, including erythrocytes, Vero cells, fallopian tube cells, respiratory cells and spermatozoa13,20.
M. genitalium has several virulence factors that are responsible for its pathogenicity. These include the ability to adhere to host epithelial cells using the terminal tip organelle with its adhesins, intracellular localization, the release of enzymes and the ability to evade the host immune response by antigenic variation. M. genitalium lipid-associated membrane proteins (LAMPs) play an important role in the genito-urinary tract inflammatory reaction20. Although mycoplasmas are shown to produce hydrogen peroxide and superoxide metabolites, much of the tissue damage is related to the host cell responses. The stimulation and suppression of cells (including lymphocytes, monocytes, macrophages) through induction of cytokine production (mainly TNF- α, IL-1α, IL-1β, IL-6, IL-8 and IL-10) have significant role in pathogenesis. Some of the mycoplasmal cell components can also act as superantigens
(i) Adhesion to host epithelium - For any Mollicute to colonize and cause infection, adhesion is the first prerequisite. Mycoplasmas are primarily considered surface parasites of mucous membrane cells as these adhere tenaciously to the epithelial linings of the respiratory or urogenital tract, rarely invading tissues. The urogenital tract appears to be the primary tissue infected by M. genitalium, but the adherence does not appear to be restricted to uroepithelial cells in vitro13. Adhesin molecules, clustered at the tip structure of the flask shaped polar cell have been intensely studied both in M. genitalium and M. pneumoniae21. Both species attach to erythrocytes from a variety of species, eukaryotic cells, such as Vero cells, but more importantly M. genitalium binds to the epithelial cells of human fallopian tubes13.
Twenty one different putative protein genes have been identified in the M. genitalium genome, but only a few have been characterised as adhesions. The major adhesin in the attachment protein complex is the MgPa protein22,23 and, collectively with the P32 (MG318)24 protein, makes up the terminal tip organelle. The MgPa encodes the P140 (MG191) and P110 (MG192) cytadherence proteins (cytadhesins) at the tip area13. These proteins are immunogenic both in experimental animals as well as in humans. Loss of either of these two proteins results in loss of motility and adherence properties of the entire MgPa attachment organelle25, thus showing the importance of these proteins in attachment. It has been shown that the 140 kDa P140 (MG191) is related to the 170 kDa main adhesion protein (P1) of M. pneumoniae whereas the 32 kDa M. genitalium protein P32 (MG318) closely resembles P30 of M. pneumoniae26.
The MG218 and MG317 cytoskeletal proteins were shown to have a role in terminal organelle organisation, gliding motility and cytodherence. The genes encoding the adherence proteins are located in three different regions of the M. genitalium genome. The genes coding for the MgPa adhesins are organised in an operon with three genes22,23. The P32 (MG318) of M. genitalium adherence components found on the tip-like terminal structures is located in operons that are a distance away from the MgPa operon. The accessory proteins and their analogues in M. genitalium are important for clustering of the adhesin at the tip and maintaining the tip of the organism and the shape of the cell, thereby acting like a cytoskeleton. MG218 is grouped in an operon with MG217 and MG21913.
(ii) Intracellular localization - From the very beginning of mycoplasma study2,15, the controversy regarding the surface versus intracellular location of mycoplasma remains. Although the intracellular location of some of the Mycoplasma spp, e.g. M. penetrans, M. fermentans and M. hominis was successfully proved27,29, the same about M. genitalium is not clear. Though various studies30,32 have been conducted regarding location of M. genitalium, any conclusion is yet to be arrived. It appears that M. genitalium behaves like a facultative intracellular pathogen i.e. capable of retaining viability both extracellularly and intracellularly in vitro13. Whether the same occurs in vivo has not been proven. However, from clinical experience with patients receiving multiple courses of highly active antibiotic treatment with temporary improvement but subsequent relapse, it seems likely that such mechanisms may act in at least in a subset of patients13.
(iii) Antigenic variation - Mycoplasmas, in order to evade host immune response, show antigenic variation of their surface components. Surface lipoproteins of mycoplasmas show antigenic variation and over generations these have evolved to generate higher frequency of phenotypic heterogeneity even in a small population of these organisms. Other mechanisms such as mimicry of host antigens may also assist in their survival within the host cells33,34.
There are two basic mechanisms for this. Either the organism controls the expression of the virulence factors molecules in accordance to the environmental changes through a signal transduction pathway or the organism may spontaneously generate mutant phenotypes which survive the changes in their environment i.e. host cell responses33. In order to evade the host immune system, proteins P140 and P110 of the MgPa have the capacity to undergo antigenic variation, thus changing the genetic sequence of the MgPa with subsequent production of variants that are not recognised by the host immune system13,35. Other survival mechanisms of this organism may be the ability to mimic host cell antigens and the intracellular location within professional macrophages13.
Tissue damage observed in M. pneumoniae infections is due to the host cell response and this may indicate what occurs during in M. genitalium infections. Mycoplasmas interact with many components of the immune system, which may lead to production of cytokines and macrophage activation. Some cell components may also act as super antigens and induce a hightened autoimmune response36.
(iv) Enzymes - Alvarez et al37 found that in the glycolytic pathway, the activity of the glycolysis enzyme glyceraldehyde 3-phosphate dehydrogenase (GAPDH) brings about attachment of M. genitalium to human vaginal and cervical mucin in female. Thus GAPDH acts as a ligand to receptors mucin and fibronectin, particularly in vaginal and cervical disease. M. genitalium translocates its cytoplasmic enzymes to the cell membrane surfaces to enhance host tissue colonization38. In addition, methionine sulphoxide reductase (MsrA) can be released to enhance the pathogenicity of its small genome39. MsrA is an antioxidant repair enzyme of the bacterium. It restores proteins that have lost their biological activity due to the oxidation of their methionines, thereby protecting the bacterium protein structure from the host oxidative damage39. The Figure shows a flow diagram depicting the pathogenesis in M. genitalium.
Fig.
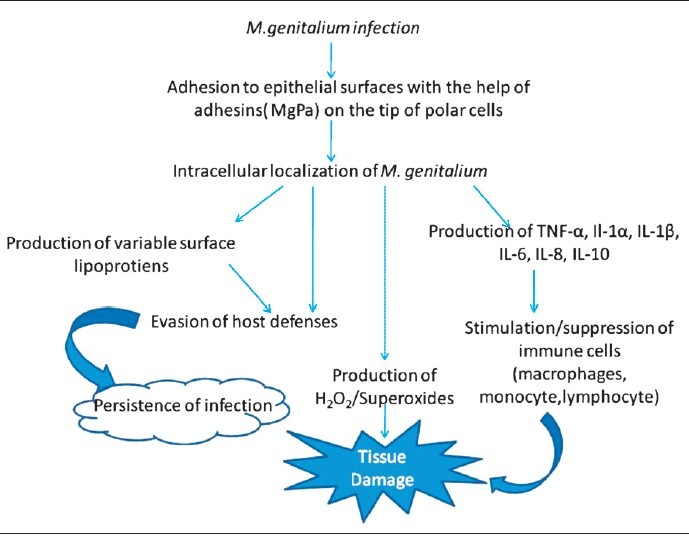
An overview of the pathogenic mechanisms of M. genitalium
INFECTIONS IN HUMANS
(A) Urogenital infection in men - Urethritis, which is a common sexually transmitted disease (STD) in heterosexual men, is classified as gonococcal or non-gonococcal depending on the presence or absence of Neisseria gonorrhoeae3. In approximately 30 per cent of the patients with NGU, neither a bacterial nor a mycoplasmal agent is recovered on usual laboratory medium but some in whom a pathogenic microorganism cannot be identified, respond to treatment with antimicrobial agents that are active against C. trachomatis or U. urealyticum40,41. These observations imply that other more fastidious mycoplasmas or other microorganisms susceptible to antimicrobial agents, such as tetracycline, macrolides and fluoroquinolones may be involved in NGU3. Due to difficulties in culturing M. genitalium, only a few epidemiological studies have been conducted after the discovery of the organism. Since DNA probe42 and PCR assays43 were developed for detecting M. genitalium, this mycoplasma has now been detected more often in patients with acute NGU than in those without urethritis44. It has been shown to cause urethritis in subhuman primates inoculated intraurethrally45,46.
The results of many studies tend to indicate that M. genitalium can cause NGU. According to these data M. genitalium is detectable in 14.147 to 33.3 per cent48 of men with acute NGU recruited at STD clinics4,44,48–52 and in 13.251 to 15.6 per cent54 of those at urology clinics. An earlier study from our centre showed that M. genitalium was detected in 6 per cent (6/100) of NGU cases. The infection rate was 7.1 per cent (5 of 70) among the HIV positive individuals whereas only one HIV negative NGU case was found to be positive (3.3%). The association of M. genitalium was independent of the presence of C. trachomatis and U. urealyticum55. The prevalence of this mycoplasma in men without urethritis who attended STD clinics is 0.8 to 9.1 per cent4,44,48,50–52, whereas that in asymptomatic men who attended urology clinic is 0 to 2 per cent53,54. Thus, most studies document that M. genitalium is evident significantly more often in patients with acute NGU than in controls without urethritis. Further, the prevalence of M. genitalium is 18.4 to 45.5 per cent in patients with acute nonchlamydial nongonococcal urethritis (NCNGU) and in most studies the prevalence is significantly higher than that in patients with acute chlamydia positive NGU or without urethritis regardless of whether they were recruited at STD or urology clinics4,44,51,53,54. The prevalence of M. genitalium in men with gonococcal urethritis is likely to be lower than that of C. trachomatis3. Most patients with NGU associated with C. trachomatis or U. urealyticum respond to antibiotic therapy. However, when neither organism is detected, NGU sometimes persists or recurs within 6 wk of treatment56,57. Various studies show that M. genitalium may have a significant role in persistent or recurrent NGU5,52,58. It has been detected in the prostate of about 4 per cent of the patients with chronic abacterial prostatitis59 but there is currently insufficient evidence to suggest that it could be an important cause of the disease60.
(B) Urogenital infections in women - Compared to the number of studies in men, only a few studies on the role of M. genitalium in women have been conducted5.
(i) Cervicitis - A few studies have addressed the correlation between M. genitalium infection and cervicitis. One of the major problems in interpreting these studies has been the varying definitions of cervicitis. Some studies have considered the presence of 10 polymorphonuclear lymphocytes (PMNLs)/high power field (hpf) in a cervical smear significant, whereas others considered 30 PMNLs/hpf to define cervicitis13. One early study by Uno et al59 defined cervicitis by endocervical discharge and > 20 PMNL/hpf and detected M. genitalium in 5 of 64 women as compared to none of 80 asymptomatic pregnant women61. In a US study using archived cervical secretions from 719 women collected on filter paper, it was found that M. genitalium was strongly associated with cervicitis being detected in 7 per cent of all the women examined but in 11 per cent of women with cervicitis (> 30 PMNLs/hpf) and in 5 per cent of women without cervicitis60. In a multivariate logistic regression analysis correcting for other factors found to be associated with cervicitis, and excluding the 172 women infected with N. gonorrohoeae and/or C. trachomatis, M. genitalium remained strongly associated with cervicitis (OR 3.1; 95% CI 1.5-6.8), further supporting an independent role for M. genitalium as a cause of cervicitis. The attributable risk per cent was 70 per cent, suggesting that among women with cervicitis and M. genitalium, 70 per cent of cervicitis can be attributed to M. genitalium62.
(ii) Pelvic inflammatory diseases (PID) - PID is the clinical syndrome caused by the spread of microorganisms from the lower to the upper genital tract. Several bacteria including those found in bacterial vaginosis, C. trachomatis, and N. gonorrhoeae can cause PID. Establishing a connection between M. genitalium and upper genital tract infection is of major importance in determining the significance of the infection13. Earlier studies relying on serology have been controversial. In a study of 115 women presenting to an STD clinic in Kenya with acute pelvic pain, plasma cell endometritis was found in 58 and M. genitalium was detected in cervical swabs or endometrial biopsies in 16 per cent compared to only 2 per cent of women without endometritis63. As many as 33 per cent of the women studied were HIV positive, but M. genitalium was not detected more often in the HIV infected women. In another study on women with clinically suspected PID64, M. genitalium was detected more often in HIV positive women (19 vs 5%). In a case-control study, Simms and colleagues65 examined 45 women with clinically diagnosed PID and found M. genitalium DNA by PCR in endocervical swabs from nine (16%) as compared to none of 37 control patients.
(iii) Bacterial vaginosis (BV) - Although in one of the early reports, M. genitalium was found in 4 (16%) of 25 unselected women and in 3 of 10 women with BV66, subsequent studies showed lack of association of M. genitalium with BV. Keane et al67 studied 15 women with BV, none of whom was M. genitalium positive, as were only 2 (12%) of 17 women without BV attending an STD clinic. Thus, unlike M. hominis, M. genitalium probably is not associated with BV17.
(iv) Adverse pregnancy outcome and infertility - There is little information available on the role of M. genitalium in causing adverse pregnancy outcome, either as preterm labour, abortion or stillbirth. In one study M. genitalium was detected in only 4 per cent of mid-trimester vaginal swabs from 124 women delivering preterm68. This is probably slightly higher than the prevalence in a normal population of pregnant women as estimated in another study69 where only 0.7 per cent of women pregnant in the first trimester were M. genitalium positive. Regarding infertility, only indirect evidence has been presented. In a Danish study70, serum samples from 308 infertile women were investigated for antibodies to M. genitalium by immunoblotting against whole cell proteins of M. genitalium and M. pneumoniae as well as against a recombinant MgPa antigen. Among the women with tubal factor infertility, 22 per cent were seropositive as compared to 7 per cent of women with either male factor infertility or unexplained infertility with normal tubes.
The results of animal experiments offer substantial evidence for the pathogenicity of M. genitalium for the urogenital tract of subhuman primates and the agent is sexually transmitted between partners13. It seems reasonable to conclude, that M. genitalium can cause mucopurulent cervicitis although the demonstration of an antibody response is lacking. M. genitalium is sexually transmissible with transmission rates similar to those of C. trachomatis13. The role of M. genitalium in women is less well established than in men, and further studies are needed to address its relation to PID and late sequelae such as infertility. Only indirect evidence exists for infertility, and BV and adverse outcome of pregnancy does not appear to be associated with M. genitalium infection. As in men, randomised controlled clinical trials aiming at determining the optimal treatment of the infection are needed.
Association of M. genitalium with other STDs
As the mode of transmission is common amongst all sexually transmitted infections, co-infection of M. genitalium with other pathogens has been observed by many authors. In a study by Yokoi et al71, rates of co-infection with M. genitalium among men with gonococcal urethritis were shown to be low (4.1%), compared with the C. trachomatis co-infection rate (21.2%). In another study, when 45 males with gonococcal urethritis were simultaneously screened for M. genitalium using PCR, 4.4 per cent showed positivity72. Gaydos et al73 while conducting studies on STIs in male attending STD clinics showed 5.9 per cent of them to be co-infected with C. trachomatis. In West Africa, Pepin et al74 showed that almost half of the infections due to M. genitalium occurred as co-infections. The prevalence of co-infection with gonococcal urethritis, C. trachomatis and Trichomonas vaginalis was 37.9, 10.6 and 7.6 per cent, respectively74. Co-infections amongst genital mycoplasmas have also been reported. In a study by Amirmozafari et al75 simultaneous occurrence of M. genitalium and U. urealyticum was shown in 1.4 per cent of women with genital infections, while triple infection of M. genitalium, U. urealyticum and M. hominis was seen in 0.5 per cent of these patients. Other authors have also demonstrated co-existence of M. genitalium with other pathogens76,77.
ANIMAL MODELS
Animal studies are useful to establish the transmissibility of M. genitalium in human. Although there are severe limitations of urogenital studies in animals, till now chimpanzees are considered the best animal models for studying male urethritis caused by M. genitalium13. Intraurethral inoculation of M. genitalium in male chimpanzees has been shown to lead to infection in them and the organisms were isolated from blood in some cases45,46. Animal studies of female M. genitalium infections have been more rewarding than those performed in male animals. Lower primates like rhesus and cynomolgus monkeys have decreased susceptibility to infection13. Studies performed in men with NGU and their female partners showed that M. genitalium was transmitted sexually as efficiently as C. trachomatis, which has been studied in more details48,78,79. Based on both the concordance rates among partners and on DNA typing showing the same sequence type among partners, it is beyond doubt that M. genitalium is a sexually transmitted pathogen80, but further studies are required to confirm.
DIAGNOSIS
Mycoplasma identification and laboratory diagnosis of mycoplasmal infections has been based on classical bacteriological tests including morphology, cultural characteristics, physiological and serological properties. New tests based on molecular analysis of genomic DNA, ribosomal RNAs, cell proteins and lipids appear to push aside the classical tests and one may expect that the molecular tests will shortly become the prevailing tests in mycoplasma identification17.
(i) Sample collection
Specimens appropriate for the detection for M. genitalium by culture or non-cultural methods include urethral swab, urine, endocervical swab and endometrial biopsy. Calcium alginate, Dacron or polyester swabs with aluminium or plastic shafts are preferred. Wooden-shaft cotton swabs should be avoided because of potential inhibitory effect. Swabs should always be removed from specimens before transportation to the laboratory81. Specimens should be inoculated at the bedside whenever possible by using appropriate transport and/or culture media. SP4 is considered to be a good transport as well as culture medium for M. genitalium. If immediate transportation to the laboratory is not possible, specimens should be refrigerated, but not beyond 24 h. Mollicutes can be stored for long periods in appropriate growth and transport medium at -80°C or in liquid nitrogen. Storage at -20°C is deleterious to detection, even by non-culture methods. Mycoplasmas of human origin can be undertaken on the laboratory bench and/or in a class 2 safety cabinet81.
(ii) Staining and Culture techniques
Direct detection of M. genitalium in the samples with the help of different staining techniques is nearly impossible due to their small size and lack of a cell wall. However, DNA fluorochromes like Hoechst 33258 or acridine orange stain may be applied to body fluids after centrifugation. M. genitalium grows slowly with the prototype strain G37 producing colonies in 6 wk or more82. After initial isolation of two M. genitalium strains in 1981, no subsequent isolate was recovered from the genital tract until 1996, when Jensen et al83 reported isolation of the organism on agar using tissue culture as an enrichment culture for eventual growth on Friis medium.
Sucrose phosphate based culture medium (SP4) played a major role in the discovery of M. genitalium. This medium designed to isolate mycoplasmas and spiroplasmas was developed by Tully et al2 at the National Institutes of Health (NIH), Maryland, USA, and consisted of mycoplasma broth base supplemented with glutamine, yeast extract, bovine serum, penicillin and phenol red as the indicator. Evidence of mycoplasmal growth was an increase in turbidity as well as the acidic pH change from red to yellow of the phenol red indicator, due to glucose fermentation by the organism84. The layer of cells adhering to the container surface was scraped off to inoculate a solid agar medium (0.6% agarose or 0.8% Noble agar in broth base) before anaerobic incubation at 37˚C. Signs of growth in the medium occurred very slowly; with a colour change only occurring after 50 days.
Another medium is the (Pleuro Pneumonia like Organisms) PPLO broth which has been extensively used for the culture of M. genitalium. It can also be used for transport of urethral swabs. The procedure can be made selective for mycoplasmas by filtering the sample through 0.45 μm syringe filter. The tubes are incubated in 5 per cent CO2 and observed thrice daily for any colour change till 15 days. As soon as the colour change to red-pink is seen in the absence of any turbidity of the medium, the growth is subcultured to corresponding PPLO agar plates. PPLO agar plates are incubated at 37°C with 5 per cent CO2 for 15 days. The plates are observed daily under the microscope for any growth till 15 days. Once the colonies appeared, the organism is identified according to standard biochemical methods and staining by Dienes and Giemsa stains as per the standard methods81. The shape of the colonies is like other mycoplasmas but not typically ‘fried egg’.
Considering the susceptibility of cultured cells to mycoplasma infection with a variety of reported species, and also with the knowledge of propagation of fastidious strains of M. hyorhinis in cell cultures85, attempts were made to grow M. genitalium in cell cultures (e.g. Vero cell lines)83. This approach proved to be very efficient but extremely time-consuming13. As there is no reliable medium for the direct isolation of M. genitalium, detection is carried out by PCR. Nevertheless, culture is important for obtaining organisms for susceptibility testing and is a topic of continuing research.
(iii) Serodiagnosis
The classical recommended tests include growth and metabolic inhibition by specific antiserum, as well as direct and indirect immunofluorescence tests applied to mycoplasma colonies. In some cases more sensitive tests based on principles of ELISA, immunobinding, immunoblotting, immunofluorescence and immunoperoxidase test have been applied to mycoplasma diagnosis. The cross-reactions between M. pneumoniae and M. genitalium have significantly hampered the use of specific serology for diagnosis and epidemiological studies17. Till date, no serologic test for genital mycoplasmas have been standardized and made commercially available for diagnostic use.
(iv) DNA probes and PCR
Before the development of PCR methods, a few attempts were made using DNA probes. The design of radiolabelled oligonucleotide probes targeting the 16S rRNA was reported to have a detection limit of approximately 1000 organisms86 and could be tailored to detect only M. genitalium. Clinical studies using such probes have not been reported, but actually, the sequence information from this study was used in one of the first publications on PCR for M. pneumoniae87. Risi et al88 used a cloned 256 bp fragment of unknown function to probe simulated female genital tract specimen and found a detection limit of approximately 10,000 genome copies. A whole-genomic, nick-translated probe with a reported detection limit of 104 to 105 genome copies was also used to study urethral specimens from 203 men89. No evidence suggesting an important role of M. genitalium in acute NGU was found, but men with recurrent NGU were more often positive. Considering that a high proportion of the patients have a very low DNA load in urogenital specimens90, it is surprising that Hooton et al89 found an overall rate of 15 per cent M. genitalium positive in their study. Highly sensitive assays are needed for detection of M. genitalium with a high clinical sensitivity. At present, only nucleic acid amplification tests (NAATs) offer the sensitivity needed and only PCR based assays have been reported so far5,82.
The first PCR based test was published in 199143 and shortly after, Palmer and colleagues64 published their method. Both were based on the MgPa DNA sequence. At that time, it was believed that an adhesin gene would be rather conserved, since it has an important role in the pathogenesis of the infection. It was, therefore, surprising that the region of MgPa flanked by the MgPa-1 and MgPa-3 primers43 appeared to be variable. Different other sequence variants were found by restriction enzyme analysis, and later by sequencing90. This observation led to further studies into the genetic variability of M. genitalium91 and to the need for alternative PCR assays92,93. The assay developed by Palmer et al94 was a hemi-nested PCR. The experience with the MgPa-476/MgPa-903 primer-set provided further impetus to develop an assay based on the 16S rRNA gene93. One of the more recent developments in diagnostic PCR is the homogeneous real-time PCR. The first real-time PCR assay for M. genitalium was developed by Yoshida et al in 200295. The assay was based on detection of the 16S rRNA gene. Subsequently, a LightCycler assay detecting the P115 gene (MG299) with LNA (locked nucleic acid) probes was applied for detection of M. genitalium and for monitoring the response to treatment in nine infected men96.
Research workers have noted the unreliability of immunological assays and some PCR tests used for detection of M. genitalium97, probably related to the extensive antigenic recombination characterized in genomic studies98. Several assays testing first void urine (FVU) and self-collected vaginal swabs have some evidence-based utility (sensitivity or specificity >95%) for detection of M. genitalium and these include multi-target real-time PCR, Gen-Probe (Gen-Probe, San Diego, CA, USA) transcription-mediated amplification research assay (GPTMARA), real-time PCR (RTPCR), MPCR Reverse Line Blot (MPCRRLB), LightCycler real- time PCR (LCRTPCR) (Roche Applied Science, Indianapolis, IN, USA) and TaqMan® real-time PCR99. In the absence of a ‘gold standard’ assay, local availability may govern the choice of assay used. Vaginal swabs reportedly have high sensitivity for detecting M. genitalium12. Presently, there is a reasonable amount of information that supports the utility of MgPa, regardless of its potential variability, as a NAAT target.
TREATMENT
Mycoplasmas including M. genitalium are normally susceptible to tetracyclines and fluoroquinolones100 but resistant to those that act on bacterial cell wall components, e.g. β-lactams due to lack of cell wall. Due to difficulty in isolating M. genitalium from clinical samples, only a few reports exist of the minimum inhibitory concentration (MIC) of various antibiotics. These MICs were determined only for a few isolates of M. genitalium that were established and maintained in the laboratory. The antimicrobial susceptibility profile of such isolates may not precisely confirm that of current clinical isolates of M. genitalium. However, these studies provide some useful information, when antimicrobial agents were chosen to treat M. genitalium infection. Data from these studies indicate that the in vitro antimicrobial susceptibility profile of M. genitalium is similar to that of M. pneumoniae101. Tetracycline, erythromycin and some newer macrolides, such as clarithromycin and azithromycin, are highly active against M. genitalium101–105. The MIC of tetracycline, including doxycycline and minocycline, for M. genitalium is 0.01 to 0.05 μg/ml101. Information on tetracycline resistance in M. genitalium does not exist, but M. genitalium-positive men with NGU and women with cervicitis may respond better to azithromycin than they to a tetracycline, possibly because of lower MICs. The MIC of erythromycin and the newer macrolides is 0.01 μg/ml or less101. Telithromycin, which is a member of the newest macrolide derivatives called ketolides, is also highly active against M. genitalium with a MIC of 0.015 μg/ml or less102. Some newer quinolones are highly active. For example, the reported MIC is 0.06 to 0.12 μg/ml for sparfloxacin, 0.06 to 0.12 μg/ml for grepafloxacin, 0.05 μg/ml for gemifloxacin and 0.03 to 0.06 μg/ml for trovafloxacin103–105. However, ofloxacin and ciprofloxacin show only moderate activity at 0.5 to 1 and 2 μg/ml, respectively101,102. Till now no universally accepted standards are established for pH, medium, incubation conditions, or duration of incubation for performing mycoplasmal susceptibility test. No MIC breakpoints specific for these organisms are endorsed by any regulatory agency.
Till date, there are no published guidelines or recommendations for treating M. genitalium positive urethritis. Only a few results of antimicrobial chemotherapy in men with M. genitalium positive urethritis have been reported44,50,52,58. In addition, these studies have some limitations, such as a small number of patients and no detection of other potentially important genital mycoplasmas or other types of organisms. Therefore, it is impossible to draw conclusions on the best strategy for managing M. genitalium positive nongonococcal urethritis3. As a specific microbiological diagnosis of mycoplasmal infection is seldom made, appropriate treatment provides antimicrobial coverage for the organisms that cause the particular syndrome. Accordingly NGU is treated with doxycycline (100 mg orally twice a day for 7 days) or azithromycin (1.0 gm as a single oral dose) to provide activity against C. trachomatis, U. urealyticum and M. genitalium106. Gambini et al50 observed that doxycycline treatment resulted in symptom alleviation and microbiological cure of infection in 94.3 per cent patients with M. genitalium positive nongonococcal urethritis. In NGU cases persistent M. genitalium in the urethra is associated with recurrent NGU. Thus, in patients with M. genitalium induced NGU a longer course of antibiotic treatment may be recommended as recommended a 2 or 3 wk course of antibiotic treatment in case of M. pneumoniae pneumonia3. The slow growth M. genitalium, and its ability to invade and multiply in the epithelial cells might account for its persistence in urethra or other sites, specially following treatment60. M. genitalium was found in some patients with chronic NGU who had been treated originally with doxycycline (100 mg/day for 10 days), and a 6 wk course of erythromycin (500 mg QDS)107. Others are found M. genitalium persisting in some patients with acute NGU after treatment with doxycycline (200 mg followed by 100 mg for 13 days) or erythromycin108, or after treatment with tetracycline (500 mg BD for 10 days)58 or after treatment with levofloxacin (100 mg TDS for 14 days)58. In one study an azithromycin regimen comprising 500 mg in a single dose on day 1 followed by 250 mg OD for 4 days provided excellent cure rates60. Further studies are needed to determine the most appropriate treatment for M. genitalium positive acute and chronic NGU and other M. genitalium-associated infections.
Conclusion
M. genitalium is one of the smallest prokaryote capable of replication, lacks a cell wall and has a characteristic pear/flask shape with a terminal tip organelle. M. genitalium has several virulence factors that are responsible for its pathogenicity. The latter includes its ability to adhere to host epithelial cells using the terminal tip organelle with its adhesins, the release of enzymes and the ability to evade the host immune response by antigenic variation. M. genitalium has emerged as an important cause of sexually transmitted infections in recent times and it is now known as established cause of non gonococcal uretheritis (NGU) in men. It is reasonable to conclude that it is strongly associated with mucopurulent cervicitis in women. The evidence for M. genitalium PID and infertility are quite convincing and indicate that this organism has potential to cause ascending infection but more studies are needed to understand the relationship between M. genitalium and reproductive tract disease in women. Further research is required to understand the dynamics of HIV and M. genitalium co-infections. Though there are variety of in-house PCRs which have been developed for diagnosing the M. genitalium infections, there is a need of highly accurate internationally validated and approved commercial NAAT. All the present evidences support the use of azithromycin as first drug of choice for M. genitalium infections. In conclusion, M. genitalium is an important cause of sexually transmitted infections in both men and women and should be treated with azithromycin when required.123
References
- 1.World Health Organization. Sexually transmitted infections fact sheet. 2011. [accessed on August 25, 2011]. Available from: http://www.who.int/mediacentre/factsheets/fs110/en/
- 2.Tully JG, Taylor-Robinson D, Cole RM, Rose DL. A newly discovered mycoplasma in the human urogenital tract. Lancet. 1981;1:1288–91. doi: 10.1016/s0140-6736(81)92461-2. [DOI] [PubMed] [Google Scholar]
- 3.Deguchi T, Maeda S. Mycoplasma genitalium: another important pathogen of nongonococcal urethritis. J Urol. 2002;167:1210–7. doi: 10.1016/s0022-5347(05)65268-8. [DOI] [PubMed] [Google Scholar]
- 4.Totten PA, Schwartz MA, Sjostrom KE, Kenny GE, Handsfield HH, Weiss JB, et al. Association of Mycoplasma genitalium with nongonococcal urethritis in heterosexual men. J Infect Dis. 2001;183:269–76. doi: 10.1086/317942. [DOI] [PubMed] [Google Scholar]
- 5.McGowin CL, Anderson-Smits C. Mycoplasma genitalium: an emerging cause of sexually transmitted disease in women. PLoS Pathog. 2011;7:e1001324. doi: 10.1371/journal.ppat.1001324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamasuna R, Imai H, Tsukino H, Jensen JS, Osada Y. Prevalence of Mycoplasma genitalium among female students in vocational schools in Japan. Sex Transm Infect. 2008;84:303–5. doi: 10.1136/sti.2007.028670. [DOI] [PubMed] [Google Scholar]
- 7.Manhart LE, Holmes KK, Hughes JP, Houston LS, Totten PA. Mycoplasma genitalium among young adults in the United States: an emerging sexually transmitted infection. Am J Public Health. 2007;97:1118–25. doi: 10.2105/AJPH.2005.074062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu JT, Tang WY, Lau KH, Chong LY, Lo KK. Asymptomatic urethral infection in male sexually transmitted disease clinic attendees. Int J STD AIDS. 2008;19:155–8. doi: 10.1258/ijsa.2007.007199. [DOI] [PubMed] [Google Scholar]
- 9.Andersen B, Sokolowski I, Ostergaard L, Kjolseth Moller J, Olesen F, Jensen JS. Mycoplasma genitalium: prevalence and behavioural risk factors in the general population. Sex Transm Infect. 2007;83:237–41. doi: 10.1136/sti.2006.022970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takahashi S, Takeyama K, Miyamoto S, Ichihara K, Maeda T, Kunishima Y, et al. Detection of Mycoplasma genitalium, Mycoplasma hominis, Ureaplasma urealyticum, and Ureaplasma parvum DNAs in urine from asymptomatic healthy young Japanese men. J Infect Chemother. 2006;12:269–71. doi: 10.1007/s10156-006-0462-y. [DOI] [PubMed] [Google Scholar]
- 11.Tosh AK, Van Der Pol B, Fortenberry JD, Williams JA, Katz BP, Batteiger BE, et al. Mycoplasma genitalium among adolescent women and their partners. J Adolesc Health. 2007;40:412–7. doi: 10.1016/j.jadohealth.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wroblewski JK, Manhart LE, Dickey KA, Hudspeth MK, Totten PA. Comparison of transcription-mediated amplification and PCR assay results for various genital specimen types for detection of Mycoplasma genitalium. J Clin Microbiol. 2006;44:3306–12. doi: 10.1128/JCM.00553-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jensen JS. Mycoplasma genitalium infections. Diagnosis, clinical aspects, and pathogenesis. Dan Med Bull. 2006;53:1–27. [PubMed] [Google Scholar]
- 14.Taylor-Robinson D, Tully JG, Furr PM, Cole RM, Rose DL, Hanna NF. Urogenital mycoplasma infections of man: a review with observations on a recently discovered mycoplasma. Isr J Med Sci. 1981;17:524–30. [PubMed] [Google Scholar]
- 15.Tully JG, Taylor-Robinson D, Rose DL, Cole RM, Bove JM. Mycoplasma genitalium, a new species from the human urogenital Tract. Int J Syst Bacteriol. 1983;33:387–96. [Google Scholar]
- 16.Taylor-Robinson D. The Harrison Lecture. The history and role of Mycoplasma genitalium in sexually transmitted diseases. Genitourin Med. 1995;71:1–8. doi: 10.1136/sti.71.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Razin S. Mycoplasma. In: Boricello SP, Murray PR, Funke G, editors. Topley & Wilson's microbiology & microbial infections. 10th ed. London: Hodder Arnold; 2005. pp. 1957–2005. [Google Scholar]
- 18.Fraser CM, Gocayne JD, White O, Adams MD, Clayton RA, Fleischmann RD, et al. The minimal gene complement of Mycoplasma genitalium. Science. 1995;270:397–403. doi: 10.1126/science.270.5235.397. [DOI] [PubMed] [Google Scholar]
- 19.Pace H. Playing God with Synthetic Life? Starting with the minimal genome project. The Triple Helix Easter. 2009:8–9. [Google Scholar]
- 20.Ekiel A, Jozwiak J, Martirosian G. Mycoplasma genitalium: a significant urogenital pathogen? Med Sci Monit. 2009;15:RA102–6. [PubMed] [Google Scholar]
- 21.Razin S, Jacobs E. Mycoplasma adhesion. J Gen Microbiol. 1992;138:407–22. doi: 10.1099/00221287-138-3-407. [DOI] [PubMed] [Google Scholar]
- 22.Inamine JM, Loechel S, Hu PC. Analysis of the nucleotide sequence of the P1 operon of Mycoplasma pneumoniae. Gene. 1988;73:175–83. doi: 10.1016/0378-1119(88)90323-x. [DOI] [PubMed] [Google Scholar]
- 23.Inamine JM, Loechel S, Collier AM, Barile MF, Hu PC. Nucleotide sequence of the MgPa (mgp) operon of Mycoplasma genitalium and comparison to the P1 (mpp) operon of Mycoplasma pneumoniae. Gene. 1989;82:259–67. doi: 10.1016/0378-1119(89)90051-6. [DOI] [PubMed] [Google Scholar]
- 24.Reddy SP, Rasmussen WG, Baseman JB. Molecular cloning and characterization of an adherence-related operon of Mycoplasma genitalium. J Bacteriol. 1995;177:5943–51. doi: 10.1128/jb.177.20.5943-5951.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burgos R, Pich OQ, Ferrer-Navarro M, Baseman JB, Querol E, Pinol J. Mycoplasma genitalium P140 and P110 cytadhesins are reciprocally stabilized and required for cell adhesion and terminal-organelle development. J Bacteriol. 2006;188:8627–37. doi: 10.1128/JB.00978-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baseman JB, Dallo SF, Tully JG, Rose DL. Isolation and characterization of Mycoplasma genitalium strains from the human respiratory tract. J Clin Microbiol. 1988;26:2266–9. doi: 10.1128/jcm.26.11.2266-2269.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lo SC, Hayes MM, Kotani H, Pierce PF, Wear DJ, Newton PB, 3rd, et al. Adhesion onto and invasion into mammalian cells by mycoplasma penetrans: a newly isolated mycoplasma from patients with AIDS. Mod Pathol. 1993;6:276–80. [PubMed] [Google Scholar]
- 28.Taylor-Robinson D, Sarathchandra P, Furr PM. Mycoplasma fermentans - HeLa cell interactions. Clin Infect Dis. 1993;17(Suppl 1):S302–4. doi: 10.1093/clinids/17.supplement_1.s302. [DOI] [PubMed] [Google Scholar]
- 29.Taylor-Robinson D, Davies HA, Sarathchandra P, Furr PM. Intracellular location of mycoplasmas in cultured cells demonstrated by immunocytochemistry and electron microscopy. Int J Exp Pathol. 1991;72:705–14. [PMC free article] [PubMed] [Google Scholar]
- 30.Mernaugh GR, Dallo SF, Holt SC, Baseman JB. Properties of adhering and nonadhering populations of Mycoplasma genitalium. Clin Infect Dis. 1993;17(Suppl 1):S69–78. doi: 10.1093/clinids/17.supplement_1.s69. [DOI] [PubMed] [Google Scholar]
- 31.Baseman JB, Lange M, Criscimagna NL, Giron JA, Thomas CA. Interplay between mycoplasmas and host target cells. Microb Pathog. 1995;19:105–16. doi: 10.1006/mpat.1995.0050. [DOI] [PubMed] [Google Scholar]
- 32.Dallo SF, Baseman JB. Intracellular DNA replication and long-term survival of pathogenic mycoplasmas. Microb Pathog. 2000;29:301–9. doi: 10.1006/mpat.2000.0395. [DOI] [PubMed] [Google Scholar]
- 33.Razin S, Yogev D, Naot Y. Molecular biology and pathogenicity of mycoplasmas. Microbiol Mol Biol Rev. 1998;62:1094–156. doi: 10.1128/mmbr.62.4.1094-1156.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rottem S. Interaction of mycoplasmas with host cells. Physiol Rev. 2003;83:417–32. doi: 10.1152/physrev.00030.2002. [DOI] [PubMed] [Google Scholar]
- 35.Ueno PM, Timenetsky J, Centonze VE, Wewer JJ, Cagle M, Stein MA, et al. Interaction of Mycoplasma genitalium with host cells: evidence for nuclear localization. Microbiology. 2008;154:3033–41. doi: 10.1099/mic.0.2008/020735-0. [DOI] [PubMed] [Google Scholar]
- 36.Svenstrup HF, Fedder J, Kristoffersen SE, Trolle B, Birkelund S, Christiansen G. Mycoplasma genitalium, Chlamydia trachomatis, and tubal factor infertility - a prospective study. Fertil Steril. 2008;90:513–20. doi: 10.1016/j.fertnstert.2006.12.056. [DOI] [PubMed] [Google Scholar]
- 37.Alvarez RA, Blaylock MW, Baseman JB. Surface localized glyceraldehyde-3-phosphate dehydrogenase of Mycoplasma genitalium binds mucin. Mol Microbiol. 2003;48:1417–25. doi: 10.1046/j.1365-2958.2003.03518.x. [DOI] [PubMed] [Google Scholar]
- 38.Blaylock MW, Musatovova O, Baseman JG, Baseman JB. Determination of infectious load of Mycoplasma genitalium in clinical samples of human vaginal cells. J Clin Microbiol. 2004;42:746–52. doi: 10.1128/JCM.42.2.746-752.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dhandayuthapani S, Blaylock MW, Bebear CM, Rasmussen WG, Baseman JB. Peptide methionine sulfoxide reductase (MsrA) is a virulence determinant in Mycoplasma genitalium. J Bacteriol. 2001;183:5645–50. doi: 10.1128/JB.183.19.5645-5650.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ibsen HH, Moller BR, Halkier-Sorensen L, From E. Treatment of nongonococcal urethritis: comparison of ofloxacin and erythromycin. Sex Transm Dis. 1989;16:32–5. doi: 10.1097/00007435-198901000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Stamm WE, Hicks CB, Martin DH, Leone P, Hook EW, 3rd, Cooper RH, et al. Azithromycin for empirical treatment of the nongonococcal urethritis syndrome in men. A randomized double-blind study. JAMA. 1995;274:545–9. [PubMed] [Google Scholar]
- 42.Hyman HC, Yogev D, Razin S. DNA probes for detection and identification of Mycoplasma pneumoniae and Mycoplasma genitalium. J Clin Microbiol. 1987;25:726–8. doi: 10.1128/jcm.25.4.726-728.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jensen JS, Uldum SA, Sondergard-Andersen J, Vuust J, Lind K. Polymerase chain reaction for detection of Mycoplasma genitalium in clinical samples. J Clin Microbiol. 1991;29:46–50. doi: 10.1128/jcm.29.1.46-50.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Horner PJ, Gilroy CB, Thomas BJ, Naidoo RO, Taylor-Robinson D. Association of Mycoplasma genitalium with acute non-gonococcal urethritis. Lancet. 1993;342:582–5. doi: 10.1016/0140-6736(93)91411-e. [DOI] [PubMed] [Google Scholar]
- 45.Taylor-Robinson D, Tully JG, Barile MF. Urethral infection in male chimpanzees produced experimentally by Mycoplasma genitalium. Br J Exp Pathol. 1985;66:95–101. [PMC free article] [PubMed] [Google Scholar]
- 46.Tully JG, Taylor-Robinson D, Rose DL, Furr PM, Graham CE, Barile MF. Urogenital challenge of primate species with Mycoplasma genitalium and characteristics of infection induced in chimpanzees. J Infect Dis. 1986;153:1046–54. doi: 10.1093/infdis/153.6.1046. [DOI] [PubMed] [Google Scholar]
- 47.Blanchard A, Hamrick W, Duffy L, Baldus K, Cassell GH. Use of the polymerase chain reaction for detection of Mycoplasma fermentans and Mycoplasma genitalium in the urogenital tract and amniotic fluid. Clin Infect Dis. 1993;17(Suppl 1):S272–9. doi: 10.1093/clinids/17.supplement_1.s272. [DOI] [PubMed] [Google Scholar]
- 48.Keane FE, Thomas BJ, Gilroy CB, Renton A, Taylor-Robinson D. The association of Chlamydia trachomatis and Mycoplasma genitalium with non-gonococcal urethritis: observations on heterosexual men and their female partners. Int J STD AIDS. 2000;11:435–9. doi: 10.1258/0956462001916209. [DOI] [PubMed] [Google Scholar]
- 49.de Barbeyrac B, Bernet-Poggi C, Febrer F, Renaudin H, Dupon M, Bebear C. Detection of Mycoplasma pneumoniae and Mycoplasma genitalium in clinical samples by polymerase chain reaction. Clin Infect Dis. 1993;17(Suppl 1):S83–9. doi: 10.1093/clinids/17.supplement_1.s83. [DOI] [PubMed] [Google Scholar]
- 50.Gambini D, Decleva I, Lupica L, Ghislanzoni M, Cusini M, Alessi E. Mycoplasma genitalium in males with nongonococcal urethritis: prevalence and clinical efficacy of eradication. Sex Transm Dis. 2000;27:226–9. doi: 10.1097/00007435-200004000-00008. [DOI] [PubMed] [Google Scholar]
- 51.Bjornelius E, Lidbrink P, Jensen JS. Mycoplasma genitalium in non-gonococcal urethritis--a study in Swedish male STD patients. Int J STD AIDS. 2000;11:292–6. doi: 10.1177/095646240001100504. [DOI] [PubMed] [Google Scholar]
- 52.Johannisson G, Enstrom Y, Lowhagen GB, Nagy V, Ryberg K, Seeberg S, et al. Occurrence and treatment of Mycoplasma genitalium in patients visiting STD clinics in Sweden. Int J STD AIDS. 2000;11:324–6. doi: 10.1177/095646240001100508. [DOI] [PubMed] [Google Scholar]
- 53.Maeda S, Tamaki M, Nakano M, Uno M, Deguchi T, Kawada Y. Detection of Mycoplasma genitalium in patients with urethritis. J Urol. 1998;159:405–7. doi: 10.1016/s0022-5347(01)63933-8. [DOI] [PubMed] [Google Scholar]
- 54.Deguchi T, Komeda H, Yasuda M, Tada K, Iwata H, Asano M, et al. Mycoplasma genitalium in non-gonococcal urethritis. Int J STD AIDS. 1995;6:144–5. doi: 10.1177/095646249500600219. [DOI] [PubMed] [Google Scholar]
- 55.Manhas A, Sethi S, Sharma M, Wanchu A, Kanwar AJ, Kaur K, et al. Association of genital mycoplasmas including Mycoplasma genitalium in HIV infected men with nongonococcal urethritis attending STD & HIV clinics. Indian J Med Res. 2009;129:305–10. [PubMed] [Google Scholar]
- 56.Bowie WR, Alexander ER, Stimson JB, Floyd JF, Holmes KK. Therapy for nongonococcal urethritis: double-blind randomized comparison of two doses and two durations of minocycline. Ann Intern Med. 1981;95:306–11. doi: 10.7326/0003-4819-95-3-306. [DOI] [PubMed] [Google Scholar]
- 57.Wong ES, Hooton TM, Hill CC, McKevitt M, Stamm WE. Clinical and microbiological features of persistent or recurrent nongonococcal urethritis in men. J Infect Dis. 1988;158:1098–101. doi: 10.1093/infdis/158.5.1098. [DOI] [PubMed] [Google Scholar]
- 58.Maeda SI, Tamaki M, Kojima K, Yoshida T, Ishiko H, Yasuda M, et al. Association of Mycoplasma genitalium persistence in the urethra with recurrence of nongonococcal urethritis. Sex Transm Dis. 2001;28:472–6. doi: 10.1097/00007435-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 59.Krieger JN, Riley DE, Roberts MC, Berger RE. Prokaryotic DNA sequences in patients with chronic idiopathic prostatitis. J Clin Microbiol. 1996;34:3120–8. doi: 10.1128/jcm.34.12.3120-3128.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Taylor-Robinson D. Mycoplasma genitalium - an up-date. Int J STD AIDS. 2002;13:145–51. doi: 10.1258/0956462021924776. [DOI] [PubMed] [Google Scholar]
- 61.Uno M, Deguchi T, Komeda H, Hayasaki M, Iida M, Nagatani M, et al. Mycoplasma genitalium in the cervices of Japanese women. Sex Transm Dis. 1997;24:284–6. doi: 10.1097/00007435-199705000-00009. [DOI] [PubMed] [Google Scholar]
- 62.Manhart LE, Critchlow CW, Holmes KK, Dutro SM, Eschenbach DA, Stevens CE, et al. Mucopurulent cervicitis and Mycoplasma genitalium. J Infect Dis. 2003;187:650–7. doi: 10.1086/367992. [DOI] [PubMed] [Google Scholar]
- 63.Cohen CR, Manhart LE, Bukusi EA, Astete S, Brunham RC, Holmes KK, et al. Association between Mycoplasma genitalium and acute endometritis. Lancet. 2002;359:765–6. doi: 10.1016/S0140-6736(02)07848-0. [DOI] [PubMed] [Google Scholar]
- 64.Irwin KL, Moorman AC, O’Sullivan MJ, Sperling R, Koestler ME, Soto I, et al. Influence of human immunodeficiency virus infection on pelvic inflammatory disease. Obstet Gynecol. 2000;95:525–34. doi: 10.1016/s0029-7844(99)00621-3. [DOI] [PubMed] [Google Scholar]
- 65.Simms I, Eastick K, Mallinson H, Thomas K, Gokhale R, Hay P, et al. Associations between Mycoplasma genitalium, Chlamydia trachomatis, and pelvic inflammatory disease. Sex Transm Infect. 2003;79:154–6. doi: 10.1136/sti.79.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Palmer HM, Gilroy CB, Claydon EJ, Taylor-Robinson D. Detection of Mycoplasma genitalium in the genitourinary tract of women by the polymerase chain reaction. Int J STD AIDS. 1991;2:261–3. doi: 10.1177/095646249100200407. [DOI] [PubMed] [Google Scholar]
- 67.Keane FE, Thomas BJ, Gilroy CB, Renton A, Taylor-Robinson D. The association of Mycoplasma hominis, Ureaplasma urealyticum and Mycoplasma genitalium with bacterial vaginosis: observations on heterosexual women and their male partners. Int J STD AIDS. 2000;11:356–60. doi: 10.1258/0956462001916056. [DOI] [PubMed] [Google Scholar]
- 68.Lu GC, Schwebke JR, Duffy LB, Cassell GH, Hauth JC, Andrews WW, et al. Midtrimester vaginal Mycoplasma genitalium in women with subsequent spontaneous preterm birth. Am J Obstet Gynecol. 2001;185:163–5. doi: 10.1067/mob.2001.115113. [DOI] [PubMed] [Google Scholar]
- 69.Oakeshott P, Hay P, Taylor-Robinson D, Hay S, Dohn B, Kerry S, et al. Prevalence of Mycoplasma genitalium in early pregnancy and relationship between its presence and pregnancy outcome. BJOG. 2004;111:1464–7. doi: 10.1111/j.1471-0528.2004.00276.x. [DOI] [PubMed] [Google Scholar]
- 70.Clausen HF, Fedder J, Drasbek M, Nielsen PK, Toft B, Ingerslev HJ, et al. Serological investigation of Mycoplasma genitalium in infertile women. Hum Reprod. 2001;16:1866–74. doi: 10.1093/humrep/16.9.1866. [DOI] [PubMed] [Google Scholar]
- 71.Yokoi S, Maeda S, Kubota Y, Tamaki M, Mizutani K, Yasuda M, et al. The role of Mycoplasma genitalium and Ureaplasma urealyticum biovar 2 in postgonococcal urethritis. Clin Infect Dis. 2007;45:866–71. doi: 10.1086/521266. [DOI] [PubMed] [Google Scholar]
- 72.Uno M, Deguchi T, Komeda H, Yasuda M, Tamaki M, Maeda S, et al. Prevalence of Mycoplasma genitalium in men with gonococcal urethritis. Int J STD AIDS. 1996;7:443–4. doi: 10.1258/0956462961918284. [DOI] [PubMed] [Google Scholar]
- 73.Gaydos C, Maldeis NE, Hardick A, Hardick J, Quinn TC. Mycoplasma genitalium as a contributor to the multiple etiologies of cervicitis in women attending sexually transmitted disease clinics. Sex Transm Dis. 2009;36:598–606. doi: 10.1097/OLQ.0b013e3181b01948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pepin J, Sobela F, Deslandes S, Alary M, Wegner K, Khonde N, et al. Etiology of urethral discharge in West Africa: the role of Mycoplasma genitalium and Trichomonas vaginalis. Bull World Health Organ. 2001;79:118–26. [PMC free article] [PubMed] [Google Scholar]
- 75.Amirmozafari N, Mirnejad R, Kazemi B, Sariri E, Bojari MR, Darkahi FD. Simultaneous detection of genital Mycoplasma in women with genital infections by PCR. J Biol Sci. 2009;9:804–9. [PubMed] [Google Scholar]
- 76.Mirnejad R, Amirmozafari N, Kazemi B. Simultaneous and rapid differential diagnosis of Mycoplasma genitalium and Ureaplasma urealyticum based on a polymerase chain reaction-restriction fragment length polymorphism. Indian J Med Microbiol. 2011;29:33–6. doi: 10.4103/0255-0857.76521. [DOI] [PubMed] [Google Scholar]
- 77.Samra Z, Rosenberg S, Madar-Shapiro L. Direct simultaneous detection of 6 sexually transmitted pathogens from clinical specimens by multiplex polymerase chain reaction and auto-capillary electrophoresis. Diagn Microbiol Infect Dis. 2011;70:17–21. doi: 10.1016/j.diagmicrobio.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 78.Tait IA, Hart CA. Chlamydia trachomatis in non-gonococcal urethritis patients and their heterosexual partners: routine testing by polymerase chain reaction. Sex Transm Infect. 2002;78:286–8. doi: 10.1136/sti.78.4.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Quinn TC, Gaydos C, Shepherd M, Bobo L, Hook EW, 3rd, Viscidi R, et al. Epidemiologic and microbiologic correlates of Chlamydia trachomatis infection in sexual partnerships. JAMA. 1996;276:1737–42. [PubMed] [Google Scholar]
- 80.Ross JD, Jensen JS. Mycoplasma genitalium as a sexually transmitted infection: implications for screening, testing, and treatment. Sex Transm Infect. 2006;82:269–71. doi: 10.1136/sti.2005.017368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Waites KB, Taylor-Robinson D. Mycoplasma and Ureaplasma. In: Murray PR, Baron EJ, Jorgensen JH, Landry ML, Pfaller MA, editors. Manual of clinical microbiology. 9th ed. Washington DC: ASM Press; 2007. pp. 1004–20. [Google Scholar]
- 82.Kenny GE. Genital Mycoplasmas: Mycoplasma genitalium, Mycoplasma hominis, and Ureaplasma species. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 7th ed. Philadelphia: Churchill Livingstone; 2010. pp. 2491–3. [Google Scholar]
- 83.Jensen JS, Hansen HT, Lind K. Isolation of Mycoplasma genitalium strains from the male urethra. J Clin Microbiol. 1996;34:286–91. doi: 10.1128/jcm.34.2.286-291.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hussain AI, Robson WL, Kelley R, Reid T, Gangemi JD. Mycoplasma penetrans and other mycoplasmas in urine of human immunodeficiency virus-positive children. J Clin Microbiol. 1999;37:1518–23. doi: 10.1128/jcm.37.5.1518-1523.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hopps HE, Del Giudice RA. Cell culture models as ancillary tools in the isolation and characterization of mycoplasmas. Isr J Med Sci. 1984;20:927–30. [PubMed] [Google Scholar]
- 86.Gobel UB, Geiser A, Stanbridge EJ. Oligonucleotide probes complementary to variable regions of ribosomal RNA discriminate between Mycoplasma species. J Gen Microbiol. 1987;133:1969–74. doi: 10.1099/00221287-133-7-1969. [DOI] [PubMed] [Google Scholar]
- 87.Jensen JS, Sondergard-Andersen J, Uldum SA, Lind K. Detection of Mycoplasma pneumoniae in simulated clinical samples by polymerase chain reaction. Brief report. APMIS. 1989;97:1046–8. doi: 10.1111/j.1699-0463.1989.tb00516.x. [DOI] [PubMed] [Google Scholar]
- 88.Risi GF, Jr, Martin DH, Silberman JA, Cohen JC. A DNA probe for detecting Mycoplasma genitalium in clinical specimens. Mol Cell Probes. 1987;1:327–35. doi: 10.1016/0890-8508(87)90014-4. [DOI] [PubMed] [Google Scholar]
- 89.Hooton TM, Roberts MC, Roberts PL, Holmes KK, Stamm WE, Kenny GE. Prevalence of Mycoplasma genitalium determined by DNA probe in men with urethritis. Lancet. 1988;1:266–8. doi: 10.1016/s0140-6736(88)90350-9. [DOI] [PubMed] [Google Scholar]
- 90.Jensen JS, Bjornelius E, Dohn B, Lidbrink P. Use of TaqMan 5’ nuclease real-time PCR for quantitative detection of Mycoplasma genitalium DNA in males with and without urethritis who were attendees at a sexually transmitted disease clinic. J Clin Microbiol. 2004;42:683–92. doi: 10.1128/JCM.42.2.683-692.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Peterson SN, Bailey CC, Jensen JS, Borre MB, King ES, Bott KF, et al. Characterization of repetitive DNA in the Mycoplasma genitalium genome: possible role in the generation of antigenic variation. Proc Natl Acad Sci USA. 1995;92:11829–33. doi: 10.1073/pnas.92.25.11829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jensen JS, Orsum R, Dohn B, Uldum S, Worm AM, Lind K. Mycoplasma genitalium: a cause of male urethritis? Genitourin Med. 1993;69:265–9. doi: 10.1136/sti.69.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jensen JS, Borre MB, Dohn B. Detection of Mycoplasma genitalium by PCR amplification of the 16S rRNA gene. J Clin Microbiol. 2003;41:261–6. doi: 10.1128/JCM.41.1.261-266.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Palmer HM, Gilroy CB, Furr PM, Taylor-Robinson D. Development and evaluation of the polymerase chain reaction to detect Mycoplasma genitalium. FEMS Microbiol Lett. 1991;61:199–203. doi: 10.1016/0378-1097(91)90551-k. [DOI] [PubMed] [Google Scholar]
- 95.Yoshida T, Deguchi T, Ito M, Maeda S, Tamaki M, Ishiko H. Quantitative detection of Mycoplasma genitalium from first-pass urine of men with urethritis and asymptomatic men by real-time PCR. J Clin Microbiol. 2002;40:1451–5. doi: 10.1128/JCM.40.4.1451-1455.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dupin N, Bijaoui G, Schwarzinger M, Ernault P, Gerhardt P, Jdid R, et al. Detection and quantification of Mycoplasma genitalium in male patients with urethritis. Clin Infect Dis. 2003;37:602–5. doi: 10.1086/376990. [DOI] [PubMed] [Google Scholar]
- 97.Edberg A, Jurstrand M, Johansson E, Wikander E, Hoog A, Ahlqvist T, et al. A comparative study of three different PCR assays for detection of Mycoplasma genitalium in urogenital specimens from men and women. J Med Microbiol. 2008;57:304–9. doi: 10.1099/jmm.0.47498-0. [DOI] [PubMed] [Google Scholar]
- 98.Ma L, Jensen JS, Myers L, Burnett J, Welch M, Jia Q, et al. Mycoplasma genitalium: an efficient strategy to generate genetic variation from a minimal genome. Mol Microbiol. 2007;66:220–36. doi: 10.1111/j.1365-2958.2007.05911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Weinstein SA, Stiles BG. A review of the epidemiology, diagnosis and evidence-based management of Mycoplasma genitalium. Sex Health. 2011;8:143–58. doi: 10.1071/SH10065. [DOI] [PubMed] [Google Scholar]
- 100.Taylor-Robinson D, Bebear C. Antibiotic susceptibilities of mycoplasmas and treatment of mycoplasmal infections. J Antimicrob Chemother. 1997;40:622–30. doi: 10.1093/jac/40.5.622. [DOI] [PubMed] [Google Scholar]
- 101.Renaudin H, Tully JG, Bebear C. In vitro susceptibilities of Mycoplasma genitalium to antibiotics. Antimicrob Agents Chemother. 1992;36:870–2. doi: 10.1128/aac.36.4.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bebear CM, Renaudin H, Bryskier A, Bebear C. Comparative activities of telithromycin (HMR 3647), levofloxacin, and other antimicrobial agents against human mycoplasmas. Antimicrob Agents Chemother. 2000;44:1980–2. doi: 10.1128/aac.44.7.1980-1982.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bebear CM, Renaudin H, Schaeverbeke T, Leblanc F, Bebear C. In-vitro activity of grepafloxacin, a new fluoroquinolone, against mycoplasmas. J Antimicrob Chemother. 1999;43:711–4. doi: 10.1093/jac/43.5.711. [DOI] [PubMed] [Google Scholar]
- 104.Bebear CM, Renaudin H, Charron A, Gruson D, Lefrancois M, Bebear C. In vitro activity of trovafloxacin compared to those of five antimicrobials against mycoplasmas including Mycoplasma hominis and Ureaplasma urealyticum fluoroquinolone-resistant isolates that have been genetically characterized. Antimicrob Agents Chemother. 2000;44:2557–60. doi: 10.1128/aac.44.9.2557-2560.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hannan PC, Woodnutt G. In vitro activity of gemifloxacin (SB 265805; LB20304a) against human mycoplasmas. J Antimicrob Chemother. 2000;45:367–9. doi: 10.1093/jac/45.3.367. [DOI] [PubMed] [Google Scholar]
- 106.McCormack WM. Infections due to mycoplasmas. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's principles of internal medicine. 17th ed. New York: McGraw-Hill Medical; 2008. pp. 1068–70. [Google Scholar]
- 107.Taylor-Robinson D, Gilroy CB, Hay PE. Occurrence of Mycoplasma genitalium in different populations and its clinical significance. Clin Infect Dis. 1993;17(Suppl 1):S66–8. doi: 10.1093/clinids/17.supplement_1.s66. [DOI] [PubMed] [Google Scholar]
- 108.Horner P, Thomas B, Gilroy CB, Egger M, Taylor-Robinson D. Role of Mycoplasma genitalium and Ureaplasma urealyticum in acute and chronic nongonococcal urethritis. Clin Infect Dis. 2001;32:995–1003. doi: 10.1086/319594. [DOI] [PubMed] [Google Scholar]
- 109.Casin I, Vexiau-Robert D, De La Salmoniere P, Eche A, Grandry B, Janier M. High prevalence of Mycoplasma genitalium in the lower genitourinary tract of women attending a sexually transmitted disease clinic in Paris, France. Sex Transm Dis. 2002;29:353–9. doi: 10.1097/00007435-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 110.Pepin J, Labbe AC, Khonde N, Deslandes S, Alary M, Dzokoto A, et al. Mycoplasma genitalium: an organism commonly associated with cervicitis among west African sex workers. Sex Transm Infect. 2005;81:67–72. doi: 10.1136/sti.2003.009100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Anagrius C, Lore B, Jensen JS. Mycoplasma genitalium: prevalence, clinical significance, and transmission. Sex Transm Infect. 2005;81:458–62. doi: 10.1136/sti.2004.012062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Falk L, Fredlund H, Jensen JS. Signs and symptoms of urethritis and cervicitis among women with or without Mycoplasma genitalium or Chlamydia trachomatis infection. Sex Transm Infect. 2005;81:73–8. doi: 10.1136/sti.2004.010439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Korte JE, Baseman JB, Cagle MP, Herrera C, Piper JM, Holden AE, et al. Cervicitis and genitourinary symptoms in women culture positive for Mycoplasma genitalium. Am J Reprod Immunol. 2006;55:265–75. doi: 10.1111/j.1600-0897.2005.00359.x. [DOI] [PubMed] [Google Scholar]
- 114.Cohen CR, Nosek M, Meier A, Astete SG, Iverson-Cabral S, Mugo NR, et al. Mycoplasma genitalium infection and persistence in a cohort of female sex workers in Nairobi, Kenya. Sex Transm Dis. 2007;34:274–9. doi: 10.1097/01.olq.0000237860.61298.54. [DOI] [PubMed] [Google Scholar]
- 115.Hogdahl M, Kihlstrom E. Leucocyte esterase testing of first-voided urine and urethral and cervical smears to identify Mycoplasma genitalium-infected men and women. Int J STD AIDS. 2007;18:835–8. doi: 10.1258/095646207782716983. [DOI] [PubMed] [Google Scholar]
- 116.Huppert JS, Mortensen JE, Reed JL, Kahn JA, Rich KD, Hobbs MM. Mycoplasma genitalium detected by transcription-mediated amplification is associated with Chlamydia trachomatis in adolescent women. Sex Transm Dis. 2008;35:250–4. doi: 10.1097/OLQ.0b013e31815abac6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Arraiz RN, Colina CS, Marcucci JR, Rondon GN, Reyes SF, Bermúdez PV, et al. Mycoplasma genitalium detection and correlation with clinical manifestations in population of the Zulia State, Venezuela. Rev Chilena Infectol. 2008;25:256–61. [PubMed] [Google Scholar]
- 118.Manhart LE, Mostad SB, Baeten JM, Astete SG, Mandaliya K, Totten PA. High Mycoplasma genitalium organism burden is associated with shedding of HIV-1 DNA from the cervix. J Infect Dis. 2008;197:733–6. doi: 10.1086/526501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Moi H, Reinton N, Moghaddam A. Mycoplasma genitalium is associated with symptomatic and asymptomatic non-gonococcal urethritis in men. Sex Transm Infect. 2009;85:15–8. doi: 10.1136/sti.2008.032730. [DOI] [PubMed] [Google Scholar]
- 120.Thurman AR, Musatovova O, Perdue S, Shain RN, Baseman JG, Baseman JB. Mycoplasma genitalium symptoms, concordance and treatment in high-risk sexual dyads. Int J STD AIDS. 2010;21:177–83. doi: 10.1258/ijsa.2009.008485. [DOI] [PubMed] [Google Scholar]
- 121.Le Roux MC, Ramoncha MR, Adam A, Hoosen AA. Aetiological agents of urethritis in symptomatic South African men attending a family practice. Int J STD AIDS. 2010;21:477–81. doi: 10.1258/ijsa.2010.010066. [DOI] [PubMed] [Google Scholar]
- 122.Shigehara K, Kawaguchi S, Sasagawa T, Furubayashi K, Shimamura M, Maeda Y, et al. Prevalence of genital Mycoplasma, Ureaplasma, Gardnerella, and human papillomavirus in Japanese men with urethritis, and risk factors for detection of urethral human papillomavirus infection. J Infect Chemother. 2011;17:487–92. doi: 10.1007/s10156-010-0203-0. [DOI] [PubMed] [Google Scholar]
- 123.Zimba TF, Apalata T, Sturm WA, Moodley P. Aetiology of sexually transmitted infections in Maputo, Mozambique. J Infect Dev Ctries. 2011;5:41–7. doi: 10.3855/jidc.1179. [DOI] [PubMed] [Google Scholar]


