Abstract
Objective
To investigate Candida species and Staphylococcus aureus and the development of ‘nipple and breast thrush’ among breastfeeding women.
Design
Prospective longitudinal cohort study.
Setting
Two hospitals in Melbourne, Australia (one public, one private) with follow-up in the community.
Participants
360 nulliparous women recruited at ≥36 weeks’ gestation from November 2009 to June 2011. Participants were followed up six times: in hospital, at home weekly until 4 weeks postpartum and by telephone at 8 weeks.
Main outcome measures
Case definition ‘nipple and breast thrush’: burning nipple pain and breast pain (not related to mastitis); detection of Candida spp (using culture and PCR) in the mother's vagina, nipple or breast milk or in the baby's mouth; detection of S aureus in the mother's nipple or breast milk.
Results
Women with the case definition of nipple/breast thrush were more likely to have Candida spp in nipple/breast milk/baby oral samples (54%) compared to other women (36%, p=0.014). S aureus was common in nipple/breast milk/baby samples of women with these symptoms as well as women without these symptoms (82% vs 79%) (p=0.597). Time-to-event analysis examined predictors of nipple/breast thrush up to and including the time of data collection. Candida in nipple/breast milk/baby predicted incidence of the case definition (rate ratio (RR) 1.87 (95% CI 1.10 to 3.16, p=0.018). We do not have evidence that S aureus colonisation was a predictor of these symptoms (RR 1.53, 95% CI 0.88 to 2.64, p=0.13). Nipple damage was also a predictor of these symptoms, RR 2.30 (95% CI 1.19 to 4.43, p=0.012). In the multivariate model, with all three predictors, the RRs were very similar to the univariate RRs. This indicates that Candida and nipple damage are independent predictors of our case definition.
Keywords: Primary Care
Article summary.
Article focus
Controversy about the condition known as ‘breast thrush’ or breast candidiasis in lactating women has led to confusion among clinicians and the community.
Previous studies have been cross-sectional.
This is the first prospective longitudinal study to examine simultaneously both Staphylococcus aureus and Candida spp in breast infections and was designed to resolve the current controversy surrounding the primary organism responsible for the condition known as ‘breast thrush’: Candida spp or S aureus?
Key messages
Candida spp is associated with burning nipple pain and breast pain.
Colonisation with S aureus is common; at least 50% of women were colonised with S aureus in nipple or milk samples by 4 weeks postpartum.
Strengths and limitation of this study
The evidence of microbiological data from this large cohort of women over 4 weeks postpartum is stronger than previous smaller cross-sectional studies.
Candida spp were more commonly identified using more sensitive molecular techniques (real-time PCR) than by using standard microbiological culture techniques.
As these techniques are not used in clinical practice currently, clinicians should continue to use their clinical skills to diagnose causes of nipple and breast pain in lactating women.
Background
Controversy about the condition known as ‘breast thrush’ or breast candidiasis in lactating women has led to confusion among clinicians and the community. While some clinicians may diagnose and treat this condition in breastfeeding women with deep, radiating breast pain associated with burning nipple pain,1–6 others doubt the relationship with fungal organisms7–11 and decry ‘the alarming trend towards believing that fungi are important in the aetiology of breast infection and deep breast pain associated with breast feeding, despite a lack of good quality evidence’ (ref. 11, p.485).
Unlike mastitis, which is diagnosed when a breastfeeding woman experiences inflammation of the breast associated with systemic symptoms,12 breast thrush is usually diagnosed when the breast is not erythematous or indurated, and the woman is afebrile and systemically well except for the typical burning pain radiating into the breast and/or the back.4 While some authors use the term ‘candida mastitis’,6 11 13 we feel this is misleading, as inflammation of the breast is not evident. Although some clinicians attribute the pain to infection with S aureus and treat women with long-term antibiotics,14 this has not been tested in trials.
The primary cause of nipple pain or damage is often the process of breastfeeding itself: trauma due to the incorrect attachment of the infant's mouth, anatomy of the mouth or dysfunctional suck.15 Nipple thrush is usually diagnosed when the nipple/areola is slightly pink, sensitive to touch and the pain described is out of proportion to the damage seen on clinical examination.4 When the areola is described as itchy and appears red and/or crusty, the diagnosis is dermatitis/eczema rather than fungal infection.16 A nipple with obvious damage is almost certainly colonised with S aureus.17 Nipple/breast pain associated with nipple blanching persisting for longer than a few seconds is likely to be nipple vasospasm; this condition is commonly confused with breast thrush because of the burning, radiating nature of the pain.18 19 The pain due to vasospasm is often secondary to nipple damage or infection, exacerbated by cold and relieved by heat or nifedipine.20 In practice, more than one cause of nipple or breast pain is commonly present,6 which makes it difficult to construct a case definition for ‘breast thrush’ for research purposes.
Previous breastfeeding studies have been largely cross-sectional,1 7 9 10 with one longitudinal study collecting microbiological data but no clinical information.21 This is the first prospective longitudinal study to examine both S aureus and Candida spp in breast infections and was designed to resolve the current controversy surrounding the primary organism responsible for the condition known as ‘breast thrush’: Candida spp or S aureus?
Methods
The CASTLE (Candida and Staphylococcus Transmission: Longitudinal Evaluation) study was a prospective longitudinal descriptive study; details have been published in the study protocol.22 A cohort of 360 nulliparous women planning to breastfeed for at least 2 months were recruited at ≥36 weeks’ gestation from two hospitals in Melbourne, Australia (November 2009–June 2011). At recruitment, nasal, nipple (both breasts) and vaginal swabs were collected and participants completed a questionnaire asking about previous Staphylococcus and Candida infections. Participants were followed up six times: face-to-face in hospital, then weekly at home until 4 weeks postpartum. The participants filled out a questionnaire at each time point to collect information about breastfeeding problems and postpartum health problems. At each visit, maternal nasal, and nipple swabs and breast milk samples (both breasts) and infant oral and nasal swabs were collected. In a final telephone interview 8 weeks postpartum, information about breastfeeding problems and postpartum health was collected.
Specimens were collected by research assistants. Fresh gloves were worn for each specimen. After sanitising their hands, research assistants collected nipple swabs, then washed the nipple/areola region twice using sterile water wipes. Midstream milk was collected in a sterile container; the first drops of breast milk were expressed and discarded. Two nipple swabs were obtained from each nipple: a standard charcoal swab for microbiological analysis (Copan Diagnostics Inc, California, USA) and a flocked swab for molecular analysis (Copan Diagnostics Inc). After first moistening in sterile saline, both the standard and flocked nipple swabs were rolled over the nipple and areola together using a 10-point swabbing technique,23 paying particular attention to any cracks/fissures present. Oral and vaginal swabs were collected for culture of S aureus and Candida spp. Breast milk samples were also cultured for S aureus, coagulase-negative staphylococci (CoNS) and Candida spp; nasal swabs were collected for culture of S aureus only.
In the studies conducted on women with vulvovaginal symptoms, molecular microbiological techniques have been useful in detecting Candida in women who were found to be negative with standard microbiology techniques.24 25 Therefore, we planned to use molecular techniques to increase detection of Candida spp in nipple specimens.22 Owing to cost constraints, we did not plan to use molecular techniques for the milk specimens (up to 4000 specimens). As participants only had one or two vaginal specimens, we extracted DNA from vaginal as well as nipple swabs for molecular identification of Candida spp using real-time PCR.22
At each contact, women were asked about their nipple pain (In the last 48 h, have you experienced nipple pain/discomfort?) and whether it was burning in quality (If yes, would you describe your nipple pain as burning?), clinical signs and symptoms of mastitis as used in previous research (ie, redness, fever, etc),26 and other types of breast pain (Have you had other breast pain in the last 2 days? No/I have had stabbing (radiating or shooting) breast pain only/I have had non-stabbing breast pain only/I have had both stabbing and non-stabbing breast pain). We also asked, ‘Do you have nipple vasospasm? (Nipple blanches or goes white in the cold or during/after feeds) No/Yes, for less than 5 min/Yes, for more than 5 min/Not sure’. Researchers also collected clinical observations of the nipple/areola and breast at each visit (weeks 1–4), including the colour of the nipple/areola. Our case definition of ‘nipple and breast thrush’ used a combination of burning nipple pain and breast pain (non-mastitis). Francis-Morrill et al found nipple appearance (‘shiny’ or ‘flaky’ nipple or with pink colour) to be predictive of Candida.27 However, in our study, very few women were described as having these appearances (shiny, n=4, flaky, n=17), while 140 women were described as having ‘pink’ nipple/s. Adding the appearance identifiers to our case definition was not helpful. Clinically, the symptoms of nipple and breast thrush develop in the first week postpartum, and since most pain in the first week postpartum in first-time mothers is likely to be due to adjustment of the body to breastfeeding, we examined the case definition at weeks 1–8, and weeks 2–8 separately.
Statistical analysis was conducted using Stata V.12. Hypothesis 1—women with nipple/breast thrush are more likely to have Candida spp isolated from culture than other women; hypothesis 2—women with nipple/breast thrush are more likely to have S aureus isolated than other women. A sample of 318 women was estimated to provide adequate power.22 χ2 tests were used for comparing categorical variables. We investigated the incidence of nipple/breast thrush using a multivariable discrete version of the proportional hazards regression model.28 Outcome variable was the incidence of new cases of our nipple and breast thrush definitions; time-varying predictors were: the presence of Candida spp, presence of S aureus and mother-reported nipple damage. We present crude rate ratios (RR), and multivariate analysis, adjusting for the presence of Candida spp, S aureus and nipple damage.
Results relating to mastitis, other breastfeeding and postpartum problems will be published separately (papers in preparation).
Results
Fourteen women withdrew from the study after giving birth, leaving 346 (96%) women available for data collection at subsequent visits; 340 (94%) women completed the study at 8 weeks postpartum. Women who participated in the study were highly educated (77% had a tertiary degree or higher) and most were married or lived with their partner (96%) (table 1). Just over half gave birth in a private hospital (56%), 45% by Caesarean section.
Table 1.
Characteristics of nulliparous women recruited in late pregnancy
| Maternal characteristics (n=346) | n (%) |
|---|---|
| Hospital | |
| Royal Women's Hospital (public) | 154 (44.5) |
| Frances Perry House (private) | 192 (55.5) |
| Age (years—mean (SD) and range) | 32.7 (4.1, 19–44) |
| Marital status | |
| Married | 229 (66) |
| Unmarried, living with partner | 103 (30) |
| Not living with partner | 2 (1) |
| Separated/divorced | 1 (0) |
| Single | 11 (3) |
| Education level | |
| Tertiary degree or higher | 267 (77) |
| Other | 79 (23) |
| Gestation at recruitment (weeks—mean (SD) and range) | 37 (1.3, 34–42) |
| Gestation at birth (weeks—mean (SD) and range) | 39 (1.2, 36–42) |
| Breastfeeding intention (months—mean and range) | 9.7 (1–24) |
| Caesarean birth | 156 (45) |
| Baby sex—male | 168 (49) |
| Any breast milk feeding at 8 weeks postpartum (n=340) | 320 (94) |
Burning nipple pain was reported by 42% of women (146/346) during weeks 1–8, or 32% women (111/346) during weeks 2–8. Radiating or non-radiating breast pain (not related to engorgement/mastitis) was reported by 54% of women (186/346) during weeks 1–8, or 47% of women (162/346) during weeks 2–8. Combining these symptoms to estimate the number of women with both burning nipple pain and non-mastitis breast pain (at the same time), there were 19% of women in weeks 1–8 (65/346), or 15% in weeks 2–8 (50/346).
Candida albicans was the most commonly isolated Candida spp in culture with Candida glabrata only isolated in one nipple specimen and one milk sample (table 2). Although ‘other Candida spp.’ were found, none speciated as Candida krusei or Candida kefyr. Candida PCR of the nipple was positive for Candida spp in 33% of women (115/346), in contrast to culture of only 3% of women (9/346) being positive for Candida spp. Candida spp were isolated from the culture of breast milk samples from 5% of the women (18/346), but no molecular analyses were conducted on these samples. Table 3 shows Candida isolated from the culture and by PCR on each visit. S aureus was isolated from the culture of the nipple and/or breast milk in 67% of women (231/346), and from the nose and/or mouth of 73% of infants (253/346) at some point during follow-up. There were 22 milk samples positive for Candida, of which 10 were only milk, and 12 were positive for nipple and milk. For S aureus, 425 milk samples were positive, of which 89 were positive in milk only.
Table 2.
Results from microbiological analysis of specimens collected from 346 women and their infants (at any time point)
| Culture positive | PCR positive | Either culture/PCR positive | |
|---|---|---|---|
| Nipple* | |||
| Candida albicans | 13 | 15 | 19 |
| Candida glabrata | 1 | 3 | 4 |
| Candida spp | 9 | 115 | 120 |
| Any Candida spp | 21 | 116 | 125 |
| Staphylococcus aureus | 206 (60%) | N/A | N/A |
| Breast milk† | |||
| C albicans | 9 | N/A | N/A |
| C glabrata | 1 | N/A | N/A |
| Candida spp | 10 | N/A | N/A |
| Any Candida spp | 18 | N/A | N/A |
| S aureus | 186 (54%) | N/A | N/A |
| Infant nose/mouth† | |||
| C albicans | 15 | N/A | N/A |
| C glabrata | 0 | N/A | N/A |
| Candida spp | 5 | N/A | N/A |
| Any Candida spp | 18 | N/A | N/A |
| S aureus | 253 (73%) | N/A | N/A |
| Any Candida spp in nipple/breast milk | 131 (38%) | ||
| Any Candida spp in nipple/breast milk/baby | 133 (38%) | ||
| Any S aureus in nipple/breast milk | 231 (67%) | ||
| Any S aureus in nipple/breast milk/baby | 277 (80%) |
*Nipple swabs collected at late pregnancy, hospital, weeks 1–4.
†Breast milk, and infant nasal and oral swabs, collected at hospital, weeks 1–4.
N/A, not applicable.
Table 3.
Candida positive on PCR or culture at each visit
| Candida PCR positive | Candida PCR negative | Total | |
|---|---|---|---|
| Candida culture positive | 88 | 41 | 129 |
| Candida culture negative | 169 | 1817 | 1986 |
| Total | 257 | 1858 | 2115 |
Burning nipple pain was very common in week 1, primarily as women adjusted to breastfeeding; therefore, we explored the relationship between Candida spp and S aureus using two case definitions: weeks 1–8 and weeks 2–8 (table 4). There was a statistically significant association between these symptoms in weeks 2–8 and Candida spp in nipple/breast milk/baby (p=0.014); as also for Candida spp in vagina/nipple/breast milk/baby (p=0.047, not shown). S aureus was common in nipple/breast milk/baby samples of women with these symptoms as well as in women without these symptoms (82% vs 79%) (p=0.597, table 4).
Table 4.
Case definition and Candida spp (culture or PCR) and Staphylococcus aureus separately (n=346)
| Nipple/breast thrush case definition: burning nipple pain weeks plus breast pain (non-mastitis) | ||
|---|---|---|
| Weeks 1–8 | ||
| Candida spp in culture/PCR (nipple/breast milk/baby)* | ||
| Nipple/breast thrush case definition | Yes (n=127) | No (n=219) |
| Yes (n=65) | 31 (48%) | 34 (21%) |
| No (n=281) | 96 (34%) | 185 (66%) |
| Staphylococcus aureus (nipple/breast milk/baby)† | ||
| Nipple/breast thrush case definition | Yes (n=274) | No (n=72) |
| Yes (n=65) | 52 (80%) | 13 (20%) |
| No (n=281) | 222 (79%) | 59 (21%) |
| Nipple/breast thrush case definition: burning nipple pain weeks plus breast pain (non-mastitis) | ||
|---|---|---|
| Weeks 2–8 | ||
| Candida spp in culture/PCR (nipple/breast milk/baby)‡ | ||
| Nipple/breast thrush case definition | Yes (n=127) | No (n=219) |
| Yes (n=50) | 26 (52%) | 24 (48%) |
| No (n=296) | 101 (34%) | 195 (66%) |
| S aureus (nipple/breast milk/baby)§ | ||
| Nipple/breast thrush case definition | Yes (n=274) | No (n=72) |
| Yes (n=50) | 41 (82%) | 9 (18%) |
| No (n=296) | 233 (79%) | 63 (21%) |
| Nipple/breast thrush case definition: burning nipple pain weeks plus breast pain (non-mastitis), excluding vasospasm | ||
|---|---|---|
| Weeks 2–8 | ||
| Candida spp in culture/PCR (nipple/breast milk/baby)¶ | ||
| Nipple/breast thrush case definition, excluding vasospasm | Yes (n=127) | No (n=219) |
| Yes (n=48) | 26 (54%) | 22 (46%) |
| No (n=298) | 101 (34%) | 197 (66%) |
| S aureus (nipple/breast milk/baby)** | ||
| Nipple/breast thrush case definition, excluding vasospasm | Yes (n=274) | No (n=72) |
| Yes (n=48) | 40 (83%) | 8 (17%) |
| No (n=298) | 234 (79%) | 64 (21%) |
| Nipple/breast thrush case definition: burning nipple pain weeks plus breast pain (non-mastitis) | ||
|---|---|---|
| Weeks 1–8 | ||
| Candida spp in culture only (nipple)†† | ||
| Nipple/breast thrush case definition | Yes (n=21) | No (n=325) |
| Yes (n=65) | 9 (14%) | 56 (86%) |
| No (n=281) | 12 (4%) | 269 (96%) |
*χ2(1)=4.1587, p=0.041.
†χ2(1)=0.0318, p=0.858.
‡χ2(1)=5.8850, p=0.015.
§χ2(1)=0.2799, p=0.597.
¶χ2(1)=7.3142, p=0.007.
**χ2(1)=0.5804, p=0.446.
††χ2(1)=8.4905, p=0.004.
As women with nipple vasospasm described burning, radiating pain, we have also analysed the case definition excluding women with vasospasm (see table 4). Only two women were removed from the analysis (n=48), which made little difference to the results.
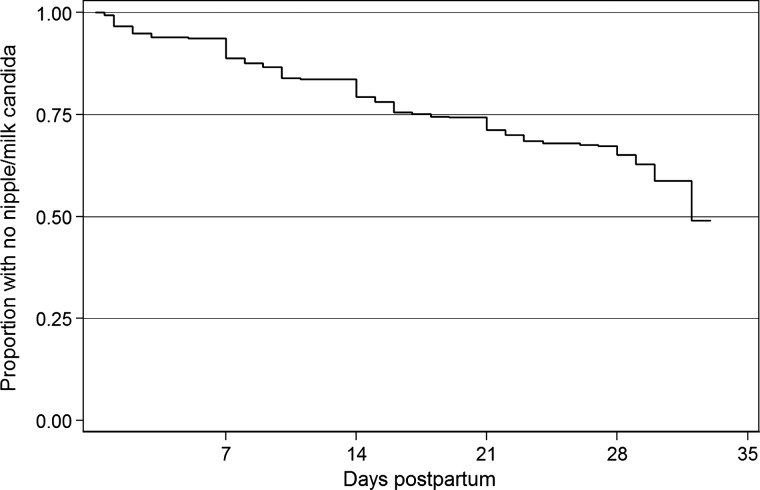
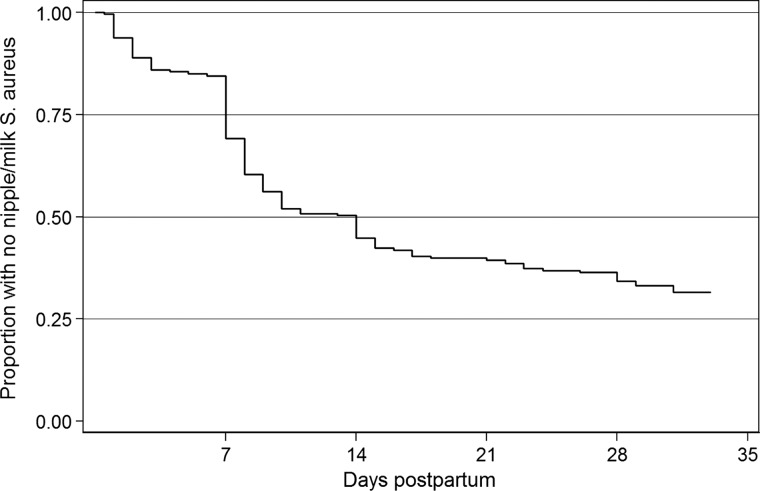
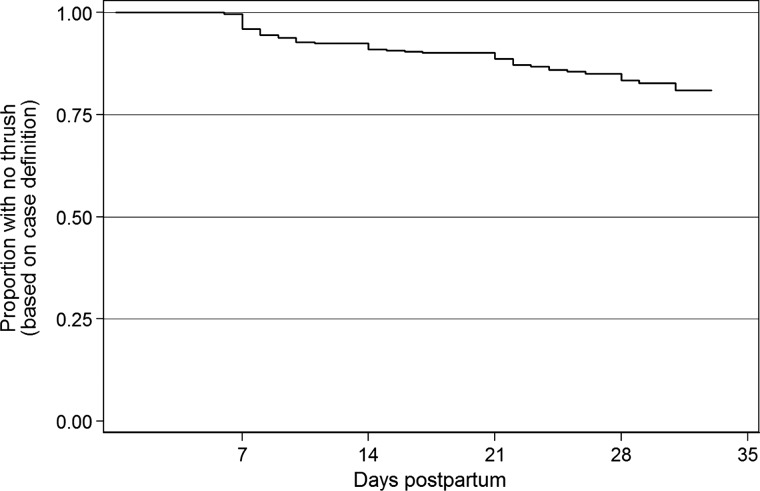
Time-to-event analysis examined predictors of our case definition of nipple/breast thrush (burning nipple and breast pain (non-mastitis)) up to and including the time of data collection in the first 4 weeks. (See unadjusted survival curves: figures 1–3 and table 5). Candida in nipple/breast milk/baby predicted incidence of the case definition (RR 1.87 (95% CI 1.10 to 3.16, p=0.018). Thus, for women with Candida in the nipple/milk/baby at any time point, the rate of subsequently developing the case definition was increased by 87%, compared to women without Candida. The evidence for S aureus colonisation as a predictor of these symptoms was not strong (RR 1.53, 95% CI 0.88 to 2.64, p=0.13). Mothers’ report of nipple damage was a predictor of these symptoms, with an RR of 2.30 (95% CI 1.19 to 4.43, p=0.012). In the multivariate model, with all three predictors, the RRs were very similar to the univariate RRs. This indicates that Candida and nipple damage are independent predictors of our case definition.
Figure 1.
Survival curve for first time to nipple/milk Candida.
Figure 2.
Survival curve for time to first nipple/milk Staphylococcus aureus.
Figure 3.
Survival curve for time to first symptoms of case definition of ‘breast thrush’.
Table 5.
Time-to-event analysis of predictors of first symptoms of case definition
| Events* | Years at risk† | Rate ratio (95% CI) | p Value | Multivariate rate ratio (95% CI) | p Value | |
|---|---|---|---|---|---|---|
| Candida (nipple/milk/baby) | ||||||
| No | 35 | 18.3 | ||||
| Yes | 23 | 6.4 | 1.87 (1.10 to 3.16) | 0.018 | 2.03 (1.19 to 3.45) | 0.009 |
| Staphylococcus aureus (nipple/milk) | ||||||
| No | 19 | 10.5 | ||||
| Yes | 39 | 14.2 | 1.53 (0.88 to 2.64) | 0.128 | 1.41 (0.80 to 2.46) | 0.234 |
| Nipple damage | ||||||
| No | 11 | 8.7 | ||||
| Yes | 47 | 16.1 | 2.3 (1.19 to 4.43) | 0.012 | 2.39 (1.21 to 4.70) | 0.012 |
*Women with case definition in the first 4 weeks postpartum.
†Total observed time between birth and first symptoms of case definition or 4-weeks postpartum (whichever occurred first).
Discussion
Principal findings
Unlike some cross-sectional studies which found no relationship between the presence of Candida spp and the condition known as breast thrush,9 10 we have shown that Candida spp is associated with burning nipple pain and breast pain—in two analyses (‘at any time’ and ‘time-to-event’). As in previous studies,1 7 we uncommonly isolated Candida spp from the nipple using standard microbiological culture techniques. However, Candida spp. were more commonly identified using more sensitive molecular techniques (real-time PCR). This test is not used in routine practice currently, and therefore it is not helpful in making the diagnosis in clinical care at this time. Candida spp were also rarely isolated in breast milk, using standard techniques. It is possible that the isolation rate would have been higher if we had used the technique of Morrill and colleagues,29 who added iron to inactivate milk lactoferrin. However, Hale et al were unable to identify Candida in breast milk of women with ‘Candida mastitis’ using culture and another specific technique (presence of 1→3-β-D-glucan).10 The 16 cases had ‘sore, inflamed, or traumatised nipples, intense stabbing or burning pain that radiated into the axilla often persisting after feeding, and painful feeding without alternate diagnosis’.10 Possible explanations for Hale et al's findings are that the women had other causes of pain (from the traumatised nipple, from maternal vasospasm, or infant posterior tongue-tie or other mechanical causes of pain); that Candida was present in the nipple (samples were only collected from the milk), or that Candida is not present in the milk of women with this syndrome. The question as to whether Candida is present in the lactiferous ducts is still open to debate; what we have shown is a link between Candida and nipple/breast pain—independent of the presence of nipple damage or S aureus.
Candida spp are commensal organisms, and therefore the presence of Candida spp does not always imply infection. Recent understanding of vulvovaginitis postulates that the threshold number of organisms for symptomatic vaginitis varies for different groups of women; women with infrequent vaginitis have a higher threshold.30 Furthermore, the symptoms associated with vaginitis may be caused by the host neutrophil response; small numbers of organisms may promote an aggressive inflammatory response in some women.30
Consistent with other studies of mothers and infants,21 31–34 colonisation with S aureus is common; at least 50% of women were colonised with S aureus in the nipple or milk samples by 4 weeks postpartum. Therefore in clinical practice, a finding of S aureus in the nipple or breast milk is not evidence that the bacteria are the principal cause of the woman's pain. Our analysis indicates that candida and S aureus are acting independently, despite often coexisting. The case-control study of women with a clinical diagnosis of nipple and breast thrush by Panjaitan et al,35 which only used molecular techniques from nipple swabs and excluded women with clinical signs of bacterial infection (exudate on nipple or inflamed breast), found that S aureus was present in equal numbers of cases and controls.
Clinical implications
Diagnostic skills are needed to make a diagnosis of nipple/breast candidiasis; clinicians should routinely consider all causes of nipple and breast pain, in the same way they consider differential diagnoses when assessing a patient with chest pain.36 Women with nipple damage or with nipple vasospasm describe pain that is burning in quality; in the past, this has often been misdiagnosed as Candida infection.37 The pain clinically associated with Candida infection is persistent, ranges from mild to severe, and is not relieved by the use of nipple shields or expressing/pumping, or applying heat. When the pain is related directly to infant feeding, the cause is likely to be mechanical, and when the pain is relieved by heat, vasospasm is the likely cause.19 We found that nipple damage was associated with burning nipple and radiating breast pain, so clinicians should be cautious about diagnosing infection (whether fungal or bacterial) in every woman with nipple damage.
Strengths and limitations
The strength of this study is that a cohort of healthy women who had not previously breastfed was recruited prior to starting breastfeeding and was followed closely until 2 months postpartum. It is the first prospective longitudinal study to examine simultaneously both S aureus and Candida spp in a cohort of breastfeeding women and their infants.
The main limitation is that we did not have a clinical diagnosis of nipple/breast thrush and had to use a case definition based on two symptoms to estimate this condition. Participants responded to questions about pain and nipple blanching, and research assistants reported nipple appearance, but these measures could not substitute for a clinical assessment. Furthermore, infant oral anatomy was not examined to exclude tongue-tie, and breastfeeds were not observed. We are not implying that all women with burning nipple and breast pain had a clinical diagnosis of nipple/breast thrush. We hypothesise that Candida is associated with nipple/breast pain in some women, in a similar manner to the relationship between Candida and vulvovaginal symptoms: Candida is a commensal in some women, while other women experience significant pain when only small numbers of organisms are present.30
Another limitation is that we only followed the cohort for 8 weeks postpartum—with microbiological data to only 4 weeks postpartum; women who developed problems after this time period were not captured in our data collection.
Conclusions
This large cohort study provides evidence that Candida spp play a role in nipple and breast pain in lactating women; however, burning nipple pain is common in breastfeeding women, and a diagnosis of Candida spp infection should not be made without considering differential diagnoses.4 Further research into the role of staphylococci in breast pain in lactating women with inflammatory symptoms and without is needed. Animal models, as have been used in vulvovaginal candidiasis,30 may be required to fully understand the pathogenesis of this condition. Future researchers may consider the RCTs for treatment or clearance of Candida.
Supplementary Material
Footnotes
Contributors: LHA conceived the study, which was designed in collaboration with all authors. SMD managed the data and conducted the statistical analyses. SMG, SNT, CMB and MSP provided microbiological expertise into study design, analysis and writing of the paper. MC was the project coordinator and contributed to the questionnaire design. MSP was the research scientist. LHA drafted the manuscript which was critically revised by all authors.
Funding: This study received financial support from the National Health & Medical Research Council (NHMRC) (project grant 541907, equipment grant, Health Professional Training Fellowship (LHA)), Helen Mcpherson Smith Trust, Faculty Research Grant, Faculty of Health Sciences, La Trobe University.
Competing interests: None.
Ethics approval: This study was approved by the La Trobe University Human Ethics Committee (06–078); Human Research Ethics Committee of the Royal Women's Hospital (06/41); Human Research Ethics Committee of the University of Melbourne (1033949); and Medical Advisory Committee at Frances Perry House.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Amir LH, Garland SM, Dennerstein L, et al. Candida albicans: is it associated with nipple pain in lactating women? Gynecol Obstet Invest 1996;41:30–4 [DOI] [PubMed] [Google Scholar]
- 2.Montgomery AM. Breastfeeding and postpartum maternal care. Prim Care 2000;27:237–50 [DOI] [PubMed] [Google Scholar]
- 3.Brent NB. Thrush in the breastfeeding dyad: results of a survey on diagnosis and treatment. Clin Pediatr (Phila) 2001;40:503–6 [DOI] [PubMed] [Google Scholar]
- 4.Moorhead AM, Amir LH, O'Brien PW, et al. A prospective study of fluconazole treatment for breast and nipple thrush. Breastfeed Rev 2011;19:25–9 [PubMed] [Google Scholar]
- 5.Hoddinott P, Tappin D, Wright C. Breast feeding. BMJ 2008;336:881–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heller MM, Fullerton-Stone H, Murase JE. Caring for new mothers: diagnosis, management and treatment of nipple dermatitis in breastfeeding mothers. Int J Dermatol 2012;51:1149–61 [DOI] [PubMed] [Google Scholar]
- 7.Thomassen P, Johansson VA, Wassberg C, et al. Breast-feeding, pain and infection. Gynecol Obstet Invest 1998;46:73–4 [DOI] [PubMed] [Google Scholar]
- 8.Carmichael AR, Dixon JM. Is lactation mastitis and shooting breast pain experienced by women during lactation caused by Candida albicans? Breast 2002;11:88–90 [DOI] [PubMed] [Google Scholar]
- 9.Graves S, Wright W, Harman R, et al. Painful nipples in nursing mothers: fungal or staphylococcal? A preliminary study. Aust Fam Physician 2003;32:570–1 [PubMed] [Google Scholar]
- 10.Hale TW, Bateman TL, Finkelman MA, et al. The absence of Candida albicans in milk samples of women with clinical symptoms of ductal candidiasis. Breastfeed Med 2009;4:57–61 [DOI] [PubMed] [Google Scholar]
- 11.Dixon JM, Khan LR. Treatment of breast infection. BMJ 2011;342:484–9 [DOI] [PubMed] [Google Scholar]
- 12.Amir LH, The Academy of Breastfeeding Medicine protocol committee. ABM clinical protocol # 4: mastitis, revision, May 2008. Breastfeed Med 2008;3:177–80 [DOI] [PubMed] [Google Scholar]
- 13.Hanna L, Cruz SA. Candida mastitis: a case report. Perm J 2011;15:62–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eglash A, Plane MB, Mundt M. History, physical and laboratory findings, and clinical outcomes of lactating women treated with antibiotics for chronic breast and/or nipple pain. J Hum Lact 2006;22:429–33 [DOI] [PubMed] [Google Scholar]
- 15.Watson Genna C. The influence of anatomical and structural issues on sucking skills. In: eds. Watson Genna C, Supporting sucking skills in breastfeeding infants. Sudbury, MA: Jones and Bartlett Publishers, 2008:181–226 [Google Scholar]
- 16.Barankin B, Gross MS. Nipple and areolar eczema in the breastfeeding woman. J Cutan Med Surg 2004;8:126–30 [DOI] [PubMed] [Google Scholar]
- 17.Livingstone V, Stringer LJ. The treatment of Staphylococcus aureus infected sore nipples: a randomized comparative study. J Hum Lact 1999;15:241–6 [DOI] [PubMed] [Google Scholar]
- 18.Page SM, McKenna DS. Vasospasm of the nipple presenting as painful lactation. Obstet Gynec 2006;108:806–8 [DOI] [PubMed] [Google Scholar]
- 19.Amir LH. Breast pain in lactating women—mastitis or something else? Aust Fam Physician 2003;32:141–5 [PubMed] [Google Scholar]
- 20.Anderson JE, Held N, Wright K. Raynaud's phenomenon of the nipple: a treatable cause of painful breastfeeding. Pediatrics 2004;113:e360–4 [DOI] [PubMed] [Google Scholar]
- 21.Peacock SJ, Justice A, Griffiths D, et al. Determinants of acquisition and carriage of Staphylococcus aureus in infancy. J Clin Microbiol 2003;41:5718–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amir LH, Cullinane M, Garland SM, et al. The role of micro-organisms (Staphylococcus aureus and Candida albicans) in the pathogenesis of breast pain and infection in lactating women: study protocol. BMC Pregnancy Childbirth 2011;11:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stuebe A. Lactation culture protocol. 2011. http://www.mombaby.org/PDF/culture_protocol.2.0.pdf (accessed 3 Mar 2013).
- 24.Weissenbacher T, Witkin SS, Ledger WJ, et al. Relationship between clinical diagnosis of recurrent vulvovaginal candidiasis and detection of Candida species by culture and polymerase chain reaction. Arch Gynecol Obstet 2009;279:125–9 [DOI] [PubMed] [Google Scholar]
- 25.Tabrizi SN, Pirotta MV, Rudland E, et al. Detection of Candida species by PCR in self-collected vaginal swabs of women after taking antibiotics (letter). Mycoses 2006;49:523–4 [DOI] [PubMed] [Google Scholar]
- 26.Amir LH, Forster DA, Lumley J, et al. A descriptive study of mastitis in Australian breastfeeding women: incidence and determinants. BMC Public Health 2007;7:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Francis-Morrill J, Heinig MJ, Pappagianis D, et al. Diagnostic value of signs and symptoms of mammary candidosis among lactating women. J Hum Lact 2004;20:288–95 [DOI] [PubMed] [Google Scholar]
- 28.Carlin JB, Wolfe R, Coffey C, et al. Analysis of binary outcomes in longitudinal studies using weighted estimating equations and discrete-time survival methods: prevalence and incidence of smoking in an adolescent cohort. Stat Med 1999;18:2655–79 [DOI] [PubMed] [Google Scholar]
- 29.Morrill JF, Pappagianis D, Heinig MJ, et al. Detecting Candida albicans in human milk. J Clin Microbiol 2003;41:475–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fidel PLJ. History and update on host defense against vaginal candidiasis. Am J Reprod Immunol 2007;57:2–12 [DOI] [PubMed] [Google Scholar]
- 31.Amir LH, Garland SM, Lumley J. A case-control study of mastitis: nasal carriage of Staphylococcus aureus. BMC Fam Pract 2006;7:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kawada M, Okuzumi K, Hitomi S, et al. Transmission of Staphylococcus aureus between healthy, lactating mothers and their infants by breastfeeding. J Hum Lact 2003;19:411–17 [DOI] [PubMed] [Google Scholar]
- 33.Jimenez-Truque N, Tedeschi S, Saye EJ, et al. Relationship between maternal and neonatal Staphylococcus aureus colonization. Pediatrics 2012;129:e1252–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leshem E, Maayan-Metzger A, Rahav G, et al. Transmission of Staphylococcus aureus from mothers to newborns. Pediatr Infect Dis J 2012;31:360–3 [DOI] [PubMed] [Google Scholar]
- 35.Panjaitan M, Amir LH, Costa A-M, et al. Polymerase chain reaction in detection of Candida albicans for confirmation of clinical diagnosis of nipple thrush (letter). Breastfeed Med 2008;3:185–7 [DOI] [PubMed] [Google Scholar]
- 36.Yelland M, Cayley WE, Jr, Vach W, et al. An algorithm for the diagnosis and management of chest pain in primary care. Med Clin North Am 2010;94:349–74 [DOI] [PubMed] [Google Scholar]
- 37.Morino C, Winn SM. Raynaud's phenomenon of the nipples: an elusive diagnosis. J Hum Lact 2007;23:191–3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.