Abstract
This study investigated the moderating role of sexual communication in the association between intentions to use condoms and unprotected sex in a sample of 358 individuals living with HIV (233 men, 125 women, M age = 43). Longitudinal analyses revealed a significant interaction between condom intentions and sexual communication: individuals who were high in both condom intentions and safer sex communication engaged in less unprotected sex with all partners and with partners of HIV negative or unknown serostatus over 6 months of follow-up. Among individuals low in communication, intentions were not associated with unprotected sex. Implications for interventions are discussed.
Keywords: Safer sex, HIV/AIDS, condom intentions, sexual communication
Introduction
For sexually active individuals, consistent condom use is the most effective method of preventing the spread of sexually transmitted diseases (STDs). It is particularly important for people living with HIV to use condoms, both to prevent them from transmitting HIV to their sexual partners and to protect each partner from acquiring or transmitting other STDs. However, the 56,000 new HIV transmissions and 19 million new STD infections occurring annually in the United States suggests there is a serious lapse in consistent condom use for many people (CDC, 2010). Such statistics beg the question: why are condoms used inconsistently or not at all in some sexual relationships? Understanding the answer to this question is of paramount importance for public health programs that seek to reduce risky sexual behavior.
The sexual decision making process that leads a person to use or not use condoms is undoubtedly complex, yet a number of health behavior theories have been applied to explain this process fairly reliably. Such theories include the Theory of Reasoned Action/Planned Behavior (TRA/TPB), Social Cognitive Theory (SCT), and the Information-Motivation-Behavioral-Skills Model (IMB; for reviews, see Fisher and Fisher, 2000; Noar, 2007). These models are common in that they each emphasize the relationship between behavioral intentions to use condoms and later condom use (Albarracín et al., 2001; Fishbein, 2008; Noar, 2007). For example, the TRA proposes that distal factors, such as individual attitudes and subjective norms, predict an individual’s intentions to use condoms, which serve as key antecedents of condom use (Albarracín et al., 2001; Fishbein, 2008; Sheeran et al., 1999). In fact, a meta-analysis of nearly 100 studies found that intentions to use condoms were strongly associated with condom use both cross-sectionally and longitudinally (weighted mean correlation = .45; Albarracín et al., 2001).
Although behavioral intentions to use condoms strongly predict condom use, some people who intend to use condoms do so successfully, while others do not follow through with their intentions (Abraham et al., 1999). Thus, there are likely important intervening factors between intentions and actions not currently accounted for in theory or research positing direct links. We are not the first to suggest that moderating or mediating process variables may explain gaps in the intention-behavior relationship. Indeed, a few studies have demonstrated support for several possible intervening variables, including preparatory behaviors, implementation intentions, and sexual communication (Abraham et al., 1998; Abraham et al., 1999; Bryan et al., 2002; de Vet et al., 2011; Noar et al., 2006a).
In describing the recently developed Integrative Model (IM) of behavioral prediction that amalgamates several behavioral theories, including the TRA and TPB, Fishbein (2008) noted, “The IM assumes that intentions are the immediate antecedents of behavior, but in addition, the IM recognizes that environmental factors and skills and abilities can moderate the intention-behavior relationship” (p. 834). In this context, moderating variables are those factors that affect the direction or strength of the relationship between intentions to use condoms and actual condom use. Identifying such moderators could shed light on why some people’s intentions are strongly associated with their behavior and others are not. Identifying moderating skills and abilities is of great theoretical relevance, and may also be of significant practical importance to HIV/STD prevention programs that seek effective targets for behavioral intervention. In this study, we focus on the possible moderating role of what sexual health scholars increasingly recognize as a critical health-protective variable – sexual communication.
The Role of Sexual Communication
Because sexual behavior frequently occurs in a dyad, using condoms likely requires communication between sexual partners (Bryan et al., 2002; Noar et al., 2006a; Sheeran et al., 1999). Therefore, sexual communication, defined here as the ability to verbally discuss and negotiate safer sex with a partner (Noar, 2007), may be a key intervening variable that helps translate intentions into actions. The direct association between sexual communication and condom use provides preliminary evidence for this possibility. Specifically, individuals who clearly communicate or intend to communicate with their sexual partners about condoms and more general sexual health topics (e.g., HIV/STDs, sexual histories) are more likely to use protection than individuals who do not communicate (Catania et al., 1992; Crosby et al., 2002; Noar et al., 2006a; Sheeran et al., 1999; Widman et al., 2006). One meta-analysis found that sexual communication was a stronger predictor of safer sex behavior than over 40 other psychosocial factors investigated, including sexual attitudes, self-efficacy, and barriers to condom use (Sheeran et al., 1999).
Despite i t s importance, sexual communication does not always occur in sexual relationships. In fact, as few as half of sexually active individuals indicate they have discussed condoms or safer sex with their partners (Bruhin, 2003; Coleman and Ingram, 1999; Crepaz and Marks, 2003). Due to barriers like HIV stigma (Smith et al., 2008), some people living with HIV may also fall short in communicating with their partners about safer sex issues. For instance, among 105 HIV-positive men, 48% of men reported discussing general safer sex issues and 65% reported specifically discussing condoms with their most recent HIV-negative or unknown serostatus sexual partner (Crepaz and Marks, 2003). This lack of communication about condom use may place some individuals at risk for unprotected intercourse, even when they have strong intentions to use condoms. In other words, the extent to which a person’s intentions predict their behavior is likely moderated by their motivation and ability to communicate about safer sex.
Purpose of the Current Project
In this study, we investigate the hypothesis that sexual communication moderates the link between condom use intentions and unprotected sex. We posit a direct relationship between intentions to use condoms and condom use (Albarracín et al., 2001; Sheeran et al., 1999), a direct relationship between sexual communication and condom use (Noar et al., 2006a; Sheeran et al., 1999), and an interaction between these predictors, such that individuals with stronger behavioral intentions and greater communication about safer sex will be the least likely to engage in unprotected sex. While both of the main effects have been examined in a host of prior studies, we are unaware of any research to date that has explicitly tested the interaction between these variables.
It is worth noting that most prior studies that have examined the intention-behavior gap in condom use have focused on HIV-negative populations (e.g., Abraham et al., 1999; Bryan et al., 2002). We test our hypotheses in a sexually active sample of individuals living with HIV, a sample for which the consequences of unprotected sex may be particularly severe. We assess sexual communication using a format that captures intentions to communicate with a partner about sex (e.g., Thompson et al., 2001), as opposed to a format that captures past sexual communication behavior (e.g., Bryan et al., 2002; Noar et al., 2002). The communication intention format has been shown to predict condom use behavior (Noar et al., 2006a) and parallels our assessment of condom use intentions. Finally, we examine our predictions longitudinally while controlling for prior risky sex so that we can examine the influence of intentions and sexual communication over and above past behavior.
Method
Participants
Data for the current project come from SafeTalk, a two-armed randomized, controlled trial of a safer sex intervention among people living with HIV (Golin et al., in press). As part of the trial, participants were randomized to either a multi-component motivational interviewing-based safer sex program or an attention-matched heart-healthy, nutrition program. To be eligible, participants had to be: (1) over 18 years old; (2) HIV-infected; (3) receiving HIV treatment at one of the three study sites; (4) English-speaking; (5) of sufficient cognitive ability to complete the consent and counseling; and (6) self-reported having oral, anal, or vaginal sex in the last 12 months. For the analyses presented here, we use the baseline and first follow-up time point (median time between baseline and follow-up = 5.7 months, SD = 2.1 months). We excluded participants who did not complete the follow-up assessment or had more than 12 months between baseline and follow-up. The university’s Office for the Protection of Human Research Subjects approved all study procedures.
Procedure
At each time, participants completed an audio computer assisted self-interview (ACASI)-administered survey (Nova Research Co) lasting 30-60 minutes. The survey assessed demographic and clinical characteristics, sexual communication, condom intentions, and risky sexual behavior. Participants received a $25.00 gift card for each assessment.
Measures
Demographic Factors
We assessed participants’ gender, sexual orientation, age, race/ethnicity, relationship status, employment status, and clinical characteristics related to HIV (i.e., time since diagnosis, viral load). For descriptive purposes, we used participants’ gender and the gender of their reported sexual partners to determine their sex preference subgroup: men who have sex with men (MSM), heterosexual men, or women. Participants who did not report any sex partners were categorized based on their self-reported sexual orientation. Men who reported both male and female sex partners or a bisexual orientation were categorized as MSM.
Condom Use Intentions
Behavioral intentions to use condoms in the future were assessed with two items: 1) “If you were going to have sex in the next 3 months, how likely or unlikely is it that every time you have sex you will actually use a condom?” and 2) “If you were going to have sex in the next 3 months, how likely or unlikely is it that every time you have sex you will use a condom even if your partner does NOT want to?” Items were reported on a scale from 1 = very unlikely to 4 = very likely, which we combined to create a total score (range 2-8). Higher scores indicated greater condom use intentions (Cronbach’s α = .74).
Sexual Communication
Sexual communication was assessed with a composite of two items that captured the likelihood or intent that verbal communication will take place: 1) “If you were going to have sex in the next 3 months, how likely or unlikely is it that every time you have sex, you will tell your partner that you need to use a condom?” and 2) “If you were going to have sex in the next 3 months, how likely or unlikely is it that every time you have sex, you will discuss safer sex with your partner?” Items were reported on a scale from 1 = very unlikely to 4 = very likely, which we combined to create a total score (range 2-8). Higher scores indicated greater sexual communication intentions (Cronbach’s α = .68).
Unprotected Sex
At baseline and follow-up, the ACASI gathered detailed information about sexual behavior over the past three months. Separate versions were used for men and women, which allowed the questions to be consistent with the participant’s gender and the reported gender(s) of their sex partners. Participants were asked whether they had HIV-positive, HIV-negative, and HIV serostatus unknown partners and how many times they had insertive or receptive vaginal or anal intercourse with each partner type in the last three months. For each type of partner and each type of sex act, participants were asked how many times they used a condom, defined as using a condom from the beginning to the end of the sex act. This measurement of condom use is robust and in line with recommendations from the methodological literature (Noar et al., 2006b).
We used this information to calculate two variables: 1) any unprotected anal or vaginal intercourse (UAVI), a dichotomous variable that represented whether or not the participant had unprotected vaginal or anal sex with a partner of any serostatus; and 2) any unprotected anal or vaginal intercourse with an at-risk partner (UAVI-AR), a dichotomous variable that represented whether or not a participant had unprotected vaginal or anal sex with a partner of HIV negative or unknown serostatus.
Results
Participant Characteristics
Of the 490 participants in SafeTalk, we excluded 80 who did not complete the follow-up survey, 40 with over 12 months between baseline and follow-up, 10 with missing sexual behavior data, and 2 with missing sexual communication data. The final sample of 358 participants (233 men, 125 women), included men who have sex with men (38%), heterosexual men (27%), heterosexual women (33%), and other/unknown sexual orientation groups (2%). Participants ranged in age from 18-70 (M = 43.3 years, SD = 9.1), were primarily African-American (71%), and largely unemployed (67%). Approximately half of the sample indicated they were single (49%), 33% were married or in a committed relationship, and 17% were divorced, separated, or widowed. Mean time since HIV diagnosis was 9.7 years (SD = 6.3), and 53% reported an undetectable viral load.
Descriptive Analyses
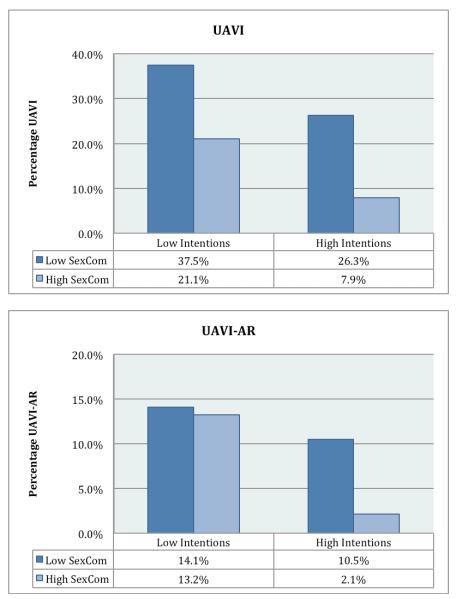
As indicated in Table 1, greater intentions and sexual communication were significantly associated with less unprotected sex, both at baseline and follow-up. Although we analyzed intentions and communication as continuous variables in our primary analyses (see below), for descriptive purposes, we dichotomized these variables to report their frequencies and examine the percentage of people engaging in UAVI and UAVI-AR in each group. To do this, we divided scores on intentions and sexual communication (possible score range = 2-8) into either “low” groups (scores of 2-6) or “high” groups (scores of 7-8) based on the scale response options (where 7-8 indicated that the participant was “very likely” to use condoms or communicate with their partner). This descriptive breakdown by the level of intentions revealed 28.4% (n = 102) of participants reported low condom intentions and 71.5% (n = 256) of participants reported high condom intentions. A descriptive breakdown by the level of sexual communication revealed that 23.2% (n = 83) of participants reported low communication and 76.8% (n = 275) reported high communication with their sexual partners. We then examined the percentage of participants engaging in UAVI and UAVI-AR (Figure 1) based on the dichotomous levels of intentions and communication. Over one third of participants with low intentions and low communication engaged in UAVI, and 14% of participants who were low in both predictors engaged in UAVI-AR. However, among participants high in both intentions and communication, 8% engaged in UAVI and 2% engaged in UAVI-AR.
Table 1.
Descriptive Statistics and Correlations among Primary Study Variablesa
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Baseline Sexual Communication | 3.56 | 0.71 | - | .73 | −.32 | −.24 | −.27 | −.15 |
| 2. Baseline Condom Intentions | 3.48 | 0.80 | - | −.40 | −.28 | −.31 | −.18 | |
| 3. Baseline UAVI (n, %) | 79 | 22.1 | - | .72 | .45 | .27 | ||
| 4. Baseline UAVI-AR (n, %) | 46 | 12.8 | − | .27 | .40 | |||
| 5. Follow-Up UAVI (n, %) | 57 | 15.9 | - | .57 | ||||
| 6. Follow-Up UAVI-AR (n, %) | 21 | 5.9 | - |
Note. UAVI = Unprotected anal or vaginal intercourse. UAVI-AR= Unprotected anal or vaginal intercourse with at-risk partners.
All correlations were significant at p < .01.
Figure 1.
Percentage of people engaging in unprotected sex by low and high intentions and sexual communication
Note: UAVI = Unprotected anal or vaginal intercourse at follow-up assessment. UAVI-AR = Unprotected anal or vaginal intercourse with at-risk partners at follow-up assessment. Low Sexual Communication / Low Intentions = scale score of 2-6; High Sexual Communication / High Intentions = scale score of 7-8 (possible scale range 2-8).
Primary Analyses
We hypothesized an interaction between condom use intentions and sexual communication would longitudinally predict unprotected sex. Two multiple logistic regression analyses were conducted with follow-up UAVI and follow-up UAVI-AR as the dependent variables. In each analysis, we entered condom intentions and sexual communication (each centered) as main effects and the two-way interaction between intentions and communication. We controlled for baseline sexual behavior, age, and treatment arm in each analysis. Consistent with predictions, the intentions X sexual communication interaction emerged for both UAVI (marginally significant, p < .08) and UAVI-AR (p < .05) (Table 2).
Table 2.
Interactions between Condom Intentions and Sexual Communication Predicting Risky Sexual Behavior over Time
| UAVI | UAVI-AR | |||||
|---|---|---|---|---|---|---|
| β | Adjusted OR | 95% CI | β | Adjusted OR | 95% CI | |
| Predictors | ||||||
| Intentions | −0.55 | 0.58+ | 0.33, 1.03 | −1.07 | 0.34* | 0.14, 0.84 |
| SexCom | −0.56 | 0.57 | 0.29, 1.12 | −0.76 | 0.47 | 0.17, 1.26 |
| Intentions X SexCom | −0.35 | 0.70+ | 0.47, 1.05 | −1.00 | 0.37* | 0.16, 0.84 |
| Control Variables | ||||||
| Age | −0.01 | 0.99 | 0.95, 1.03 | −0.04 | 0.96 | 0.90, 1.02 |
| Treatment Arm | 0.12 | 1.12 | 0.58, 2.17 | −0.45 | 0.64 | 0.23, 1.79 |
| Baseline Sexual Behaviora | 1.98 | 7.21*** | 3.62, 14.40 | 2.33 | 10.31*** | 3.59, 29.58 |
Note: UAVI = unprotected sex with any partner at follow-up assessment. UAVI-AR = unprotected sex with a partner who was “at-risk” (i.e., HIV serostatus negative or unknown) at follow-up assessment. Intentions = condom use intentions. SexCom = sexual communication. Intentions and SexCom were analyzed as continuous variables.
p = .08
p < .05
p < .001.
Baseline UAVI was entered in the model predicting follow-up UAVI; Baseline UAVI-AR was entered in the model predicting follow-up UAVI-AR.
To understand how the simple slopes of intentions changed depending on the level of communication, we compared the simple slopes of intentions at “high” levels of the sexual communication (+1 standard deviation above the mean) and “low” levels of sexual communication (-1 SD below the mean; Aiken and West, 1991). This test indicated that intentions led to less UAVI among participants who were high in sexual communication (Adjusted OR = 0.45, 95% CI [0.22, 0.94], p < .05); however, intentions were not related to UAVI for participants who were low in sexual communication (Adjusted OR = 0.74, 95% CI [0.44, 1.26], p = .27). Similarly, intentions led to less UAVI-AR among participants who were high in sexual communication (Adjusted OR = 0.17, 95% CI [0.05, 0.63], p < .01); however, intentions were not related to UAVI-AR for participants who were low in sexual communication (Adjusted OR = 0.70, 95% CI [0.33, 1.49], p = .36).
Post-hoc Analyses
Although we did not have a priori predictions, we were interested in understanding more about the way that condom use intentions and sexual communication might vary by gender and sexual orientation. We conducted descriptive post-hoc analyses for these purposes. First, using independent samples t-tests, we examined if the mean level of condom use intentions or sexual communication differed by gender. We did not find any significant differences in either intentions [t(356) = −0.06] or sexual communication [t(356) = −1.41] between men and women (p values > .15). Next, using one-way ANOVAs and posthoc Tukey tests, we examined if the mean level of condom use intentions or sexual communication differed among sexual orientation groups. We found there were differences in the mean level of intentions [F(2,349) = 6.24, p < .01]: MSM had lower intentions than heterosexual men (mean difference= −.38, p < .01). The intentions of heterosexual women did not differ from MSM or heterosexual men. Additionally, we found there were differences in the mean level of sexual communication by sexual orientation groups [F(2,349) = 13.03, p < .001]: MSM had lower communication than heterosexual men (mean difference= −.45, p < .01) and heterosexual women (mean difference = −.15, p < .05). The communication of heterosexual men and women did not differ.
Discussion
Consistent condom use, particularly among sexually active people living with HIV, is necessary to reduce the transmission of HIV and other STDs. Even in a prevention field that is increasingly moving toward a greater role for biomedical prevention, condom use will remain an important option on the prevention menu (Merson et al., 2008). However, similar to past research (Courtenay-Quirk et al., 2008; Golin et al., 2009; Marks et al., 2005), we found a sizable minority of people living with HIV engage in unprotected sex. At baseline, over 20% of participants had unprotected sex with partners of any serostatus and 13% did so with partners of HIV-negative or unknown serostatus in the prior three months.
The main purpose of this study was to investigate the links among intentions to use condoms, sexual communication, and unprotected sex. Consistent with previous research (Albarracín et al., 2001; Fishbein, 2008), we found an association between condom use intentions and sexual behavior: people with higher intentions were less likely to engage in unprotected sex with any partners and also with HIV-negative or unknown partners. Also consistent with prior research (Noar et al., 2006; Sheeran et al., 1999), we found that sexual communication predicted sexual behavior: people with more sexual communication were less likely to engage in unprotected sex, both at baseline and over approximately 6 months. However, this study extends past research through an examination of the interaction between intentions and communication. We found that it is not, in fact, intentions alone, or communication alone, but rather the confluence of high intentions and communication that is most predictive of safer sex. Specifically, people who were high in condom intentions and high in sexual communication reported less unprotected sex with all partners and with at-risk partners over 6 months. Moreover, when sexual communication was low, condom intentions did not predict less unprotected sex.
These results highlight the importance of understanding moderators of the intention-behavior relationship. Although intentions are clearly important for condom use, they do not fully explain behavior for all people. Even highly explanatory models of health behavior, such as Fishbein’s Integrative Model (2008), do not fully specify the skills and abilities that are required to translate intentions into actions. The current work sheds light on the essential moderating role of sexual communication. It is only the people who can express to their partners their desires to use condoms whose behavior is driven by their intentions. These findings are consistent with AIDS specific theories, such as the IBM Model (Fisher and Fisher, 1992) and the AIDS Risk Reduction Model (Catania et al., 1990), which posit that behavioral skills are essential to sexual risk reduction (see also Bryan et al., 2002; Sales et al., 2011). These findings also suggest that variables other than intentions to reduce risks influence whether one will actually engage in risk reduction.
Implications for HIV Prevention Interventions
The current research findings have important implications for HIV prevention interventions. Most notably, results suggest that safer sex is most likely among people who have both high intentions to use condoms and the ability to communicate about sex with their partners. Interventions likely need to address each of these areas to be most successful. We found a sizeable minority of sexually active individuals – just over one quarter of participants - did not have high condom use intentions. For these individuals, enhancing motivation to engage in safer sex will likely be necessary before additional skill building around sexual communication can be implemented. However, for individuals who have strong intentions but lack sexual communication skills, skills training will likely facilitate their abilities to act on their intentions. A pre-assessment could help tailor interventions to individuals, not just to groups. This tailoring may be particularly useful for men who have sex with men, a group that we found to be lower in both sexual communication skills and condom use intentions compared with heterosexual men and women. This individual tailoring can be achieved through interpersonal interventions or, increasingly, through the use of interactive computer technologies that can assess individuals on theoretical determinants and provide individually-tailored feedback and skills training exercises (Noar et al., 2011).
Finally, although several investigators have recognized the importance of including sexual communication skills-building in safer sex interventions (e.g., Edgar et al., 2008; Kelly and Kalichman, 1995), the most effective way to build these skills is unclear. We currently lack a clear understanding about the ways in which people successfully initiate sexual health discussions, how sexual communication skills develop over time and with different partners, and which aspects of communication are most closely associated with practicing safer sex. These knowledge gaps limit our ability to design more effective interventions. We urgently need future research on the sexual communication process, especially among people living with HIV.
Limitations
This research was not without limitations. First, we used an intentional format to measure sexual communication, though it would have been useful to also assess communication with a behavioral format, particularly at the follow-up time point. A meta-analysis of sexual communication demonstrated the behavioral format is more predictive of condom use than the intentional format (effect size r = .29 and .18 for behavior and intentions, respectively; Noar et al., 2006a). Given that we used communication intentions, our results may actually underestimate the effects of sexual communication on sexual behavior. Second, we assessed communication with two items and the reliability between these items was lower than we desired. Research on sexual communication could benefit from a new, reliable sexual communication scale that captures multiple aspects of communication, including content (e.g., condom use, STDs, partner history), quality (e.g., openness, comfort level), and style (e.g., verbal, non-verbal). Third, although we used ACASI to protect confidentiality and minimize reporting biases, our assessment of unprotected sex came through self-report. Since unprotected sex is likely perceived as a socially undesirable, particularly among people living with HIV, some people may have underreported this behavior. Future research could gather data from sexual partners and compare reports of both communication and unprotected sex. Finally, our sample included primarily African American sexually active adults living with HIV in the southeastern United States; it is uncertain how our findings may generalize across other ages, ethnic groups, or regions of the country.
Conclusions
This study sheds new light on the important role of condom use intentions and sexual communication among sexually active people living with HIV. Increasing safer sex motivation and the behavioral skills to communicate openly with sexual partners, particularly partners at risk for HIV, should remain a focus in future interventions. Although openly discussing sexual issues, such as history of HIV/STDs and condom use, is not easy for many people, the ongoing stigma that surrounds HIV may make it even more difficult for people living with HIV to initiate these difficult but important conversations (Smith et al., 2008). Treatment providers and intervention specialists would be wise to recognize these barriers to communication and seek more effective methods of increasing communication abilities.
References
- Abraham C, Sheeran P, Johnson M. From health beliefs to self-regulation: Theoretical advances in the psychology of action control. Psychology and Health. 1998;13:569–591. [Google Scholar]
- Abraham C, Sheeran P, Norman P, Conner M, de Vries N, Otten W. When good intentions are not enough: Modeling postdecisional cognitive correlates of condom use. Journal of Applied Social Psychology. 1999;29:2591–2612. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- Albarracín D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin. 2001;127:142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruhin E. Power, communication and condom use: patterns of HIV-relevant sexual risk management in heterosexual relationships. AIDS Care. 2003;15:389–401. doi: 10.1080/0954012031000105441. [DOI] [PubMed] [Google Scholar]
- Bryan A, Fisher J, Fisher W. Tests of the mediational role of preparatory safer sexual behavior in context of the theory of planned behavior. Health Psychology. 2002;21:71–80. [PubMed] [Google Scholar]
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: An AIDS risk-reduction model (ARRM) Health Education Quarterly. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- Catania JA, Coates TJ, Kegeles S, et al. Condom use in multi-ethnic neighborhoods of San Francisco: The population-based AMEN (AIDS in Multi-Ethnic Neighborhoods) study. American Journal of Public Health. 1992;82:284–287. doi: 10.2105/ajph.82.2.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Sexually Transmitted Disease Surveillance 2009. U.S. Department of Health and Human Services; Atlanta: 2010. [Google Scholar]
- Coleman LM, Ingham R. Exploring young people’s difficulties in talking about contraception: How can we encourage more discussion between partners? Health Education Research. 1999;14:741–750. doi: 10.1093/her/14.6.741. [DOI] [PubMed] [Google Scholar]
- Courtenay-Quirk C, Pals SL, Colfax G, McKirnan D, Gooden L, Eroğlu D. Factors associated with sexual risk behavior among persons living with HIV: Gender and sexual identity group differences. AIDS and Behavior. 2008;12:685–694. doi: 10.1007/s10461-007-9259-y. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Serostatus disclosure, sexual communication and safer sex in HIV-positive men. AIDS Care. 2003;15:379–387. doi: 10.1080/0954012031000105432. [DOI] [PubMed] [Google Scholar]
- Crosby RA, DiClemente RJ, Wingood GM, et al. Condom use and correlates of African American adolescent females’ infrequent communication with sex partners about preventing sexually transmitted diseases and pregnancy. Health Education and Behavior. 2002;29:219–231. doi: 10.1177/109019810202900207. [DOI] [PubMed] [Google Scholar]
- de Vet E, Gebhardt WA, Sinnige J, Van Puffelen A, Van Lettow B, de Wit JBF. Implementation intentions for buying, carrying, discussing and using condoms: The role of the quality of plans. Health Education Research. 2011;26:443–455. doi: 10.1093/her/cyr006. [DOI] [PubMed] [Google Scholar]
- Edgar T, Noar SM, Murphy B. Communication skills training in HIV prevention interventions. In: Edgar T, Noar SN, Freimuth VS, editors. Communication perspectives on HIV/AIDS for the 21st century. Lawrence Erlbaum Associates/Taylor & Francis Group; New York: 2008. pp. 29–66. [Google Scholar]
- Fishbein M. A reasoned action approach to health promotion. Medical Decision Making. 2008;28:834–844. doi: 10.1177/0272989X08326092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV Prevention. Kluwer Academic/Plenum Publishers; New York: 2000. pp. 3–55. [Google Scholar]
- Golin CE, Earp JA, Grodensky CA, et al. Longitudinal effects of SafeTalk, a motivational interviewing-based program to improve safer sex practices among people living with HIV/AIDS. AIDS and Behavior. doi: 10.1007/s10461-011-0025-9. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golin CE, Marks G, Wright J, et al. Psychosocial characteristics and sexual behaviors of people in care for HIV infection: An examination of men who have sex with men, heterosexual men and women. AIDS and Behavior. 2009;13:1129–42. doi: 10.1007/s10461-009-9613-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, Kalichman SC. Increased attention to human sexuality can improve HIV-AIDS prevention efforts: Key research issues and directions. Journal of Consulting and Clinical Psychology. 1995;63:907–918. doi: 10.1037//0022-006x.63.6.907. [DOI] [PubMed] [Google Scholar]
- Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: Implications for HIV prevention programs. Journal of Acquired Immune Deficiency Syndrome. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- Merson M, Padian N, Coates TJ, et al. Combination HIV prevention. Lancet. 2008;372:1805–1806. doi: 10.1016/S0140-6736(08)61752-3. [DOI] [PubMed] [Google Scholar]
- Noar SM. An interventionist’s guide to AIDS behavioral theories. AIDS Care. 2007;19:392–402. doi: 10.1080/09540120600708469. [DOI] [PubMed] [Google Scholar]
- Noar SM, Carlyle K, Cole C. Why communication is crucial: Meta-analysis of the relationship between safer sexual communication and condom use. Journal of Health Communication: International Perspectives. 2006a;11:365–390. doi: 10.1080/10810730600671862. [DOI] [PubMed] [Google Scholar]
- Noar SM, Cole C, Carlyle K. Condom use measurement in 56 studies of sexual risk behavior: Review and recommendations. Archives of Sexual Behavior. 2006b;35:327–345. doi: 10.1007/s10508-006-9028-4. [DOI] [PubMed] [Google Scholar]
- Noar SM, Morokoff PJ, Redding CA. Sexual assertiveness in heterosexually active men: A test of three samples. AIDS Education and Prevention. 2002;14:330–342. doi: 10.1521/aeap.14.5.330.23872. [DOI] [PubMed] [Google Scholar]
- Noar SM, Webb EM, Van Stee SK, et al. Using computer technology for HIV prevention among African Americans: Development of a tailored information program for safer sex (TIPSS) Health Education Research. 2011;26(3):393–406. doi: 10.1093/her/cyq079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sales JM, Lang DL, DiClemente RJ, et al. [accessed online 10 November 2011];The mediating role of partner communication frequency on condom use among African American adolescent females participating in an HIV prevention intervention. Health Psychology. 2011 doi: 10.1037/a0025073. 00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: A meta-analysis. Psychological Bulletin. 1999;125:90–132. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- Smith RA, Rossetto KR, Peterson BL. A meta-analysis of disclosure of one’s HIV+ status, stigma, and social support. AIDS Care. 2008;20:1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- Thompson KL, Geher G, Stevens KF, Stem ST, Lintz MK. Psychological predictors of sexual behaviors related to AIDS transmission. Psychological Reports. 2001;88:51–67. doi: 10.2466/pr0.2001.88.1.51. [DOI] [PubMed] [Google Scholar]
- Widman L, Welsh DP, McNulty JK, Little KC. Sexual communication and contraceptive use in adolescent dating couples. Journal of Adolescent Health. 2006;39:893–899. doi: 10.1016/j.jadohealth.2006.06.003. [DOI] [PubMed] [Google Scholar]