Abstract
Objectives
To evaluate the complications, and visual and graft survival outcomes in eyes that had undergone penetrating keratoplasty (PKP) for keratoconus.
Methodology
This restrospective study includes 311 patients with keratoconus who had undergone PKP between January 1, 2001, and December 31, 2002, at King Khaled Eye Specialist Hospital. All patients were followed up postoperatively (maximum follow-up, 65.77 months).
Results
The mean age of patients with keratoconus at transplantation was 23.72 years. A preoperative best spectacle-corrected visual acuity (BSCVA) OF 20/40 or better was achieved in 13 eyes (4.2%). At a mean follow-up of 27 months, 212 eyes (68.2%) achieved a BSCVA of 20/40 or better. Postoperative visual acuity was significantly associated with preoperative visual acuity (P < 0.00). Only 6 eyes (1.9%) experienced graft failure, with a mean follow-up of 23.62 months. The graft rejection rate (6.8%) was a significant risk factor for failure (P = 0.00). Age, gender, corneal graft diameter, and intraoperative vitreous loss had no statistically significant effects on the PKP outcome (P> 0.05). Kaplan-Meier analysis revealed that the probabilities of graft survival were 99.8% at 1 year and 97.6% at 5 years after transplantation.
Conclusion
Performing PKP in eyes with keratoconus is associated with good visual results and an excellent graft outcome.
Keywords: penetrating keratoplasty, keratoconus, graft failure
Introduction
In keratoconus, the cornea progressively thins and steepens, leading to the development of myopia and irregular astigmatism and, eventually, to the loss of best spectacle-corrected visual acuity (BSCVA); this noninflammatory ecstatic corneal disorder occurs naturally and is characterized as bilateral but asymmetrical. (1) Various therapeutic modalities for this disorder exist, including spectacles, contact lenses, lamellar keratoplasty (LK), penetrating keratoplasty (PKP), and, recently, intracorneal rings (ICRs). (1, 2) The type of treatment chosen depends on the severity of the disorder. In patients with keratoconus who have contact lens failure or apical scarring, PKP is a well-accepted treatment. (2, 3) Previous researches have revealed that keratoconus is one of the leading indications for corneal transplantation in Saudi Arabia and throughout the world. (3, 13) The purpose of this retrospective study is to determine the outcomes of a series of consecutive PKPs performed for patients with keratoconus at King Kahled Eye Specialist Hospital in Riyadh, Saudi Arabia.
Methods
After approval was obtained from the Institutional Review Board, a retrospective review was conducted of the medical records of all patients with keratoconus who had undergone PKP from January 1, 2001, through December 31, 2002, at King Khaled Eye Specialist Hospital. All patients included in this retrospective review had been followed up for a minimum period of 2 months. Members of the Anterior Segment Division in the Department of Ophthalmology at King Khaled Eye Specialist Hospital performed all surgeries. Patients were clinically diagnosed as having keratoconus based on history and results from slit-lamp examination, keratometry, corneal topography, and refraction. Poor functional vision and intolerance of other methods of optimal optical correction (eg, spectacles, rigid gas permeable contact lenses) were indications for corneal graft surgery in all patients. Following surgery, patients were administered topical corticosteroids (Prednisolone acetate 1%) and antibiotics at tapered dosages. After about 2 to 4 weeks, the administration of topical antibiotics was discontinued. Based on the clinical outcome, patients underwent a gradual taper from topical steroids over at least a 6-month period. Most patients were evaluated on the first postoperative day; after 1 week; after 1, 3, 6, 9, 12, 18, and 24 months; and annually thereafter. Treating ophthalmologists either removed all sutures after 12 to 36 months or only selectively removed loose or tight sutures that induced unacceptable levels of postoperative astigmatism. Data from the medical records included demographic data, preoperative best spectacle-corrected visual acuity (BSCVA), previous medical and surgical procedures, graft rejection episodes, graft clarity, visual acuity (VA), and follow-up interval. Graft survival and VA were the primary outcome measures. Patients with an irreversible loss of central graft clarity (regardless of the VA measurement) were identified as experiencing graft failure. The follow-up period for patients with grafts that remained clear was the length of time between surgery and the most recent examination. For patients with grafts that failed, the follow-up period was the length of time between surgery and the first visist when irreversible loss of central graft clarity was recorded. Measurements of VA were recorded preoperatively and at the most recent examination using snellen chart. If available, measurements of BSCVA were used for statistical analysis; in those cases in which measurements of BSCVA were not available, uncorrected VA measurements (considered equivalent to BSCVA) were used instead. The time of graft failure was the postoperative visit at which irreversible loss of graft clarity was first recorded. Graft failures caused by endothelial decompensation were categorized as immunologic rejections if a graft rejection episode had been recorded and if factors contributing to endothelial attrition had not been detected. All data were entered into Statistical Product and Service Solutions (SPSS) software (version 17.0) for analysis. Descriptive statistics were used to calculate mean ± SD values for numeric variables. The chi square test was used for analysis of variance. The Kaplan-Meier method was performed to analyze graft survival. Nominal P values were used for all comparison. Results were considered statistically significant if P ≤ 0.05.
Results
Of the 311 patients with keratoconus who underwent PKP, there were 199 men (64.0%) and 112 women (36.0%). In 145 cases (46.6%), the procedure was performed on the right eye, and in 166 cases (53.4%) on the left eye. The mean age at time of surgery was 23.72 years (range, 10–62 years; SD, 6.39). The mean period of follow-up after PKP was 40.67 months (range, 2.10–65.77 months; SD, 14.45). Five patients had previously undergone cataract extraction surgery. The mean host corneal bed size was 7.44 mm (median, 7.50 mm; range, 6.0–8.30 mm), and the mean donor corneal button size was 7.68 mm (median, 7.75 mm; range, 6.0–8.5 mm). The most common host corneal bed sizes were 7.50 mm, used in 160 eyes (51.45%), and 7.00 mm, used in 74 eyes (23.8%). The most common donor graft button sizes were 7.75 mm, used in 154 eyes (49.52%), and 7.25 mm and 7.50 mm, used in 53 eyes (17.0%) and 41 eyes (13.18%), respectively. Graft-host disparity was ≤0.25 mm in 286 eyes (92.0%), and >0.25 mm in 25 eyes (8.0%) (Table 1). Surgical procedures had previously been performed on 10 eyes (3.2%) (5 cataract surgeries, 7 others). At the time of PKP, concomitant cataract extraction and intraocular lens (IOL) implantation were performed on only 1 patient; planned surgical iridotomy was also performed on 2 patients.
Table (1).
Demographic and Clinical Features of Patients With Keratoconus Who Underwent Penetrating Keratoplasty (PKP)
| Variables | Clear Graft | Failed Graft | Total N | P |
|---|---|---|---|---|
| Gender, n (%) | ||||
| Male | 194 (97.5) | 5.0 (2.5) | 199 | 0.319 |
| Female | 111 (99.1) | 1.0 (0.9) | 112 | 0.137 |
| Eye,n (%) | ||||
| Right | 144 (99.3) | 1.0 (0.7) | 145 | |
| Left | 161 (97.0) | 5.0 (3.0) | 166 | |
| Age, y | ||||
| Mean | 23.67 | 26.3 | ||
| Age at surgery, y,n(%) | ||||
| ≤15 | 21 (95.45) | 1 (4.55) | 22 | 0.223 |
| 16–19 | 34 (94.44) | 2 (5.60) | 36 | |
| 20–24 | 137 (99.3) | 1 (0.72) | 138 | |
| ≥25 | 113 (98.3) | 2 (1.7) | 115 | |
| Follow-up, months | ||||
| Mean | 41 | 23.62 | >0.05 | |
| Range | 2.1–65.7 | 2.6–44.73 | ||
| Recipient bed diameter, mm | ||||
| Mean | 7.44 | 7.58 | ||
| Range | 6.0–8.25 | 7.5–8.00 | ||
| Donor graft diameter, mm | ||||
| Mean | 7.68 | 7.87 | ||
| Range | 6.0–8.50 | 7.75–8.25 | ||
| Lens status,n(%) | ||||
| Pseudophakia | 5.0 (83.3) | 1.0 (16.7) | 6 | 0.008 |
| Phakia | 300 (98.4) | 5.0 (1.6) | 305 | |
| Recipient size,n(%) | ||||
| ≤7.5 mm | 248 (98.0) | 5.0 (2.0) | 253 | >0.05 |
| >7.5 mm | 57 (98.3) | 1.0 (1.7) | 58 | |
| Previous surgery,n(%) | 5.0 (100) | 0.0 (0.00) | 5 | 0.652 |
| Additional surgery,n(%) | ||||
| Cataract surgery | 0.0 (0.00) | 1.0 (100) | 1 | 0.00 |
| Others | 2.0 (100) | 0.0 (0.00) | 2 | |
| Previous glaucoma,n(%) | 2.0 (100) | 0.0 (0.00) | 2 | 0.842 |
| Glaucoma escalation,n(%) | 7.0 (100) | 0.0 (0.00) | 7 | 0.707 |
| Rejection,n(%) | 19 (90.5) | 2.0 (9.5) | 21 | 0.009 |
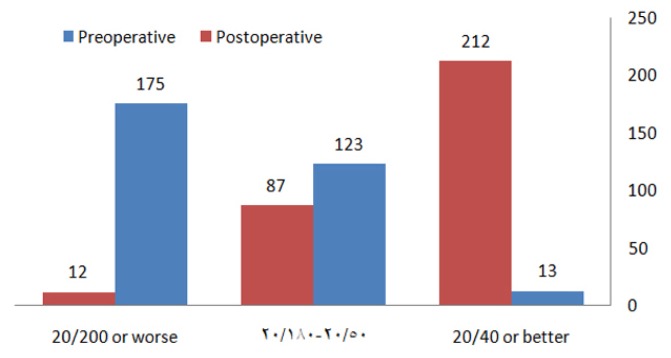
At the last follow-up visit, 212 eyes (68.2%) had a BCVA of 20/40 or better, 87 eyes (28.0%) were between 20/50 and 20/180, and 12 eyes (3.9%) were 20/200 or worse. Table 2 shows a statistically significant difference between preoperative and postoperative BCVA
Table (2).
Comparison Between Preoperative and Postoperative Best spectacle-corrected Visual Acuity (BSCVA)
| Preoperative BSCVA | Postoperative BSCVA | ||||
|---|---|---|---|---|---|
| n (%) | Cumulative % | n (%) | Cumulative % | P | |
| 20/40 or better | 13 (4.2) | 4.2 | 212 (68.2) | 68.2 | 0.000 |
| 20/50-20/180 | 123 (39.5) | 43.7 | 87 (28.0) | 96.2 | |
| 20/200 or worse | 175 (56.3) | 100.0 | 12 (3.8) | 100.0 | |
Discussion
The number of keratoconus surgeries being performed in Saudi Arabia is rising. This rise has been attributed to population explosion, better patient access, improved healthcare availability, and an increased availability of grafts. (7) The demographic data for patients with keratoconus who underwent PKP in the present study are generally consistent with those from previous reports. (14–16) In this study, PKP was performed in relatively young patients (mean age was 23.72 years at the time of PKP), with a male predominance of 64.0%. In a study by Javadi et al, (16) the mean age at the time of surgery was 28.2 years, with values of patients (P = 0.00) (Figure 1). All eyes with graft failure had VA values that were equal to or less than 20/200.
Fig. (1).
Distribution of best spectacle-corrected visual acuity (BCVA) comparing preoperative and postoperative vision.
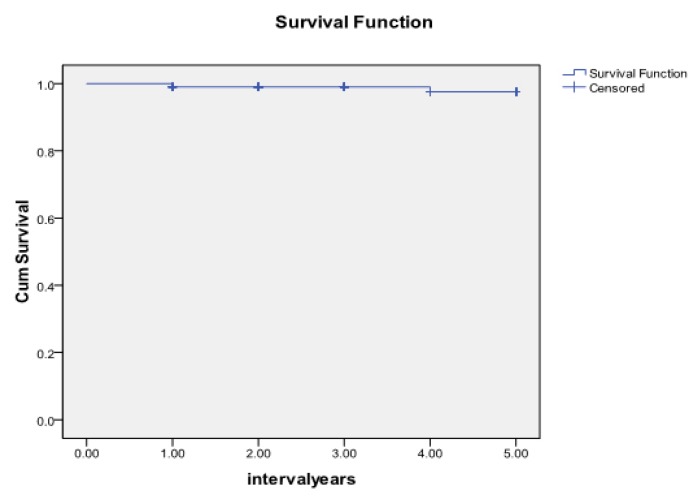
At the most recent visit, 305 grafts (98.1%) were clear, and only 6 grafts (1.9%) had failed. The mean time to graft failure was 23.62 months (range, 2.63–44.7 months) after transplantation. The overall probabilities of graft survival were 99.8% at 1 year and 97.6% at 5 years (Figure 2). At least one episode of a rejection reaction occurred in 21 eyes (6.8%) of 311 eyes, with 3 eyes (0.96%) developing irreversible graft failure (P = 0.009). Of 218 eyes with a recipient size of ≥7.5 mm, 15 eyes (6.9%) developed a graft rejection episode compared with 6 eyes (6.45%) of 93 eyes with a recipient size of <7.5 mm, which is not statistically significant (P > 0.05).
Fig. (2).
Kaplan-Meier cumulative survival proportion curve showing graft survival after penetrating keratoplasty (PKP) procedure in patients with keratoconus.
Logistic regression with adjustment for intereye dependence revealed that age (hazard ratio, 1.05; 95% confidence interval [CI], 0.95–1.18; P = 0.33), gender (hazard ratio, 3.4; 95% CI, 0.38–30.12; P = 0.28), recipient size (hazard ratio, 2.73; 95% CI, 0.24–31.50; P = 0.422), and postoperative glaucoma (hazard ratio, 0.00; P = 0.99) were not significantly associated with graft failure. A significant association was found between rejection and graft failure (hazard ratio, 7.86; 95% CI, 1.27–48.66; P = 0.027). None of the eyes had cataract. At a mean time of 28 months after surgery, 7 eyes (2.3%) developed glaucoma escalation; however, none of these patients had a family history of glaucoma or had a failed graft. Control of intraocular pressure was achieved with the administration of topical medications in 7 eyes, and only 1 eye required a trabeculectomy.
73.2% of patients being male. However, de Lavalette et al (17) reported a female predominance of 65% in their study. Various studies have reported that keratoconus has an equal prevalence in both genders, (1, 18) a greater prevalence in males, (14–16, 19) and a greater prevalence in females. (20) One possible reason for the increased relative frequency of male subjects undergoing transplantation compared with female subjects is an increased tendency for males to receive surgical treatment so as to improve occupational performance.
The graft survival rate of 98.1% in this series compares favorably to the results of previous series. (14–17,21,22) In a previous series of 90 consecutive PKPs performed in eyes with keratoconus and vernal keratoconjunctivitis between 1986 and 1996 in Saudi Arabia, 83 grafts (92.2%) were clear after a mean follow-up period of 44.7 months.(22) Price et al(21) found a 5-year graft survival rate of 98% among patients who underwent PKP for keratoconus. In the present study, complications other than graft rejection were not significantly related to graft failure after PKP (P = 0.511). Of the 311 eyes in this study, 21 eyes (6.8%) had rejection episodes, and 3 eyes (0.96%) developed irreversible graft failure. This rate of rejection episodes is lower than in other series. For instance, Watson et al (23) reported 11 rejection episodes in 22 patients who underwent PKP, and Troutman and Lawless (8) reported a rejection rate of 18.5%. There was no significant difference in graft failure rates between male and female patients in any age group. In the current series, donor-recipient disparity had no effect on survival outcome.
The prognosis for graft survival in patients with keratoconus is considered excellent if surgery is performed on young patients who are highly motivated and compliant and who do not have other conditions that compromise visual potential (eg, age-related retinal disease). The 5-year Kaplan-Meier survival rate in the present series of 97.6% is comparable to those of other series.(24,25) Age, gender, and recipient size did not contribute to an increased risk of graft failure after PKP in the present study’s patients.
The mean BSCVA at the last visit was 20/30, which is within the range of 20/25 to 20/32 in other published series. Sayegh et al(26) and Brierly et al(4) reported similar results. In the present study, 68.2% of patients achieved 20/40 or better following surgery, which compares favorably with rates of 47% to 91% reported in the literature. (22–30) Mahmood and Wagoner (22) found that 55 eyes (61.1%) achieved a BCVA of 20/40 or better, and Claesson et al(27) reported that 47% of patients with keratoconus achieved a BSCVA of 20/40 or better. A study by Funnell et al (28) reported that the majority (85%) of subjects achieved a binocular VA of 20/40 or better following surgery at 12 months. In addition, Lim et al (29) reported that 87% of keratoconic eyes achieved 20/40 or better following PKP, with a mean follow-up of 56.5 months.
The incidence of successful 20/40 VA was not significantly affected by graft rejections. Only 2 patients who had experienced an episode of rejection had a VA worse than 20/60. These findings may indicate that an adverse effect on VA cannot be attributed to a rejection episode that has been successfully treated.
In summary, PKP is associated with a good visual outcome and prognosis for graft survival with a low complication rate in eyes with keratoconus.
Footnotes
The author does not have any proprietary interest or conflict of interest with respect to any equipment or products mentioned in this paper.
Research was carried out in the Department of Anterior Segment, King Khaled Eye Specialist Hospital, P.O. Box 7191, Riyadh 11462, Kingdom of Saudi Arabia
References
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Tan DT, Por YM. Current treatment options for corneal ectasia. Curr Opin Ophthalmol. 2007;18:284–89. doi: 10.1097/ICU.0b013e3281a7ecaa. [DOI] [PubMed] [Google Scholar]
- 3.Kelly TL, Williams KA, Coster DJ the Australian Corneal Graft Registry. Corneal transplantation for keratoconus: a registry study. Arch Ophthalmol. 2011;129(6):691–97. doi: 10.1001/archophthalmol.2011.7. [DOI] [PubMed] [Google Scholar]
- 4.Brierly SC, Izquierdo L, Jr, Mannis MJ. Penetrating keratoplasty for keratoconus. Cornea. 2000;19:329–32. doi: 10.1097/00003226-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Doyle SJ, Harper C, Marcyniuk B, Ridgway AEA. Prediction of refractive outcome in penetrating keratoplasty for keratoconus. Cornea. 1996;15:441–45. [PubMed] [Google Scholar]
- 6.Edwards M, Clover GM, Brookes N, Pendergrast D, Chaulk J, McGhee CN. Indications for corneal transplantation in New Zealand: 1991–1999. Cornea. 2002;21:152–55. doi: 10.1097/00003226-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Al-Towerki AE, Gonnah el-S, Al-Rajhi A, Wagoner MD. Changing indications for corneal transplantation at the King Khaled Eye Specialist Hospital (1983–2002) Cornea. 2004;23:584–88. doi: 10.1097/01.ico.0000121708.58571.5b. [DOI] [PubMed] [Google Scholar]
- 8.Troutman RC, Lawless MA. Penetrating keratoplasty for keratoconus. Cornea. 1987;6:298–305. doi: 10.1097/00003226-198706040-00013. [DOI] [PubMed] [Google Scholar]
- 9.Lawless MA, Troutman RC. The role of penetrating keratoplasty and epikeratoplasty in the surgical management of keratoconus. Aust N Z J Ophthalmol. 1989;17:387–93. doi: 10.1111/j.1442-9071.1989.tb00559.x. [DOI] [PubMed] [Google Scholar]
- 10.Cosar CB, Sridhar MS, Cohen EJ, et al. Indications for penetrating keratoplasty and associated procedures, 1996–2000. Cornea. 2002;21:148–51. doi: 10.1097/00003226-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Chen WL, Hu FR, Wang IJ. Changing indications for penetrating keratoplasty in Taiwan from 1987 to 1999. Cornea. 2001;20(2):141–44. doi: 10.1097/00003226-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Siganos CS, Tsiklis NS, Miltsakakis DG, et al. Changing indications for penetrating keratoplasty in Greece, 1982–2006: a multicenter study. Cornea. 2010;29(4):372–74. doi: 10.1097/ICO.0b013e3181bd44a1. [DOI] [PubMed] [Google Scholar]
- 13.Kanavi MR, Javadi MA, Sanagoo M. Indications for penetrating keratoplasty in Iran. Cornea. 2007;26(5):561–63. doi: 10.1097/ICO.0b013e318041f05c. [DOI] [PubMed] [Google Scholar]
- 14.Sharif KW, Casey TA. Penetrating keratoplasty for keratoconus: complications and long-term success. Br J Ophthalmol. 1991;75:142–46. doi: 10.1136/bjo.75.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pramanik S, Musch DC, Sutphin JE, Farjo AA. Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology. 2006;113:1633–38. doi: 10.1016/j.ophtha.2006.02.058. [DOI] [PubMed] [Google Scholar]
- 16.Javadi MA, Motlagh BF, Jafarinasab MR, et al. Outcomes of penetrating keratoplasty in keratoconus. Cornea. 2005;24(8):941–46. doi: 10.1097/01.ico.0000159730.45177.cd. [DOI] [PubMed] [Google Scholar]
- 17.De Lavalette JG, de Lavalette AR, van Rij G, Beekhuis WH, de Beijer-Dominicus JA. Long-term results of corneal transplantations in keratoconus patients. Doc Ophthalmol. 1985;59:93–97. doi: 10.1007/BF00162016. [DOI] [PubMed] [Google Scholar]
- 18.Li X, Rabinowitz YS, Rasheed K, Yang H. Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology. 2004;111:440–46. doi: 10.1016/j.ophtha.2003.06.020. [DOI] [PubMed] [Google Scholar]
- 19.Wagner H, Barr JT, Zadnik K. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study: methods and findings to date. Cont Lens Anterior Eye. 2007;30:223–32. doi: 10.1016/j.clae.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stein HA, Stein RM, Freeman MI. The Ophthalmic Assistant: A Text for Allied and Associated Ophthalmic Personnel. 8th ed. Canada: Elsevier Mosby; 2006. p. 396. [Google Scholar]
- 21.Price FW, Jr, Whitson WE, Marks RG. Graft survival in four common groups of patients undergoing penetrating keratoplasty. Ophthalmology. 1991;98:322–28. doi: 10.1016/s0161-6420(91)32292-9. [DOI] [PubMed] [Google Scholar]
- 22.Mahmood MA, Wagoner MD. Penetrating keratoplasty in eyes with keratoconus and vernal keratoconjunctivitis. Cornea. 2000;19:468–70. doi: 10.1097/00003226-200007000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Watson SL, Ramsay A, Dart JKG, Bunce C, Craig E. Comparison of deep lamellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology. 2004;111(9):1676–82. doi: 10.1016/j.ophtha.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 24.Dong XG, Xie LX. Evaluation of penetrating keratoplasty for the treatment of keratoconus [in Chinese; English abstract] Zhonghua Yan Ke Za Zhi. 1992;28:144–46. [PubMed] [Google Scholar]
- 25.Inoue K, Amano S, Oshika T, Sawa M, Tsuru T. A 10-year review of penetrating keratoplasty. Jpn J Ophthalmol. 2000;44:139–45. doi: 10.1016/s0021-5155(99)00190-2. [DOI] [PubMed] [Google Scholar]
- 26.Sayegh FN, Ehlers N, Farah I. Evaluation of penetrating keratoplasty in keratoconus. Nine years follow-up. Acta Ophthalmol (Copenh) 1988;66:400–03. doi: 10.1111/j.1755-3768.1988.tb04030.x. [DOI] [PubMed] [Google Scholar]
- 27.Claesson M, Armitage WJ, Olsson-Abdellatif K, Sargent N. Corneal transplant outcome in the Palestinian territories: a 2-year follow-up study. Eye (Lond) 2009;23:1423–26. doi: 10.1038/eye.2008.263. [DOI] [PubMed] [Google Scholar]
- 28.Funnell CL, Ball J, Noble BA. Comparative cohort study of the outcomes of deep lamellar keratoplasty and penetrating keratoplasty for keratoconus. Eye (Lond) 2006;20(5):527–32. doi: 10.1038/sj.eye.6701903. [DOI] [PubMed] [Google Scholar]
- 29.Lim L, Pesudovs K, Coster DJ. Penetrating keratoplasty for keratoconus: visual outcome and success. Ophthalmology. 2000;107(6):1125–31. doi: 10.1016/s0161-6420(00)00112-3. [DOI] [PubMed] [Google Scholar]
- 30.Han DC, Mehta JS, Por YM, Htoon HM, Tan DT. Comparison of outcomes of lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2009;148(5):744–51. doi: 10.1016/j.ajo.2009.05.028. [DOI] [PubMed] [Google Scholar]