Abstract
Objectives. In this study a new method for asthma outcome prediction, which is based on Principal Component Analysis and Least Square Support Vector Machine Classifier, is presented. Most of the asthma cases appear during the first years of life. Thus, the early identification of young children being at high risk of developing persistent symptoms of the disease throughout childhood is an important public health priority. Methods. The proposed intelligent system consists of three stages. At the first stage, Principal Component Analysis is used for feature extraction and dimension reduction. At the second stage, the pattern classification is achieved by using Least Square Support Vector Machine Classifier. Finally, at the third stage the performance evaluation of the system is estimated by using classification accuracy and 10-fold cross-validation. Results. The proposed prediction system can be used in asthma outcome prediction with 95.54 % success as shown in the experimental results. Conclusions. This study indicates that the proposed system is a potentially useful decision support tool for predicting asthma outcome and that some risk factors enhance its predictive ability.
1. Introduction
Asthma is a chronic inflammatory disorder of the airways characterized by an obstruction of airflow, which may be completely or partially reversed with or without specific therapy [1]. Airway inflammation is the result of interactions between various cells, cellular elements, and cytokines. In susceptible individuals, airway inflammation may cause recurrent or persistent bronchospasm, with symptoms like wheezing, breathlessness, chest tightness, and cough, particularly at night or after exercise. Asthma is a disease with polymorphic phenotype affected by several environmental and genetic factors which both play a key role in the development and persistence of the disease [2, 3]. Among these factors family history of asthma, presence of atopic dermatitis or allergic rhinitis, wheezing episodes during childhood, maternal smoking during pregnancy, and several prenatal and environmental factors are included [4–7].
Most children who suffer from asthma develop their first symptoms before the 5th year of age [8]. However, it is difficult to discriminate asthma from other wheezing disorders of the childhood because the symptoms are similar. Thus, children with asthma may often be misdiagnosed as having a common cold, bronchiolitis, or pneumonia. For the diagnosis of asthma a detailed medical history and physical examination along with a lung function test is usually required. On the other hand, lung function test is hard to be performed in children younger than five years old.
In preventive medicine, the value of a test lies in its ability to identify those individuals who are at high risk of an illness and who therefore require intervention while excluding those who do not require such intervention. The accuracy of the risk classification is of particular relevance in the case of asthma disease. Early identification of patients at high risk for asthma disease progression may lead to better treatment opportunities and hopefully better disease outcomes in adulthood [9–13].
Several efforts have been made by different groups to discover a safe way of prediction of asthma outcome such as asthma index API or modified asthma index mAPI in children younger than five years old [14, 15]. To the knowledge of the authors, this is the first study where machine learning techniques are used in the prediction of persistent asthma. However, Principal Component Analysis (PCA) has been used in several medical studies as for instance to evaluate the multivariate association between functional microvascular variables and clinical-laboratorial-anthropometrical measurements [16]. Moreover, in the study of [17], multivariate projection techniques have been utilized to reveal how inflammatory mediators demonstrate a distinct pattern of response to traumatic brain injury in humans. Finally, in [18], PCA was used for Gait Kinematics Data in Acute and Chronic Stroke Patients. Least Square Support Vector Machine (LSSVM) classifiers have been used with success for diagnosis of lung cancer [19] and in a hepatitis diagnosis system [20].
PCA provides a powerful method for exploring complex datasets with multiple variables and missing data points with relatively small numbers of observations [21]. LSSVM is a robust and reliable classifier system and has the ability to perform fast classification. For these reasons, those two techniques have been chosen for this study [22].
In this paper an intelligent system approach for asthma prediction outcome is presented. The system consists of three stages: (a) feature extraction and reduction through PCA, (b) pattern classification by using LSSVM classifier, and (c) the performance evaluation of the classifier by means of accuracy, sensitivity, specificity, and 10-fold cross validation. The paper is organized as follows. Section 2.1 presents the experimental dataset which has been used for this study. In Section 2.2 brief description of the PCA is shown, while in Section 2.3 the LSSVM classifier is introduced. In Section 2.4 the proposed prediction system is presented, while the results are shown in Section 3. The discussion and the final conclusions are described in Sections 4 and 5, respectively.
2. Methods
2.1. Clinical Data
Data from 148 patients from the Pediatric Department of the University Hospital of Alexandroupolis, Greece were collected during the period 2008–2010 and recorded. A group of 148 patients who received a diagnosis of asthma were studied prospectively from the 7th to 14th year of age. All patients with missing data were excluded from the present study, leaving a total of 112 patients.
A case history, including data on asthma, allergic diseases, and lifestyle factors was obtained by questionnaires. The participants (parents and their children) answered questions regarding asthmatic and allergic symptoms, wheezing episodes until the 5th year, pet keeping, family members, parental history, and some other useful information. The prognostic factors that were used in the questionnaire have been derived from previous studies [2–10]. A total of 46 prognostic factors have been considered and they are summarized in Table 1. For some of them a kind of encoding was required in order to be efficiently utilized for the current investigation. Their encoding is presented in Table 2.
Table 1.
Prognostic factors.
| Category | Prognostic factors |
|---|---|
| Demographic | age, sex, ethnicity#, height, weight, waist's perimeter, residence# |
| Wheezing episodes | until 3rd year, between 3rd and 5th year |
| Symptoms | wheezing*, cough*, allergic rhinitis*, runny nose*, congestion*, eczema*, food allergy*, pharmaceutical allergy*, allergic conjunctivitis*, dyspnea*, seasonal symptoms# |
| Parental history | asthma* |
| House conditions | number of family members, pets*, type of heating# |
| Pharmaceutical therapy | bronchodilators, corticosteroids inhaled*, corticosteroids per os*, antileukotriene*, antihistamine* |
| Breathing tests | FEV1%, FEF25/75% |
| Tests | Ig E U/Ml |
| Allergens | d. pteronyssinus #, d. farinae #, olive#, pellitory#, graminaceae#, pine#, cypress#, cat#, dog#, alternaria # |
| Neonatal period | pregnancy duration, breastfeeding duration#, smoking during pregnancy* |
| Asthma | treatment* |
*The encoding is binary: yes (1) or no (0).
#The encoding is shown in Table 2.
All other factors are numerical.
Table 2.
Encoding of some prognostic factors.
| Prognostic factor | Coding | |||||
|---|---|---|---|---|---|---|
| Sex | 0 (Male) | 1 (Female) | ||||
| Residence | 0 (Urban) | 1 (Semiurban) | 2 (Rural) | |||
| Season of the symptoms | 0 (None) | 1 (Winter) | 2 (Autumn) | 3 (Spring) | 4 (Summer) | 5 (>2 Seasons) |
| Type of heating | 0 (Central heating) |
1 (Wood stove) |
2 (Oil stove) |
3 (Fireplace) | 4 (Central heating + Fireplace) |
|
| Pregnancy duration in weeks | 0 (<37) | 1 (37-38) | 2 (>38) | |||
| Allergens | 0 (0) | 1 (3.5–6 mm) | 2 (>6 mm) | |||
2.2. Principal Component Analysis for Feature Reduction
In the present study, the dimension of the input vector is large, while at the same time the components of the vectors are strongly correlated. It is, therefore, useful in this case to reduce the dimension of the input vectors. An effective procedure to perform this operation is to employ the PCA method. This technique has three effects: it orthogonalizes the components of the input vectors so that they are uncorrelated with each other, it sorts the resulting orthogonal components (principal components) so that those with the largest variation come first, and, finally, it eliminates those components that contribute the least to the variation in the data set [23].
According to the literature [24], the most common definition of PCA is that for a set of observed vectors {v i}, i ∈ {1,2,…, N}, the q principal axes w j, j ∈ {1,2,…, q} are those orthonormal axes onto which the retained variance under projection is maximal. It can be shown that the vectors w j are given by the q dominant eigenvectors (i.e., those with largest associated eigenvalues) of the covariance matrix
| (1) |
such that Cw j = λ i w j, where is the simple mean value and λ i is a scalar, termed the eigenvalue corresponding to w j.
The vector , where W = (w 1, w 2,…, w q), is a q-dimensional reduced representation of the observed vector ν i [25].
2.3. Least Square Support Vector Machine Classifier
Support Vector Machine (SVM) is a classification and regression prediction tool that uses machine learning theory to maximize predictive accuracy while automatically avoiding over-fit to the data. The foundations of SVMs have been developed by Vapnik [26] and gained popularity due to many promising features. SVMs perform classification by constructing an N-dimensional hyperplane that optimally separates the data into two categories. The goal of SVM is to produce a model in the form of f(x) = ω T x + b which predicts the target values of the test data given only the test data attributes. The training set {x i,y i}i=1 l, where x i ∈ ℜ n is the input and y i ∈ {−1, +1} is the output, shows the class.
The Representer Theorem [27] states that the solution ω can always be written as a linear combination of the training data:
| (2) |
In that way, the SVM can be formulated to learn a linear classifier
| (3) |
by solving an optimization problem over a i, where a i are Lagrange, b is a real constant, and N is the size of the training data.
K(x i, x j) is a nonlinear kernel function given by K(x i, x j) = φ(x i)T φ(x j), where φ(x) is the nonlinear map from original space to the high dimensional space.
The SVM classifiers solve the following quadratic programming problem:
| (4) |
subject to y i(ω T ϕ(x i) + b) = 1 − ξ i, ξ i ≥ 0, i = 1,…, N, ξ i represents the degree of misclassification of the data x i and C is the penalty parameter of the error term [28].
In this paper the least squares version of SVM is used, whose main advantage is that it is computationally more efficient than the standard SVM method. In this case the training process requires the solution of a linear equation set instead of the quadratic programming problem involved by the standard SVM. The LSSVM method—when Radial Basis Function (RBF) kernels are used—requires only two parameters (C and σ), while the time consumed by the training method is reduced, by replacing the quadratic optimization problem with a simple linear equation set [29]. In LSSVMs, an equality constraint-based formulation is made within the context of ridge regression as follows:
| (5) |
subject to y i(ω T ϕ(x i) + b) = 1 − e i, i = 1,…, N.
2.4. The Intelligent PCA-LSSVM Prediction System
The asthma prediction system which is presented in this study consists of three stages: (i) the feature extraction and dimension reduction through PCA, (ii) the pattern classification by employing LSSVM classifier, and (iii) the performance evaluation by using classification accuracy, sensitivity, specificity, and 10-fold cross-validation. The flowchart of the intelligent system for asthma prediction is illustrated in Figure 1. The implementation steps of the algorithm follow a certain sequence. First of all, the patient's data were collected and prepared in an electronic form suitable for further processing. After this step, all the parameters (where it is necessary) were encoded and the outputs were assigned either with label 1 (asthma persistence) or 0 (no asthma persistence). At last, the dimension of the dataset which had 46 features was reduced to 18 features using the PCA method.
Figure 1.
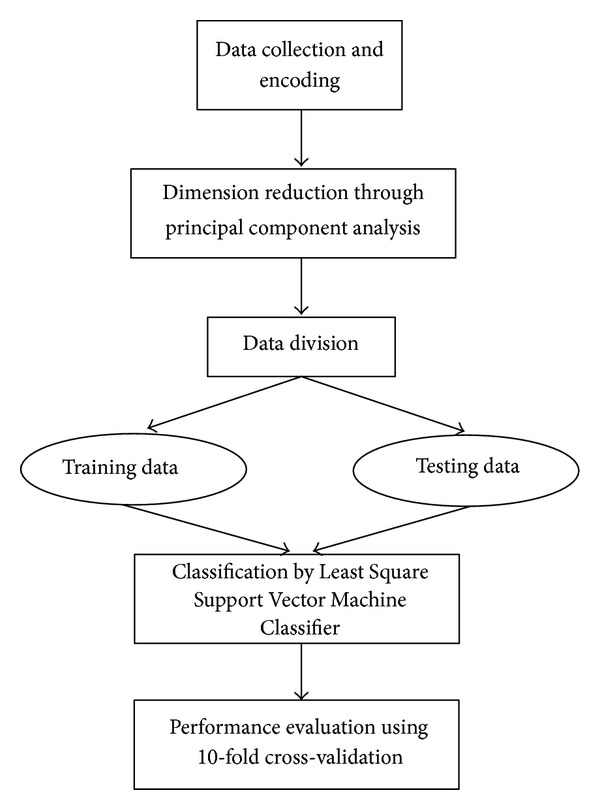
Flowchart diagram of the proposed intelligent system for asthma prediction.
In the classification stage of PCA-LSSVM intelligent prediction system, the reduced features obtained from the first stage were fed to the LSSVM classifier. LSSVM classifiers parameters, which are σ (the width of RBF kernel) and margin-losses trade-off C, affect the prediction performance. The best combination of C and σ was selected by the grid search with growing sequences of C (1–1000 with a step equals 10) and σ (1–100 with a step equals 1). Each combination of parameter choices was checked using 10-fold cross-validation. At first, the 112 patients were divided into 10 almost equal subgroups. One of the 10 subgroups has been used as the evaluation data and the rest as the learning data for the classification. The evaluation data were changed 10 times, so that each group was investigated once as evaluation data. The average value of all obtained accuracies of the evaluation data was considered as the estimation ability of the model. The parameters with best cross-validation accuracy were picked.
3. Results
The experimental results are presented in terms of accuracy, sensitivity, and specificity as shown in Table 3. The prediction is considered to be true positive (TP) if the patient has asthma and it is correctly predicted as asthmatic. On the contrary, if the asthmatic patient is incorrectly predicted as nonasthmatic, the prediction is assigned as false negative (FN) [30]. False positive (FP) and true negative (TN) predictions can be determined in the same way. Looking into the training model, there are 68 positive data (presence of asthma according to the physicians) and 44 negative (absence of asthma according to the physicians). The sensitivity, specificity, and accuracy have been estimated using the following equations:
| (6) |
where N TP, N TN, N FP, N FN are the number of TP, TN, FP, FN, respectively [31]. Sensitivity and specificity are statistical measures of the performance of a binary Classification test. Sensitivity measures the percentage of positive (asthmatic) people that have been correctly identified as having asthma. Specificity measures the percentage of negative (not asthmatic) people which have been correctly identified as not having asthma. The accuracy is the degree of how close the predicted values are to the actual ones.
Table 3.
Accuracy, sensitivity, and specificity percent values for 10 combinations of C and σ.
| Selection of σ parameter | Selection of C parameter | Accuracy | Sensitivity | Specificity |
|---|---|---|---|---|
| 30 | 10 | 93.75 | 97.73 | 91.18 |
| 28 | 100 | 94.64 | 97.73 | 92.65 |
| 62 | 100 | 93.75 | 97.73 | 91.18 |
| 7 | 10 | 95.54 | 95.45 | 95.59 |
| 15 | 10 | 94.64 | 97.73 | 92.65 |
| 72 | 1000 | 93.75 | 97.73 | 91.18 |
| 49 | 100 | 93.75 | 97.73 | 91.18 |
| 58 | 10 | 90.18 | 95.45 | 86.76 |
| 25 | 10 | 93.75 | 97.73 | 91.18 |
| 50 | 1000 | 94.64 | 97.73 | 92.65 |
In Table 3, the best-performed 10 combinations of C and σ values and the correct asthma prediction rates are presented. As it can be seen from these results, the value having the highest prediction accuracy for the proposed asthma prediction intelligent method was found to be 95.54%, for the case where σ = 7 and C = 10.
4. Discussion
The predictive accuracy of the proposed system is not easily comparable with that of other studies because of differences in study design and objectives. To the authors' knowledge a limited number of studies have been published on asthma prediction in children at the age when the symptoms are observed. In the study of Caudri et al. [32] the asthma prediction was based on eight clinical parameters, considering children from 7 to 8 years of age. These eight parameters were male sex, postterm delivery, parental education and inhaled medication, wheezing frequency, wheeze/dyspnea apart from colds, respiratory infections, and eczema. In 72% of the cases, the model accurately discriminated the asthmatic and the nonasthmatic children. Clough et al. [33] have developed models to examine the potential risk factors for wheeze that persists for at least 12 months after presentation in a group of young children, each with at least one atopic parent, with early-life wheezing. This paper has shown that increased age at presentation, personal atopy and raised soluble IL-2R are all associated with increased risk. Castro-Rodríguez et al. [34] developed two clinical indices at 3 years of age for the prediction of asthma in school age. It was shown that 59% of children with a positive loose index and 76% of those with a positive stringent index had active asthma in at least one survey during the school years. Their indices include characteristics of wheezing during the first 3 years of life, parental asthma or eczema, wheezing without colds, eosinophilia, or allergic rhinitis. Finally, in the study of Devulapalli et al. [35] the number of hospital admissions for obstructive airways disease within the first 2 years of life has been included in the predictive model, giving positive predictive values and negative predictive value of 55% and 92%, respectively.
Based on the comparison, which has been already shown above, it seems that there are valuable studies published on asthma prediction. However, these prediction methods are not able to achieve substantially high predictive accuracies. It is, therefore, meaningful to utilize computational intelligence methods in order to overcome such problems. Such an example has been shown in this paper. The proposed method for asthma prediction up to the age of 5 might predict the asthma with an accuracy exceeding 95%. However future studies should be performed to further evaluate our proposed method in clinical practice. Moreover, regardless of the prediction outcome using the presented algorithm, an evaluation of the results in cooperation with medical doctors who are asthma specialists must be performed in order to decide if either the patient needs treatment or not.
5. Conclusions
In this paper, a new intelligent system based on the Principal Component Analysis and Least Square Support Vector Machine classifier for asthma prediction has been proposed. The used parameter vector had a significantly high dimensionality and it was, therefore, necessary to be reduced in order to achieve as low computational cost as possible on the one hand, while on the other hand to minimize the complexity of the system. Due to the fact that asthma is a serious health condition, the various models, which have been used to detect it, must have high accuracy so that patients with asthma are not overlooked.
The experimental results show that the proposed method can predict 95.54% of patients with asthma. To conclude, the proposed system can give a significant contribution and be a useful tool in clinical practice for the physicians in order to overcome many of the therapeutic dilemmas.
Conflict of Interests
The authors report no conflict of interests.
References
- 1.Eder W, Ege MJ, von Mutius E. The asthma epidemic. The New England Journal of Medicine. 2006;355(21):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 2.Bracken MB, Belanger K, Cookson WO, Triche E, Christiani DC, Leaderer BP. Genetic and perinatal risk factors for asthma onset and severity: a review and theoretical analysis. Epidemiologic Reviews. 2002;24(2):176–189. doi: 10.1093/epirev/mxf012. [DOI] [PubMed] [Google Scholar]
- 3.Lange NE, Rifas-Shiman SL, Camargo CA, Gold DR, Gillman MW, Litonjua AA. Maternal dietary pattern during pregnancy is not associated with recurrent wheeze in children. Journal of Allergy and Clinical Immunology. 2010;126(2):250–255. doi: 10.1016/j.jaci.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Porsbjerg C, von Linstow ML, Ulrik CS, Nepper-Christensen S, Backer V. Risk factors for onset of asthma: a 12-year prospective follow-up study. Chest. 2006;129(2):309–316. doi: 10.1378/chest.129.2.309. [DOI] [PubMed] [Google Scholar]
- 5.Tolomeo C, Savrin C, Heinzer M, Bazzy-Asaad A. Predictors of asthma-related pediatric emergency department visits and hospitalizations. The Journal of Asthma. 2009;46(8):829–834. [PubMed] [Google Scholar]
- 6.Zahran HS, Person CJ, Bailey C, Moorman JE. Predictors of asthma self-management education among children and adults—2006-2007 behavioral risk factor surveillance system asthma call-back survey. The Journal of Asthma. 2012;49(1):98–106. doi: 10.3109/02770903.2011.644012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hansel NN, Matsui EC, Rusher R, et al. Predicting future asthma morbidity in preschool inner-city children. The Journal of Asthma. 2011;48(8):797–803. doi: 10.3109/02770903.2011.604887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagel G, Weinmayr G, Kleiner A, et al. Effect of diet on asthma and allergic sensitisation in the International Study on Allergies and Asthma in Childhood (ISAAC) Phase Two. Thorax. 2010;65(6):516–522. doi: 10.1136/thx.2009.128256. [DOI] [PubMed] [Google Scholar]
- 9.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The New England Journal of Medicine. 1995;332(3):133–138. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 10.Toelle BG, Xuan W, Peat JK, Marks GB. Childhood factors that predict asthma in young adulthood. European Respiratory Journal. 2004;23(1):66–70. doi: 10.1183/09031936.03.00046903. [DOI] [PubMed] [Google Scholar]
- 11.Balemans W, van der Ent C, Schilder A, Sanders E, Zielhuis G, Rovers M. Prediction of asthma in young adults using childhood characteristics: development of a prediction rule. Journal of Clinical Epidemiology. 2006;59(11):1207–1212. doi: 10.1016/j.jclinepi.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Bacopoulou F, Veltsista A, Vassi I, et al. Can we be optimistic about asthma in childhood? A Greek cohort study. The Journal of Asthma. 2009;46(2):171–174. doi: 10.1080/02770900802553128. [DOI] [PubMed] [Google Scholar]
- 13.Porpodis K, Papakosta D, Manika K, et al. Long-term prognosis of asthma is good—a 12-year follow-up study. Influence of treatment. The Journal of Asthma. 2009;46(6):625–631. doi: 10.1080/02770900903029796. [DOI] [PubMed] [Google Scholar]
- 14.Castro-Rodriguez JA. The asthma predictive index: a very useful tool for predicting asthma in young children. Journal of Allergy and Clinical Immunology. 2010;126(2):212–216. doi: 10.1016/j.jaci.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 15.Castro-Rodriguez JA, Cifuentes SL, Rodríguez-Martínez CE. The asthma predictive index remains a useful tool to predict asthma in young children with recurrent wheeze in clinical practice. Journal of Allergy and Clinical Immunology. 2011;127(4):1082–1083. doi: 10.1016/j.jaci.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 16.Panazzolo DG, Sicuro FL, Clapauch R, Maranhão PA, Bouskela E, Kraemer-Aguiar LG. Obesity, metabolic syndrome, impaired fasting glucose, and microvascular dysfunction: a principal component analysis approach. BMC Cardiovascular Disorders. 2012;12(article 102) doi: 10.1186/1471-2261-12-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Helmy A, Antoniades CA, Guilfoyle MR, Carpenter KL, Hutchinson PJ. Principal component analysis of the cytokine and chemokine response to human traumatic brain injury. PLoS One. 2012;7 doi: 10.1371/journal.pone.0039677.e39677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Milovanović I, Popović DB. Principal component analysis of gait kinematics data in acute and chronic stroke patients. Computational and Mathematical Methods in Medicine. 2012;2012:8 pages. doi: 10.1155/2012/649743.649743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Avci E. A new expert system for diagnosis of lung cancer: GDA-LS_SVM. Journal of Medical Systems. 2012;36(3):2005–2009. doi: 10.1007/s10916-011-9660-y. [DOI] [PubMed] [Google Scholar]
- 20.Çalişir D, Dogantekin E. A new intelligent hepatitis diagnosis system: PCA-LSSVM. Expert Systems with Applications. 2011;38(8):10705–10708. [Google Scholar]
- 21.Eriksson L, Johansson E, Kettaneh-Wold N, Wold S. Multi- and Megavariate Data Analysis: Principles and Applications. Umetrics AB; 2001. [Google Scholar]
- 22.Jiang H, Ching W. Correlation Kernels for support vector machines classification with applications in cancer data. Computational and Mathematical Methods in Medicine. 2012;2012:7 pages. doi: 10.1155/2012/205025.205025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lansangan JRG, Barrios EB. Principal components analysis of nonstationary time series data. Statistics and Computing. 2009;19(2):173–187. [Google Scholar]
- 24.Hotelling H. Analysis of a complex of statistical variables into principal components. Journal of Educational Psychology. 1933;24(6):417–441. [Google Scholar]
- 25.Widodo A, Yang BS. Application of nonlinear feature extraction and support vector machines for fault diagnosis of induction motors. Expert Systems with Applications. 2007;33(1):241–250. [Google Scholar]
- 26.Vapnik V. The support vector method. Proceeding of the 7th International Conference on Artificial Neural Networks (ICANN '97); 1997; pp. 263–271. [Google Scholar]
- 27.Kimeldorf G, Wahba G. Some results on Tchebycheffian spline functions. Journal of Mathematical Analysis and Applications. 1971;33(1):82–95. [Google Scholar]
- 28.Slawski M. The structured elastic net for quantile regression and support vector classification. Statistics and Computing. 2012;22(1):153–168. [Google Scholar]
- 29.Sabzekar M, Yazdi HS, Naghibzadeh M. Relaxed constraints support vector machine. Expert Systems. 2012;29(5):506–525. [Google Scholar]
- 30.Chatzimichail EA, Rigas AG, Paraskakis EN. An artificial intelligence technique for the prediction of persistent asthma in children. Proceedings of the 10th International Conference on Information Technology and Applications in Biomedicine (ITAB '10); November 2010; pp. 1–4. [Google Scholar]
- 31.Chatzimichail E, Rigas A, Paraskakis E, Chatzimichail A. Diagnosis of asthma severity using artificial neural networks. Proceedings of the 12th Mediterranean Conference on Medical and Biological Engineering and Computing (MEDICON '10); May 2010; pp. 600–603. [Google Scholar]
- 32.Caudri D, Wijga A, Chipper CM, et al. Predicting the long-term prognosis of children with symptoms suggestive of asthma at preschool age. The Journal of Allergy and Clinical Immunology. 2009;124(5):903–910. doi: 10.1016/j.jaci.2009.06.045. [DOI] [PubMed] [Google Scholar]
- 33.Clough JB, Keeping KA, Edwards LC, Freeman WM, Warner JA, Warner JO. Can we predict which wheezy infants will continue to wheeze? American Journal of Respiratory and Critical Care Medicine. 1999;160(5):1473–1480. doi: 10.1164/ajrccm.160.5.9807019. [DOI] [PubMed] [Google Scholar]
- 34.Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. American Journal of Respiratory and Critical Care Medicine. 2000;162(4):1403–1406. doi: 10.1164/ajrccm.162.4.9912111. [DOI] [PubMed] [Google Scholar]
- 35.Devulapalli CS, Carlsen KCL, Håland G, et al. Severity of obstructive airways disease by age 2 years predicts asthma at 10 years of age. Thorax. 2008;63(1):8–13. doi: 10.1136/thx.2006.060616. [DOI] [PubMed] [Google Scholar]


