Abstract
AIM: To investigate the clinical efficiency of percutaneous trans-hepatic bilateral biliary metallic stenting for the management of Bismuth IV malignant obstructive disease.
METHODS: Our hospital’s database was searched for all patients suffering from the inoperable malignant biliary obstruction Bismuth IV, and treated with percutaneous bilateral trans-hepatic placement of self-expandable nitinol stents. The indication for percutaneous stenting was an inoperable, malignant, symptomatic, biliary obstruction. An un-correctable coagulation disorder was the only absolute contra-indication for treatment. Bismuth grading was performed using magnetic resonance cholangiopancreatography. Computed tomography evaluation of the lesion and the dilatation status of the biliary tree was always performed prior to the procedure. All procedures were performed under conscious sedation. A single trans-hepatic track technique was preferred (T-configuration stenting) and a second, contra-lateral trans-hepatic track (Y-configuration stenting) was used only in cases of inability to access the contra-lateral lobe using a single track technique. The study’s primary endpoints were clinical success, defined as a decrease in bilirubin levels within 10 d and patient survival rates. Secondary endpoints included peri-procedural complications, primary and secondary patency rates.
RESULTS: A total of 35 patients (18 female, 51.4%) with a mean age 69 ± 13 years (range 33-88) were included in the study. The procedures were performed between March 2000 and June 2008 and mean time follow-up was 13.5 ± 22.0 mo (range 0-96). The underlying malignant disease was cholangiocarcinoma (n = 10), hepatocellular carcinoma (n = 9), pancreatic carcinoma (n = 5), gastric cancer (n = 2), bile duct tumor (n = 2), colorectal cancer (n = 2), gallbladder carcinoma (n = 2), lung cancer (n = 1), breast cancer (n = 1) or non-Hodgkin lymphoma (n = 1). In all cases, various self-expandable bare metal stents with diameters ranging from 7 to 10 mm were used. Stents were placed in Y-configuration in 24/35 cases (68.6%) using two stents in 12/24 patients and three stents in 12/24 cases (50%). A T-configuration stent placement was performed in 11/35 patients (31.4%), using two stents in 4/11 cases (36.4%) and three stents in 7/11 cases (63.6%). Follow-up was available in all patients (35/35). Patient survival ranged from 0 to 1763 d and the mean survival time was 168 d. Clinical success rate was 77.1% (27/35 cases), and peri-procedural mortality rate was 5.7% (2/35 patients). Biliary re-obstruction due to stent occlusion occurred in 25.7% of the cases (9/35 patients), while in 7/11 (63.6%) one additional percutaneous re-intervention due to stent occlusion resulting in clinical relapse of symptomatology was successfully performed. In the remaining 4/11 patients (36.4%) more than 1 additional reintervention was performed. The median decrease of total serum bilirubin was 60.5% and occurred in 81.8% of the cases (27/33 patients). The median primary and secondary patency was 105 (range 0-719) and 181 d (range 5-1763), respectively. According to the Kaplan-Meyer survival analysis, the estimated survival rate was 73.5%, 47.1% and 26.1% at 1, 6 and 12 mo respectively, while the 8-year survival rate was 4.9%. Major and minor complication rates were 5.7% (2/35 patients) and 17.1% (6/35 patients), respectively.
CONCLUSION: Percutaneous bilateral biliary stenting is a safe and clinically effective palliative approach in patients suffering from Bismuth IV malignant obstruction.
Keywords: Bismuth IV, Malignant biliary obstruction, Percutaneous bilateral stenting, Nitinol stents, Palliative treatment, Fluoroscopically-guided
INTRODUCTION
Malignant biliary tree obstruction occurs due to primary biliary or metastatic carcinomas. The most common causes of this condition are cholangiocarcinoma, gallbladder cancer and pancreatic carcinoma[1]. Although surgery is indicated in many cases for the management of malignant biliary obstruction, nearly 80% of the patients are inoperable by the time of diagnosis and the median survival ranges between 3 and 10 mo[2-4]. Minimally invasive decompression drainage modalities are established palliative methods for the management of inoperable hilar lesions and include percutaneous trans-hepatic biliary drainage, endoscopic stricture stenting and percutaneous trans-hepatic biliary stenting (PTBS)[4-7]. Malignant obstructions of the hepatic hilum are characterized by extremely poor prognosis resulting in a 5-year survival rate around 5%, and are also the most technically challenging biliary lesions for both endoscopic and interventional radiology management approaches[2]. Palliative decompression of the biliary tree using metallic stents focuses on achieving relief from obstruction-related pathology, in order to improve the patient’s quality of life and survival. In Bismuth-Corlette III and IV lesions the percutaneous trans-hepatic approach is the modality of choice[8,9].
To date, data regarding percutaneous trans-hepatic bilateral stenting in Bismuth IV lesions are scarce and the clinical decision whether to drain both hepatic lobes remains controversial[10-12]. The present study investigated the safety and clinical efficiency of palliative, percutaneous trans-hepatic bilateral metallic stenting, for the management of Bismuth IV malignant hilar obstructive disease.
MATERIALS AND METHODS
Board approval was obtained by the hospital’s Scientific and Ethics Committee. Our hospital’s databases were retrospectively searched for all patients suffering from Bismuth disease who were managed using percutaneous bilateral trans-hepatic placement of self-expandable nitinol stents in the Interventional Radiology Unit. The indication for percutaneous stenting was an inoperable, malignant, symptomatic, biliary obstruction. An un-correctable coagulation disorder was the only absolute contra-indication for treatment. The international normalized ratio (INR) value required was < 1.5 and platelet count > 50 × 109/L. Bismuth grading was performed using magnetic resonance cholangiopancreatography. Computed tomography evaluation of the lesion and the dilatation status of the biliary tree were always performed prior to the procedure.
The patients were hospitalized at least 24 h before the drainage and were kept nil per mouth for at least 6 h prior to the procedure. Baseline pre-procedural laboratory tests included blood count, serum bilirubin, renal function and coagulation profile (INR, prothrombin time, partial thromboplastin time). Any clotting disorder was corrected appropriately. Prophylactic treatment with broad spectrum antibiotics (second-generation cephalosporin) was administrated 24 h prior to the procedure and continued for five days thereafter. Written informed consent was attained from all patients. All procedures were performed under conscious sedation using a combination of opioid analgesic (Fentanyl) and a sedative (Midazolam). Initial doses of 25-50 μg of Fentanyl and 1-2 mg of Midazolam were administrated and these were repeated when needed. The access site (right or left lobe puncture) was chosen according to the pre-procedural imaging. A fine 21 G × 15 cm Chiba needle was utilized and ultrasound-guidance was mainly used in left-lobe access. Following the initial diagnostic percutaneous trans-hepatic cholangiography a single trans-hepatic track technique was preferred (T-configuration stenting) and a second, contra-lateral trans-hepatic track (Y-configuration stenting) was used only in cases of inability to access the contra-lateral lobe using a single track technique. Access through the obstructed bile ducts to the small intestine was obtained using standard Interventional Radiology techniques and materials. In cases where bile tree infection was suspected, an external drainage catheter was positioned and stent placement was performed a few days later, following iv antibiotic therapy and bile tree decompression. Where no infection was suspected, moderate balloon pre-dilatation and self-expandable bare metal stenting was performed. The Kissing balloon technique was used for pre-dilatation prior to Y-configuration stenting. At the end of the procedure, a closed external-internal drainage catheter was left in place and was removed over-the-wire if good stent patency, without any signs of bleeding, was confirmed two days after. Post-procedural laboratory tests were repeated every day until the patient’s discharge and monthly thereafter. In cases of significant bilirubin level increase and/or cholangitis, re-evaluation with ultrasound and revision was performed if needed.
The study’s primary endpoint was clinical success defined as relief or improvement from the initial symptoms and survival rates. Secondary endpoints included peri-procedural 24 h major and minor complication rates, primary patency rates defined as the patency of the deployed stents without any additional intervention and secondary patency rates defined as the stent patency following one additional percutaneous or endoscopic re-intervention due to clinical relapse of the symptoms. Stents were considered patent in cases in which no increase in serum bilirubin levels or dilatation of the intrahepatic ducts was noted. Complications were divided into major and minor according to the standards of the Society of Interventional Radiology[13]. Statistical analysis was performed using dedicated statistical analysis software (GraphPad Prism version 5; San Diego, CA, United States).
RESULTS
In total, 35 patients (18 female, 51.4%) with a mean age 69 ± 13 years (range 33 to 88 years) were included in the study. All patients suffered from Bismuth IV type malignant disease and were considered unsuitable for operation due to tumour extension and/or poor physical conditions. The procedures were performed between March 2000 and June 2008 and mean time clinical follow-up was 13.5 ± 22.0 mo (range 0 to 96 mo). The underlying malignant disease was cholangio-carcinoma (n = 10), hepatocellular carcinoma (n = 9), pancreatic carcinoma (n = 5), gastric cancer (n = 2), bile duct tumour (n = 2), colorectal cancer (n = 2), gallbladder carcinoma (n = 2), lung cancer (n = 1), breast cancer (n = 1) or non-Hodgkin lymphoma (n = 1). Patient baseline demographics are analytically reported in Table 1. All procedures were performed by two senior interventional radiologists. In all cases various self-expandable bare metal stents with diameters ranging from 7 to 10 mm were used. Stents were placed in Y-configuration in 24/35 cases (68.6%) using two stents in 12/24 patients and three stents in 12/24 cases (50%). A T-configuration stent placement was performed in 11/35 patients (31.4%), using two stents in 4/11 cases (36.4%) and three stents in 7/11 cases (63.6%). Follow-up was available in all patients (35/35). Patient survival ranged from 0 to 1763 d and the mean survival time was 168 d. According to the Kaplan-Meyer survival analysis, the estimated survival rate was 73.5%, 47.1% and 26.1% at 1, 6 and 12 mo respectively, while the 8 year survival rate was 4.9% (Figure 1). The clinical success rate was 77.1% (27/35 cases), as 2/35 patients (5.7%) died within the first 24 h and in 6/33 patients (18.2%) a total serum bilirubin increase by 107% (range, 101%-112%), compared to baseline, was recorded. In 27/33 patients (81.8%) a decrease in total serum bilirubin level by 60.5% (range, 23%-92%) was noted, resulting in relief or improvement of symptoms.
Table 1.
Patients’ baseline demographics
| Patients (n) | 35 |
| Female | 18/35 (51.4) |
| Age (yr), mean ± SD | 69 ± 13 |
| Tumor type | |
| Cholangiocarcinoma | 10/35 (28.5) |
| Hepatocellular carcinoma | 9/35 (25.7) |
| Pancreatic carcinoma | 5/35 (14.3) |
| Gastric cancer | 2/35 (5.7) |
| Bile duct cancer | 2/35 (5.7) |
| Colorectal cancer | 2/35 (5.7) |
| Gallbladder carcinoma | 2/35 (5.7) |
| Lung cancer | 1/35 (2.8) |
| Breast cancer | 1/35 (2.8) |
| Non-Hodgkin lymphoma | 1/35 (2.8) |
Figure 1.
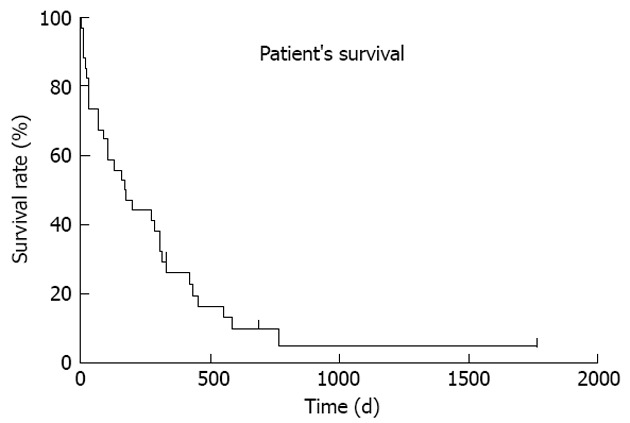
Overall patients’ survival Kaplan-Meyer plot.
The median primary and secondary patency were 105 d (range: 0 to 719 d) and 181 d (range: 100 to 1763 d), respectively. During the follow-up period biliary re-obstruction due to stent occlusion occurred in 25.7% of cases (9/35 patients). In 7/11 (63.6%) one additional percutaneous re-intervention because of stent occlusion resulting in clinical relapse of symptomatology was successfully performed. In the remaining 4/11 patients (36.4%) more than 1 additional reintervention was performed. In three cases, 2 additional successful re-interventions were performed, while only one patient underwent 3 additional re-interventions at 121, 305 and 526 d after the first stent insertion. The post-procedural, mean hospitalization period was of 10.2 ± 3.9 d. The peri-procedural mortality rate was 5.7% (2/35 patients) as one patient died during the procedure due to heart failure and a second patient died a day after the procedure due to aspiration. The major complications rate was 5.7% (2/35 cases) as one patient developed septicaemia, was further hospitalized and successfully treated, while one patient developed a right hepatic artery pseudoaneurysm causing haemobilia. The latter was successfully treated with percutaneous endovascular coil embolization. Minor complications (cholangitis) were observed in 6/35 patients (17.1%) and were successfully managed using conservative antibiotic therapy. Procedural outcomes are analytically reported in Table 2.
Table 2.
Procedural details and outcomes
| Stents used (n) | 48 |
| Stent deployment | |
| Y-configuration | 18/35 (51.4%) |
| T-configuration | 17/35 (48.6%) |
| Technical success | 35/35 (100%) |
| Clinical success | 27/35 (77.1%) |
| Decreased bilirubin levels | 27/33 (81.8%) |
| Serum bilirubin decrease | 60.5% (23%-92%) |
| Survival interval (d), mean (range) | 168 (0-1763) |
| 6-mo survival rate | 47.10% |
| Primary patency (d), mean (range) | 105 ( 0-719) |
| Secondary patency (d), mean (range) | 181 (100-1763) |
| Peri-procedural death | 2/35 (5.7%) |
| Major complications | 2/35 (5.7%) |
| Minor complications | 6/35 (17.1%) |
| Hospitalization time (d), mean ± SD | 10.2 ± 3.9 |
DISCUSSION
The Bismuth-Corlette classification describes the extension of malignant disease into the intrahepatic bile ducts.In type IV disease the tumour extends from the confluence into both the right and left segmental hepatic ducts. Symptoms include severe jaundice, pruritus, cholangitis and right flank pain, rapidly leading to hepatic failure and death. Percutaneous biliary metallic stenting is the recommended palliative decompression method in patients suffering from Bismuth IV malignant obstructive jaundice, as it is characterized by lower technical failure and complication rates than the endoscopic approach[8,14]. Biliary drainage aims at the alleviation of symptoms and the amelioration of the patients’ quality of life. In lesions involving both hepatic ducts a decision must made whether draining both hepatic lobes would improve palliation outcomes. In most cases the right hepatic duct drains 2/3 of the hepatic parenchyma and therefore unilateral right drainage should be sufficient to produce the desired palliative effect[15]. However, an un-drained left side could incite cholangitis and bilateral stenting offers the opportunity to choose the most appropriate lobe for drainage in cases where any repeat procedures may be necessary[16]. In very advanced disease the clinical effectiveness of single-lobe drainage remains controversial as some authors have reported superior patency rates and clinical outcomes in patients with Bismuth type IV obstruction when both biliary ducts were stented[12]. Furthermore, in cases of extensive right lobe tumour, unilateral right bile drainage could result in insufficient serum bilirubin level decrease, a clinical endpoint that has been identified as a main independent predictor of survival[17]. On the other hand, single left lobe drainage is rarely sufficient to eliminate or ease obstructive symptoms. For these reasons even multi-segmental biliary stenting should be performed in cases in which the tumoral obstruction extends beyond the segmental ducts and neither Y- nor T-configuration techniques can ensure the adequate decompression of the affected biliary tree (Figure 2). Few authors have investigated various techniques to achieve a bi-lobar hepatic drain in an attempt to increase clinical effectiveness[1,18-20]. To date, there are insufficient data to support either of the two percutaneous approaches in Bismuth IV lesions. This retrospective study was designed to investigate the clinical efficiency, as judged by survival and relief from jaundice symptoms, following percutaneous bi-lobar stenting for the management of Bismuth IV malignant disease. Bismuth IV disease has been identified as an independent predictor of almost 5-fold increased mortality following PTBS[17]. In this series the mean survival time of 169 d is comparable and even superior to previously reported results involving patients with less advanced, Bismuth I -IV, disease[2,3]. In addition, a very satisfactory 6- and 12 mo survival rate of 47.1% and 26.1% respectively was observed, while surprisingly 1 patient (4.9%) suffering from non-Hodgkin lymphoma was alive after 8 years of follow-up.
Figure 2.
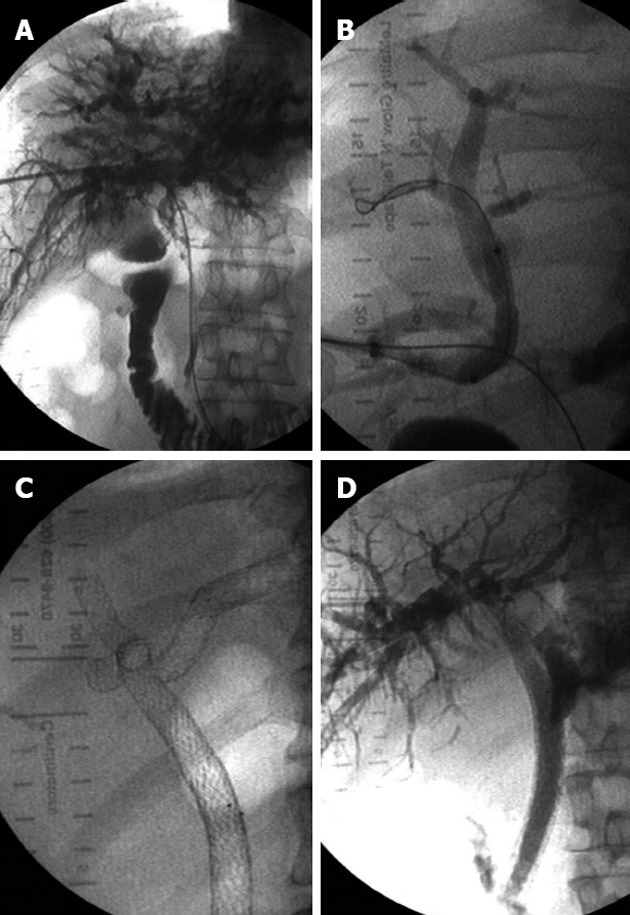
Bismuth IV lesions. A: Percutaneous trans-hepatic cholangiography image demonstrating a Bismuth IV biliary obstruction; B: Right-sided approach; C: Multiple (n = 4) bilateral stenting in segmental ducts communicating with the stented common bile duct; D: Final fluoroscopic image demonstrating the flow of contrast medium into the duodenum.
Furthermore, post-procedural clinical response was very encouraging. Serum total bilirubin level decrease was attained in almost 82% of the cases with a mean decrease of 61.3% ± 19.1%. The mean primary patency rate was 174.1 d, while biliary re-obstruction reoccurred in the 25.7% of our patients. This is in accordance with the 11%-29% reoccurrence reported by Inal et al[12], in a study investigating 32 patients suffering from Bismuth IV biliary obstructions. The fact that this satisfactory clinical success rate was coupled with very low re-obstruction rates, stresses the clinical significance of bilateral decompression.
Some issues regarding bilateral stenting still need to be addressed. For example, a higher risk of complications following the bilateral approach has been reported, and some authors advocate that this risk should not be taken as even 30% of functional liver parenchyma could be sufficient[1-6,20-25]. Nonetheless, although no control group was available, the authors support the notion that in the specific population of end-stage, advanced, hilar disease, bilateral decompression was vital for the clinical success and survival rates achieved. Recently published data coming from a single-center study comparing endoscopic bilateral versus unilateral stent deployment demonstrated the superior cumulative stent patency of the bilateral approach, further supporting this suggestion[26]. Moreover, in our study, the long-term clinical effectiveness was maintained by the successful revisions resulting in high secondary patency rates following stent occlusion. In detail, stent re-occlusion due to tumour overgrowth was detected in 27.3% (9/33 cases) that were subsequently managed successfully, using percutaneous balloon dilatation and additional stenting.
Only bare metal stents are used in our department as their superiority over plastic endoprosthesis has been widely reported[18]. Covered stents could also be used in hilar lesions in a Y-configuration. Recent data regarding covered metal stents have demonstrated significantly lower re-intervention rates. However, they are associated with complications such as cholecystitis, pancreatitis and stent migration[22,23,27].
The majority of the procedures were performed with a single right-sided access, following the pre-procedural imaging assessment. Major complication rates following biliary stenting ranges between 7% and 35%. In our study the safety of the bilateral approach was demonstrated by the low procedure-related major complication rate of 5.7%, considerably below the 10% threshold recommended for PTBS[7,23,28]. Peri-procedural mortality was 5.7%, while one patient died on the operating table from heart failure. This fact highlights the procedural risks, given that the majority of these drainages are performed in end-stage patients with poor general conditions.
The study’s limitations include the lack of a predefined clinical and imaging follow-up, because of the retrospective design, as well as the inability to obtain detailed data regarding the patients’ post-procedural quality of life using dedicated questionnaires. However, as quality of life in patients suffering from advanced cancer is mainly influenced by the frequency and length of hospitalization, as well as and the need for repeated procedures, it is the authors’ belief that this technique contributed to the patient’s quality of life overall. Finally, further limitations of this study were the possible bias generated by use of various metallic stents and the lack of a control group undergoing unilateral stenting procedures, which would allow direct comparison between the two methods.
In conclusion, in the present study, bilateral PTBS using self-expandable metallic stents was proven a safe and clinically effective, minimally invasive palliative method for the management of malignant, Bismuth IV, biliary obstruction.
COMMENTS
Background
Biliary drainage aims for the alleviation of symptoms and the amelioration of the patients’ quality of life. In lesions involving both hepatic ducts a decision must be made whether draining both hepatic lobes would improve palliation outcomes.
Research frontiers
To date, data regarding percutaneous trans-hepatic bilateral stenting in Bismuth IV lesions are scarce and the clinical decision whether to drain both hepatic lobes remains controversial. The present study investigated the safety and clinical efficiency of palliative, percutaneous trans-hepatic bilateral metallic stenting, for the management of Bismuth IV malignant hilar obstructive disease. Both T- configuration and Y-configuration stenting were performed.
Innovations and breakthroughs
Bismuth IV disease has been identified as an independent predictor of almost 5-fold increased mortality following percutaneous trans-hepatic biliary stenting. In this series, the mean survival time of 169 d is comparable and even superior to previously reported results involving patients with less advanced, Bismuth I - IV, disease. In addition, a very satisfactory 6 and 12 mo survival rate of 47.1% and 26.1% respectively was noted.
Applications
Biliary drainage aims for the alleviation of symptoms and the amelioration of the patients’ quality of life. The authors support the notion that in lesions involving both hepatic ducts the decision to drain both hepatic lobes using nitinol bare stents would improve palliation outcomes.
Terminology
Bismuth IV obstructive disease: Malignant disease expanding in both left and right hepatic bile ducts; T-configuration biliary stenting: Bilateral biliary drainage achieved after single hepatic lobe access, using two stents one within the other; Y-configuration biliary stenting: Bilateral biliary drainage achieved after both right and left hepatic lobe access, using two stents side by side.
Peer review
The authors herein report the safety and long-term feasibility of bilateral self-expandable biliary stenting in advanced Bismuth IV biliary neoplastic disease. The article is very interesting and informative, and has sufficient value to be published.
Footnotes
P- Reviewers Rajeshwari K, Liu Q S- Editor Song XX L- Editor Hughes D E- Editor Li JY
References
- 1.Bae JI, Park AW, Choi SJ, Kim HP, Lee SJ, Park YM, Yoon JH. Crisscross-configured dual stent placement for trisectoral drainage in patients with advanced biliary hilar malignancies. J Vasc Interv Radiol. 2008;19:1614–1619. doi: 10.1016/j.jvir.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Kim CW, Park AW, Won JW, Kim S, Lee JW, Lee SH. T-configured dual stent placement in malignant biliary hilar duct obstructions with a newly designed stent. J Vasc Interv Radiol. 2004;15:713–717. doi: 10.1097/01.rvi.0000133508.79090.a2. [DOI] [PubMed] [Google Scholar]
- 3.Schoder M, Rossi P, Uflacker R, Bezzi M, Stadler A, Funovics MA, Cejna M, Lammer J. Malignant biliary obstruction: treatment with ePTFE-FEP- covered endoprostheses initial technical and clinical experiences in a multicenter trial. Radiology. 2002;225:35–42. doi: 10.1148/radiol.2251011744. [DOI] [PubMed] [Google Scholar]
- 4.Dambrauskas Z, Paskauskas S, Lizdenis P, Uktveris R, Pranculis A, Kaupas RS, Barauskas G, Pundzius J. Percutaneous transhepatic biliary stenting: the first experience and results of the Hospital of Kaunas University of Medicine. Medicina (Kaunas) 2008;44:969–976. [PubMed] [Google Scholar]
- 5.Kaufman SL, Kadir S, Mitchell SE, Kinnison ML, Chang R. Left lobe of the liver: percutaneous biliary drainage. Radiology. 1989;170:191–194. doi: 10.1148/radiology.170.1.2909096. [DOI] [PubMed] [Google Scholar]
- 6.Lee SH, Park JK, Yoon WJ, Lee JK, Ryu JK, Yoon YB, Kim YT. Optimal biliary drainage for inoperable Klatskin’s tumor based on Bismuth type. World J Gastroenterol. 2007;13:3948–3955. doi: 10.3748/wjg.v13.i29.3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.LaBerge JM, Doherty M, Gordon RL, Ring EJ. Hilar malignancy: treatment with an expandable metallic transhepatic biliary stent. Radiology. 1990;177:793–797. doi: 10.1148/radiology.177.3.2173842. [DOI] [PubMed] [Google Scholar]
- 8.Paik WH, Park YS, Hwang JH, Lee SH, Yoon CJ, Kang SG, Lee JK, Ryu JK, Kim YT, Yoon YB. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. 2009;69:55–62. doi: 10.1016/j.gie.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Mukai T, Yasuda I, Nakashima M, Doi S, Iwashita T, Iwata K, Kato T, Tomita E, Moriwaki H. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2013;20:214–222. doi: 10.1007/s00534-012-0508-8. [DOI] [PubMed] [Google Scholar]
- 10.Maetani I, Inoue H, Ogawa S, Sato M, Igarashi Y, Sakai Y. Percutaneous T-tube placement for bilateral internal drainage in malignant hilar obstruction. Hepatogastroenterology. 2000;47:1509–1513. [PubMed] [Google Scholar]
- 11.Adam A. Metallic biliary endoprostheses. Cardiovasc Intervent Radiol. 1994;17:127–132. doi: 10.1007/BF00195504. [DOI] [PubMed] [Google Scholar]
- 12.Inal M, Akgül E, Aksungur E, Seydaoğlu G. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: unilobar versus bilobar drainage. J Vasc Interv Radiol. 2003;14:1409–1416. doi: 10.1097/01.rvi.0000096762.74047.a6. [DOI] [PubMed] [Google Scholar]
- 13.Dahlstrand U, Sandblom G, Eriksson LG, Nyman R, Rasmussen IC. Primary patency of percutaneously inserted self-expanding metallic stents in patients with malignant biliary obstruction. HPB (Oxford) 2009;11:358–363. doi: 10.1111/j.1477-2574.2009.00069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saluja SS, Gulati M, Garg PK, Pal H, Pal S, Sahni P, Chattopadhyay TK. Endoscopic or percutaneous biliary drainage for gallbladder cancer: a randomized trial and quality of life assessment. Clin Gastroenterol Hepatol. 2008;6:944–950.e3. doi: 10.1016/j.cgh.2008.03.028. [DOI] [PubMed] [Google Scholar]
- 15.van Delden OM, Laméris JS. Percutaneous drainage and stenting for palliation of malignant bile duct obstruction. Eur Radiol. 2008;18:448–456. doi: 10.1007/s00330-007-0796-6. [DOI] [PubMed] [Google Scholar]
- 16.Adam A, Dondeliger RF, Mueller PR. Interventional Radiology in Cancer. Berlin, Heidelberg: Springer-Verlag; 2004. pp. 1–20. [Google Scholar]
- 17.Brountzos EN, Ptochis N, Panagiotou I, Malagari K, Tzavara C, Kelekis D. A survival analysis of patients with malignant biliary strictures treated by percutaneous metallic stenting. Cardiovasc Intervent Radiol. 2007;30:66–73. doi: 10.1007/s00270-005-0379-3. [DOI] [PubMed] [Google Scholar]
- 18.Piñol V, Castells A, Bordas JM, Real MI, Llach J, Montañà X, Feu F, Navarro S. Percutaneous self-expanding metal stents versus endoscopic polyethylene endoprostheses for treating malignant biliary obstruction: randomized clinical trial. Radiology. 2002;225:27–34. doi: 10.1148/radiol.2243011517. [DOI] [PubMed] [Google Scholar]
- 19.Covey AM, Brown KT. Percutaneous transhepatic biliary drainage. Tech Vasc Interv Radiol. 2008;11:14–20. doi: 10.1053/j.tvir.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Morgan RA, Adam AN. Malignant biliary disease: percutaneous interventions. Tech Vasc Interv Radiol. 2001;4:147–152. doi: 10.1016/s1089-2516(01)90021-6. [DOI] [PubMed] [Google Scholar]
- 21.Maybody M, Brown KT, Brody LA, Covey AM, Sofocleous CT, Thornton RH, Getrajdman GI. Primary patency of Wallstents in malignant bile duct obstruction: single vs. two or more noncoaxial stents. Cardiovasc Intervent Radiol. 2009;32:707–713. doi: 10.1007/s00270-009-9577-8. [DOI] [PubMed] [Google Scholar]
- 22.Isayama H, Nakai Y, Togawa O, Kogure H, Ito Y, Sasaki T, Sasahira N, Hirano K, Tsujino T, Tada M, et al. Covered metallic stents in the management of malignant and benign pancreatobiliary strictures. J Hepatobiliary Pancreat Surg. 2009;16:624–627. doi: 10.1007/s00534-009-0133-3. [DOI] [PubMed] [Google Scholar]
- 23.Lee DK. Drug-eluting stent in malignant biliary obstruction. J Hepatobiliary Pancreat Surg. 2009;16:628–632. doi: 10.1007/s00534-009-0135-1. [DOI] [PubMed] [Google Scholar]
- 24.Lammer J, Klein GE, Kleinert R, Hausegger K, Einspieler R. Obstructive jaundice: use of expandable metal endoprosthesis for biliary drainage. Work in progress. Radiology. 1990;177:789–792. doi: 10.1148/radiology.177.3.2243991. [DOI] [PubMed] [Google Scholar]
- 25.Brown KT, Covey AM. Management of malignant biliary obstruction. Tech Vasc Interv Radiol. 2008;11:43–50. doi: 10.1053/j.tvir.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 26.Naitoh I, Ohara H, Nakazawa T, Ando T, Hayashi K, Okumura F, Okayama Y, Sano H, Kitajima Y, Hirai M, et al. Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol. 2009;24:552–557. doi: 10.1111/j.1440-1746.2008.05750.x. [DOI] [PubMed] [Google Scholar]
- 27.Krokidis M, Fanelli F, Orgera G, Tsetis D, Mouzas I, Bezzi M, Kouroumalis E, Pasariello R, Hatzidakis A. Percutaneous palliation of pancreatic head cancer: randomized comparison of ePTFE/FEP-covered versus uncovered nitinol biliary stents. Cardiovasc Intervent Radiol. 2011;34:352–361. doi: 10.1007/s00270-010-9880-4. [DOI] [PubMed] [Google Scholar]
- 28.Lee KH, Lee DY, Kim KW. Biliary intervention for cholangiocarcinoma. Abdom Imaging. 2004;29:581–589. doi: 10.1007/s00261-004-0192-5. [DOI] [PubMed] [Google Scholar]


