Abstract
Objectives
The aim of this systematic review is to appraise the evidence for the use of anti-VEGF drugs and steroids in diabetic macular oedema (DMO) as assessed by change in best corrected visual acuity (BCVA), central macular thickness and adverse events
Data source
MEDLINE, EMBASE, Web of Science with Conference Proceedings and the Cochrane Library (inception to July 2012). Certain conference abstracts and drug regulatory web sites were also searched.
Study eligibility criteria, participants and interventions
Randomised controlled trials were used to assess clinical effectiveness and observational trials were used for safety. Trials which assessed triamcinolone, dexamethasone, fluocinolone, bevacizumab, ranibizumab, pegaptanib or aflibercept in patients with DMO were included.
Study appraisal and synthesis methods
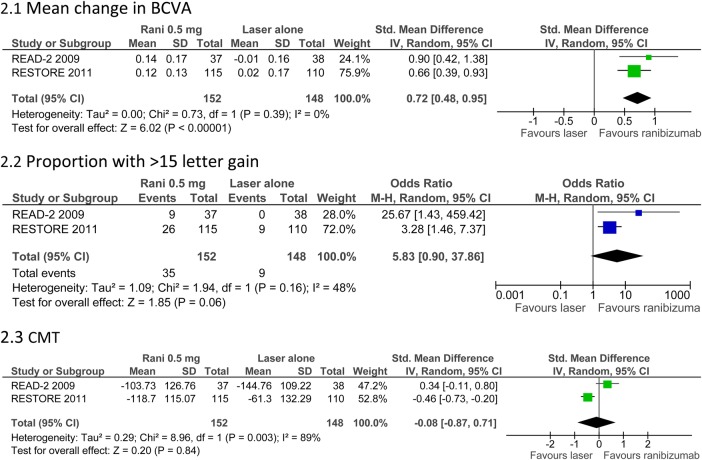
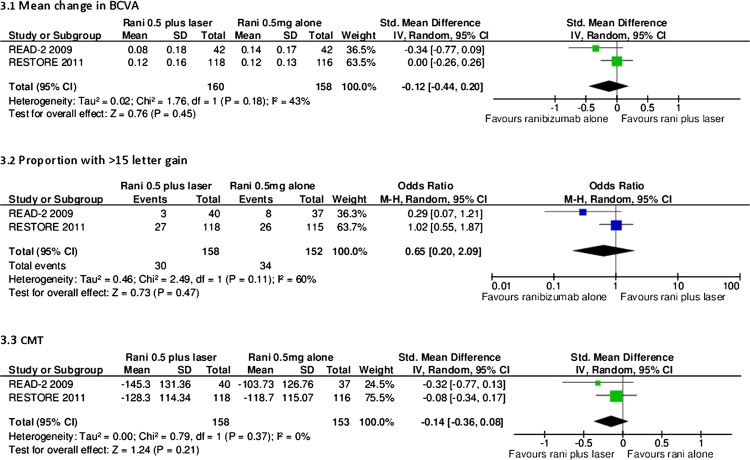
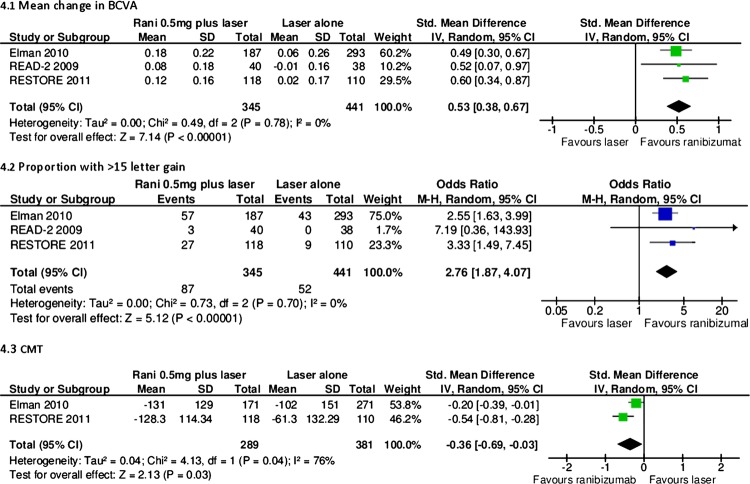
Risk of bias was assessed using the Cochrane risk of bias tool. Study results are narratively described and, where appropriate, data were pooled using random effects meta-analysis.
Results
Anti-VEGF drugs are effective compared to both laser and placebo and seem to be more effective than steroids in improving BCVA. They have been shown to be safe in the short term but require frequent injections. Studies assessing steroids (triamcinolone, dexamethasone and fluocinolone) have reported mixed results when compared with laser or placebo. Steroids have been associated with increased incidence of cataracts and intraocular pressure rise but require fewer injections, especially when steroid implants are used.
Limitations
The quality of included studies varied considerably. Five of 14 meta-analyses had moderate or high statistical heterogeneity.
Conclusions and implications of key findings
The anti-VEGFs ranibizumab and bevacizumab have consistently shown good clinical effectiveness without major unwanted side effects. Steroid results have been mixed and are usually associated with cataract formation and intraocular pressure increase. Despite the current wider spectrum of treatments for DMO, only a small proportion of patients recover good vision (≥20/40), and thus the search for new therapies needs to continue.
Keywords: Ophthalmology
Article summary.
Article focus
To review the evidence for triamcinolone, dexamethasone, fluocinolone, bevacizumab, ranibizumab, pegaptanib and aflibercept in the treatment of diabetic macular oedema.
Key messages
The anti-VEGFs ranibizumab and bevacizumab have consistently shown good clinical effectiveness in the short term without major unwanted side effects.
Steroid results have been mixed and are usually associated with cataract formation and IOP increase.
Strengths and limitations of this study
A robust, detailed review of the literature has been undertaken and, when appropriate, data have been combined in meta-analysis.
The quality of studies included varied considerably.
Introduction
Diabetic macular oedema (DMO) is a complication of diabetic retinopathy and a leading cause of blindness. The prevalence of DMO is likely to increase with more people suffering from diabetes.1 Increasing DMO has significant implications for patients, healthcare providers and wider society. Laser has been the mainstay of treatment, but recently antivascular endothelial growth factor (anti-VEGF) drugs and steroids have been introduced as potential alternatives to laser photocoagulation.
Burden of disease
Diabetic retinopathy is present at the time of diagnosis of diabetes mellitus in 0–30% of individuals.2 The incidence is estimated to be 2.3/100 person-years for the overall diabetic population and 4.5 for patients on insulin therapy.3 There is good evidence that progression to DMO is associated with duration of disease,4–7 poor glycaemic control8 and, in type 2 diabetes, the need for insulin,9 though the need for insulin therapy is more a marker for duration and poor control.
The number of people with DMO is likely to increase as diabetes becomes more common. Some reports have suggested a decrease in progression to severe visual loss between 1975–1985 and 1986–2008 in a combined population of types 1 and 2.10 Regular screening for retinopathy and better glycaemic control are thought to have reduced the progression to severe visual loss. Diabetic retinopathy is associated with a reduced quality of life. Compared with all diabetic complications, blindness was perceived to be the third worst health state after a major stroke and amputation.11
In the USA, the presence of DMO at diagnosis is associated with 29% additional costs within the first 3 years compared with individuals without retinopathy at diagnosis.12 In 2010, the estimated healthcare costs for DMO in England were £92 million, with £65.6 million being spent on hospital treatment and related costs.13
Visual impairment results in increased welfare costs, early retirement and costs of home help and carers.14 In England in 2010 (total population 52.23 million), the estimated population with diabetes was 2.34 million; the above social costs were estimated to be £11.6 million for DMO.13
Overview of pathophysiology
DMO is caused mainly by disruption of the blood-retinal barrier. The complex pathway that leads to this disruption has been previously described in this journal.15 Sustained hyperglycaemia causes a multifactorial cascade of physiological processes, involving increased permeability, cytokine activation, altered blood flow, hypoxia and inflammation. Vascular endothelial growth factor-A (VEGF-A) is a major contributor to the inflammatory process and, in particular, to angiogenesis and permeability.16 Hypoxia caused by microvascular disease stimulates the release of VEGF-A to aid perfusion. There are six major isoforms of VEGF-A: 121, 145, 165, 183, 189 and 206. In addition to causing widespread microvascular injury, there is now evidence that hyperglycaemia results in preceding neuronal dysfunction, which may contribute to visual loss.17
Overview of current treatments
Laser photocoagulation has been the mainstay of treatment for DMO. The landmark Diabetic Retinopathy Study18 and the Early Treatment Diabetic Retinopathy Study (ETDRS)19 20 demonstrated its clinical effectiveness. However, although laser photocoagulation was clearly effective in preserving vision, it was less successful in restoring it, once lost. Furthermore, patients with perifoveal ischaemia are not amenable to this form of therapy. In EDTRS, although laser was shown to reduce the risk of moderate visual loss (a loss of three ETDRS lines) by 50%, visual acuity improved in only 3% of patients.20 However, in some recent trials, laser has improved the proportion of patients with more than or equal to 10 letters by 7–31%.21–24 In addition, laser is not without side effects. Foveal burns, visual field defects, retinal fibrosis and laser scars have been reported.25 Over the following decade it became apparent that certain patients suffered severe visual loss despite aggressive treatment.26
Steroids and anti-VEGF drugs are newer treatments in DMO. Intravitreal corticosteroids have potent anti-inflammatory effects. Triamcinolone (Kenalog) is not licensed for eye use but has been used to treat DMO for over 10 years. Triamcinolone (Trivaris), recently, was licensed for eye use. The development of intravitreal implants has allowed sustained release formulations. Fluocinolone acetonide (Iluvien, Alimera Sciences) and dexamethasone (Ozudex, Allergan) are implants that have been introduced recently.
Anti-VEGF agents have shown efficacy compared with laser. Bevacizumab (Avastin, Genenetch/Roche) is a monoclonal antibody that targets all VEGF isoforms. Although being developed for colorectal cancer, it is widely used off-label, as an intravitreal treatment for macular oedema of different aetiologies. Ranibizumab (Lucentis, Genentech/Roche) is a fragment of the bevacizumab antibody (molecular weight of ranibizumab 48.4 KDa compared with 149 KDa for bevacizumab). It was designed specifically for use in the eye. Ranibizumab is considerably more expensive than bevacizumab (the estimated cost of ranibizumab is $2000/dose compared with $50 for bevacizumab).27 Pegaptanib (Macugen, Eyetech Pharmaceuticals/Pfizer) is a PEGylated aptamer, with a high affinity to the VEGF isoform 165, and was approved for the treatment of exudative AMD in 2004. Aflibercept (Regeneron/Bayer HealthCare) is a recent addition to the anti-VEGF class that targets all forms of VEGF-A and placental growth factor.
Aim of the review
The aim of this review is to provide clinicians with an up-to-date overview of current intraocular drug treatments for DMO. It is hoped that the information contained herein will assist clinicians to present their patients with the best evidence supporting each treatment, including possible complications. In addition, this review may be helpful to policy makers. The review focuses on the current evidence for the use of anti-VEGF drugs and steroids to treat DMO, as assessed by change in best corrected visual acuity (BCVA) (mean and proportion with more than two lines improvement), central macular thickness (CMT), as determined by optical coherence tomography (OCT), and their adverse events.
Evidence acquisition
A systematic literature search was performed. The databases searched included MEDLINE, EMBASE, Web of Science with Conference Proceedings and the Cochrane Library. The dates searched were from the inception of each database until July 2012.
The search terms combined the following key words:
ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or macugen or aflibercept or vegf trap-eye or steroid* or corticosteroid* or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor*
AND
DMO or diabetic macular edema or diabetic retinopathy or diabetic maculopathy
AND
(masked or sham or placebo OR control group or random*) OR (systematic review or meta-analysis) OR (risk or safety or adverse or harm or pharmacovigilance or side-effect* or precaution* or warning* or contraindication* or contra-indication* or tolerability or toxic)
The meeting abstracts of the Association for Research in Vision and Ophthalmology, the American Diabetes Association (2002–2012) and the European Association for the Study of Diabetes were searched from 2002 to 2012.
In addition, the web sites of the European Medicines Agency and the US Food and Drug Association were searched for data on registration status and safety. Clinicaltrials.gov and the EU Clinical Trials Register were searched in July 2012 for data on ongoing research.
Full details of the searches are shown in appendix 1.
Randomised controlled trials (RCT) were used to evaluate clinical effectiveness. Safety was assessed through both RCTs and observational studies.
RCTs were included provided that they (1) addressed the use of triamcinolone, dexamethasone, fluocinolone, bevacizumab, ranibizumab, pegaptanib or aflibercept in patients with DMO, (2) had a minimum follow-up of 6 months and (3) had a minimum of 25 eyes per study arm. Studies were excluded if they (1) evaluated laser only, (2) assessed the effect of the aforementioned treatments in macular oedema due to other retinal diseases (instead of DMO), (3) used only a single dose, (4) were combined with a surgical intervention or (5) published studies in languages other than English. There were no exclusions based on drug dose. Trials were excluded if they evaluated combined drug treatment with surgery or systemic treatment.
Search results were screened by two independent authors (JF and PR/DS). Data were extracted by one author (CC) and checked by a second (JF). Data extracted included inclusion/exclusion criteria, baseline demographics, BCVA expressed as a change in logMAR/ETDRS letters or proportion of participants with more than two or three lines BCVA improvement, CMT and adverse events. Risk of bias was assessed using the Cochrane risk of bias tool.
Studies were assessed for similarity in study population, interventions (dose and frequency), outcomes and time to follow-up, with a view to including similar studies in a meta-analysis. Conference abstracts were excluded from the meta-analysis because their quality and detailed methodology were not clear. A difference of 6 months was allowed between study follow-ups because of the potential heterogeneity from disease progression and differences in the number of doses prescribed. If salient data were not reported, such as SDs, data were sought by personal communication with authors. Data were analysed using Review Manager software. If data from multiple time-points were available, the primary end-point data were used. Data were entered by one author (JF) and double-checked by a second (DS). Mean differences were calculated for change in BCVA and CMT and ORs were calculated for proportion of participants with more than two lines improvement. The 95% CIs were calculated for all outcomes. Statistical heterogeneity was measured through I2 scores. A score of less than 30% was considered as low heterogeneity, a score of more than 70% was considered as high heterogeneity and scores between 30% and 70% were considered as moderate. A random effects model was used throughout. The random effects model assumes variability between studies and therefore models uncertainty into the meta-analysis. Fixed assumes no variability. Generally speaking, the random effects model results in wider CIs.
Results
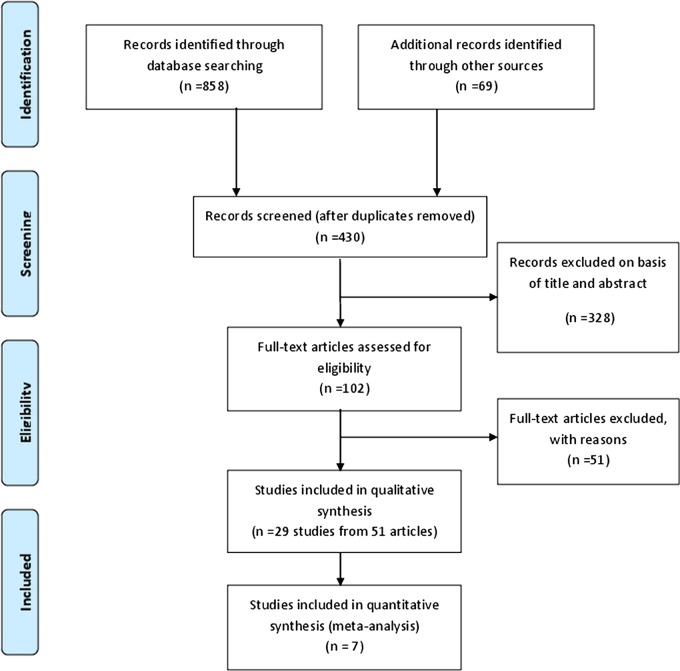
The literature search identified 430 unique articles for possible inclusion, as shown in figure 1. In total, 328 articles were excluded on the basis of title and abstract, leaving 102 full papers to be read. Fifty-one of these articles were excluded; the reasons for their exclusion are summarised in table 1. Fifty-one articles from 29 studies met the inclusion criteria and were included in the review; these are described in tables 3–16. Seven studies were suitable for meta-analysis.
Figure 1.
PRISMA flow diagram.
Table 1.
List of excluded studies
| Study | Reason |
|---|---|
| Active comparator trials | |
| Cho et al87 | Single dose |
| DRCRN 2010 (Googe et al)88 | <6 months f/u |
| Faghihi et al89 | Single dose |
| Figueroa et al90 | Single dose |
| Isaac et al91 | Single dose |
| Paccola et al92 | Single dose |
| Prager et al93 | <25 pts per arm |
| Ozturk et al94 | Non-RCT |
| Marey and Ellakwa95 | <6 months |
| Shahin and El-Lakkany96 | Single dose |
| Pegaptanib | |
| Loftus et al97 | Quality of life data |
| Ranibizumab | |
| Ferrone and Jonisch98 | <25 pts per arm |
| Bevacizumab | |
| Solaiman et al99 | Single dose |
| DRCRN—Scott et al100 | <25 pts per arm |
| Lee101 | Non-RCT |
| Isaac et al91 | Single dose |
| Trimacinolone | |
| Audren et al102 | Single dose (dosing study) |
| Audren et al103 | Single dose |
| Avitabile104 | Mixed RVO and DMO |
| Bandello et al105 | Case report+PDR |
| Bonini et al106 | Single dose injection technique |
| Cellini et al107 | Single injection PSTI |
| Cardillo et al108 | Single injection PSTI |
| Chung et al109 | Single injection PSTI |
| Dehghan et al110 | Single dose |
| DRCRN—Chew et al 111 | <25 pts per arm |
| Gil et al112 | <25 pts per arm |
| Entezari et al113 | <6 months |
| Hauser et al114 | Single dose |
| Jonas et al115 | Single dose |
| Joussen et al116 | Study protocol |
| Avci and Kaderli117 | Anaesthetic technique |
| Kang et al118 | Single dose |
| Kim et al119 | Single injection and CME |
| Lam et al120 | Single injection |
| Lee121 | Single injection |
| Maia et al122 | Single dose |
| Massin et al123 | Single dose |
| Mohamed et al124 | Post hoc analysis |
| Nakamura et al125 | Single dose |
| Spandau et al126 | Single dose |
| Tunc127 | <6 months |
| Verma et al128 | Single dose |
| Wickremasinghe et al129 | Single dose |
| Yalcinbayir et al130 | Single dose |
| Dexamethasone | |
| Haller et al131 | <6 months |
| Haller et al132 | <25 pts per arm |
| Kuppermann et al 133 | Mixture of macular oedema causes |
| Boyer et al134 | Non-randomised |
| Fluocinolone | |
| Campochiaro et al135 | <25 pts per arm |
| Diclofenac | |
| Elbendary71 | <35 pts per arm |
CME, cystoid macular edema; DMO, diabetic macular oedema PDR, proliferative diabetic retinopathy; PSTI, posterior subtenon injection; RVO, retinal vein occlusion.
Table 3.
Ranibizumab trials
| Study | Participants and baseline values | Intervention | Outcome (change from baseline at study end) | ||
|---|---|---|---|---|---|
| READ-2 Study (Nguyen et al)28
47 USA Multicenter Design: 3-arm RCT Follow-up: 6 months, 2-year extension (no relevant outcomes as IVR received by all groups by that time, no safety outcomes for 2-year data) |
N: 126 eyes of 126 patients Inclusion criteria: ≥18 years, type 1 or 2 DM, DMO, BCVA 20/40-20/320, CMT ≥250 µm, HbA1c ≥6% within 12 months before randomisation; expectation that scatter laser photocoagulation not required for 6 months Exclusion criteria: contributing causes to reduced BCVA other than DMO, focal/grid laser within 3 months, intraocular steroid within 3 months, intraocular VEGF antagonist within 2 months Age: 62 years Sex: 52–69% female Diabetes type: not reported HbA1c: 7.39–7.77% Baseline VA: ETDRS letter score 24.85–28.35 Baseline CMT: excess foveal thickness 198.75–262.52 µm Comorbidities: not reported |
Group 1 (IVR, n=42 eyes): IV injections of 0.5 mg ranibizumab at baseline, 1, 3 and 5 months Group 2 (L, n=42 eyes): focal/grid laser at baseline and 3 months if CMT ≥250 µm Group 3 (IVRL, n=42 eyes): IV injections of 0.5 mg ranibizumab at baseline and 3 months, followed by focal/grid laser treatment 1 week later Regimen for all groups: after 6 months, patients could receive IV injections of ranibizumab no more than every 2 months or focal/grid laser no more than every 3 months if CMT ≥250 µm Laser Modified ETDRS protocol was used |
At 6 months BCVA (ETDRS): |
||
| BCVA (letters) | p Value | ||||
| IVR | +7.24 | 0.0003 vs L | |||
| L | −0.43 | ||||
| IVRL | +3.80 | NS vs IVR or L |
|||
| Plus ≥3 lines | |||||
| IVR | 22% | <0.05 vs L | |||
| L | 0 | ||||
| IVRL | 8% | ||||
| CMT (OCT): | |||||
| CMT (µm) | p Value | ||||
| IVR | −106.3 | All <0.01 vs baseline, NS for elimination of ≥50% excess foveal thickness between groups | |||
| L | −82.8 | ||||
| IVRL | −117.2 | ||||
| READ-3 Study (Do et al) USA50 Design: phase 2, 2-arm RCT Follow-up: 6 months |
N: 152 eyes Inclusion criteria: NR Exclusion criteria: NR Age: NR Sex: NR Diabetes type: NR HbA1c: NR Baseline VA: Mean BCVA Snellen equivalent 20/63 in the 2.0 mg group and 20/80 in the 0.5 mg group Baseline CST (central subfield thickness): 432 µm in the 2.0 mg group and 441 µm in the 0.5 mg group Comorbidities: NR |
Group 1 (IVR2.0, n=NR): monthly injections Group 2 (IVR0.5, n=NR): monthly injections After month 6, eyes evaluated and additional ranibizumab injections given on an as needed basis if DMO still present on OCT. |
At 6 months: BCVA |
||
| Mean BCVA letters gain | p Value | ||||
| IVR2.0 | +7.46 | NR | |||
| IVR0.5 | +8.69 | NR | |||
| CST | CST reduction | ||||
| IVR2.0 | −163.86 µm | NR | |||
| IVR0.5 | −169.27 µm | NR | |||
| RESOLVE Study (Massin et al)36 Multicenter international Design: 3-arm placebo-controlled RCT Follow-up: 12 months |
N: 151 eyes of 151 patients Inclusion criteria: >18 years, type 1 or 2 DM, clinically significant DMO, BCVA 20/40–20/160, HbA1c <12%, decreased vision attributed to foveal thickening from DMO, laser photocoagulation could be safely withheld in the study eye for at least 3 months after randomisation Exclusion criteria: unstable medical status, panretinal laser photocoagulation performed within 6 months before study entry, previous grid/laser photocoagulation except patients with only mild laser burns at least 1000 µm from the centre of the fovea performed >6 months previously Age: 63–65 (range 32–85) years Sex: 43.1–49% female Diabetes type: 96.1–98% type 2 DM HbA1c: 7.3–7.6 (range 5.3–11.1) % Baseline VA: ETDRS letter score 59.2–61.2 SD9.0–10.2 Baseline CMT: 448.9–459.5 SD102.8–120.1 µm Comorbidities: not reported |
Group 1 (IVR0.3, n=51 eyes): 0.3 mg (0.05 ml) IV ranibizumab, 3 monthly injections (dose up to 0.6 mg, see below)
Group 2 (IVR0.5, n=51 eyes): 0.5 mg IV (0.05 ml) ranibizumab, 3 monthly injections (dose up to 1.0 mg, see below) Group 3 (C, n=49 eyes): sham treatment, 3 monthly injections Regimen for all groups: after month 1, the injection dose could be doubled if CMT remained >300 µm or was >225 µm and reduction in retinal oedema from previous assessment was <50 µm; once injection volume was 0.1 ml it remained that for subsequent injections; if treatment had been withheld for >45 days, subsequent injections restarted at 0.05 ml; 68.6% of dose doubling with ranibizumab, 91.8% with sham; 34.7% of rescue laser photocoagulation in sham group, 4.9% in ranibizumab group |
At 12 months BCVA (ETDRS): |
||
| BCVA (letters) | p Value | ||||
| IVR0.3 | +11.8 SD6.6 | <0.0001 vs C | |||
| IVR0.5 | +8.8 SD11.0 | <0.0001 vs C | |||
| C | −1.4 SD14.2 | ||||
| Change ≥10 letters | |||||
| IVR0.3 | Gain 72.5% loss 0 |
<0.0001 vs C | |||
| IVR0.5 | Gain 49% loss 9.8% |
0.001 vs C | |||
| C | Gain 18.4% loss 24.5% |
||||
| CMT (OCT): | |||||
| CMT (µm) | p Value | ||||
| IVR0.3 | −200.7 SD122.2 | <0.0001 vs C | |||
| IVR0.5 | −187.6 SD147.8 | <0.0001 vs C | |||
| C | −48.4 SD153.4 | ||||
| RESTORE Study (Mitchell et al)24
49 Multicenter international Design: 3-arm RCT Follow-up: 12 months |
N: 345 eyes of 345 patients Inclusion criteria: ≥18 years, type 1 or 2 DM, HbA1c ≤10%, visual impairment due to DMO (eligible for laser treatment), stable medication for management of diabetes, BCVA ETDRS letter score 39–78 Exclusion criteria: concomitant eye conditions that could affect VA, active intraocular inflammation or infection, uncontrolled glaucoma in either eye, panretinal laser photocoagulation within 6 months or focal/grid laser photocoagulation within 3 months prior to study entry, history of stroke, hypertension Age: 62.9–64.0 SD8.15–9.29 years Sex: 37.1–47.7% female Diabetes type: 86.4–88.8% type 2 DM HbA1c: not reported Baseline VA: ETDRS letter score 62.4–64.8 SD9.99–11.11 Baseline CMT: 412.4–426.6 SD118.01–123.95 Comorbidities: not reported |
Group 1 (IVR, n=116 eyes): 0.5 mg IV ranibizumab plus sham laser (median injections 7 (range 1–12), median sham laser treatments 2 (range 1–5)) Group 2 (IVRL, n=118 eyes): 0.5 mg IV ranibizumab plus active laser (median injections 7 (range 2–12), median laser treatments 1 (range 1–5)) Group 3 (L, n=111 eyes): laser treatment plus sham injections (median sham injections 7 (range 1–12), median laser treatments 2 (range 1–4)) Regimen for all groups: 3 initial monthly injections, followed by retreatment schedule; 1 injection per month if stable VA not reached; Laser retreatments in accordance with ETDRS guidelines at intervals no shorter than 3 months from previous treatment |
At 12 months BCVA (ETDRS): |
||
| BCVA (letters) | p Value | ||||
| IVR | +6.1 SD6.43 | <0.0001 vs L | |||
| IVRL | +5.9 SD7.92 | <0.0001 vs L | |||
| L | +0.8 SD8.56 | ||||
| BCVA change categories | |||||
| IVR | Plus ≥10: 37.4% Loss ≥10: 3.5% |
<0.0001 vs L | |||
| IVRL | Plus ≥10: 43.2% Loss ≥10: 4.2% |
<0.0001 vs L | |||
| L | Plus ≥10: 15.5% Loss ≥10: 12.7% |
||||
| CMT (OCT): | |||||
| CMT (µm) | p Value | ||||
| IVR | −118.7 SD115.07 | 0.0002 vs L | |||
| IVRL | −128.3 SD114.34 | <0.0001 vs L | |||
| L | −61.3 SD132.29 | ||||
| REVEAL Study (Ohji and Ishibashi )48 Japan Multicenter Design: phase III double-masked RCT Follow-up: 12 months |
N: 396 patients Inclusion criteria: NR Exclusion criteria: NR Age: 61.1 years Sex: NR Diabetes type: 98.7% with type 2 diabetes HbA1c: 7.5% Baseline VA: 58.6 letters Baseline CMT: 421.9 µm Comorbidities: NR |
Group 1 (IVR 0.5 + sham laser, n=133): day 1, month 1, 2 and pro-renata thereafter based on BCVA Group 2 (IVR 0.5+ active laser, n=132): day 1, month 1, 2 and pro-renata thereafter based on BCVA Group 3 (sham injection + active laser, n=131): day 1, month 1, 2 and pro-renata thereafter based on BCVA Active/sham laser photocoagulation performed according to ETDRS guidelines at ≥3 month intervals |
At 12 months BCVA: |
||
| Mean average change from baseline to months 1–12 | p Value | ||||
| IVR+sham laser | +5.9 | vs laser <0.0001 | |||
| IVR+laser | +5.7 | vs laser <0.0001 | |||
| Laser+sham | +1.4 | ||||
| Mean change from baseline to month12 in BCVA and CRT | |||||
| IVR+sham laser | +6.6; −148.0 µm | vs C <0.0001 | |||
| IVR+laser | +6.4; −163.8 µm | vs C <0.0001 | |||
| Laser+sham | +1.8; −57.1 µm | ||||
| RISE Study (Brown et al/Nguyen et al)38
139 USA Multicenter Design: 3-arm double-blind sham-controlled RCT Follow-up: 24 months |
N: 377 eyes of 377 patients Inclusion criteria: ≥18 years, type 1 or 2 diabetes, BCVA 20/40–20/320, DMO CMT ≥275 µm Exclusion criteria: prior vitreoretinal surgery, recent history (within 3 months of screening) of panretinal or macular laser in the study eye, intraocular corticosteroids or antiangiogenic drugs, those with uncontrolled hypertension, uncontrolled diabetes (HbA1c >12%), recent (within 3 months) cerebrovascular accident or myocardial infarction Age: 61.7–62.8 SD8.9–10.0 (range 21–87) years Sex: 41.6–48% female Diabetes type: type 1 or 2 HbA1c: 7.7% SD 1.4–1.5; ≤8% (65–68.3%); >8% (31.7%–35%) Baseline VA: Mean ETDRS letter score 54.7–57.2; ≤20/200 (7.9–13.6%); >20/200 but <20/40 (72.4–72.8%); ≥20/40 (13.6–19.7%) Baseline CMT: 463.8–474.5 µm Comorbidities: History of smoking 46.4–51.2% |
Group 1 (IVR0.3, n=125 eyes): 0.3 mg IV ranibizumab Group 2 (IVR0.5, n=125 eyes): 0.5 mg IV ranibizumab Group 3 (C, n=127 eyes): sham injection Regimen for all groups: monthly injections; need for macular rescue laser assessed monthly starting at month 3 |
At 24 months BCVA: |
||
| Plus ≥15 letters | p Value | ||||
| IVR0.3 | 44.8% | <0.0001 vs C | |||
| IVR0.5 | 39.2% | =0.0002 vs C | |||
| C | 18.1% | ||||
| Loss of <15 letters | |||||
| IVR0.3 | 97.6% | =0.0086 vs C | |||
| IVR0.5 | 97.6% | =0.0126 vs C | |||
| C | 89.8% | ||||
| Snellen equivalent of 20/40 or better | |||||
| IVR0.3 | 60% | <0.0001 vs C | |||
| IVR0.5 | 63.2% | <0.0001 vs C | |||
| C | 37.8% | ||||
| Mean BCVA gain (letters) | |||||
| IVR0.3 | +12.5 SD14.1 | <0.0001 vs C | |||
| IVR0.5 | +11.9 SD12.1 | <0.0001 vs C | |||
| C | +2.6 SD13.9 | ||||
| CFT: | |||||
| Mean change from baseline | p Value | ||||
| IVR0.3 | −250.6 SD212.2 | <0.0001 vs C | |||
| IVR0.5 | −253.1 SD183.7 | <0.0001 vs C | |||
| C | −133.4 SD209.0 | ||||
| RIDE study (Boyer et al/Nguyen et al)38
140 USA Multicentre Design: 3-arm double-blind sham-controlled RCT Follow-up: 24 months |
N: 382 eyes Inclusion criteria: ≥18 years, type 1 or 2 diabetes, BCVA 20/40–20/320 and DMO CMT ≥275 µm Exclusion criteria: prior vitreoretinal surgery, recent history (within 3 months of screening) of panretinal or macular laser in the study eye, intraocular corticosteroids or antiangiogenic drugs, those with uncontrolled hypertension, uncontrolled diabetes (HbA1c >12%), recent (within 3 months) cerebrovascular accident or myocardial infarction Age: 61.8–63.5 (range 22–91) years Sex: 37–49.1% female Diabetes type: type 1 or 2 HbA1c: 7.6 SD1.3–1.5; ≤8% (65.8–67.5%); >8% (32.5–34.2%) Baseline VA: Mean ETDRS letter score 56.9–57.5 Baseline CMT: 447.4–482.6 µm Comorbidities: history of smoking 33.6–51.6% |
Group 1 (IVR0.3, n=125 eyes): 0.3 mg IV ranibizumab Group 2 (IVR0.5, n=127 eyes): 0.5 mg IV ranibizumab Group 3 (C, n=130 eyes): sham injection Regimen for all groups: Patients were eligible for rescue macular laser starting at month 3 |
At 24 months BCVA: |
||
| More than 15 letters | p Value | ||||
| IVR0.3 | 33.6% | <0.0001 vs C | |||
| IVR0.5 | 45.7% | <0.0001 vs C | |||
| C | 12.3% | ||||
| Less than 15 letters | |||||
| IVR0.3 | 1.6% | >0.05 vs C | |||
| IVR0.5 | 3.9% | <0.05 vs C | |||
| C | 8.5% | ||||
| Snellen equivalent of 20/40 or better | |||||
| IVR0.3 | 54.4% | =0.0002 vs C | |||
| IVR0.5 | 62.2% | <0.0001 vs C | |||
| C | 34.6% | ||||
| Mean BCVA gain (letters) | |||||
| IVR0.3 | +10.9 SD10.4 | <0.0001vs C | |||
| IVR0.5 | +12.0 SD14.9 | <0.0001 vs C | |||
| C | +2.3 SD14.2 | ||||
| CMT: | |||||
| Mean change from baseline | p Value | ||||
| IVR0.3 | −259.8 SD169.3 | <0.0001 vs C | |||
| IVR0.5 | −270.7 SD201.6 | <0.0001 vs C | |||
| C | −125.8 SD198.3 | ||||
Injections are intravitreal unless otherwise noted.
BCVA, best corrected visual acuity; C, control; CMT, central macular thickness; CSME, clinically significant macular oedema; DDS, dexamethasone; DIL, dexamethasone followed by laser; DM, diabetes mellitus; DMO, diabetic macular oedema; DP, diastolic pressure; DR, diabetic retinopathy; HR QoL, health-related quality of life; IOP, intraocular pressure; IV, intravitreal; IVB, intravitreal bevacizumab; IVP, intravitreal pegaptanib; IVR, intravitreal ranibizumab; IVT, intravitreal triamcinolone; IVTL, intravitreal triamcinolone plus laser; IVVTE, intravitreal VEGF Trap Eye; L, laser; MLT/MPC, macular laser therapy/macular photocoagulation; NEI VFQ-25, National Eye Institute Visual Function Questionnaire-25; NPDR, non-proliferative diabetic retinopathy; NR, not reported; OCT, optical coherence tomography; PDR, proliferative diabetic retinopathy; PRP, panretinal photocoagulation; RCT, randomised controlled trial; SOC, standard of care; SP, systolic pressure; SRFA, fluocinolone; VA, visual acuity; VEGF, vascular endothelia growth factor.
Table 4.
Bevacizumab studies
| Study | Participants and baseline values | Intervention | Outcome (change from baseline at study end) | ||
|---|---|---|---|---|---|
| BOLT Study (Michaelides et al/Rajendram et al))23
52
85 UK Design: 2-arm RCT Follow-up: 12 months |
N: 80 eyes of 80 patients Inclusion criteria: ≥18 years, type 1 or 2 DM, BCVA in the study eye 35–69 ETDRS letters at 4 m (≥6/60 or ≤6/12), center-involving clinically significant DMO with CMT ≥270 µm; media clarity, papillary dilation and cooperation sufficient for adequate fundus imaging; a least 1 prior macular laser therapy; IOP <30 mm Hg; fellow eye BCVA ≥3/60; fellow eye received no anti-VEGF in past 3 months and no expectation of such therapy Exclusion criteria: (ocular for study eye) macular ischemia, macular oedema due to causes other than DMO, coexistent ocular disease affecting VA or DMO, any treatment for DMO in prior 3 months, PRP within 3 months prior to randomisation or anticipated, PDR, HbA1c >11%, medical history of chronic renal failure; any thromboembolic event within 6 months prior to randomisation, unstable angina, evidence of active ischemia on ECG; major surgery within 28 days of randomisation or planned; participation in an investigational drug trial; systemic anti-VEGF or pro-VEGF treatment within 3 months of enrolment; pregnancy, lactation; intraocular surgery within 3 months of randomisation; aphakia; uncontrolled glaucoma; significant external ocular disease Age: 64.2 SD8.8 years Sex: 31% female Diabetes type: 90% type 2 DM, 10% type 1 DM HbA1c: 7.5–7.6 SD1.2–1.4% Baseline VA: ETDRS letter score 54.6–55.7 SD8.6–9.7 Baseline CMT: 481–507 SD121–145 µm Comorbidities: 19% mild NPDR (level 35), 46% moderate NPDR (level 43), 19% moderately severe NPDR (level 47), 13% severe NPDR (level 53), 3% moderate PDR (level 65), 79–88% phakic |
Group 1 (MLT, n=38 eyes): modified ETDRS macular laser therapy; reviewed every 4 months up to 52 weeks; retreatment performed if clinically indicated by ETDRS guidelines (median 4 laser treatments) Group 2 (IVB, n=42 eyes): 1.25 mg (0.05 ml) IV bevacizumab at baseline, 6 and 12 weeks; subsequent IVB injections (up to 52 weeks) guided by an OCT-based retreatment protocol (median 13 injections) Laser modified ETDRS protocol, retreatment by ETDRS guidelines |
At 24 months BCVA (ETDRS): |
||
| BCVA.mean (SD) | p Value | ||||
| MLT | −0.5 (10.6) | ||||
| IVB | +8.6 (9.1) | 0.005 vs MLT | |||
| BCVA gain categories (letters) | |||||
| MLT | gaining ≥10: 7% losing >15: 4% |
||||
| IVB | gaining ≥10: 49% losing >15: 32% |
0.001 vs MLT 0.004 vs MLT |
|||
| CMT (µm, quartiles) | p Value | ||||
| MLT | −118 SD171 | ||||
| IVB | −146 SD122 | 0.62 vs MLT | |||
| Lam et al35 Hong Kong Design: 2-arm RCT Follow-up: 6 months |
N: 52 eyes of 52 patients Inclusion criteria: ≥18 years, type 1 or 2 DM, clinically significant DMO (slit-lamp biomicroscopy, ETDRS criteria; leakage confirmed by fluorescein angiography, CMT ≥250 µm on OCT), BCVA ≥1.3 ETDRS logMAR units; only patients with diffuse DMO recruited Exclusion criteria: macular oedema due to reasons other than diabetes, significant media opacities, macular ischemia of ≥1 disk area, vitreomacular traction, PDR, aphakia, glaucoma or ocular hypertension, previous anti-VEGF treatment, intraocular surgery except uncomplicated cataract extraction (but > 6 months prior), focal DMO, any laser procedure within previous 4 months, subtenon or intravitreal triamcinolone injection within 6 months, pregnancy Age: 65.3 SD8.9 years Sex: 46.2% female Diabetes type: not reported HbA1c: 7.5 SD1% Baseline VA: 0.61 SD0.29 logMAR Baseline CMT: 466 SD127 µm Comorbidities: not reported |
Group 1 (IVB1.25, n=26 eyes): 1.25 mg bevacizumab (0.05 ml) Group 2 (IVB2.5, n=26 eyes): 2.5 mg bevacizumab (0.1 ml) Regimen for all groups: 3 monthly IV injections, topical 0.5% levofloxacin 4×/day for up to 2 weeks after each injection |
At 6 months BCVA (ETDRS chart): |
||
| BCVA (logMAR) | p Value | ||||
| IVB1.25 | 0.11 SD0.31 (+5.5 letters) | 0.018 vs baseline, NS vs IVB2.5 | |||
| IVB2.5 | 0.13 SD0.26 (+6.5 letters) | 0.003 vs baseline | |||
| CMT (OCT) | CMT (µm) | p Value | |||
| IVB1.25 | 96 | 0.002 vs baseline, NS vs IVB2.5 | |||
| IVB2.5 | 74 | 0.013 vs baseline | |||
| Subgroups: ▸ For patients with previous DMO treatment (mainly laser): no significant reduction in CMT at 6 months (452 µm at baseline to 416 µm at 6 months, p=0.22); no significant improvement in BCVA (0.66 logMAR at baseline to 0.56 logMAR at 6 months (+5 letters), p=0.074) |
|||||
| Faghihi et al53 Iran Design: 2-arm RCT Follow-up: 6 months |
N: 80 eyes of 40 patients Inclusion criteria: Bilateral non-tractional CSME, 10/10> V.A≥1/10, Controlled blood pressure. Exclusion criteria: Advanced or advanced active PDR, significant cataract, glaucoma, history of recent vascular accident (eg, MI, CVA), Previous treatment of CSME or PDR, or pharmacotherapy for CSME, macular ischemia and uncontrolled hypertension Age: 57.7±8 years Sex: 27.5% females Diabetes type: NR HbA1c: 8.42±1.82 g/dl Baseline VA: 0.326–0.409 (SD 0.279–0.332) Baseline CMT: 277 um–287 um (SD 78–98) Comorbidities: not reported |
Group 1 (IVB, n=40 eyes): 1.25 mg bevacizumab Group 2 (IVB+MPC, n=40 eyes): 1.25 mg bevacizumab Regimen for all groups: Eyes examined every 2 months and if evidence of CSME IVB was injected. Mean of the number of IVB injections in IVB group and IVB+MPC group were 2.23±1.24 and 2.49±1.09, respectively |
At 6 months Mean change in BCVA (ETDRS chart): |
||
| BCVA (logMAR) | p Value | ||||
| IVB | 0.138 | <0.05 vs baseline | |||
| IVB+MPC | 0.179 | <0.05 vs baseline | |||
| ▸ no statistically significant difference between the two groups CMT (OCT): |
|||||
| CMT (µm) | p Value | ||||
| IVB | −39 | <0.05 vs baseline | |||
| IVB+MPC | −39 | <0.05 vs baseline | |||
| ▸ No statistically significant difference between the two groups | |||||
BCVA, best corrected visual acuity; C, control; CMT, central macular thickness; CSME, clinically significant macular oedema; DDS, dexamethasone; DIL, dexamethasone followed by laser; DM, diabetes mellitus; DMO, diabetic macular oedema; DP, diastolic pressure; DR, diabetic retinopathy; HR QoL, health-related quality of life; IOP, intraocular pressure; IV, intravitreal; IVB, intravitreal bevacizumab; IVP, intravitreal pegaptanib; IVR, intravitreal ranibizumab; IVT, intravitreal triamcinolone; IVTL, intravitreal triamcinolone plus laser; IVVTE, intravitreal VEGF Trap Eye; L, laser; MLT/MPC, macular laser therapy/macular photocoagulation; NEI VFQ-25, National Eye Institute Visual Function Questionnaire-25; NPDR, non-proliferative diabetic retinopathy; NR, not reported; OCT, optical coherence tomography; PDR, proliferative diabetic retinopathy; PRP, panretinal photocoagulation; RCT, randomised controlled trial; SOC, standard of care; SP, systolic pressure; SRFA, fluocinolone; VA, visual acuity; VEGF, vascular endothelia growth factor.
Table 5.
Pegaptanib and aflibercept studies
| Study | Participants and baseline values | Intervention | Outcome (change from baseline at study end) | ||
|---|---|---|---|---|---|
| Pegaptanib | |||||
| Cunningham et al/Adamis et al39
57 USA Design: 4-arm phase II RCT Follow-up: 36 weeks |
N: 172 eyes of 172 patients Inclusion criteria: ≥18 years, type 1 or 2 DM, DMO involving the center of the macula with corresponding leakage from microaneurysms, retinal telangiectasis, or both; clear ocular media, BCVA letter scores between 68 and 25 in the study eye and at least 35 in the fellow eye; IOP ≤23 mm Hg, focal photocoagulation could be safely deferred for 16 weeks; no ECG abnormalities, no major serological abnormalities Exclusion criteria: history of panretinal or focal photocoagulation; neodymium:yttrium–aluminum–garnet laser or peripheral retinal cryoablation in previous 6 months; any ocular abnormality interfering with VA assessment or fundus photography; vitreoretinal traction; vitreous incarceration; retinal vein occlusion involving the macula; atrophy/scarring/fibrosis or hard exudates involving the center of the macula; history of intraocular surgery within previous 12 months, myopia of ≥8 diopters, axial length of ≥25 mm, likelihood of requiring panretinal photocoagulation within following 9 months; cataract surgery within 12 months; active ocular or periocular infection; previous therapeutic radiation to the eye, head, or neck; known serious allergies to fluorescein dye; HbA1c ≥13%, pregnancy Age: 61.3–64.0 SD9.3–10.1 years Sex: 45–55% female Diabetes type: 5–10% IDDM HbA1c: 7.1–7.7 SD1.2–1.6 Baseline VA: letter score 55.0–57.1 SD9.1–11.5 Baseline CMT: 423.2–476.0 µm Comorbidities: not reported |
Group 1 (IVP0.3, n=44 eyes): 0.3 mg IV pegaptanib (90 µl) (median 5 injections (range 1–6)) Group 2 (IVP1, n=44 eyes): 1 mg IV pegaptanib (90 µl) (median 6 injections (range 3–6)) Group 3 (IVP3, n=42 eyes): 3 mg IV pegaptanib (90 µl) (median 6 injections (range 1–6)) Group 4 (C, n=42 eyes): sham injection (median 5 injections (range 1–6)) Regimen for all groups: injections at baseline, week 6 and week 12; thereafter, additional injections administered every 6 weeks at the discretion of the investigators if judged indicated (maximum of 6 injections up to week 30); laser photocoagulation allowed after week 13 if judged indicated by the study-masked ophthalmologist (25% for IVP0.3, 30% for IVP1, 40% for IVP3, 48% for C) |
At 36 weeks BCVA: |
||
| BCVA (letters) | p Value | ||||
| IVP0.3 | +4.7 | 0.04 vs C | |||
| IVP1 | +4.7 | 0.05 vs C | |||
| IVP3 | +1.1 | NS vs C | |||
| C | −0.4 | ||||
| Plus ≥10 letters | |||||
| IVP0.3 | 34% | 0.003 vs C | |||
| IVP1 | 30% | ||||
| IVP3 | 14% | ||||
| C | 10% | ||||
| CMT (OCT): | |||||
| CMT (µm, 95% CI) | p Value | ||||
| IVP0.3 | −68.0 (−118.9 to −9.88) | 0.02 vs C | |||
| IVP1 | −22.7 (−76.9 to +33.8) | NS vs C | |||
| IVP3 | −5.3 (−63.0 to +49.5) | NS vs C | |||
| C | +3.7 | ||||
| ▸ Subgroups: of 16 participants with retinal neovascularisation at baseline, 8 of 13 (62%) in the pegaptanib groups and 0 of 3 in the sham group had regression of neovascularisation at 36 weeks | |||||
| Sultan et al40 Multicenter international Design: 2-arm placebo-controlled RCT Follow-up: 2 years (primary efficacy endpoint at 1 year) |
N: 260 eyes of 260 patients Inclusion criteria: ≥18 years, type 1 or 2 DM, DMO involving the center of the macula not associated with ischemia, CMT ≥250 µm, BCVA letter score 65–35, IOP ≤21 mm Hg, clear ocular media Exclusion criteria: any abnormality other than DMO affecting VA assessment, vitreomacular traction; yttrium–aluminium–garnet laser, peripheral retinal cryoablation, laser retinopexy for retinal tears, focal or grid photocoagulation within prior 16 weeks; panretinal photocoagulation <6 months before baseline or likely to be needed within 9 months; significant media opacities; intraocular surgery in prior 6 months; pathological high myopia; prior radiation in region of study eye; history of severe cardiac or peripheral vascular disease, stroke in prior 12 months, major surgery in prior 1 month, treatment in prior 90 days with any investigational agent or with bevacizumab for any nonocular condition, HbA1c ≥10% or signs of uncontrolled diabetes, hypertension, known relevant allergies; pregnant or lactating Age: 62.3–62.5 SD9.3–10.2 years Sex: 39–46% female Diabetes type: 6.3–7.5% type 1 DM, 92.5–93.7% type 2 DM HbA1c: 42.5–45.9% <7.6%, 54.1–57.5% >7.6% Baseline VA: letter score 57.0–57.5 SD8.1–8.9 Baseline CMT: 441.6–464.6 SD135.5–148.5 µm Comorbidities: not reported |
Group 1 (IVP, n=133 eyes): 0.3 mg IV pegaptanib sodium (mean number of injections 12.7 SD4.6) Group 2 (C, n=127 eyes): sham injection (mean number of injections 12.9 SD4.4) Regimen for all groups: injections every 6 weeks up to week 48 (9 injections); at investigator determination (ETDRS criteria), laser photocoagulation could be performed at week 18, with possible repeat treatment at a minimum of 17 weeks later (maximum 3 treatments per year) (laser treatments in 25.2% of IVP group and 45% of C group); in year 2, injections as judged necessary |
At 1 year BCVA (ETDRS): |
||
| BCVA (letters) | p Value | ||||
| IVP | +5.2 | <0.05 vs C | |||
| C | +1.2 | ||||
| Plus ≥10 letters | |||||
| IVP | 36.8% | 0.0047 vs C | |||
| C | 19.7% | ||||
| Retinopathy: | |||||
| Increase in degree by ≥2 steps | |||||
| IVP | 4.1% | 0.047 vs C | |||
| C | 12.4% | ||||
| Decrease in degree by ≥2 steps | |||||
| IVP | 10.2% | NS vs C | |||
| C | 3.1% | ||||
| CMT (OCT): | Decrease in CMT | ||||
| IVP | ≥25%: 31.7% ≥50%: 14.6% |
NS vs C | |||
| C | ≥25%: 23.7% ≥50%: 11.9% |
||||
| At 2 years | |||||
| BCVA (ETDRS): | |||||
| BCVA (letters) | p Value | ||||
| IVP | +6.1 | <0.01 vs C | |||
| C | +1.3 | ||||
| Plus ≥10 letters | |||||
| IVP | 38.3% | NS vs C | |||
| C | 30% | ||||
| Retinopathy: | |||||
| Increase in degree by ≥2 steps | |||||
| IVP | 6.3% | NS vs C | |||
| C | 13.8% | ||||
| Decrease in degree by ≥2 steps | |||||
| IVP | 16.3% | 0.03 vs C | |||
| C | 3.8% | ||||
| CMT (OCT): | |||||
| Decrease in CMT | |||||
| IVP | ≥25%: 40.4% ≥50%: 19.2% |
NS vs C | |||
| C | ≥25%: 44.6% ≥50%: 26.1% |
||||
| QoL: ▸ NEI VFQ-25: between group differences not significant at 54 weeks; at 102 weeks, significantly greater improvement in composite score and subscales distance vision activities, social functioning and mental health with pegaptanib ▸ EQ-5D: no significant differences between groups in EQ-5D scores at weeks 54 or 102 |
|||||
| Aflibercept | |||||
| DA VINCI 2010 (Do et al)30
58 Multicenter Design: 5-arm phase II RCT Follow-up: 24 weeks |
N: 221 eyes of 221 patients Inclusion criteria: aged >18 years and diagnosed with type 1 or 2 diabetes mellitus, with DMO involving the central macula defined as CRT (>250 um in the central subfield. Participants were required to have BCVA letter score at 4 m of 73–24. Women of childbearing potential were included only if they were willing to not become pregnant and to use a reliable form of birth control during the study period Exclusion criteria: history of vitreoretinal surgery; panretinal or macular laser photocoagulation or use of intraocular or periocular corticosteroids or antiangiogenic drugs within 3 months of screening; vision decrease due to causes other than DMO; proliferative diabetic retinopathy (unless regressed and currently inactive); ocular inflammation; cataract or other intraocular surgery within 3 months of screening, laser capsulotomy within 2 months of screening; aphakia; spherical equivalent of >8 diopters; or any concurrent disease that would compromise visual acuity or require medical or surgical intervention during the study period: active iris neovascularisation, vitreous hemorrhage, traction retinal detachment, or preretinal fibrosis involving the macula; visually significant vitreomacular traction or epiretinal membrane evident biomicroscopically or on OCT; history of idiopathicor autoimmune uveitis; structural damage to the center of the macula that is likely to preclude improvement in visual acuity after the resolution of macular oedema; uncontrolled glaucoma or previous filtration surgery; infectious blepharitis, keratitis, scleritis, or conjunctivitis; or current treatment for serious systemic infection: uncontrolled diabetes mellitus; uncontrolled hypertension; history of cerebral vascular accident or myocardial infarction within 6 months; renal failure requiring dialysis or renal transplant; pregnancy or lactation; history of allergy to fluorescein or povidone iodine; only 1 functional eye (even if the eye met all other entry criteria); or an ocular condition in the fellow eye with a poorer prognosis than the study eye Age: 60.7–64.0 years (SD 8.1–11.5) Sex: % female 35.6–47.6% Diabetes type: percentage of type 2, 88.6–97.7% HbA1c: 7.85–8.10 (SD 1.71–1.94) Baseline VA: 57.6–59.9 (SD 10.1–12.5) Baseline CMT: 426.1–456.6 µm (SD 111.8–152.4) Comorbidities: history of any cardiac disease was twice as common in the VEGF Trap-Eye groups compared with the laser group |
Trial of VEGF Trap-Eye (VTE), randomised on a 1 : 1:1 : 1:1 basis Group 1 (IVVTE1, n=44 eyes): IVVTE, 0.5 mg every 4 weeks Group 2 (IVVTE2, n=44 eyes): IVVTE, 2 mg every 4 weeks Group 3 (IVVTE3, n=42 eyes): IVVTE, 2 mg for 3 initial months then every 8 weeks Group 4 (IVVTE4, n=45 eyes): IVVTE, 2 mg for 3 initial months then as needed Group 5 (L, n=44 eyes): laser photocoagulation Laser modified ETDRS protocol |
At 6 months | ||
| BCVA (letters) | p Value | ||||
| IVVTE1 | +8.6 | 0.005 vs L | |||
| IVVTE2 | +11.4 | <0.0001 vs L | |||
| IVVTE3 | +8.5 | 0.008 vs L | |||
| IVVTE3 | +10.3 | 0.0004 vs L | |||
| L | +2.5 | ||||
| plus ≥10 letters | |||||
| IVVTE1 | 50% | NR | |||
| IVVTE2 | 64% | NR | |||
| IVVTE3 | 43% | NR | |||
| IVVTE3 | 58% | NR | |||
| L | 32% | NR | |||
| CMT(um) | |||||
| IVVTE1 | −144.6 | 0.0002 vs L | |||
| IVVTE2 | −194.5 | <0.0001 vs L | |||
| IVVTE3 | −127.3 | 0.007 vs L | |||
| IVVTE3 | −153.3 | <0.0001 vs L | |||
| L | −67.9 | ||||
| At 12 months | |||||
| BCVA (letters) | p Value | ||||
| IVVTE1 | +11.0 | ≤0.0001 vs L | |||
| IVVTE2 | +13.1 | ≤0.0001 vs L | |||
| IVVTE3 | +9.7 | ≤0.0001 vs L | |||
| IVVTE3 | +12.0 | ≤0.0001 vs L | |||
| L | −1.3 | ||||
| Plus ≥15 letters | |||||
| IVVTE1 | 40.9% | 0.0031 vs L | |||
| IVVTE2 | 45.5% | 0.0007 vs L | |||
| IVVTE3 | 23.8% | 0.1608 vs L | |||
| IVVTE3 | 42.2% | 0.0016 vs L | |||
| L | 11.4% | ||||
| Plus ≥10 letters | |||||
| IVVTE1 | 57% | 0.0031 vs L | |||
| IVVTE2 | 71% | 0.0007 vs L | |||
| IVVTE3 | 45% | 0.1608 vs L | |||
| IVVTE3 | 62% | 0.0016 vs L | |||
| L | |||||
| CMT(µm) | |||||
| IVVTE1 | −165.4 | <0.0001 vs L | |||
| IVVTE2 | −227.4 | <0.0001 vs L | |||
| IVVTE3 | −187.8 | <0.0001 vs L | |||
| IVVTE3 | −180.3 | <0.0001 vs L | |||
| L | −58.4 | ||||
BCVA, best corrected visual acuity; C, control; CMT, central macular thickness; CSME, clinically significant macular oedema; DDS, dexamethasone; DIL, dexamethasone followed by laser; DM, diabetes mellitus; DMO, diabetic macular oedema; DP, diastolic pressure; DR, diabetic retinopathy; HR QoL, health-related quality of life; IOP, intraocular pressure; IV, intravitreal; IVB, intravitreal bevacizumab; IVP, intravitreal pegaptanib; IVR, intravitreal ranibizumab; IVT, intravitreal triamcinolone; IVTL, intravitreal triamcinolone plus laser; IVVTE, intravitreal VEGF Trap Eye; L, laser; MLT/MPC, macular laser therapy/macular photocoagulation; NEI VFQ-25, National Eye Institute Visual Function Questionnaire-25; NPDR, non-proliferative diabetic retinopathy; NR, not reported; OCT, optical coherence tomography; PDR, proliferative diabetic retinopathy; PRP, panretinal photocoagulation; RCT, randomised controlled trial; SOC, standard of care; SP, systolic pressure; SRFA, fluocinolone; VA, visual acuity; VEGF, vascular endothelia growth factor.
Table 6.
Dexamethasone and fluocinolone studies
| Study | Participants and baseline values | Intervention | Outcome (change from baseline at study end) | ||
|---|---|---|---|---|---|
| Dexamethasone | |||||
| Callanan et alUSA44 Design: 2-arm RCT Follow-up: 12 months |
N: 253 eyes of 253 patients Inclusion criteria: diffuse DMO, CMT ≥275 µm, BCVA ≥34 and ≤70 letters Exclusion criteria: not reported Age: not reported Sex: not reported Diabetes type: not reported HbA1c: not reported Baseline VA: not reported Baseline CMT: not reported Comorbidities: not reported |
Group 1 (DIL, n=126 eyes): dexamethasone IV implant followed by laser photocoagulation after 1 month (mean 1.6 implants; 78.6% completion) Group 2 (L, n=127 eyes): laser alone (79.5% completion) Regimen for all groups: if needed, patients were retreated with the dexamethasone implant at months 6 or 9, and with laser at months 4, 7 and 10; mean 2.2 laser treatments per patient Laser protocol not reported |
At 12 months BCVA: |
||
| Plus ≥10 letters (%) | p Value | ||||
| DIL | 28 | NS vs L | |||
| L | 24 | ||||
| ▸ Patients in DIL group had significantly greater increases in BCVA from baseline than patients in the laser group (p<0.05) at months 1–9 only CMT (OCT): ▸ Patients in DIL group had significantly greater mean reductions from baseline in CMT at months 1 and 6 only (p<0.001) |
|||||
| Haller et al59 USA Multicenter Design: 3-arm RCT Follow-up: 6 months (180 days), primary outcome 3 months (90 days) |
N: 171 eyes of 171 patients Inclusion criteria: ≥12 years, DMO persisting for ≥90 days after laser treatment or medical therapy, BCVA by ETDRS between 20/40 (67 letters) and 20/200 (35 letters) due to clinically detectable DMO; analysis includes only eyes with DMO associated with DR Exclusion criteria: history of vitrectomy in the study eye; use of systemic, periocular, or intraocular steroids within 30 days of enrolment; moderate or severe glaucoma in the study eye; poorly controlled hypertension (SP >160 mm Hg or DP >90 mm Hg); poorly controlled diabetes (HbA1c >13%) Age: 62.9–63.8 years SD10.2–12.0 Sex: 45.6–49.1% female Diabetes type: not reported HbA1c: 7.3–7.6% Baseline VA: letter score 54.4–54.7 SD9.96–11.88 Baseline CMT: 417.5–446.5 µm SD123.7–155.9 Comorbidities: 19–21% prior cataract extraction |
Group 1 (DDS350, n=57 eyes): 350 µg dexamethasone IV drug delivery system, implanted into the vitreous cavity Group 2 (DDS700, n=57 eyes): 700 µg dexamethasone IV drug delivery system, implanted into the vitreous cavity Group 3 (C, n=57 eyes): no treatment Regimen for all groups: eyes demonstrating a VA loss of ≥5 letters could be treated with any other therapy (including laser photocoagulation and IV triamcinolone) (n=4 with photocoagulation or IV triamcinolone in the C group, n=2 in the DDS350 group, none in the DDS700 group) |
At 90 days BCVA (ETDRS): |
||
| Plus ≥10 letters | p Value | ||||
| DDS350 | 21% (graph) | NS vs C | |||
| DDS700 | 33% | 0.007 vs C | |||
| C | 12% | ||||
| CMT (OCT): | |||||
| CMT (µm) | p Value | ||||
| DDS350 | −42.57 SD95.96 | NS (p=0.07) vs C | |||
| DDS700 | −132.27 SD160.86 | <0.001 vs C | |||
| C | +30.21 SD82.12 | ||||
|
At 180 days BCVA (ETDRS): |
|||||
| Plus ≥10 letters | p Value | ||||
| DDS350 | 20% (graph) | NS vs C | |||
| DDS700 | 33% (graph) | NS vs C | |||
| C | 23% (graph) | ||||
| Fluocinolone | |||||
| FAME Study (Campochiaro et al/Campochiaro et al)29
60 Multicenter international Design: 3-arm placebo-controlled RCT Follow-up: 24 months; abstract with 36 month outcomes |
N: 956 eyes of 956 patients Inclusion criteria: DMO, CMT ≥250 µm despite at least 1 prior focal/grid macular laser photocoagulation treatment, BCVA ETDRS letter score between 19 and 68 (20/50–20/400) Exclusion criteria: glaucoma, ocular hypertension, IOP >21 mm Hg, taking IOP lowering drops; laser treatment for DMO within 12 weeks of screening, any ocular surgery in the study eye within 12 weeks of screening; ocular or systemic steroid therapy; active ocular infection; pregnancy Age: 62.5 SD9.4 years Sex: 40.6% Diabetes type: 6.6% type 1 DM, 92% type 2 DM, 1.4% uncertain HbA1c: 7.8 SD1.59% Baseline VA: ETDRS letter score 53.4 SD12.23 Baseline CMT: 469.0 SD164.78 µm Comorbidities: 47.1% cataract at baseline, 62.7–67.4% phakic |
Group 1 (0.5, n=375 eyes): intravitreal insert releasing 0.2 µg/day fluocinolone acetonide (FA) (2, 3, or 4 treatments received by 21.3, 1.9 and 0.3%) Group 2 (SRFA0.5, n=393 eyes): intravitreal insert releasing 0.5 µg/day fluocinolone acetonide (2, 3, or 4 treatments received by 22.6, 2.5 and 0.3%) Group 3 (C, n=185 eyes): sham injection (2, 3, or 4 treatments received by 19.5, 2.7 and 1.6%) Regimen for all groups: patients could receive rescue focal/grid laser therapy any time after the first 6 weeks for persistent oedema (35.2–36.7% in FA groups, 58.9% control group, p<0.001); treatments were allowed every 3 months for persistent or recurrent oedema; patients eligible for another FA insert at 1 year if ≥5 letter reduction in BCVA or >50 µm CMT increase from best status |
At 24 months BCVA (ETDRS): |
||
| BCVA (letters) | p Value | ||||
| SRFA0.2 | +4.4 | 0.02 vs C | |||
| SRFA0.5 | +5.4 | 0.017 vs C | |||
| C | +1.7 | ||||
| Plus ≥15 letters (%) | p Value | ||||
| SRFA0.2 | 29 | 0.002 SRFA vs C | |||
| SRFA0.5 | 29 | ||||
| C | 16 | ||||
| Subgroups: ▸ BCVA benefits only in pseudophakic eyes (cataract surgery before or during the study), in phakic eyes, BCVA letter score was reduced by 5 (high dose) and 9 (low dose) from baseline at 24 months CMT (optical coherence tomography): |
|||||
| CMT (µm) | p Value | ||||
| SRFA0.2 | −167.8 | 0.005 vs C | |||
| SRFA0.5 | −177.1 | <0.001 vs C | |||
| C | −111.3 | ||||
| ▸ effect maintained at 36 months At 36 months |
|||||
| Plus ≥15 letters | p Value | ||||
| SRFA0.2/0.5 | 28.7% | 0.018 SRFA vs C | |||
| C | 18.9% | ||||
| Pearson et al43 USA Multicenter Design: 2-arm RCT Follow-up: 36 months |
N: 196 patients Inclusion criteria: persistent or recurrent unilateral or bilateral DMO with retinal thickening involving fixation of ≥1 disc area in size, ETDRS visual acuity of ≥20 letters (20/400) to ≤68 letters (20/50) and ≥1 macular laser treatment in the study eye more than 12 weeks prior to enrolment Exclusion criteria: Ocular surgery within 3 months prior to enrolment, uncontrolled IOP within the past 12 months while on ≥1 antiglaucoma medication, IOP of ≥22 mm Hg at screening while on ≥1 antiglaucoma medication, peripheral retinal detachment in the area of implantation or media opacity precluding diagnosis of status in the study eye Age: 61.4–62.7 years Sex: 41.7–42% female Diabetes type: 62.3–70% on insulin HbA1c: not reported Baseline VA: not reported Baseline CMT: not reported Comorbidities: not reported |
Group 1 (SRFA, n=127): 0.5 mg sustained release fluocinolone acetonide intravitreal implant Group 2 (SOC, n=69): standard of care—either repeat laser or observation Laser ETDRS protocol |
At 3 years BCVA: |
||
| Gain ≥15 letters | p Value | ||||
| SRFA | 31% | NS | |||
| SOC | 20% | ||||
| Loss ≥15 letters | |||||
| SRFA | 17% | NS | |||
| SOC | 14% | ||||
| CMT: | |||||
| Mean change in baseline CMT | p Value | ||||
| SRFA | −86 | NS | |||
| SOC | −110 | ||||
BCVA, best corrected visual acuity; C, control; CMT, central macular thickness; CSME, clinically significant macular oedema; DDS, dexamethasone; DIL, dexamethasone followed by laser; DM, diabetes mellitus; DMO, diabetic macular oedema; DP, diastolic pressure; DR, diabetic retinopathy; HR QoL, health-related quality of life; IOP, intraocular pressure; IV, intravitreal; IVB, intravitreal bevacizumab; IVP, intravitreal pegaptanib; IVR, intravitreal ranibizumab; IVT, intravitreal triamcinolone; IVTL, intravitreal triamcinolone plus laser; IVVTE, intravitreal VEGF Trap Eye; L, laser; MLT/MPC, macular laser therapy/macular photocoagulation; NEI VFQ-25, National Eye Institute Visual Function Questionnaire-25; NPDR, non-proliferative diabetic retinopathy; NR, not reported; OCT, optical coherence tomography; PDR, proliferative diabetic retinopathy; PRP, panretinal photocoagulation; RCT, randomised controlled trial; SOC, standard of care; SP, systolic pressure; SRFA, fluocinolone; VA, visual acuity; VEGF, vascular endothelia growth factor.
Table 7.
Triamcinolone studies
| Study | Participants and baseline values | Intervention | Outcome (change from baseline at study end) | |||
|---|---|---|---|---|---|---|
| DRCR Network 2008 (Ip et al/Beck et al/Bressler et al)22
61
63
64 USA Multicenter Design: 3-arm RCT Follow-up: 2 years, additional 3 year follow-up |
N: 840 eyes of 693 patients Inclusion criteria: >18 years, type 1 or 2 DM, study eye: (1) BCVA (E-ETDRS) between 24 and 73 (20/320 and 20/40), (2) retinal thickening due to DMO involving the center of the macula main cause for visual loss, (3) CMT ≥250 µm, (4) no expectation of scatter photocoagulation within 4 months Exclusion criteria: any prior treatment with IV corticosteroids, peribulbar steroid injection within prior 6 months, photocoagulation for DMO within prior 15 weeks, panretinal scatter photocoagulation within prior 4 months, pars plana vitrectomy, history of open-angle glaucoma or steroid-induced IOP elevation requiring IOP-lowering treatment, and IOP ≥25 mm Hg Age: 63 SD9 years Sex: 49% female Diabetes type: 95% type 2 DM, 5% type 1 DM HbA1c: 7.9 SD1.8% Baseline VA: ETDRS letter score 59 SD11 (∼20/63) Baseline CMT: 24 SD130 µm Comorbidities: 21% pseudophakic, 2% ocular hypertension, 7% mild NPDR, 13% moderate NPDR, 40% moderately severe NPDR, 11% severe NPDR, 23.5% mild to moderate, 3% high risk PDR |
Group 1 (IVT1, n=256 eyes): 1 mg IV triamcinolone (3.5 treatments) Group 2 (IVT4, n=254 eyes): 4 mg IV triamcinolone (3.1 treatments) Group 3 (L, n=330 eyes): focal/grid photocoagulation (2.9 treatments) Regimen for all groups: retreatment protocol: where indicated, retreatment was performed within 4 weeks after the follow-up visit and no sooner than 3.5 months from the time of last treatment; eyes were generally retreated unless: (1) little or no oedema involving the center of the macula present and CMT ≤225 µm, (2) VA letter score ≥79 (20/25 or better), (3) substantial improvement in macular oedema since last treatment (eg, ≥50% decrease in CMT), (4) clinically significant adverse effect from prior treatment, (5) additional treatment deemed futile (<5 letter improvement in VA letter score or lack of CMT reduction) and (6) for laser group, complete focal/grid photocoagulation already given, with no areas identified for which additional treatment was indicated Laser Modified ETDRS protocol as used in prior DRCR.net protocols |
At 2 years BCVA (E-ETDRS): |
|||
| BCVA (letters) | p Value | |||||
| IVT1 | −2 SD18 | 0.02 vs L NS vs IVT4 |
||||
| IVT4 | −3 SD22 | 0.002 vs L | ||||
| L | +1 SD17 | |||||
| BCVA gain categories | ||||||
| IVT1 | +10 or more: 25% +9 to −9: 50% −10 – more: 26% |
0.03 vs L, NS vs IVT4 | ||||
| IVT4 | +10 or more: 28% +9 to −9: 44% −10 or more: 28% |
0.01 vs L | ||||
| L | +10 or more: 31% +9 to −9: 50% −10 or more: 19% |
|||||
| Subgroups: ▸ Similar results when considering only pseudophakic eyes or eyes with minimal cataract no substantially different results based on baseline VA, baseline CMT, history of focal/grid photocoagulation for DMO ▸ 3 year results consistent with 2 year results for BCVA and CMT |
||||||
| CMT (OCT): | ||||||
| CMT (µm) | p Value | |||||
| IVT1 | −86 SD167 | <0.001 vs L, NS vs IVT4 |
||||
| IVT4 | −77 SD160 | <0.001 vs L | ||||
| L | −139 SD148 | |||||
| Progression of retinopathy: | ||||||
| 2 years | 3 years | p Value | ||||
| IVT1 | 29% | 35% | ||||
| IVT4 | 21% | 30% | <0.05 vs L | |||
| L | 31% | 37% | ||||
| Gillies et al Sutter et al
32
136–138 Australia Design: 2-arm placebo-controlled RCT Follow-up: 2 years, additional 3-year follow-up |
N: 69 eyes of 43 patients Inclusion criteria: patients with persistent (≥3 months after adequate laser treatment) DMO involving the central fovea, BCVA in the affected eye ≤6/9 Exclusion criteria: uncontrolled glaucoma, loss of vision due to other causes, systemic treatment with >5 mg prednisolone (or equivalent) daily, intercurrent severe systemic disease, any condition affecting follow-up or documentation Age: 62.4–69.6 SD9.2–12.5 years Sex: 52% female Diabetes type: not reported HbA1c: 7.63–8.28 SD1.12–1.41 Baseline VA: ETDRS letter score 60.5–61.3 SD11.9–13.2 Baseline CMT: 439–444 SD101–125 µm Comorbidities: 25% pseudophakic |
Group 1 (IVT, n=34 eyes): 4 mg (0.1 ml) IV triamcinolone acetonide (mean 2.6 injections over 2 years) Group 2 (C, n=35 eyes): placebo injection (subconjunctival saline injection) (mean 1.8 injections over 2 years) Regimen for all groups: retreatment considered at each visit as long as treatments were at least 6 months apart (retreatment if VA decreased ≥5 letters from previous peak value and persistent CMT >250 µm), if no improvement after 4 weeks, further laser treatment was applied (n=1 laser treatment in intervention group, n=16 in placebo group, p=0.0001) Laser ETDRS protocol |
At 2 years BCVA (ETDRS): |
|||
| BCVA (letters) | p Value | |||||
| IVT | +3.1 | 0.01 vs C | ||||
| C | −2.9 | |||||
| CVA gain categories | ||||||
| IVT | +10 or more: 21% +9 to −9: 70% −10 or more: 9% |
0.013 vs C | ||||
| C | +10 or more: 12% +9 to −9: 62% −10 or more: 25% |
|||||
| CMT (OCT): | ||||||
| CMT (µm) | p Value | |||||
| IVT | −125 | 0.009 vs C, difference between groups 59 µm (95% CI 15 to 104) | ||||
| C | −75 | |||||
| Gillies et al33 Australia Design: 2-arm RCT Follow-up: 24 months |
N: 84 eyes of 54 patients Inclusion criteria: DMO involving the central fovea, CMT ≥250 µm, BCVA 17–70 letters (∼20/40–20/400), laser treatment could be safely delayed for 6 weeks without significant adverse effects Exclusion criteria: uncontrolled glaucoma, controlled glaucoma but with a glaucomatous visual field defect, loss of vision resulting from other causes, systemic treatment with >5 mg prednisolone (or equivalent) daily, retinal laser treatment within 4 months, intraocular surgery within 6 months, concurrent severe systemic disease, any condition affecting follow-up or documentation Age: 65.4–66.9 SD8.9–9.5 years Sex: 38.1–47.6% female Diabetes type: not reported HbA1c: 7.81–8.02 SD1.44–1.63% Baseline VA: letter score 55.2–55.5 SD11.3–12.5 Baseline CMT: 482.1–477.4 SD122.7–155.5 µm Comorbidities: not reported |
Group 1 (IVTL, n=42 eyes): 4 mg (0.1 ml) IV triamcinolone acetonide followed by laser treatment (at least 1 retreatment in 2nd year in 69%) Group 2 (L, n=42 eyes): sham injection followed by laser treatment (at least 1 retreatment in 2nd year in 45%) Regimen for all groups: retreatment with injection followed by laser at discretion of chief investigator, with at least 6 weeks between treatments; no retreatment if: (1) investigator considered the macula nearly flat and CMT <300 µm; (2) VA was ≥79 letters (20/25) or VA had improved by ≥5 letters compared with the best VA after treatment or baseline acuity; (3) laser treatment was considered by the investigator as inappropriate or had no potential for improvement |
At 24 months BCVA (ETDRS): |
|||
| BCVA (letters) | p Value | |||||
| ITL | +0.76 | NS vs L | ||||
| L | −1.49 | |||||
| BCVA gain categories | ||||||
| IVTL | +10 or more: 36% +9 to −9: 31% −10 or more: 33% |
0.049 vs L | ||||
| L | +10 or more: 17% +9 to −9: 59% −10 or more: 24% |
|||||
| Subgroups: ▸ BCVA outcome not significantly affected by cataract surgery CMT (OCT): |
||||||
| CMT (µm) | p Value | |||||
| IVTL | −137.1 | NS vs L | ||||
| L | −109.6 | |||||
| Kim et al45 Korea Design: 2-arm RCT Follow-up: 3 years |
N: 86 eyes of 75 patients Inclusion criteria: diffuse DMO Exclusion criteria: not reported Age: not reported Sex: not reported Diabetes type: not reported HbA1c: not reported Baseline VA: not reported Baseline CMT: not reported Comorbidities: not reported |
Group 1 (IVT, n=38 eyes): 4 mg IV triamcinolone (1.88 additional treatments, completion 68.1%)
Group 2 (IVTL, n=48 eyes): macular laser photocoagulation 4 weeks after 4 mg IV triamcinolone (0.92 additional treatments, completion 77.1%) Regimen for all groups: additional treatment possible, criteria not mentioned Laser protocol not reported |
At 3 years BCVA: not reported Outcomes related to DMO: |
|||
| No DMO recurrence | p Value | |||||
| IVT | 3.9% | |||||
| IVTL | 24.3% | 0.028 vs IVT | ||||
| Time DMO not present | ||||||
| IVT | 10.33 months | |||||
| IVTL | 19.88 months | 0.027 vs IVT | ||||
| Lam et al34 Hong Kong Design: 3-arm RCT Follow-up: 6 months (2 years planned) |
N: 111 eyes of 111 patients Inclusion criteria: >18 years, type 1 or 2 DM, clinically significant DMO (ETDRS), CMT ≥250 µm Exclusion criteria: macular oedema due to causes other than diabetic maculopathy, signs of vitreomacular traction, proliferative diabetic retinopathy, aphakia, history of glaucoma or ocular hypertension, macular ischemia, any laser procedure within 3 months, ocular surgery within 6 months, significant media opacities Age: 64.7–67.2 SD8.2–10.3 years Sex: 42–59% female Diabetes type: not reported HbA1c: not reported Baseline VA: ETDRS logMAR 0.64–0.72 SD0.34–0.36 Baseline CMT: 385–424 SD91–108 µm Comorbidities: 66–84% phakic eyes |
Group 1 (IVT, n=38 eyes): 4 mg IV triamcinolone (no retreatments) Group 2 (IVTL, n=36 eyes): 4 mg IV triamcinolone followed by grid laser photocoagulation (ETDRS) (laser treatment once the macular oedema had reduced to <250 µm at the foveal center or at 1 to 2 months after injection, whichever was earlier) Group 3 (L, n=37 eyes): grid laser photocoagulation (n=3 retreatments) (no retreatments) Regimen for all groups: in case of recurrence or persistence of macular oedema, retreatment offered according to study group, at intervals no less than 4 months Laser ETDRS protocol |
At 6 months BCVA (ETDRS): |
|||
| BCVA improvement | p Value | |||||
| IVT | −0.7 SD 10.7 log MAR Plus ≥15 letters: 5% |
NS between groups | ||||
| IVTL | −1.1 SD 10.8 log MAR Plus ≥15 letters: 3% |
|||||
| L | −1.6 SD 11.5 log MAR Plus ≥15 letters: 5% |
|||||
| CMT (OCT): | ||||||
| CMT (µm) | p Value | |||||
| IVT | 342 SD124 (−54) | NS between groups, <0.01 vs baseline | ||||
| IVTL | 307 SD181 (−116) | <0.01 vs baseline | ||||
| L | 350 SD169 (−35) | |||||
| Ockrim et al/Sivaprasad et al42
62 UK Design: 2-arm RCT Follow-up: 1 year |
N: 88 eyes of 88 patients Inclusion criteria: clinically significant DMO persisting ≥4 months, ≥1 previous laser treatment, BCVA 6/12–3/60, VA in fellow eye ≥3/60, duration visual loss <24 months Exclusion criteria: significant macular ischemia, baseline IO >23 mm Hg, glaucoma, coexistent renal disease, loss of VA due to other causes, previous vitrectomy, intraocular surgery within 3 months of study entry, previous inclusion in other DR trials, inability to return to follow-up, inability to give informed consent Age: 62.3–64.8 SD7.5–10.1 years Sex: 28.9–34.9% female Diabetes type: 97.8–100% type 2 DM HbA1c: 7–7.8 IQR6.5–8.7% Baseline VA: ETDRS letter score 53.0–54.6 SD13.3–14.2 Baseline CMT: 410.4–413.4 SD127.8–134.1 µm Comorbidities: 17.8–19.5% PDR, 13.3–18.6% pseudophakia, 15–17.8% posterior vitreous detachment |
Group 1 (IVT, n=43 eyes): 4 mg IV triamcinolone (mean number of IVT injections 1.8 (range 1–3)) Group 2 (L, n=45 eyes): ETDRS laser photocoagulation (mean number of grid laser sessions 2.1 (range 1–3)) Regimen for all groups: patients retreated at 4 and 8 months if they had persistent macular oedema Laser ETDRS protocol |
At 12 months BCVA (ETDRS): |
|||
| BCVA (letters) | p Value | |||||
| IVT | −0.2 | NS vs L | ||||
| L | +1.7 | |||||
| Plus ≥15 letters | ||||||
| IVT | 4.8% | NS vs L | ||||
| L | 12.2% | |||||
| CMT (optical coherence tomography): | ||||||
| CMT (µm) | p Value | |||||
| IVT | −91.3 | NS vs L | ||||
| L | −63.7 | |||||
BCVA, best corrected visual acuity; C, control; CMT, central macular thickness; CPL, control plus laser; CSME, clinically significant macular oedema; DDS, dexamethasone; DIL, dexamethasone followed by laser; DM, diabetes mellitus; DMO, diabetic macular oedema; DP, diastolic pressure; DR, diabetic retinopathy; HR QoL, health-related quality of life; IOP, intraocular pressure; IV, intravitreal; IVB, intravitreal bevacizumab; IVP, intravitreal pegaptanib; IVR, intravitreal ranibizumab; IVT, intravitreal triamcinolone; IVTL, intravitreal triamcinolone plus laser; IVVTE, intravitreal VEGF Trap Eye; L, laser; MLT/MPC, macular laser therapy/macular photocoagulation; NEI VFQ-25, National Eye Institute Visual Function Questionnaire-25; NPDR, non-proliferative diabetic retinopathy; NR, not reported; OCT, optical coherence tomography; PDR, proliferative diabetic retinopathy; PRP, panretinal photocoagulation; RCT, randomised controlled trial; RDL, ranibizumab plus deferred laser; RPL, ranibizumab plus laser; SOC, standard of care; SP, systolic pressure; SRFA, fluocinolone; TPL, triamcinoloine plus laser; VA, visual acuity; VEGF, vascular endothelia growth factor.
Table 8.
Trials assessing more than one drug
| Study | Participants and baseline values | Intervention | Outcome (change from baseline at study end) | ||
|---|---|---|---|---|---|
| Ahmadieh et al31 Iran Design: 3-arm placebo-controlled RCT Follow-up: 24 weeks |
N: 115 eyes of 101 patients Inclusion criteria: eyes with clinically significant DMO unresponsive to previous macular laser photocoagulation (last session >3 months prior) Exclusion criteria: visual acuity ≥20/40; history of cataract surgery within past 6 months; prior intraocular injection or vitrectomy, glaucoma or ocular hypertension; PDR with high-risk characteristics; vitreous hemorrhage; significant media opacity; presence of traction on the macula; pregnancy; serum creatinine ≥3 mg/100 ml; monocular patients Age: 59.7 SD8.3 years (range 39–74) Sex: 50.5% female Diabetes type: not reported, 27.6–33.3% on insulin HbA1c: 9.35–10.06% Baeline VA: not reported Baseline CMT: not reported Comorbidities: (percentage of eyes) 13.9% history of cataract surgery, 81.7% NPDR, 4.3% early PDR, 13.9% regressed PDR; no iris neovascularisation |
Group 1 (IVB, n=41 eyes): bevacizumab 1.25 mg (0.05 ml) Group 2 (IVB/IVT, n=37 eyes): combined bevacizumab (1.25 mg (0.05 ml)) and triamcinolone (2 mg (0.05 ml)), followed by two injections of bevacizumab alone Group 3 (C, n=37 eyes): sham injection Regimen for all groups: 3 consecutive IV injections at 6-week intervals |
At 24 weeks BCVA (Snellen chart): |
||
| BCVA (logMAR), 95% CI | p Value | ||||
| IVB | −0.18 (–0.29, −0.08) (+9 letters (4, 14.5)) | 0.01 vs C, NS vs IVB/IVT | |||
| IVB/IVT | −0.21 (−0.30, −0.12) (+10.5 letters (6, 15)) | 0.006 vs C | |||
| C | −0.03 (−0.08, 0.14) (+1.5 letters (−7, 4)) | ||||
| CMT (OCT): | |||||
| CMT (µm), 95% CI | p Value | ||||
| IVB | −95.7 (−172.2, −19.3) | 0.012 vs C, NS vs IVB/IVT | |||
| IVB/IVT | −92.1 (−154.4, −29.7) | 0.022 vs C | |||
| C | 34.9 (7.9, 61.9) | ||||
| ATEMD Oliveira Neto et al56 Multicenter Design: 3-arm RCT Follow-up: 6 months Note: only 48.3% completion |
N: 120 eyes of 120 patients Inclusion criteria: DMO, BCVA 20/40–20/400, CMT ≥275 µm Exclusion criteria: PDR, laser photocoagulation in previous 3 months, no IV corticosteroid or anti-VEGF in previous 3 months Age: not reported Sex: not reported Diabetes type: not reported HbA1c: not reported Baseline VA: not reported Baseline CMT: not reported Comorbidities: not reported |
Group 1 (IVB, n=NR eyes): 1.25 mg (0.05 ml) of IV bevacizumab Group 2 (IVT, n=NR eyes): 4 mg (0.1 ml) of IV triamcinolone acetonide Group 3 (IVB/IVT, n=NR eyes): 1.25 mg (0.05 ml) of IV bevacizumab plus 4 mg (0.1 ml) of IV triamcinolone acetonide Regimen for all groups: monthly injections |
At 6 months BCVA: ▸ no significant difference between groups (between 1.7 and 2.3 lines gained in the different groups in 2010 report (n=18)) CMT (OCT): ▸ CMT reduced in all 3 groups (between 17 and 33% reduction in the different groups in 2010 report (n=18)); no significant difference between groups |
||
| DRCR Network 2010 (Elman et al)21
46 USA Multicenter Design: 4-arm placebo-controlled RCT Follow-up: 1–2 years; 2 years extension (Elman)46 for consenting patients |
N: 854 eyes of 691 patients Inclusion criteria: ≥18 years, type 1 or 2 DM; study eye: (1) BCVA letter score 78–24 (20/32–20/320), (2) definite retinal thickening due to DMO assessed to be main cause of visual loss, (3) retinal thickness measured on time domain OCT ≥250 µm in central subfield (2 study eyes per patient could be included if both were eligible at study entry) Exclusion criteria: (1) treatment for DMO within the prior 3 months, (2) panretinal photocoagulation within the prior 4 months or anticipated need for panretinal photocoagulation within the next 6 months, (3) major ocular surgery within the prior 4 months, (4) history of open-angle glaucoma or steroid-induced IOP elevation, requiring IOP-lowering treatment, (5) IOP ≥25 mm Hg; systolic pressure >180 mm Hg, diastolic pressure >110 mm Hg; myocardial infarction, other cardiac event requiring hospitalisation, cerebrovascular accident, transient ischemic attack, treatment for acute congestive heart failure within 4 months before randomisation Age: median 62–64 years (25th, 75th centile 55–58, 69–70) Sex: 41–46% female Diabetes type: 6–9% type 1 DM, 89–92% type 2 DM, 2–3% uncertain HbA1c: median 7.3–7.5% (25th, 75th centile 6.5–6.7, 8.3–8.6) Baseline VA: letter score 63 SD12 (∼20/63 SD2.4 lines) Baseline CMT: 405 SD134 µm Comorbidities: 60–67% prior treatment for DMO; 61–68% with NPDR, 26–36% with PDR or PDR scars |
Group 1 (CPL, n=293 eyes): sham injection plus prompt (within 3–10 days after injection) focal/grid photocoagulation Group 2 (RPL, n=187 eyes): 0.5 mg IV ranibizumab plus prompt focal/grid photocoagulation Group 3 (RDL, n=188 eyes): 0.5 mg IV ranibizumab plus deferred (≥24 weeks) focal/grid photocoagulation Group 4 (TPL, n=186 eyes): 4 mg IV triamcinolone plus prompt focal/grid photocoagulation Regimen for all groups: Baseline treatment 0.5 mg IV ranibizumab and 4 mg preservative free triamcinolone; study treatment every 4 weeks up to 12 weeks, then retreatment algorithm: 16 to 20 weeks, monthly retreatment unless ‘success’ criteria were met (visual acuity letter score ≥84 (20/20) or OCT central subfield thickness <250 µm); 24–48 weeks, patients subdivided (according to predefined criteria) into ‘success’, ‘improvement’, ‘no improvement’ or ‘failure’; ‘improvement’ group continued treatment, other groups treated at investigator discretion; alternative treatment permitted if eye met criteria for ‘failure’ or ‘futility’. In the case of retreatment, ranibizumab could be given as often as every 4 weeks, and triamcinolone every 16 weeks (with sham injections as often as every 4 weeks). Retreatment for focal/grid laser (after ≥13 weeks from previous treatment) if there was oedema involving or threatening the center of the macula and if complete laser had not been given; retreatment algorithms facilitated by web-based real-time data entry system. Median number of drug injections before 1 year visit was 8–9 for ranibizumab, 3 for triamcinolone, and 5 sham injections. Retreatment between 1 and 2 years (Elman 2011): median injections 2 in RPL group, 3 in RDL group; in TPL group 68% of eyes received at least 1 injection; at least one focal/grid laser sessions between 1 and 2 years: 51% CPL, 40% RPL, 29% RDL, 52% TPL Laser Modified ETDRS protocol as used in prior DRCR.net protocols |
At 1 year BCVA (E-ETDRS Visual Acuity Test): |
||
| BCVA (letters) | p Value | ||||
| CPL | +3 SD13 | ||||
| RPL | +9 SD11 | <0.001 vs CPL | |||
| RDL | +9 SD12 | <0.001 vs CPL | |||
| TPL | +4 SD13 | NS vs CPL | |||
| BCVA gain categories (letters) | |||||
| CPL | +10 or more: 28% +9 to −9: 59% −10 or more: 13% |
||||
| RPL | +10 or more: 50% +9 to −9: 45% −10 or more: 4% |
<0.001 vs CPL | |||
| RDL | +10 or more: 47% +9 to −9: 51% −10 or more: 3% |
<0.001 vs CPL | |||
| TPL | +10 or more: 33% +9 to −9: 52% −10 or more: 14% |
NS vs CPL | |||
| Subgroups: ▸ BCVA results in TPL group substantially better for pseudophakic eyes than for phakic eyes (comparable to results for RPL and RDL groups) (p not reported) ▸ No difference in results according to prior treatment for DMO, baseline VA, baseline CMT, baseline level of retinopathy, focal or diffuse oedema |
|||||
| CMT (OCT): | |||||
| CMT (µm) | p Value | ||||
| CPL | −102 SD151 | ||||
| RPL | −131 SD129 | <0.001 vs CPL | |||
| RDL | −137 SD136 | <0.001 vs CPL | |||
| TPL | −127 SD140 | <0.001 vs CPL | |||
|
Subgroups: ▸ pattern of CMT decrease similar for groups with CMT <400 and ≥400 µm at baseline ▸ Significantly more patients with severe NPDR or worse improved by 2 levels or more in the ranibizumab groups (28%, no significant change in the other groups) |
|||||
| At 2 years (expanded results, Elman 2011) | |||||
| BCVA (E-ETDRS Visual Acuity Test): | |||||
| BCVA (letters) | p Value | ||||
| CPL (n=211) | +3 SD15 | ||||
| RPL (n=136) | +7 SD13 | 0.03 vs CPL | |||
| RDL (n=139) | +9 SD14 | <0.001 vs CPL | |||
| TPL (n=142) | +2 SD19 | NS vs CPL | |||
| BCVA gain categories (letters) | |||||
| CPL | +10 or more: 36% +9 to −9: 52% −10 or more: 13% |
||||
| RPL | +10 or more: 44% +9 to −9: 49% −10 or more: 7% |
NS vs CPL | |||
| RDL | +10 or more: 49% +9 to −9: 48% −10 or more: 3% |
0.01 vs CPL | |||
| TPL | +10 or more: 41% +9 to −9: 40% −10 or more: 19% |
NS vs CPL | |||
| CMT (OCT): | |||||
| CMT (µm) | p Value | ||||
| CPL | −138 SD149 | ||||
| RPL | −141 SD155 | 0.003 vs CPL | |||
| RDL | −150 SD143 | 0.01 vs CPL | |||
| TPL | −107 SD145 | NS vs CPL | |||
| Jorge et al51 Brazil Design: Prospective RCT Follow-up: 24 and 48 weeks (to date, 73% and 56% of patients completed 24 and 48 weeks, respectively) |
N: 63 eyes of 47 patients Inclusion criteria: Refractory cener-involving DMO Exclusion criteria: NR Age: NR Sex: NR Diabetes type: NR HbA1c: NR Baseline VA: NR Baseline CMT: NR Comorbidities: NR |
Group 1 (IVB 1.5 mg, n=NR): injections at baseline and monthly if CSFT (central subfield thickness) measured by SDOCT (spectral domain OCT) >275 µm Group 2 (IVR 0.5 mg, n=NR): injections at baseline and monthly if CSFT >275 µm |
At 48 weeks BCVA |
||
| Mean BCVA reduction from baseline (logMAR) | p Value | ||||
| IVB1.5 | −0.21 | vs baseline <0.05 at all-time points vs IVR0.5: no significant difference at all time-points |
|||
| IVR0.5 | −0.21 | vs baseline <0.05 at all time-points vs IVB1.5: no significant difference at all time-points |
|||
| CSFT | |||||
| Mean CSFT reduction from baseline | p Value | ||||
| IVB1.5 | −129.6 µm | vs baseline <0.05 at all-time points vs IVR0.5 no significant different at all-time points |
|||
| IVR0.5 | −137.9 µm | vs baseline <0.05 at all-time points vs IVB1.5 no significant different at all-time points |
|||
| Lim et al55 Korea Design: 3-arm RCT Follow-up: 12 months |
N: 111 eyes of 105 patients Inclusion criteria: eyes with clinically significant DMO based on ETDRS and DMO with central macular thickness of at least 300 µm by optical coherence tomography (OCT) Exclusion criteria: unstable medical status, including glycemic control and blood pressure; any previous treatment for DMO, including intravitreal, sub-Tenon injection or macular photocoagulation, history of vitreoretinal surgery, uncontrolled glaucoma; proliferative diabetic retinopathy with active neovascularisation, previous panretinal photocoagulation, presence of vitreomacular traction, history of systemic corticosteroids within 6 months, contraindications for bevacizumab or triamcinolone acetonide Age: 60.4 SD 7.4 (range 48–70) years Sex: 52% female Diabetes type: NR HbA1c: 7.2 SD 1.2–7.4 SD1.2 Baseline VA: 0.62 SD 0.23–0.65 SD 0.28 logMAR Baseline CMT: 447 SD 110–458 SD 92 µm Comorbidities: NR |
Group 1 (IVB/IVT, n=36): IV injection of 1.25 mg (0.05 ml) IVB at 0 and 6 weeks and IV injection of 2 mg (0.05 ml) IVT at 0 weeks. Mean number of addition injection 1.28 Group 2 (IVB, n=38): IV injection of 1.25 mg (0.05 ml) IVB at 0 and 6 weeks. Mean number of injections 2.54. Group 3 (IVT, n=37): IV injection of 2 mg (0.05 ml) IVT at 0 weeks. Mean number of injections 1.04 Unclear if rescue laser was available IVB injections were repeated if CMT appeared >300 µm on OCT in at least 6 weeks in all three groups |
At 12 months | ||
| BCVA (logMAR) | p Value | ||||
| IVB/IVT | −0.15 | 0.088 (between groups) | |||
| IVB | −0.16 | ||||
| IVT | −0.16 | ||||
| CMT (µm) | p Value | ||||
| IVB/IVT | −199 | 0.132 (between groups) | |||
| IVB | −17s9 | ||||
| IVT | −200 | ||||
| Soheilian et al37
41
54
141 Iran Design: 3-arm RCT Follow-up: 36 weeks(Soheilian 2007 reports 12 week results of the same trial, these were not considered here) |
N: 150 eyes of 129 patients Inclusion criteria: eyes with clinically significant DMO (ETDRS criteria) Exclusion criteria: previous panretinal of focal laser photocoagulation, prior ocular surgery or injection, history of glaucoma or ocular hypertension, VA ≥20/40 or <20/300, iris neovascularisation, high risk PDR, significant media opacity, monocularity, pregnancy, serum creatinine ≥3 mg/dL, uncontrolled DM Age: 61.2 SD6.1 years Sex: 47.3% female Diabetes type: not reported HbA1c: not reported Baseline VA: 0.55–0.73 SD0.26–0.28 logMAR Baseline CMT: 300–359 SD118–149 µm Comorbidities: 94% NPDR, 6% early PDR |
Group 1 (IVB, n=50 eyes): IV injection of bevacizumab 1.25 mg (0.05 ml) (retreatment IVB 14 eyes) Group 2 (IVB/IVT, n=50 eyes): IV injection of combined bevacizumab (1.25 mg (0.05 ml)) and triamcinolone (2 mg (0.05 ml)), followed by two injections of bevacizumab alone (retreatment IVB/IVT 10 eyes) Group 3 (MPC, n=50 eyes): focal or modified grid laser (retreatment MPC 3 eyes) Regimen for all groups: Retreatments performed at 12 week intervals as required |
At 36 weeks BCVA (Snellen chart): |
||
| BCVA (logMAR), SD | p Value | ||||
| IVB | −0.28 SD0.25 (+14 SD12.5 letters) | 0.053 vs IVB/IVT or MPC | |||
| IVB/IVT | −0.04 SD0.33 (+2 SD16.5 letters) | NS vs MPC | |||
| MPC | +0.01 SD0.27 (−0.5 SD13.5 letters) | ||||
| Snellen line changes | |||||
| IVB | +2 lines or more: 37% stable within 2 lines: 59.3% −2 lines or more: 3.7% |
NS between groups | |||
| IVB/IVT | +2 lines or more: 25% stable within 2 lines: 54.2% −2 lines or more: 20.8% |
||||
| MPC | +2 lines or more: 14.8% stable within 2 lines: 66.7% −2 lines or more: 18.5% |
||||
| CMT (OCT): | |||||
| CMT (µm), SD | p Value | ||||
| IVB | −56 SD140 | 0.044 vs baseline, NS between groups | |||
| IVB/IVT | −5 SD113 | ||||
| MPC | −8 SD67 | ||||
| Subgroups: ▸ larger CMT reduction in subgroup with ≥400 µm at baseline (36 weeks: IVB −27.2 SD34.8%, IVB/IVT –8.8 SD35.9%, MPC −15.1 SD14.6%, p<0.001 vs baseline in IVB and MPC groups only) |
|||||
BCVA, best corrected visual acuity; C, control; CMT, central macular thickness; CSME, clinically significant macular oedema; DDS, dexamethasone; DIL, dexamethasone followed by laser; DM, diabetes mellitus; DMO, diabetic macular oedema; DP, diastolic pressure; DR, diabetic retinopathy; HR QoL, health-related quality of life; IOP, intraocular pressure; IV, intravitreal; IVB, intravitreal bevacizumab; IVP, intravitreal pegaptanib; IVR, intravitreal ranibizumab; IVT, intravitreal triamcinolone; IVTL, intravitreal triamcinolone plus laser; IVVTE, intravitreal VEGF Trap Eye; L, laser; MLT/MPC, macular laser therapy/macular photocoagulation; NEI VFQ-25, National Eye Institute Visual Function Questionnaire-25; NPDR, non-proliferative diabetic retinopathy; NR, not reported; OCT, optical coherence tomography; PDR, proliferative diabetic retinopathy; PRP, panretinal photocoagulation; RCT, randomised controlled trial; SOC, standard of care; SP, systolic pressure; SRFA, fluocinolone; VA, visual acuity; VEGF, vascular endothelia growth factor.
Table 9.
Ranibizumab safety data
| READ-2 study28 47 | RESOLVE study36 | RESTORE study24 | RISE study38 | RIDE study38 | |
|---|---|---|---|---|---|
| Number of patients | IVR: n=42; L: n=42; IVRL: n=42 | IVR0.3: n=51; IVR0.5: n=51; C: n=49 | IVR: n=116; IVRL: n=118; L: n=111 | IVR0.3: 125; IVR0.5: 126; C: 123 | IVR0.3: 125; IVR0.5: 124; C: 127 |
| Ocular adverse events | |||||
| Eye pain | NR | IVR0.3: n=9 (18%); IVR0.5: n=9 (18%); C: n=10 (20%) | IVR: n=13 (11%); IVRL: n=10 (8%); L: n=12 (11%) | IVR0.3: 26%; IVR0.5: 21%; C: 19% | IVR0.3: 8%; IVR0.5: 12.9%; C: 7.1% |
| Conjunctival hyperaemia | NR | NR | IVR: n=9 (8%); IVRL: n=6 (5%); L: n=6 (5%) | NR | NR |
| Conjunctival haemorrhage | NR | IVR0.3: n=10 (20%); IVR0.5: n=13 (25%); C: n=7 (14%) | IVR: n=8 (7%); IVRL: n=10 (8%); L: n=0 | IVR0.3: 54%; IVR0.5: 52%; C: 32% | IVR0.3: 40.8%; IVR0.5: 50%; C: 31.5% |
| IOP increase | NR | IVR0.3: n=6 (12%); IVR0.5: n=15 (29%); C: n=1 (2%) | IVR: n=1 (<1%); IVRL: n=1 (<1%); | IVR0.3: 20%; IVR0.5: 14%; C: 2% | IVR0.3 : 15.2%;IVR0.5: 18.5%; C: 11% |
| Vitreous haemorrhage | IVR: n=1 (2%); L: n=4 (10%); IVRL: n=3 (7%) | IVR0.3: n=1 (2%); IVR0.5: n=0; C: n=0 | NR | IVR0.3: 3.2%; IVR0.5: 3.2%; C: 13% | IVR0.3: 0.8%; IVR0.5: 2.4%; C: 15% |
| Substantial worsening of DMO | L: n=1 (2%) | NR | NR | NR | |
| Retinal ischaemia | NR | IVR0.3: n=0; IVR0.5: n=1 (2%); C: n=0 | NR | NR | NR |
| Retinal artery occlusion | NR | IVR0.3: n=0; IVR0.5: n=1 (2%); C: n=0 | NR | NR | NR |
| Endophthalmitis | NR | IVR0.3: n=1 (2%); IVR0.5: n=1 (2%); C: n=0 | NR | IVR0.3: 0.8%; IVR0.5: 0; C: 0 | IVR0.3+IVR0.5: 1.2%; C: 0% |
| Retinal detachment | NR | IVR0.3: n=0; IVR0.5: n=0; C: n=1 (2%) | NR | IVR0.3: 0.8%; IVR0.5: 0; C: 0.8% | IVR0.3+IVR0.5: 0.4%; C: 0% |
| Neovascularisation | NR | NR | NR | IVR0.3: 0; IVR0.5: 0; C: 0.8% | IVR0.3: 0.8%; IVR0.5: 0.8%; C: 5.5% |
| Traumatic cataract | NR | NR | NR | IVR0.3: 0.8%; IVR0.5: 0.8%; C: 0 | IVR0.3+IVR0.5: 0.4%; C: 0% |
| Uveitis | NR | NR | NR | NR | IVR0.3+IVR0.5: 0.4%; C: 0% |
| Macular oedema | NR | NR | NR | IVR0.3: 16.8%; IVR0.5: 20.6%; C: 21.1% | IVR0.3: 19.2%; IVR0.5: 13.7%; C: 20.5% |
| Retinal exudates | NR | NR | NR | IVR0.3: 19.2%; IVR0.5: 17.5%; C: 20.3% | IVR0.3: 16%; IVR0.5: 15.3%; C: 11% |
| Retinal haemorrhage | NR | NR | NR | IVR0.3: 12.8%; IVR0.5: 12.7%; C: 20.3% | IVR0.3: 15.2%; IVR0.5: 22.6%; C: 18.9% |
| Cataract | NR | NR | NR | IVR0.3: 16.8%; IVR0.5: 11.9%; C: 14.6% | IVR0.3: 20%; IVR0.5: 23.4%; C: 23.6% |
| Vitreous detachment | NR | NR | NR | IVR0.3: 13.6%; IVR0.5: 11.1%; C: 15.4% | IVR0.3: 8.8%; IVR0.5: 12.9%; C: 15% |
| Ocular hyperemia | NR | NR | NR | IVR0.3: 15.2%; IVR0.5: 11.1%; C: 10.6% | IVR0.3: 3.2%; IVR0.5: 3.2%; C: 7.9% |
| Vitreous floaters | NR | NR | NR | IVR0.3: 12.8%; IVR0.5: 14.3%; C: 5.7% | IVR0.3: 7.2%; IVR0.5: 8.1%; C: 3.1% |
| Eye irritation | NR | NR | NR | IVR0.3: 10.4%; IVR0.5: 9.5%; C: 6.5% | IVR0.3: 5.6%; IVR0.5: 5.6%; C: 3.1% |
| Foreign body sensation in eyes | NR | NR | NR | IVR0.3: 12.8%; IVR0.5: 7.1%; C: 4.1% | IVR0.3: 8%; IVR0.5: 2.4%; C: 5.5% |
| Systematic adverse events | |||||
| Arterial thromboembolic events | Stroke in 1 pt (2%) in IVRL group- not related to study drug | IVR0.3: n=0; IVR0.5: n=3 (6%); C: n=2 (4%) | IVR: n=6 (5%); IVRL: n=1 (<1%); L: n=1 (<1%) | IVR0.3: 3.2% (n=1 stroke); IVR0.5: 7.9% (n=5 strokes); C: 7.3% (n=2 strokes) | IVR0.3: 1.6% (stroke), 5.6% (heart attack); IVR0.5: 2.4% (stroke), 2.4% (heart attack); C: 1.6% (stroke), 5.6% (heart attack) |
| Hypertension | NR | IVR0.3: n=4 (8%); IVR0.5: n=5 ((10%); C: n=5 (10%) | IVR: n=9 (8%); IVRL: n=6 (5%); L: n=9 (8%) | Serious IVR0.3: 0.8%; IVR0.5: 3.2%; C: 0.8% |
Serious IVR0.3: 1.6%; IVR0.5: 1.6%; C: 0% |
| Non-ocular haemorrhage | NR | IVR0.3: n=1 (2%); IVR0.5: n=1 (2%); C: n=0 | IVR: n=1 (<1%); IVRL: n=0; L: n=1 (<1%) | NR | NR |
| Proteinuria | NR | NR | IVR: n=1 (<1%); IVRL: n=1 (<1%); L: n=0 | NR | NR |
| Deaths | 1 (2%) due to CVA in IVRL group | NR | IVR: n=2 (2%); IVRL: n=2 (2%); L: n=2 (2%) | IVR0.3: 2.4%; IVR0.5: 4%; C: 0.8% | IVR0.3: 3.2%; IVR0.5: 4.8%; C: 1.6% |
C, control; DMO, diabetic macular oedema; IOP, intraocular pressure; IVR, intravitreal ranibizumab; IVRL, intravitreal ranibizumab plus laser; L, laser; NR, not reported.
Table 10.
Bevacizumab safety
| BOLT study23 52 | Lam et al35 | Faghihi et al53 | |
|---|---|---|---|
| Number of patients | MLT: n=38; IVB: n=42 | IVB1.25, n=26; IVB2.5, n=26 | IVB1.25 n=40 IVB 1.25 plus MLT n=40 |
| Ocular adverse events | Not reported | ||
| Loss of _15 or _30 ETDRS letters | MLT: n=1 transient, 3 at 24 month analysis; IVB: n=4 transient | No significant ocular events (IOP increase, retinal tear, retinal detachment, endophthalmitis); no significant difference in change in cataract scores between groups | |
| Vitreous haemorrhage | MLT: n=1; IVB: n=0 | ||
| Eye pain/irritation/watering during or after injection | MLT:n=0; IVB: n=8 | ||
| Red eye after injection | MLT: n=0; IVB: n=8 | ||
| Endophthalmitis | NR | ||
| Transient IOP increase | ≥30 mm Hg—MLT: 0; IVB: n=4≥45 mm Hg—MLT: n=1; IVB: n=1 | ||
| Floaters after injection | MLT: n=0; IVB: n=2 | ||
| Corneal epithelial defect | MLT:n=0; IVB:n=1 | ||
| Vitreomacular traction with macular oedema | MLT: n=1; IVB: n=0 | ||
| Systematic adverse events | |||
| Anaemia | MLT: n=1; IVB: n=0 | No systematic adverse effects (1 patient in 1.25 mg group with foot gangrene requiring amputation due to worsening diabetic neuropathy, considered unrelated to treatment) | |
| Vomiting after FFA | MLT: n=1; IVB: n=0 | ||
| Uncontrolled hypertension | MLT:n=0; IVB: n=1 | ||
| Polymyalgia rheumatica | MLT:n=0; IVB: n=1 | ||
| Intermittent claudication | MLT:n=0; IVB: n=1 | ||
| Gastroenteritis | MLT:n=0; IVB: n=1 | ||
| Fall | MLT:n=2; IVB: n=0 | ||
| Urinary tract infection | MLT:n=0; IVB: n=1 | ||
| Chest infection | MLT:n=0; IVB: n=1 | ||
| Headaches, dizziness, tiredness | MLT:n=1; IVB: n=0 | ||
| Bell palsy | MLT:n=1; IVB: n=0 | ||
| Admission for diabetic foot ulcer | MLT:n=1; IVB: n=1 | ||
| Admission for cholecystectomy | MLT:n=0; IVB: n=1 | ||
| Admission for fall/loss of consciousness | MLT:n=1; IVB: n=0 | ||
| Angina—hospital admission | MLT:n=1; IVB: n=0 | ||
| Cerebrovascular accident | MLT:n=1; IVB: n=0 | ||
| Myocardial infarction | MLT:n=0; IVB: n=2 | ||
| Coronary artery bypass graft | MLT:n=0; IVB: n=1 | ||
| Dyspnea, chest pain–admitted for hospital observation | MLT:n=0; IVB: n=1 | ||
| Death | NR | ||
ETDRS, Early Treatment Diabetic Retinopathy Study; FFA, fundus fluorescein; IOP, intraocular pressure; IVB, intravitreal bevacizumab; MLT, macular laser therapy; NR, not reported.
Table 11.
Pegaptanib safety
| Cunningham et al / Adamis et al39 57 | Sultan et al40 | |
|---|---|---|
| Number of patients | IVP0.3, n=44 eyes; IVP1, n=44 eyes; IVP3, n=42 eyes | IVP, n=133 eyes; C, n=127 eyes |
| Ocular adverse events | ||
| Eye pain | Pegaptanib: 31%; C: 17% | IVP: 11.1%; C: 7% |
| Vitreous haemorrhage | Pegaptanib: 22%; C: 7% | IVP: 6.3%; C: 7.7% |
| Punctuate keratitis | Pegaptanib: 18%; C: 17% | IVP: 11.8%; C: 6.3% |
| Cataract | Pegaptanib: 13%; C: 10% | IVP: 8.3%; C: 9.2% |
| Eye discharge | Pegaptanib: 11%; C: 10% | NR |
| Conjunctival haemorrhage | Pegaptanib: 10%; C: 0% | IVP: 22.2%; C: 14.1% |
| Vitreous opacities | Pegaptanib: 9%; C: 5% | NR |
| Blurred vision | Pegaptanib: 7%; C: 5% | NR |
| Other vitreous disorder | Pegaptanib: 7%; C: 0% | NR |
| Other visual disturbance | Pegaptanib: 7%; C: 0% | NR |
| Culture-negative endophthalmitis | Pegaptanib: n=1 | NR |
| IOP increase | NR | IVP: 17.4%; C: 6.3% |
| Retinal haemorrhage | NR | IVP: 6.3%; C: 10.6% |
| Retinal exudates | NR | IVP: 6.3%; C: 5.6% |
| Conjunctivitis | NR | IVP: 5.6%; C: 4.2% |
| Lacrimation increased | NR | IVP: 5.6%; C: 2.8% |
| Diabetic retinal oedema | NR | IVP: 11.1%; C: 17.6% |
| Macular oedema | NR | IVP: 9.7%; C: 11.6% |
| Systemic adverse events | ||
| Non-ocular hypertension | NR | IVP: 13.9%; C: 9.9% |
| Cardiac disorders | NR | IVP: 6.9%; C: 5.6% |
| Deaths | NR | IVP: n=4 |
IOP, intraocular pressure; IVP, intravitreal pegaptanib; NR, not reported.
Table 12.
Aflibercept safety
| DA VINCI 201030 58 | |
|---|---|
| Number of patients | IVVTE (all doses) n=175, laser n=44 |
| Ocular adverse events | |
| Conjunctival hemorrhage | At 6 months: Laser 18.2%, IVVTE 18.9% At 12 months: Laser 18.2%, IVVTE 26.9% |
| IOP increase | At 6 months: Laser 2.3%, IVVTE 9.7% At 12 months: Laser 2.3%, IVVTE 9.7% |
| Eye pain | At 6 months: Laser 4.5%, IVVTE 8.6% At 12 months: Laser 4.5%, IVVTE 13.7% |
| Ocular hyperaemia | At 6 months: Laser 4.5%, IVVTE 6.3% At 12 months: Laser 4.5%, IVVTE 7.4% |
| Vitreous floaters | At 6 months: Laser 4.5%, IVVTE 5.1% At 12 months: Laser 4.5%, IVVTE 6.9% |
| Endophthalmitis | At 6 months: Laser 0%, IVVTE 1.1% At 12 months: Laser 0%, IVVTE 1.1% |
| Uveitis | At 6 months: Laser 0%, IVVTE 0.6% At 12 months: Laser 0%, IVVTE 0.6% |
| Diabetic retinal oedema | At 6 months: Laser 2.3%, IVVTE 0% At 12 months: Laser 2.3%, IVVTE 4.6% |
| Visual acuity reduced | At 6 months: Laser 2.3%, IVVTE 0% At 12 months: Laser 2.3%, IVVTE 0% |
| Vitreous hemorrhage | At 6 months: Laser 2.3%, IVVTE 0% At 12 months: Laser 6.8%, IVVTE 0% |
| Corneal abrasion | At 6 months: Laser 0%, IVVTE 0.6% At 12 months: Laser 0%, IVVTE 4.6% |
| Retinal tear | At 6 months: Laser 0%, IVVTE 0.6% At 12 months: NR |
| Systematic events | |
| Hypertension | At 6 months: Laser 6.8%, IVVTE 9.7% At 12 months: Laser 0%, IVVTE 1.7% |
| Myocardial infarction | At 6 months: Laser 0%, IVVTE 1.1% At 12 months: Laser 0%, IVVTE 1.7% |
| Cerebrovascular event | At 6 months: Laser 0%, IVVTE1.1% At 12 months: Laser 2.3%, IVVTE 1.7% |
| Death | At 6 months: Laser 0%, IVVTE 1.7% At 12 months: Laser 2.3%, IVVTE 4% |
IOP, intraocular pressure; IVVTE, intravitreal vascular endothelial growth factor Trap Eye.
Table 13.
Dexamethasone safety
| Callanan et al44 | Haller et al59 | |
|---|---|---|
| Number of patients | ||
| Ocular adverse events | ||
| IOP elevation | DIL: 20% (p<0.001); 1% ≥10 mm HgL: 1.6% ; 0% ≥10 mm Hg | |
| Cataract | NR | NR |
| Anterior chamber cells | NR | DDS350: 29.1%; DDS700: 26.4%; C: 1.8% |
| Anterior chamber flare | NR | DDS350: 27.3%; DDS700: 20.8%; C: 8.8% |
| Vitreous haemorrhage | NR | DDS350: 20%; DDS700: 22.6%; C: 5.3% |
| Eye pain | NR | DDS350: 18.2%; DDS700: 9.4%; C: 3.5% |
| Vitreous disorder | NR | DDS350: 20%; DDS700: 15.1%; C: 3.5% |
| Increased IOP | NR | DDS350: 14.5%; DDS700: 9.4%; C: 0% |
| Conjunctival haemorrhage | NR | DDS350: 14.5%; DDS700: 7.5%; C: 0% |
| Vitreous floaters | NR | DDS350: 7.3%; DDS700: 17%; C: 0% |
| No significant differences in: reduced VA, eye irritation, abnormal sensation in eye, macular oedema, eye pruritus, retinal hemorrhage, DR, nonocular events | ||
Dil, dexamethasone followed by laser; DDS, dexamethasone; IOP, intraocular pressure; NR, not reported.
Table 14.
Fluocinolone safety
| FAME study (Campochiaro et al)29 60 | Pearson et al43 | |
|---|---|---|
| Number of patients | ||
| Ocular adverse events | ||
| IOP at 12 months | NR | NR |
| Progression of cataract | NR | NR |
| Cataract | NR | SRFA: 55.9%; SOC: 21.7% |
| Transient vitreous floaters | NR | NR |
| Transient subconjunctival haemorrhage | NR | NR |
| Cataract surgery | SRFA0.2: 41.1% (74.9% of those without cataract surgery at baseline, 80% at 36 months); SRFA0.5: 50.9% (84.5% of those without cataract surgery at baseline, 87.2% at 36 months); C: 7% (23.1% of those without cataract surgery at baseline, 27.3% at 36 months) | NR |
| Glaucoma | SRFA0.2: 1.6%; SRFA0.5: 2.3%; C: 0.5% | NR |
| Increased IOP | SRFA0.2: 3.2%; SRFA0.5: 3.3%; C: 0% | SRFA: 69.3%; SOC: 11.6% |
| IOP >30 mm Hg at any point during 36 months | SRFA0.2: 18.4%; SRFA0.5: 22.9%; C: 4.3% | NR |
| Trabeculectomy | SRFA0.2: 2.1%; SRFA0.5: 4.8%; C: 0% | NR |
| Other glaucoma surgery | SRFA0.2: 1.3%; SRFA0.5: 1.3%; C: 0.5% | NR |
| Trabeculoplasty | SRFA0.2: 0.8%; SRFA0.5: 2.3%; C: 0% | NR |
| Vitreous haemorrhage | NR | SRFA: 40.2%; SOC: 18.8% |
| Abnormal sensation in eye | NR | SRFA: 37%; SOC: 11.6% |
| Macular oedema | NR | SRFA: 34.6% |
| Eye pain | NR | SRFA: 26.8%; SOC: 15.9% |
| Eye irritation | NR | SRFA: 22%; SOC: 10.1% |
| Increased lacrimation | NR | SRFA: 22%; SOC: 8.7% |
| Photophobia | NR | SRFA: 21.3%; SOC: 21.7% |
| Blurred vision | NR | SRFA: 21.3%; SOC: 15.9% |
| Vitreous floaters | NR | SRFA: 21.3%; SOC: 8.7% |
| Systemic adverse events | ||
| Serious cardiovascular events | SRFA0.2: 12%; SRFA0.5: 13.2%; C: 10.3% | |
| Pruritus | NR | SRFA: 38.6%; SOC: 21.7% |
| Deaths | NR | NR |
IOP, intraocular pressure; NR, not reported; SOC, standard of care; SRFA, fluocinolone.
Table 15.
Triamcinolone safety
| DRCR Network 2008 (Ip et al/Beck et al/ Bressler et al) 22 61 63 64 | Gillies et al/Sutter et al32 136–138 | Gillies et al33 | Kim et al45 | Lam et al34 | Ockrim et al/ Sivaprasad et al42 62 | |
|---|---|---|---|---|---|---|
| Number of patients | ||||||
| Ocular adverse events | ||||||
| At 2 years (or 3 years when indicated) | At 2 years | – | Not reported | – | At 12 months | |
| IOP ≥30 mm Hg | IVT1: n=22; IVT4: n=53; L: n=3 | NR | NR | NR | IVT: IOP significantly higher than in L group (18.2 mm Hg, range 12–26 mm Hg); no cases of glaucoma | |
| IOP >22 mm Hg | NR | NR | NR | IVT: 37% (p=0.002 vs L); IVTL: 36% (p=0.002 vs L); L: 5% | NR | |
| IOP ≥10 mm Hg from baseline | IVT1: n=41; IVT4: n=85; L: n=12 | NR | NR | NR | NR | |
| IOP ≥5 mm Hg | NR | IVT: 68% (p=0.007 vs C); C: 10% | NR | NR | NR | |
| IOP lowering medication used | IVT1: n=31; IVT4: n=76; L: n=25 | IVT: 44% (p=0.0002 vs C); C: 3% | IVTL: 64% (p<0.001); L: 24% | NR | NR | |
| Cataract surgery | IVT1: 23% (of those phakic at baseline, 46% by 3 years (p<0.001 between all groups); IVT4: 51% (of those phakic at baseline, 83% by 3 years); L: 13% (of those phakic at baseline, 31% by 3 years) | IVT: 56% (of phakic eyes over 3 years, p<0.001 vs C); C: 8% (of phakic eyes over 3 years) | NR | NR | ||
| Ptosis | NR | NR | NR | NR | NR | |
| Retinal detachment | IVT1: n=2; IVT4: n=4; L: n=2 | NR | NR | None | NR | |
| Retinal vein occlusion | IVT1: n=1; IVT4: n=2; L: n=3 | NR | NR | NR | NR | |
| Retinal artery occlusion | IVT1: n=0; IVT4: n=0; L: n=1 | NR | NR | NR | NR | |
| Anterior ischemic optic neuropathy | IVT1: n=1; IVT4: n=0; L: n=0 | NR | NR | NR | NR | |
| Vitrectomy | IVT1: n=26; IVT4: n=19; L: n=31 | NR | NR | NR | NR | |
| Open angle glaucoma | IVT1: n=2; IVT4: n=7; L: n=2 | NR | NR | NR | NR | |
| Glaucoma filtering surgery | IVT1: n=0; IVT4: n=2; L: n=0 | NR | NR | NR | NR | |
| Laser trabeculoplasty | IVT1: n=0; IVT4: n=1; L: n=0 | IVT: n=2; C: n=0 | IVTL: n=1 | NR | NR | |
| Ciliary body destruction | IVT1: n=0; IVT4: n=1; L: n=0 | NR | NR | NR | NR | |
| Endophthalmitis | IVT1: n=0; IVT4: n=;0 L: n=0 | (Infectious) IVT: n=1; C: NR | (Culture-negative) IVTL: n=1 | None | (sterile) IVT: n=1 | |
| Pseudoendophthalmitis | IVT1: n=0; IVT4: n=;0 L: n=0 | NR | NR | NR | NR | |
| Chemosis | NR | NR | NR | NR | NR | |
| Percentage of increase in cataract scores | NR | NR | NR | IVT:+1.0 SD1.1 (p=NS vs L); IVTL:+1.3 SD1.9 (p=NS vs L); L:+0.5 SD0.9 | NR | |
| Ocular hypertension (>21 mm Hg) | NR | NR | NR | NR | NR | |
| Cataract progression | NR | NR | Phakic eyes, progression by ≥2 AREDS grade, IVTL: 64% (p<0.001); L: 11% (p<0.001) | NR | NR | |
| Corneal decompensation | NR | IVT: NR; C: n=1 | NR | NR | NR | |
| Cataract surgery | NR | NR | IVTL: 61% (p<0.001); L: 0% | NR | IVT: n=2; L: n=1 | |
| Vitreous haemorrhage | NR | NR | NR | IVTL: n=1 | ||
| Lens opacity | NR | NR | NR | NR | Significantly greater change in lens opacity in IVT group than in L group (1.9) | |
| Deaths | N=33, unrelated to study treatment | IVT: n=1; C: n=2 | IVTL: n=2; L: n=1 | NR | NR | |
CPL, control plus laser; IOP, intraocular pressure; NR, not reported; IVT, intravitreal triamcinolone; IVTL, intravitreal triamcinolone plus laser; RDL, ranibizumab plus deferred laser; RPL, ranibizumab plus laser; TPL, triamcinoloine plus laser.
Table 16.
Safety data in trials assessing more than one drug
| Ahmadieh31 | ATEMD 2011 (Oliveira Neto et al)56 | DRCR Network 2010 (Elman et al, )21 46 | Lim et al55 | Soheilian et al37 41 | |
|---|---|---|---|---|---|
| Number of patients | |||||
| Ocular adverse events | |||||
| Mild anterior chamber reaction | IVB: 19.5% (n=8 eyes), resolved after 1 week of no treatment; IVB/IVT: 18.9% (n=7 eyes), resolved after 1 week of no treatment | NR | NR | NR | IVB: 20% (n=10 eyes), resolved after 1 week; IVB/IVT: 18% (n=9 eyes), resolved after 1 week |
| Marked anterior chamber reaction | IVB: n=1 (topical corticosteroid and cycloplegic drops) | NR | NR | NR | IVB: n=1 (topical corticosteroids and cycloplegic drops); |
| Progression of fibrous proliferation | IVB: n=1 with no sign of retinal traction | NR | NR | NR | IVB: n=1 with no sign of retinal traction; |
| Vitreous haemorrhage | IVB/IVT: n=1 after third injection (excluded from study) | NR | NR | NR | NR |
| IOP rise | IVB: 23, 22 and 28 mm Hg at 6, 12 and 18 weeks (anti-glaucoma drops) | NR | IOP elevation more frequent with triamcinolone + PL | IVB/IVT: 8.3% IVT: 10.8% |
NR |
| IOP ≥10 mm Hg from baseline | NR | NR | CPL: n=16; RPL: n=10; RDL: n=5; TPL: n=70 | NR | NR |
| IOP ≥30 mm Hg from baseline | NR | NR | CPL: n=3; RPL: n=2; RDL: n=4; TPL: n=46 | NR | NR |
| Initiation of IOP lowering treatment at any visit | NR | NR | CPL: n=9; RPL: n=5; RDL: n=4; TPL: n=41 | NR | NR |
| Iris neovascularisation | None | NR | NR | NR | NR |
| Lens opactiy | None | NR | NR | NR | Severe lens opacity IVB/IVT: n=4 eyes; MPC: n=1 eye |
| Endophthalmitis | NR | NR | CPL: n=1; RPL: n=1; RDL: n=1; TPL: n=0 | NR | None |
| Pseudoendophthalmitis | NR | NR | CPL: n=1; RPL: n=0; RDL: n=0; TPL: n=1 | NR | NR |
| Ocular vascular event | NR | NR | CPL: n=1; RPL: n=1; RDL: n=0; TPL: n=2 | NR | NR |
| Retinal detachment | NR | NR | CPL: n=0; RPL: n=0; RDL: n=1; TPL: n=0 | NR | None |
| Vitrectomy | NR | NR | CPL: n=7; RPL: n=0; RDL: n=3; TPL: n=0 | NR | NR |
| Vitreous haemorrhage | NR | NR | CPL: n=15; RPL: n=3; RDL: n=4; TPL: n=2 | NR | None |
| Cataract surgery | NR | NR | CPL: n=11 (of those phakic at baseline); RPL: n=6 (of those phakic at baseline); RDL: n=8 (of those phakic at baseline); TPL: n=19 (of those phakic at baseline) | NR | NR |
| Glaucoma surgery | NR | NR | NR | NR | NR |
| Retinal neovascularisation | NR | NR | NR | NR | IVB: n=4 (all resolved); MPC: n=3 eyes (2 resolved) |
| Development of early PDR | NR | NR | NR | NR | IVB: n=1; IVB/IVT: n=4; MPC: n=3 |
| Progression to high-risk PDR | NR | NR | NR | NR | IVB: n=4; IVB/IVT: n=3; MP: n=3 |
| Ocular hypertension (≥23 mm HG) | NR | NR | NR | NR | IVB/IVT: 16% (n=8 of eyes), controlled medically in all except 1 that progressed to neovascular glaucoma |
| Systemic adverse events | |||||
| Acute myocardial infarction | N=1, considered not to be related to the study drug | No specific systemic adverse events that could be attributed to chance | No significant blood pressure increase, no thromboembolic events | ||
| Deaths | C: n=1 | N=1, considered not to be related to the study drug | CPL: n=8; RPL: n=5; RDL: n=3; TPL: n=2 | IVB/IVT: n=2; MPC: n=2 | |
C, control; CPL, control plus laser; DMO, diabetic macular oedema; IOP, intraocular pressure; IVB, intravitreal bevacizumab; IVR, intravitreal ranibizumab; IVRL, intravitreal ranibizumab plus laser; IVT, intravitreal triamcinolone; L, laser; NR, not reported; PDR, proliferative diabetic retinopathy; RDL, ranibizumab plus deferred laser; RPL, ranibizumab plus laser; TPL, triamcinoloine plus laser.
Study quality
The quality of the included studies was, in general, good as is shown in table 2. (Note that the meeting abstracts were not quality assessed, owing to the lack of details reported on the methods.) Most studies adequately described sequence generation, except in three studies where it was unclear.28–30 However, allocation concealment was poorly described throughout, with only eight reports addressing this issue appropriately.31–38 Reporting of masking also varied. A number of studies masked patients using sham injection or sham laser.21 24 29 31 33 36 38 39 40 Various studies reported that masking of patients was impossible. Assessors, where reported, were masked. In two studies, incomplete outcomes were not addressed.31 41 Baseline characteristics were consistent within study treatment arms. Administration of laser followed the ETDRS protocol, or a modified version, in all studies that described laser administration.21–24 28 30 33 34 42 43 Two studies, both available only as meeting abstracts, did not report the laser administration details.44 45
Table 2.
Study quality
| Study (author and year) | Adequate sequence generation | Allocation concealment | Masking | Incomplete outcome data addressed | Free of selective reporting | Free of other bias (eg, similarity at baseline, power assessment) | Funder |
|---|---|---|---|---|---|---|---|
| Anti-VEGFs | |||||||
| Ranibizumab | |||||||
| READ-2 Study28 47 | Unclear | Unclear | Unclear | Yes (91.3% completion) | Yes | Comparison groups similar at baseline; power analysis not mentioned | Juvenile Diabetes Research Foundation, Genentech Inc |
| RESOLVE Study (Massin et al)36 | Yes | Yes | Yes (patients and outcome assessors) | Yes (82% completion in sham arm, 90.2% with ranibizumab) | Yes | Comparison groups similar at baseline; power analysis unclear | Novartis Pharma, Switzerland |
| RESTORE Study (Mitchell et al)24 | Yes | Unclear | Yes (patients, outcome assessors) | Yes (87.3–88.3% completion) | Yes | Comparison groups similar at baseline; power analysis carried out (power adequate for VA changes) | Novartis Pharma, Switzerland |
| RISE and RIDE (Nguyen et al)38 | Yes | Yes | Yes (patients, treating physician masked to assigned dose of ranibizumab) | Yes (2 year study completed by 83.3% of patients in RISE and by 84.6% in RIDE) | Yes | Comparison groups similar at baseline; ITT analysis; power analysis carried out (power adequate for primary endpoint) | Genentech Inc |
| Bevacizumab | |||||||
| BOLT Study (Michaelides et al)23 52 | Yes | Unclear | Partial (outcome assessors, not patients) | Yes (97.5% completion) | Yes | Comparison groups similar at baseline (except laser group had longer duration of clinically significant DMO); power analysis carried out (power adequate for VA changes) | Moorfields Special Trustees, National Institute for Health Research |
| Faghihi et al53 | Yes | Unclear | Yes (patient | Yes (100% completion) | Yes | Comparable groups at baseline | Not specified |
| Lam et al35 | Yes | Yes | Yes (patients and technicians assessing BCVA, OCT and IOP) | Yes (92.3% follow-up at 6 months) | Yes | Comparison groups similar at baseline; power analysis carried out (power adequate for CMT changes) | Supported in part by the Action for Vision Eye Foundation Hong Kong (charity) |
| Pegaptanib | |||||||
| Cunningham et al/Adamis et al39 57 | Yes | Unclear | Yes (patients and outcome assessors) | Yes (95% completion) | Yes | Comparison groups similar at baseline; acknowledge lack of power to detect differences between doses of pegaptanib | Eyetech Pharmaceuticals Inc, New York, and Pfizer Inc, New York |
| Sultan et al40 | Yes | Unclear | Yes (patients and outcome assessors) | Yes (69.9–73.8% completion) | Yes | Comparison groups similar at baseline; power analysis carried out (power adequate for VA changes) | Pfizer Inc, New York |
| Aflibercept | |||||||
| Da Vinci et al30 58 | Unclear (predetermined randomisation scheme) | Unclear | Yes (patients) | Yes (85% completion) | Yes | Comparison groups similar at baseline, power calculation completed | Regeneron Pharmaceuticals, Inc, New York |
| Steroids | |||||||
| Dexamethasone | |||||||
| Haller et al59 | Yes | Unclear | Yes (patients to dexamethasone dose, outcome assessors) | Yes (92% completion) | Yes | Comparison groups similar at baseline; power analysis carried out, but study not powered to detect differences in subgroups | Oculex Pharmaceuticals Inc |
| Fluocinolone | |||||||
| FAME Study (Campochiaro et al)29 60 | Unclear | Unclear | Partial (patients, masking of outcome assessment not mentioned) | Yes (drop-out rate 19.0–22.7%) | Yes | Comparison groups similar at baseline; power analysis not mentioned | Alimera Sciences Inc, Atlanta, Georgia; Psivida Inc, Watertown, Massachusetts |
| Pearson et al43 | Yes | Unclear | Third party masked design (patient and investigator not masked) | No losses to follow-up | Yes | Demographic characteristics were similar between implant and SOC groups; power calculation done, study adequately powered | Bausch & Lomb Inc, Rochester, New York |
| Triamcinolone | |||||||
| DRCR Network 2008 22 61 63 64 | Yes | Unclear | Partial (patients to triamcinolone dose, outcome assessors not formally masked but generally not aware of participant’s study group) | Yes (81–86% completion) | Yes | Comparison groups similar at baseline; power analysis carried out (power adequate for VA changes) | Cooperative agreement from the National Eye Institute, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Department of Health and Human Services |
| Gillies et alSutter et al32 136–138 | Yes | Yes | Yes (patients, outcome assessors) | Yes (91% completion intervention, 83% control) | Yes | Comparison groups similar at baseline (but limited demographic data); power analysis carried out (power adequate for VA changes) | Sydney Eye Hospital Foundation and Juvenile Diabetes Research Foundation, New York |
| Gillies et al33 | Yes | Yes | Yes (patients, outcome assessors) | Yes (84.5% completion) | Yes | Power analysis carried out (power adequate for VA changes) | National Health and Medical Research Council, Canberra, Australia, and the Sydney Eye Hospital Foundation Sydney, Australia |
| Lam et al34 | Yes | Yes | Partial (outcome assessors) | No losses to follow-up | Yes | Comparison groups similar at baseline; power analysis carried out (power adequate for CMT changes) | Action for Vision Foundation, Hong Kong |
| Ockrim et al/Sivaprasad et al42 62 | Yes | Unclear | Unclear | Yes (94% completion) | Yes | Comparison groups similar at baseline; power analysis carried out (power adequate for VA changes) | Special Trustees of Moorfields Eye Hospital |
| Active comparator trials | |||||||
| Ahmadieh et al31 | Yes | Yes | Yes (patients and outcome assessors) | Unclear | Yes | CMT lower in control group at baseline (p<0.05), other baseline values similar; power analysis carried out (power adequate for CMT changes) | Not reported |
| DRCR Network 21 46 | Yes | Unclear | Yes (patients, except deferred laser group; outcome assessors); masking discontinued after the first year | Yes (1 year completion for 91–95% of eyes) | Yes | Comparison groups similar at baseline; power analysis carried out (power adequate for VA changes) | Cooperative agreement from the National Eye Institute, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health and Human Services; Ranibizumab provided by Genentech, triamcinolone provided by Allergan Inc; companies also provided funds to defray the study's clinical site costs |
| Lim et al55 | Yes | Unclear | Yes (investigators only) | Yes (7.5% drop out after enrolment) | Yes | Groups similar at baseline. The bevacizumab group received more injections | Not reported |
| Soheilian et al37 41 | Yes | Yes | Yes (patients and outcome assessors) | Unclear (36 week completion for 76–88%) | Yes | CMT significantly lower and VA significantly better in MPC group at baseline, other baseline values similar; power analysis carried out (power adequate for VA changes) | Ophthalmic Research Centre, Labbafinejad Medical Center, Tehran |
MPC, macular photocoagulation.
Intravitreal anti-VEGFs
The characteristics of all published studies including design, inclusion/exclusion criteria, intervention, outcomes and their timing are shown in tables 3–8. Safety data for each drug are shown in tables 9–16.
Ranibizumab
Nine RCTs have evaluated ranibizumab as a potential new treatment for patients with DMO (tables 3 and 8); seven were sponsored by industry, and two were led by independent investigators)(table 7).21 46 READ-2 was the first large RCT (n=126).28 47 It compared ranibizumab (0.5 mg) alone, and ranibizumab in combination with laser and laser alone. At 6 months, BCVA had improved significantly in the ranibizumab alone group compared with laser alone or ranibizumab plus laser. Addition of laser to ranibizumab did not provide additional BCVA gain. REVEAL (n=396) compared ranibizumab (0.5 mg) with ranibizumab plus laser and laser alone.48 At 12 months, both ranibizumab arms resulted in a statistically significantly better improvement in BCVA compared to laser alone. The addition of laser did not confer further benefit.
Within the past 2 years, the results of RESOLVE,36 RESTORE24 and RISE and RIDE38 have been published in peer-reviewed journals. RESTORE (n=345) randomised similar groups as the READ-2 study (ranibizumab (0.5 mg) alone, laser alone and ranibizumab plus laser); outcomes were evaluated at 12 months. Ranibizumab improved mean BCVA, with laser providing no additional benefit. Two-year extended follow-up suggested that these results continued.49 RESOLVE (n=151) compared two doses of ranibizumab (0.3 and 0.5 mg) with sham injection. The greatest improvement in BCVA at 12 months was in the 0.3 mg group (11.8 letter gain) compared to the 0.5 mg group (8.8 letter gain) or sham injection (1.4 letter loss). In this study, rescue laser was allowed after 3 months of treatment, if BCVA had decreased by 10 letters or more, or if the investigator considered the macula not to be flat as assessed by OCT. Only 4.9% of the ranibizumab group required rescue laser, compared with 34.7% in the sham injection group.
READ-2 and RESTORE were suitable for pooling through meta-analysis and, when doing so, it was found that ranibizumab statistically significantly improved mean BCVA compared with laser (figure 2). In regard to the proportion of patients gaining more than or equal to 15 letters, individual trials showed a statistically significant difference between laser and ranibizumab but when these two trials were pooled using a random effects model, the result was no longer statistically significant. When a fixed effects model was used, the result was statistically significant (figure not shown). Adding laser to ranibizumab did not add any significant benefit (figure 3). In fact, the mean change in BCVA and the proportion of patients with more than 15 letter gain favoured, although not statistically significantly so, ranibizumab alone compared with ranibizumab plus laser. This was probably a chance effect.
Figure 2.
Ranibizumab 0.5 mg alone versus laser alone. (A) Mean change in best corrected visual acuity. (B) Proportion with >15 letter gain. (C) central macular thickness.
Figure 3.
Ranibizumab 0.5 mg plus laser versus ranibizumab 0.5 mg alone. (A) Mean change in best corrected visual acuity. (B) Proportion with >15 letter gain. (C) central macular thickness.
RISE (n=377) and RIDE (n=382) were identical in design. The study arms are similar to those in the RESOLVE study, 0.3 or 0.5 mg ranibizumab compared with sham. In the RISE study, the proportion of patients with 15 or more letter gain was greatest in the 0.3 mg group at 24 months, whereas in the RIDE study this was greatest in the 0.5 mg group. In the DRCRN trial (n=854), Elman and colleagues compared ranibizumab (0.5 mg) plus prompt (within 3–10 days post ranibizumab) or deferred (≥24 weeks) laser with sham injection plus prompt laser, or triamcinolone (4 mg, Trivaris) plus prompt laser (table 8). At 1 year, both ranibizumab groups reported greater gains in mean BCVA change than triamcinolone or laser alone. Interestingly, at 2 years (n=628), the proportion of patients with 10 or more letter gain was not statistically significantly different between ranibizumab plus prompt laser and laser alone groups, but was statistically significant in the ranibizumab plus deferred laser compared with laser alone comparison. The reason for this is not clear.
READ-3 (n=152) has been published in abstract form and compared monthly injections of intravitreal ranibizumab high dose (2.0 mg) and low dose (0.5 mg).50 At 6 months, there was no statistically significant difference in BCVA between groups.
One study (n=63), published in abstract form, was identified which directly compared monthly injections of ranibizumab (0.5 mg) with bevacizumab (1.5 mg).51 At 48 weeks, the authors found no statistically significant difference between bevacizumab and ranibizumab.
RESTORE, READ-2 and DRCRN (12 month data used) were suitable for pooling through meta-analysis to compare ranibizumab plus laser and laser alone (figure 4). Ranibizumab plus laser resulted in a statistically significantly greater change in mean BCVA, proportion of patients with more than 15 letter gain and CMT reduction versus laser alone.
Figure 4.
Ranibizumab 0.5 mg plus laser versus laser alone. (A) Mean change in best corrected visual acuity. (B) Proportion with >15 letter gain. (C) Central macular thickness.
Adverse events are shown in tables 9 and 16. Conjunctival haemorrhages were higher in the ranibizumab arms compared with laser (RESTORE) or no treatment (RESOLVE). In the RESOLVE, RISE and RIDE studies, a considerably higher incidence of intraocular pressure (IOP) increase was reported in the ranibizumab arm compared to control. This increase in IOP was not demonstrated in the RESTORE study. There were no consistent differences in systemic adverse events between ranibizumab and laser or placebo.
Bevacizumab
Eight RCTs investigating the use of bevacizumab in DMO were identified (tables 4 and 8). One RCT, the BOLT study (n=80), randomised patients to laser therapy or 1.25 mg intravitreal bevacizumab.23 52 At 24 months, the mean changes in BCVA and the proportion of patients who gained 10 ETDRS letters or more was statistically significantly higher in the bevacizumab arm than in the laser arm. Faghihi et al53 (n=80) compared 1.25 mg bevacizumab (average 2.23 injections per patient) with 1.25 mg bevacizumab plus a single laser treatment (average 2.49 injections per patient). After 6 months, the authors found both treatments to be effective at improving BCVA, but neither treatment was found to result in a greater benefit.
Lam et al35 (n=52) compared two doses of bevacizumab (1.25 and 2.5 mg) in patients with diffuse DMO. Patients with focal DMO associated with localised retinal thickening were excluded. At 6 months, following 3 initial monthly injections (no treatment in the remaining 3 months), both groups showed a statistically significantly increased mean BCVA compared with baseline vision, but there was no difference between doses.
Four trials have investigated the combination of bevacizumab and triamcinolone. Ahmadieh et al31 (n=115) compared combined bevacizumab (three 1.25 mg injections at 6 week intervals) plus triamcinolone (2 mg baseline injection only, Triamhexal) with bevacizumab alone (three 1.25 mg at 6 week intervals) and sham injection in patients who had DMO unresponsive (definition not reported) to previous laser (last session more than 3 months previously). The combination arm and bevacizumab alone arm improved mean BCVA more than the sham injection. For BCVA, the combination of bevacizumab plus triamcinolone was non-statistically significantly better than bevacizumab alone.
Soheilian et al37 41 (n=150) compared combined bevacizumab (1.25 mg) plus triamcinolone (2 mg) with bevacizumab alone and laser alone in patients who were laser naïve. At 36 weeks, bevacizumab alone improved BCVA more than either combination therapy or laser, although the difference was not statistically significant. Extended follow-up at 24 months showed that there was no statistically significant difference between groups for BCVA; however, the direction of effect favours the bevacizumab and combination arms more than the laser.54
Lim et al55 (n=111) also evaluated the combination of bevacizumab plus triamcinolone when compared with bevacizumab alone or triamacinolone alone. At 12 months, the authors found no statistically significant difference between groups for BCVA or CMT.
The Efficacy Study of Triamcinolone and Bevacizumab Intravitreal for Treatment of Diabetic Macular Oedema (ATEMD) study, currently only published in abstract form, compared combined therapy with bevacizumab (1.25 mg) and triamcinolone (4 mg) with each of these alone.56 At 6 months, they found no statistically significant difference between groups. One study comparing bevacizumab with ranibizumab is discussed above.51 No bevacizumab trials were suitable for meta-analysis because treatment arms were not comparable among included studies.
Adverse events are shown in tables 10 and 16.There was a low frequency of adverse events reported in the included trials. A higher incidence of mild anterior chamber reaction was reported in bevacizumab groups compared with controls. The incidence of IOP increase was comparable between bevacizumab and laser. Soheilian et al37 41 were the only authors to report the incidence of lens opacity. No patients in the bevacizumab alone group were found to have lens opacities but in four patients (8%) in the bevacizumab plus triamcinolone group, this finding was observed over the 36-week follow-up period.
Pegaptanib
Two studies have evaluated pegaptanib in DMO and both compared it with sham injection (table 5). Cunningham et al39 57 compare three doses of pegaptanib (0.3, 1 and 3 mg) and sham injection in laser-naive patients (n=172). At 6 months, patients in the 0.3 and 1 mg groups performed statistically significantly better than those in either the 3 mg or sham groups. Six injections (median) were administered in the 0.3 and 1 mg groups, whereas only five (median) injections were administered in the 3 mg group.
The second trial (n=260), reported by Sultan and colleagues in 2011, compared pegaptanib (0.3 mg) and sham injection. At 2 years, the pegaptanib group showed a statistically significantly greater improvement in mean BCVA compared with sham.40 However, there was no statistically significant difference in the proportion of patients with an improvement of 10 letters or more. Patients were allowed rescue laser at the assessors’ discretion (25.2% of patients in the pegaptanib group and 45% of patients in the sham group received rescue treatment). In regard to meta-analysis, data were only available to combine these trials for the proportion of patients with more than 15 letter gain. Although neither trial individually demonstrated a statistically significant difference favouring pegaptanib over sham (figure 5), when pooled together in meta-analysis, a statistically significant difference was found in favour of pegaptanib (OR 1.94, 95% CI 1.01 to 3.71).
Figure 5.
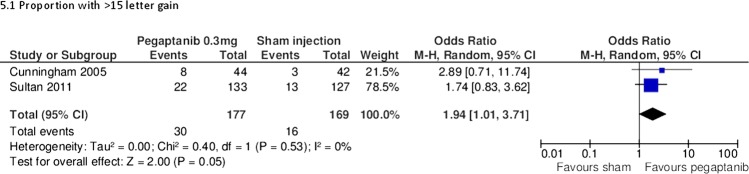
Pegaptanib 0.3 mg versus sham injection. (A) Proportion with >15 letter gain.
Adverse events for pegaptanib are shown in table 11. There was a higher incidence of eye pain compared to control (31% vs 17%).39 57 Cataract formation was similar between the pegaptanib and control groups. There was a higher incidence of IOP increase in the pegaptanib arm compared to control (17.4% vs 6.3%).40
Other anti-VEGF
Aflibercept has been evaluated in the Da Vinci study (n=219)30 58 (table 5). Four regimens of aflibercept (0.5 mg 4 weekly, 2 mg 4 weekly, 2 mg monthly for 3 months, then every 8 weeks, and 2 mg monthly for 3 months followed by treatment as required) were compared with laser. At 6 months, all aflibercept arms had a statistically better BCVA and CMT change than the laser arm. The regimen that resulted in the greatest BCVA gain and CMT reduction was 2 mg every 4 weeks; however, statistical significance between aflibercept arms was not reported. One year extended follow-up showed that all aflibercept arms were found to have a statistically significantly better BCVA compared to laser.58
Adverse events are shown in table 12. There was a higher incidence of IOP increase and eye pain in the aflibercept group compared with laser. Other adverse events were too infrequent to draw meaningful conclusions. The incidence of cataracts was not reported.
Steroids
Dexamethasone
Two included trials assessed the use of dexamethasone to treat DMO (table 6): Haller 2010 (full text available)59 and Callanan (available to date only in an abstract form).44 Haller 2010 (n=171) compared two doses of dexamethasone, administered as an intravitreal implant (350 and 700 µm) through a 20-gauge transscleral incision, with no treatment. At 90 days only, the 700 µm group showed a statistically significantly higher proportion of patients with 10 or more letter gain compared to no treatment (33% compared with 12%, p=0.007). The 350 µm group showed a non-statistically significant improvement compared with laser alone (21% compared with 12%). At 180 days, there was no statistically significant difference between either the dexamethasone group or no treatment group. The treatment effect appeared to peak at 3 months.
The second trial, by Callanan and colleagues (n=253), compared dexamethasone (dose not reported) plus laser with laser alone. Although a greater improvement in mean BCVA was seen at 1–9 months in the dexamethasone plus laser group compared with laser alone, there was no statistically significant difference at 12 months. A mean of 1.6 implants were used over the 12 month period.
These trials were not suitable for meta-analysis since one study is only available in abstract form.
Adverse events are shown in table 13. In the 350 and 700 µm groups compared with no treatment, there was a higher incidence of anterior chamber cells (29.1/26.4% compared with 1.8%), anterior chamber flare (27.3/20.8% compared with 8.8%), vitreous haemorrhage (20/22.6% compared with 5.3%) and increased IOP (14.5/9.4% compared with 0%). However, there was no statistically significant difference in cataract formation between groups at 12 months.59 Callanan et al44 reported an increase in IOP in the dexamethasone plus laser group compared with laser alone (20% compared with 1.6%).
Fluocinolone
Two trials assessed fluocinolone implant for DMO (table 6). The FAME study (n=956) compared two doses of fluocinolone (0.2 and 0.5 µg/day) with sham injection in patients with at least one prior laser treatment.29 Approximately 25% of patients in each group had more than one prior laser treatment. At 24 months, both doses of fluocinolone showed a statistically significant improvement in mean BCVA compared to sham. There was a modest difference between fluocinolone groups. Rescue laser was given after the first 6 weeks for persistent oedema and was allowed every 3 months. A range of 35–37% of patients in the fluocinolone group and 59% in the sham injection group required rescue laser. Extended follow-up at 36 months showed that both the fluocinolone arms continued to result in a statistically significant benefit compared with sham.60
Pearson et al43 (n=196) compared fluocinolone (0.59 mg) with standard of care, either laser or no treatment. At 3 years, there was no statistically significant difference in the proportion of patients with 15 letter gain or more (31% fluocinolone compared with 20% standard of care) between groups and the proportion of patients losing 15 letters or more in the fluocinolone group (17% compared with 14%). Increased incidence of cataracts may have contributed to this difference.
These trials were not suitable for meta-analysis.
Adverse events are shown in table 14. Pearson and colleagues reported a higher incidence of cataracts at 3 years in the fluocinolone group compared with standard of care (55.9% compared with 21.7%). In the extended report of the FAME study, there was a considerably higher incidence of cataract surgery in phakic eyes in the 0.2 and 0.5 µg/day fluocinolone groups (80% and 87.2% compared with 27.3%) and increased IOP at any point (37% and 46% compared with 12%).
Following the demonstration in the FAME trial that a lower dose was about as good as higher ones, the higher doses are unlikely to be used.
Triamcinolone
Ten trials evaluating triamcinolone were identified (tables 7 and 8). All trials evaluated intravitreal administration of triamcinolone, but there were no trials evaluating posterior or anterior subtenon injections. Two trials used Trivaris,21 61 two trials used Kenacort,32 33 one trial used Kenalog,62 one trial used Trimahexal31 and four trials did not report the type of triamcinolone used.34 37,45 56 Three doses were assessed in the included studies (1, 4 and 8 mg) and triamcinolone has been combined with laser or bevacizumab.
Ip and colleagues (n=840) were the only authors to evaluate triamcinolone 1 mg (Trivaris).22 61 63 64 They found a statistically significant improvement in mean BCVA at 2 years in the laser group compared with the triamcinolone group and no significant difference between 1 compared with 4 mg.
Several trials compared 4 mg intravitreal triamcinolone. Ip and colleagues (n=840) found that laser therapy resulted in a greater improvement in mean BCVA at 2 years compared to 4 mg triamcinolone (Trivaris).22 61 63 64 Lam et al34 (n=111) found no statistically significant difference between laser and triamcinolone at 6 months (triamcinolone type not reported). When these two trials were pooled through meta-analysis, the treatment effect favoured laser but the differences were not statistically significant (figure 6). Ockrim et al62 (n=88) compared 4 mg intravitreal triamcinolone (Kenalog) with laser alone. At 12 months, they found no statistically significant BCVA improvement between the triamcinolone and laser groups. Gillies et al32 (n=69) compared 4 mg of triamcinolone (Kenacort) with sham injection. Mean BCVA improved statistically significantly with triamcinolone at 24 months compared with sham injection (3.1 letter gain compared with 2.9 letter loss, p=0.01).
Figure 6.
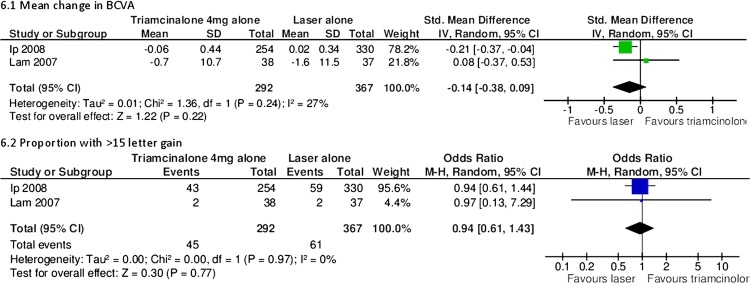
Triamcinolone 4 mg versus laser alone. (A) Mean change in best corrected visual acuity. (B) Proportion with >15 letter gain.
Lam et al34 (n=111) compared triamcinolone 4 mg alone with 4 mg of triamcinolone plus laser or laser alone. At 6 months, the authors found no difference in BCVA between any of the groups. Elman et al21 (n=854) compared 4 mg of triamcinolone (Trivaris) plus laser with ranibizumab plus prompt (within 3–10 days) or deferred (more than 24 week) laser and laser alone. At 2 years, they found a statistically significant difference in mean BCVA between ranibizumab plus prompt/deferred laser compared with laser alone (7 letter gain/9 letter gain compared with 3 letter gain), but no difference with triamcinolone plus laser compared with laser alone (2 letter gain compared with 3 letter gain). Neto et al56 (n=120) compared 4 mg triamcinolone alone (triamcinolone type not reported) with 4 plus 1.25 mg bevacizumab. At 6 months, they found no statistically significant difference between groups.
The Elman and Lam studies were suitable for meta-analysis, which showed non-statistically significant improvements in mean BCVA and the proportions of patients with more or equal than 15 letter gain in the triamcinolone plus laser group compared with laser alone (figure 7).
Figure 7.
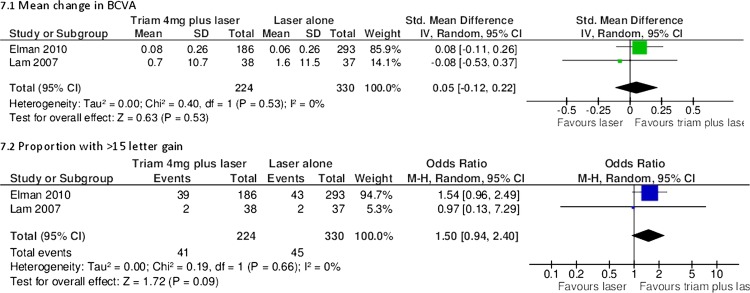
Triamcinolone 4 mg plus laser versus laser alone. (A) Mean change in best corrected visual acuity. (B) Proportion with >15 letter gain.
Adverse events are shown in tables 15 and 16. Triamcinolone was associated with consistently higher incidences of IOP increase and cataracts. Gilles and colleagues reported a cataract rate of over 50% by 3 years in patients treated with triamcinolone.
Other pertinent studies
Only one study in abstract form directly compared bevacizumab with ranibizumab.51 Bevacizumab and ranibizumab have been compared through an indirect comparison of five trials.65 There was no evidence of a difference between the drugs; however, wide credible intervals meant that the superiority of either drug could not be excluded.
Two-year results of the CATT (Comparison of AMD Treatment Trials) and 1 year results of the IVAN (Inhibit VEGF in Age-related choroidal Neovascularisation), recently published, have demonstrated a good safety profile of anti-VEGF therapies when used to treat patients with age-related macular degeneration.66 67 The CATT study randomised 1208 patients with AMD to monthly or as required injection of either ranibizumab or bevacizumab. At 1 year, the mean BCVA was similar in both groups (8 letter gain in bevacizumab and 8.5 in ranibizumab). Over 2 years, the rates of deaths, myocardial infarction and stroke did not differ between the ranibizumab and bevacizumab treatment groups. However, there was a higher rate of serious adverse events in the bevacizumab group compared with the ranibizumab group. This increased event rate was driven mainly by hospitalisations (RR 1.29, 95% CI 1.01 to 1.66). However, the hospitalisations were not caused by known adverse events of bevacizumab. Arteriothrombotic events and heart failure occurred in less than 2% of participants in the IVAN, and they were more often observed in the ranibizumab group than in the bevacizumab group (p=0.03). Further data from other ongoing clinical trials may provide more insight on the safety or anti-VEGF treatment and possible differences on this respect among available drugs.
Campbell et al68 conducted a population-based nested case–control study of 91 378 older adults with a history of physician-diagnosed retinal disease. The authors found that neither ranibizumab nor bevacizumab was associated with significant risks of ischaemic stroke, acute myocardial infarction, congestive heart failure or venous thromboembolism.
A recent systematic review specifically assessing adverse events in anti-VEGF drugs found a low incidence of serious (below 1 in 100) and non-serious ocular events (below 1 in 500) from ranibizumab, bevacizumab and pegaptanib.69
Fung et al70 used an internet-based survey of clinicians to assess the safety of bevacizumab. The survey covered over 5000 patients and found that bevacizumab was associated with an infrequent incidence of adverse events (all less than 0.21%).
One study, which assessed diclofenac, did not meet the inclusion criteria (follow-up for only 12 weeks).71 The authors randomised 32 patients to either intravitreal diclofenac or triamcinolone and found that both diclofenac and triamcinolone reduced CMT, but a statistically significant visual improvement was observed only in the triamcinolone group.
Sfikakis et al72 undertook a 30-week randomised crossover trial comparing infliximab and placebo. The study failed to meet our inclusion criteria (only 11 patients included). The authors found that infliximab resulted in a 28.6% improvement in vision compared with 4.3% with placebo. The improvement seen with placebo could be due to a ‘carry over effect’, seen in cross-over trials.
The Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) trial was primarily a study to see if the lipid-lowering agent fenofibrate could reduce macrovascular and microvascular events in type 2 diabetes.73 However, a substudy within FIELD recruited 1012 patients to a retinopathy study. The primary outcome in the main study was need for laser therapy (3.4% on fenofibrate vs 4.9% on placebo), but the substudy used retinal photography to assess progression of retinopathy or development of macular oedema. The HR at 6 years for DMO was 0.69 (95% CI 0.54 to 0.87) in the fenofibrate group compared to placebo.
Ruboxistaurin is another oral agent which has been assessed for the treatment of DMO. Aiello and colleagues randomised 686 patients to receive placebo or one of three doses of ruboxistaurin.74 75 There was no statistically significant difference in delay to sight-threatening DMO in any ruboxistaurin group compared to placebo. The authors suggest that differences in laser treatment between groups may have contributed to the non-significant finding.
Assessment of heterogeneity within meta-analysis
Heterogeneity was assessed methodologically and statistically. Methodological heterogeneity was assessed by comparing the study population, interventions, outcome measures and follow-up. Studies that were not methodologically comparable were excluded from the meta-analysis. For example, bevacizumab trials were not pooled because Soheilian et al37 included patients who were laser naïve and Ahmadieh et al31 included patients who were unresponsive to laser. Some analyses were also excluded because sufficient details were not reported in the studies. For example, several studies failed to report SDs.35 39
Statistical heterogeneity was assessed through I2 scores. High statistical heterogeneity was found in two analyses (2.3 and 4.3). Therefore, these results should be interpreted with due caution. Moderate heterogeneity was found in three analyses (2.2, 3.1 and 3.2). Low heterogeneity was found in the remaining eight analyses.
Ongoing trials
There are numerous ongoing studies listed in appendix 2. The most salient studies include a study to compare ranibizumab and bevacizumab (Schmidt-Erfurth), a study investigating rescue ranibizumab treatment for patients who have failed on bevacizumab (Chaudhry), a study evaluating two algorithms for ranibizumab, ‘treat and extend’ and ‘as required’ (RETAIN), further studies of Trap-eye (VIVID and VISTA) and trials which are examining the use of NSAIDs, such as diclofenac and nepafenac (NEVANAC and Soheilian).
Discussion
It appears that anti-VEGF treatment is effective in DMO, especially ranibizumab and bevacizumab. Meta-analysis of available short-term data (up to 2 years) suggests that ranibizumab is superior to laser and that adding laser to ranibizumab treatment does not confer additional benefit. Steroid treatment has demonstrated mixed success and, almost uniformly, increased the incidence of cataracts and IOP. The licence for fluocinolone takes note of this and it is positioned as a treatment when others have failed.
Strengths and limitations of the review
There are a number of strengths of this review. A robust systematic review methodology was used. Reliability was improved by excluding trials with small sample sizes or short follow-up. Since a number of trials included similar intervention arms, consistent treatment effects further improve reliability. Validity was improved by assessing the quality of trials using the Cochrane risk of bias tables. Including abstracts from ARVO provided up-to-date results. Pooling results through meta-analysis provided further evidence. The random effects model was used throughout to allow for heterogeneity among studies.
This review, however, has limitations. Although the inclusion of abstracts provides more up-to-date results, the studies contained in these abstracts could not be assessed for risk of bias and should therefore be interpreted with caution. In addition, reporting of quality assessment criteria was variable. Allocation concealment was especially poorly reported. There was only one study which compared different anti-VEGFs51 and none that compared steroids (fluocinolone vs dexamethasone vs triamcinolone). Therefore, it is difficult to assess the effectiveness within drug classes. As with any meta-analysis, questions of heterogeneity arise. Follow-up periods varied among studies. A difference of 6 months was allowed for studies to be pooled for meta-analysis, but this could have still resulted in heterogeneity. High statistical heterogeneity was found in a quarter of the analyses. Furthermore, because of the low number of trials included, publication bias could not be assessed by funnel plot analysis. The manufacturers funded most of the trials for ranibizumab, pegaptanib, dexamethasone and fluocinolone, whereas trials for bevacizumab and triamcinolone were generally funded by non-pharmaceutical organisations. Generally, the non-commercial studies had smaller numbers, perhaps because of the funding restraints.
It is important to note that there may be differences in laser treatment protocol between studies. This applies to trials which combine drug treatments with laser or include laser as a comparator. All studies referred to the ETDRS protocol19 20 or a modified version of it. In the ETDRS, once a diagnosis of clinically significant macular oedema was made, an angiogram was obtained to identified ‘treatable lesions’. ‘Treatable lesions’ included discrete points of retinal hyperfluorescence or leakage (most of these are often microaneurysms), areas of diffuse leakage within the retina related to microaneurysms, intraretinal microvascular abnormalities, diffusely leaking retinal capillary bed and retinal avascular zones. In the ETDRS protocol, treatment of lesions closer than 500 microns from the centre of the macula was not required initially; however, if vision was less than 20/40 and the oedema and leakage persisted, treatment up to 300 microns from the centre of the macula was recommended unless there was capillary dropout; in the latter case, treatment was not recommended as it may lead to further loss of perifoveal capillaries.
However, in routine clinical practice, clinicians generally use lighter and less intense treatment than specified in the ETDRS protocol.76 In addition, some centres do not use fluorescein angiography (unlike the ETDRS study19) to guide treatment. The exact adherence to the ETDRS protocol within studies is unclear. For example, in the BOLT study, a modified ETDRS protocol was used. One of the aims of the protocol was ‘not darkening/whitening of microaneurysms’, which is not consistent with the ETDRS protocol.
Interpretation of the results
The anti-VEGF drugs appear to be clinically effective in treating DMO in short-term studies (up to 2 years). Ranibizumab has the most robust evidence base and has shown superiority compared to laser and sham injection in all trials and meta-analyses, except for the proportion of patients with 10 or more letter gain in the DRCR.net study published by Elman et al46 at 2 years follow-up. Adding laser to ranibizumab conferred no benefit. Bevacizumab has also been shown to be superior to laser. Three doses have been used (1.25, 1.5 and 2.5). The higher dose does not appear to add further benefit, and most studies in the literature use 1.25 mg. The addition of triamcinolone to bevacizumab did not provide further benefits. Pegaptanib has only been compared to sham injection. Mean change in BCVA favoured pegaptanib, but only through meta-analysis did the proportion of patients with more than 15 letter gain favour pegaptanib. Further published data are required before drawing conclusions on aflibercept. However, although the anti-VEGF drugs are a significant advance, they fail to improve BCVA by 10 or more letters in half or more patients, and so they do not provide a complete answer to DMO.
Steroid treatments have inconsistent results and are undoubtedly associated with increased IOP and cataract. The effects of dexamethasone appear to peak at 3 months. At 6 months, there was no significant difference compared with laser. This might imply that earlier retreatment is needed if the beneficial effect is to be maintained, but increasing the number of treatments would very likely increase the associated complications, especially with the relatively large needle size. The addition of laser did not appear to add further benefit. There was no significant difference in cataract formation at 6 months with dexamethasone compared to observation, but it is likely that a higher incidence of cataracts would be seen with longer follow-up. Significantly more patients suffered increased IOP in the dexamethasone group compared with observation. Fluocinolone has been shown to be effective compared with sham injection (FAME);29 60 however, when compared to standard of care (laser or observation at clinician's discretion), there was no significant difference in the proportion of patients with a 15 letter or more gain. Both studies reported higher incidence of cataract formation in the fluocinolone group, with over 80% at 3 years at the higher dose. Results for triamcinolone are inconsistent. Ip et al61 found that laser was more effective, while others have found no statistically significant difference. Triamcinolone combined with laser, however, seemed to have similar efficacy as ranibizumab combined with laser in pseudophakic eyes.21 46 Triamcinolone is more effective than sham injection. Triamcinolone has consistently been associated with increased incidence of cataract and raised IOP.
Steroids and laser therapy may affect CMT in a different manner from anti-VEGF drugs. For example, when ranibizumab alone is compared with ranibizumab plus laser, it appears to be more effective in terms of mean change in BCVA and proportion of patients with more than 15 letter gain. However, ranibizumab plus laser is more effective at reducing CMT. Furthermore, when triamcinolone plus laser is compared with ranibizumab plus laser, the latter appears to be more effective in terms of change in BCVA and proportion of patients with more than 15 letter gain, but triamcinolone plus laser is more effective at reducing CMT. The reasons for this are unclear. There is a weak correlation between CMT and BCVA. However, the long-term benefits of reducing CMT are currently unknown.
No large observational studies were identified that compared anti-VEGF drugs. Using an internet-based survey, Fung et al70 found the incidence of adverse events in bevacizumab to be low. One small outbreak of sterile endophthalmitis was reported with a single batch of bevacizumab in Canada, emphasising the need for sterility when preparing aliquots.77 Curtis et al78 carried out a very large retrospective cohort study in 146 942 patients aged 65 and over with age-related macular degeneration (AMD). Their aim was to examine cardiovascular outcomes in patients treated with the four options: photodynamic therapy (PDT), pegaptanib, bevacizumab and ranibizumab. The authors reported that one of their comparisons showed an increase in overall mortality and stroke risk with bevacizumab compared to ranibizumab, with HRs of 0.86 (95% CI 0.75 to 0.98) and 0.78 (0.64 to 0.96), respectively. However, owing to the very large cost differences between bevacizumab and ranibizumab, the authors noted that selection bias might be operating, with poorer people (with poorer health) more likely to be treated with bevacizumab. They therefore carried out another analysis using only ophthalmological clinics which used only one drug, to avoid selection bias. This analysis showed no significant difference: overall mortality HR for ranibizumab 1.10 (95% CI 0.85 to 1.141); MI 0.87 (0.53 to 1.14); stroke 0.87 (0.61 to 1.24).
Gower et al79 analysed 77 886 anti-VEGF injections from Medicare data (46% ranibizumab and 54% bevacizumab). Results have only been published in abstract form. The authors found an increased risk of overall mortality and cerebrovascular events in the bevacizumab group (HR 1.11 99% CI 1.01 to 1.23 and 1.57, 1.04 to 2.37, respectively). There was no statistically significantly increased risk in the ranibizumab group. The authors acknowledge that a limitation of the study is a failure to adjust for important confounding factors (such as smoking, hypertension and hyperlipidaemia). Considering the cost difference, it is likely that patients treated with bevacizumab would have been in a lower socioeconomic class and therefore at high risk of mortality and vascular disease.
Implications for clinicians
The anti-VEGF drugs appear to be a significant advance in the treatment of DMO and are regarded now as the treatment of choice for patients affected by this condition. Studies assessing the effectiveness of steroids have reported mixed results. The high rates of cataract and increased IOP are a drawback. Triamcinolone combined with laser may be a good option for pseudophakic patients and may be more cost-effective than treatment with ranibizumab. However, the need for fewer administrations, potentially one every 3 years with fluocinolone, is advantageous. From an administration perspective, some patients might prefer infrequent steroid injections with a sizeable risk of cataract, and a small, but existent, risk of glaucoma, to frequent anti-VEGF injections, even if the potential gain may not be fully comparable. Steroids may also be considered for patients who do not adequately respond to anti-VEGFs. Currently, the role of laser in the treatment of DMO is debatable. Short-term data from available trials have demonstrated the superiority of anti-VEGF with regard to laser treatment but have failed to demonstrate a benefit of combining both treatment approaches. It is possible that some ophthalmologists may still opt to offer laser treatment to patients with very focal areas of leakage.
Currently, there is more evidence for the effectiveness of ranibizumab and bevacizumab than for pegaptanib and VEGF-trap eye. The results of direct head to head trials of ranibizumab and bevacizumab are awaited. Bevacizumab is not licensed for intraocular use but costs considerably less than other forms of therapy. Ranibizumab is licensed and more expensive, but its use is supported by large manufacturer-funded trials demonstrating its clinical effectiveness. In the UK, the General Medical Council recommends that unlicensed medications should only be prescribed if ‘an alternative, licensed medicine would not meet the patient's needs’ and there is ‘a sufficient evidence base and/or experience of using the medication to demonstrate its safety and efficacy’.80 The FDA says that when using a drug ‘off-label’, clinicians ‘have the responsibility to be well informed about the product, to base its use on firm scientific rationale and on sounded medical evidence, and to maintain records of the product’s use and effects’.81 Patients should be fully aware of the use of any unlicensed medication and consent to any safety or efficacy uncertainties.
The place of intravitreal steroids needs consideration now that we have the anti-VEGFs drugs, as does the role of laser. The anti-VEGFs drugs may now be the first-line treatment in place of laser, with laser being used selectively for focal lesions, and in sequence after anti-VEGF therapy once the retinal thickness has been reduced. However, it should be noted that about half of the patients do not get good results with anti-VEGFs. In RESTORE, only 50% of patients had gains in VA of 10 or more letters. So the anti-VEGFs are ‘game-changers’, but their impact should not be overestimated.
In those who do not respond to anti-VEGFs or laser, there remains a place for steroids, despite their high adverse effect rates. The European licence for fluocinolone recognises this, by stating that it should be used when other therapies have not had sufficient effect.82 The commonest adverse effect is cataract, but that is very common in people with diabetes, and many are already pseudophakic when treatment of DMO is required.
Vitreoretinal surgery for the treatment of DMO was not included in our review. Laidlaw reviewed the literature and only found evidence for vitrectomy when there were signs of clinical or OCT traction.83 However, even in these cases, the evidence was not strong.
Implications for policy makers
In the UK, the National Institute of Health and Clinical Excellence (NICE) has recently made the decision not to recommend ranibizumab for the treatment of DMO.84 NICE concluded that ranibizumab, although clinically effective, was not cost-effective compared to laser therapy. Bevacizumab is less than a tenth of the cost of ranibizumab but is unlikely to be licensed. This beckons the question as to whether policy makers should recommend cheaper unlicensed medications over a more expensive licensed alternative when their efficacy and side effects appear to be similar.
Unanswered questions
Several unanswered questions remain. Studies evaluating the effectiveness of ranibizumab compared with bevacizumab are needed. Although the anti-VEGFs are clinically effective and a major step forward in the management of DMO, it has to be noted that they have little effect in a large number of patients. Generally speaking, the proportion of patients who have demonstrated 10 or more letter gain using anti-VEGFs is between 30% to 50% in the trials that demonstrate the greatest effectiveness. Most of these patients would not achieve the 20/40 visual acuity required for driving. More effective treatments, or combinations of treatments, are required.
There is a lack of specific evidence for the use of anti-VEGF drugs or steroids in patients with macular ischaemia secondary to DMO. A number of trials excluded patients with macular ischaemia.23 34 35 40 53 62 The RESTORE trial included patients with macular ischaemia and undertook a subgroup analysis.24 The authors compared patients with (n=34) and without (n=35) macular ischaemia at baseline. They found that those without macular ischaemia responded better to ranibizumab (mean average change in BCVA at 12 months 7.2 letters gain compared with 6.3 letters). Larger trials are needed to assess the use of anti-VEGF drugs and steroids in patients with macular ischaemia.
The duration of treatment is as yet uncertain. Most of the included studies use a retreatment protocol based on clinical need or OCT results. For example, in the BOLT study, patients received a median of nine injections of bevacizumab over 24 months.23 85 However, it is not yet known for how frequent long-term maintenance injections will be needed and whether laser treatment in sequence could potentially reduce the number of anti-VEGF injections required. Other treatment strategies to apply laser, such as using laser power at subthreshold levels, may prove more effective.86 Future trials should use active comparators which are used in routine clinical practice and avoid placebo-controlled trials.
Conclusion
This review evaluated current treatments for DMO. Undoubtedly, the use of anti-VEGFs heralds a new era for patients who suffer from DMO. Currently, the anti-VEGFs ranibizumab and bevacizumab have consistently shown good clinical effectiveness without major unwanted side effects. Steroid results have been mixed and are usually associated with cataract formation and IOP increase. Based on the short-term data available, adding laser therapy to anti-VEGFs does not appear to confer additional benefit.
Despite the current wider spectrum of treatments for DMO, only a small proportion of patients recover good vision (≥20/40), and thus the search for new therapies to prevent and manage DMO needs to be continued.
Supplementary Material
Appendix 1: Methods of the literature search
Searches for clinical trials
Ovid MEDLINE 1948-week 2 July 2012 and Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations 11 July 2012
Diabetic Retinopathy/dt (Drug Therapy)
Macular Edema/dt (Drug Therapy)
(diabet* adj2 macular adj (edema or oedema)).tw.
(diabet* adj2 maculopathy).tw.
(diabet* adj2 retinopathy).tw.
1 or 2 or 3 or 4 or 5
(ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or macugen or aflibercept or vegf trap-eye or steroid* or corticosteroid* or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor*).tw.
exp Vascular Endothelial Growth Factor A/
exp Fluocinolone Acetonide/
exp Triamcinolone/
7 or 8 or 9 or 10
6 and 11
randomised controlled trial.pt.
controlled clinical trial.pt.
(masked or sham or placebo or control group or random*).tw.
13 or 14 or 15
12 and 16
(case reports or editorial or letter or review).pt.
17 not 18
limit 19 to humans
EMBASE 1947–2012 week 27
(ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or macugen or aflibercept or vegf trap-eye or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor*).m_titl.
(diabetic macular edema or diabetic macular oedema or diabetic retinopathy or diabetic maculopathy).m_titl.
1 and 2
random*.tw.
3 and 4
Cochrane Central Register of Controlled Trials, Issue 7 of 12, July 2012
Ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or macugen or aflibercept or vegf trap-eye or steroid* or corticosteroid* or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor* in Record Title and diabetic macular edema or diabetic macular oedema or diabetic retinopathy or diabetic maculopathy in Record Title
Web of Science—with Conference Proceedings (updated 12 July 2012)
Title=(ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or macugen or aflibercept or vegf trap-eye or steroid* or corticosteroid* or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor*) AND Title=(diabetic macular edema or diabetic macular oedema or diabetic retinopathy or diabetic maculopathy) AND Title=(random*)
Searches for systematic reviews
Ovid MEDLINE(R) Daily Update 11 July 2012, Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations 11 July 2012
Diabetic Retinopathy/dt (Drug Therapy)
Macular Edema/dt (Drug Therapy)
(diabet* adj2 macular adj (edema or oedema)).tw.
(diabet* adj2 maculopathy).tw.
(diabet* adj2 retinopathy).tw.
1 or 2 or 3 or 4 or 5
(ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or macugen or aflibercept or vegf trap-eye or steroid* or corticosteroid* or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor*).tw.
exp Vascular Endothelial Growth Factor A/
exp Fluocinolone Acetonide/
exp Triamcinolone/
7 or 8 or 9 or 10
6 and 11
(systematic review or meta-analysis or pubmed or medline).tw.
meta-analysis.pt.
cochrane.af.
13 or 14 or 15
12 and 16
Cochrane Database of Systematic Reviews and Technology Assessments Database, Cochrane Library July Issue, 2012
Ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or macugen or aflibercept or vegf trap-eye or steroid* or corticosteroid* or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor* in Record Title and diabetic macular edema or diabetic macular oedema or diabetic retinopathy or diabetic maculopathy in Record Title
Searches for safety and adverse events
Ovid MEDLINE(R) Daily Update 11 July 2012, Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations 11 July 2012 ; EMBASE 1980–2012 week 27
(ranibizumab or lucentis or bevacizumab or avastin or pegaptanib or aflibercept or vegf trap-eye or macugen or dexamethasone or fluocinolone or triamcinolone or anti-VEGF* or anti-vascular endothelial growth factor*).m_titl.
(diabetic macular edema or diabetic macular oedema or diabetic retinopathy or diabetic maculopathy).m_titl.
1 and 2
(risk or safety or adverse or harm or pharmacovigilance).tw.
(side-effect* or precaution* or warning* or contraindication$ or contra-indication* or tolerability or toxic*).tw.
4 or 5
3 and 6
Searches of the annual meeting abstracts (for trials, reviews and safety studies)
ARVO (Association for Research in Vision and Ophthalmology) (2002–2012)
ADA (American Diabetes Association) (2002–2012)
EASD (European Association for the Study of Diabetes) (2002–2012)
Other searches
Web sites of the following
Drugs@FDA: FDA Approved Drug Products
European Medicines Association
ClinicalTrials.gov
EU Clinical Trials Register
National Institute for Health and Clinical Excellence
Appendix 2: Ongoing Trials in ClinicalTrials.gov
Schmidt-Erfurth and colleagues are comparing ranibizumab and bevacizumab in DME (NCT00545870)
TRIASTIN study is comparing ranibizumab, triamcinolone and sham injection (NCT00682539)
Maturi and colleagues are comparing bevacizumab plus dexamethasone with bevacizumab alone (NCT01309451)
IBeTA study (Jorge and colleagues) is comparing bevacizumab (1.5 mg) plus laser, triamcinolone (4 mg) plus laser with laser alone (NCT00997191)
Chaudhry and colleagues are evaluating ranibizumab in patients who have failed with 3–6 injections of bevacizumab (NCT01253694)
MIDME study (Pfizer) is comparing pegaptanib 0.3 mg with sham injection (NCT01175070)
Figueira and colleagues are comparing pegaptanib plus laser with laser alone (NCT01281098)
RESPOND (Novartis) is comparing ranibizumab (0.5 mg) alone with ranibizumab plus laser or laser alone (NCT01135914)
RETAIN (Novartis) study is comparing two different ranibizumab algorithms; ‘treat and extend’ versus as needed (NCT01171976)
RED-ES (Novartis) is comparing ranibizumab with laser in patients with visual impairment due to DME (NCT00901186)
READ 3 study (Do and colleagues) are comparing two doses of ranibizumab 0.5 and 2 mg (NCT01077401)
VIVID-DME and VISTA DME studies (Bayer) are comparing aflibercept with laser. (NCT01331681 and NCT01363440)
Gillies and colleagues are comparing bevacizumab with dexamethasone (NCT01298076)
Soheilian and colleagues are performing a phase I study looking at the use of diclofenac compared with bevacizumab in DME (NCT00999791)
López-Miranda and colleagues are comparing the use of bevacizumab before and after laser therapy (NCT00804206)
NEVANAC study is comparing triamcinolone alone with triamcinolone plus nepafenac (NSAID) (NCT00780780)
Elman and colleagues are comparing laser alone, laser combined with an intravitreal injection of triamcinolone, laser combined with an intravitreal injection of ranibizumab, or intravitreal injection of ranibizumab alone (NCT00444600)
BRDME (Schlingemann and collagues) study is comparing the use of bevacizumab and ranibizumab in the treatment of patients with DME (OCT central area thickness > 275 μm) (NCT01635790)
Wiley and colleagues are comparing bevacizumab and ranibizumab in patients with DME in at least one eye (NCT01610557)
Protocol T study (Wells and colleagues) is comparing effectiveness of a aflibercept, bevacizumab and ranibizumab for DME (NCT01627249)
Allergan-funded study comparing safety and efficacy of 700 µg dexamethasone implant against 0.5 mg ranibizumab in patients with DME (NCT01492400)
Pfizer-funded study comparing effectiveness of 0.3 mg pegaptanib against sham injection (NCT01100307)
Allergan-funded study comparing safety and efficacy of an intravitreal dexamethasone implant (700 and 350 µg) against sham in patients with DME (NCT00168389)
Allergan-funded study comparing safety and efficacy of an intravitreal dexamethasone implant (700 and 350 µg) against sham in patients with DME (NCT00168337)
Footnotes
Contributors: JAF screened titles, checked data extraction, performed the meta-analysis and drafted the manuscript. NL conceived the idea, interpreted the results and provided clinical expertise throughout. PR performed the literature search, updated the searches, screened the titles and managed the references. CC extracted data from the studies. DS screened the titles and checked the meta-analysis. NW designed the review and supervised the running of the study. All authors contributed to the final draft.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Disclosure: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Data sharing statement: No additional data are available.
Protocol: This review was built upon several technology appraisals for NICE, and therefore no protocol exists.
References
- 1.Holman N, Forouhi NG, Goyder E, et al. The Association of Public Health Observatories (APHO) Diabetes Prevalence Model: estimates of total diabetes prevalence for England, 2010–2030. Diabet Med 2011;28:575–82 [DOI] [PubMed] [Google Scholar]
- 2.Williams R, Airey M, Baxter H, et al. Epidemiology of diabetic retinopathy and macular oedema: a systematic review. Eye (London) 2004;18:963–83 [DOI] [PubMed] [Google Scholar]
- 3.Henricsson M, Sellman A, Tyrberg M, et al. Progression to proliferative retinopathy and macular oedema requiring treatment. Assessment of the alternative classification of the Wisconsin Study. Acta Ophthalmol Scand 1999;77:218–23 [DOI] [PubMed] [Google Scholar]
- 4.Chen E, Looman M, Laouri M, et al. Burden of illness of diabetic macular edema: literature review. Curr Med Res Opin 2010;26:1587–97 [DOI] [PubMed] [Google Scholar]
- 5.Hirai FE, Knudtson MD, Klein BE, et al. Clinically significant macular edema and survival in type 1 and type 2 diabetes. Am J Ophthalmol 2008;145:700–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klein R, Klein BE, Moss SE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XVII. The 14-year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Ophthalmology 1998;105:1801–15 [DOI] [PubMed] [Google Scholar]
- 7.Klein R, Knudtson MD, Lee KE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy XXIII: the twenty-five-year incidence of macular edema in persons with type 1 diabetes. Ophthalmology 2009;116:497–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knudsen LL, Lervang HH, Lundbye-Christensen S, et al. The North Jutland County Diabetic Retinopathy Study (NCDRS) 2. Non-ophthalmic parameters and clinically significant macular oedema. Br J Ophthalmol 2007;91:1593–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas RL, Dunstan F, Luzio SD, et al. Incidence of diabetic retinopathy in people with type 2 diabetes mellitus attending the Diabetic Retinopathy Screening Service for Wales: retrospective analysis. BMJ 2012;344:e874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong TY, Mwamburi M, Klein R, et al. Rates of progression in diabetic retinopathy during different time periods: a systematic review and meta-analysis. Diabetes Care 2009;32:2307–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang ES, Brown SE, Ewigman BG, et al. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care 2007;30:2478–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shea AM, Curtis LH, Hammill BG, et al. Resource use and costs associated with diabetic macular edema in elderly persons. Arch Ophthalmol 2008;126:1748–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Minassian DC, Owens DR, Reidy A. Prevalence of diabetic macular oedema and related health and social care resource use in England. Br J Ophthalmol 2012;96:345–9 [DOI] [PubMed] [Google Scholar]
- 14.Happich M, Reitberger U, Breitscheidel L, et al. The economic burden of diabetic retinopathy in Germany in 2002. Graefes Arch Clin Exp Ophthalmol 2008;246:151–9 [DOI] [PubMed] [Google Scholar]
- 15.Bhagat N, Grigorian RA, Tutela A, et al. Diabetic macular edema: pathogenesis and treatment. Surv Ophthalmol 2009;54:1–32 [DOI] [PubMed] [Google Scholar]
- 16.Murata T, Ishibashi T, Khalil A, et al. Vascular endothelial growth factor plays a role in hyperpermeability of diabetic retinal vessels. Ophthalmic Res 1995;27:48–52 [DOI] [PubMed] [Google Scholar]
- 17.Barile GR, Pachydaki SI, Tari SR, et al. The RAGE axis in early diabetic retinopathy. Invest Ophthalmol Vis Sci 2005;46:2916–24 [DOI] [PubMed] [Google Scholar]
- 18.The Diabetic Retinopathy Study Research Group Preliminary report on effects of photocoagulation therapy. Am J Ophthalmol 1976;81:383–96 [DOI] [PubMed] [Google Scholar]
- 19.Early Treatment Diabetic Retinopathy Study research group Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol 1985;103:1796–806 [PubMed] [Google Scholar]
- 20.Early Treatment Diabetic Retinopathy Study research group Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 2. Ophthalmology 1987;94:761–74 [DOI] [PubMed] [Google Scholar]
- 21.Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2010;117:1064–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ip MS, Bressler SB, Antoszyk AN, et al. A randomized trial comparing intravitreal triamcinolone and focal/grid photocoagulation for diabetic macular edema: baseline features. Retina 2008;28:919–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michaelides M, Kaines A, Hamilton RD, et al. A prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (BOLT study) 12-month data: report 2. Ophthalmology 2010;117:1078–86 [DOI] [PubMed] [Google Scholar]
- 24.Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 2011;118:615–25 [DOI] [PubMed] [Google Scholar]
- 25.Lovestam-Adrian M, Agardh E. Photocoagulation of diabetic macular oedema—complications and visual outcome. Acta Ophthalmol Scand 2000;78:667–71 [DOI] [PubMed] [Google Scholar]
- 26.Lee CM, Olk RJ. Modified grid laser photocoagulation for diffuse diabetic macular edema. Long-term visual results. Ophthalmology 1991;98:1594–602 [DOI] [PubMed] [Google Scholar]
- 27.Nwanze CC, Akinwale A, Adelman RA. Bevacizumab vs. Ranibizumab in preserving or improving vision in patients with wet, age-related macular degeneration: a cost-effectiveness review. Clin Med Insights: Ther 2012;4:29–38 [Google Scholar]
- 28.Nguyen QD, Shah SM, Khwaja AA, et al. Two-year outcomes of the ranibizumab for edema of the mAcula in diabetes (READ-2) study. Ophthalmology 2010;117:2146–51 [DOI] [PubMed] [Google Scholar]
- 29.Campochiaro PA, Brown DM, Pearson A, et al. Long-term benefit of sustained-delivery fluocinolone acetonide vitreous inserts for diabetic macular edema. Ophthalmology 2011;118:626–35 [DOI] [PubMed] [Google Scholar]
- 30.Do DV, Schmidt-Erfurth U, Gonzalez VH, et al. The DA VINCI Study: phase 2 primary results of VEGF Trap-Eye in patients with diabetic macular edema. Ophthalmology 2011;118:1819–26 [DOI] [PubMed] [Google Scholar]
- 31.Ahmadieh H, Ramezani A, Shoeibi N, et al. Intravitreal bevacizumab with or without triamcinolone for refractory diabetic macular edema; a placebo-controlled, randomized clinical trial. Graefes Arch Clin Exp Ophthalmol 2008;246:483–9 [DOI] [PubMed] [Google Scholar]
- 32.Gillies MC, Sutter FK, Simpson JM, et al. Intravitreal triamcinolone for refractory diabetic macular edema: two-year results of a double-masked, placebo-controlled, randomized clinical trial. Ophthalmology 2006;113:1533–8 [DOI] [PubMed] [Google Scholar]
- 33.Gillies MC, McAllister IL, Zhu M, et al. Intravitreal triamcinolone prior to laser treatment of diabetic macular edema: 24-month results of a randomized controlled trial. Ophthalmology 2011;118:866–72 [DOI] [PubMed] [Google Scholar]
- 34.Lam DS, Chan CK, Mohamed S, et al. Intravitreal triamcinolone plus sequential grid laser versus triamcinolone or laser alone for treating diabetic macular edema: six-month outcomes. Ophthalmology 2007;114:2162–7 [DOI] [PubMed] [Google Scholar]
- 35.Lam DS, Lai TY, Lee VY, et al. Efficacy of 1.25 MG versus 2.5 MG intravitreal bevacizumab for diabetic macular edema: six-month results of a randomized controlled trial. Retina 2009;29:292–9 [DOI] [PubMed] [Google Scholar]
- 36.Massin P, Bandello F, Garweg JG, et al. Safety and efficacy of ranibizumab in diabetic macular edema (RESOLVE Study): a 12-month, randomized, controlled, double-masked, multicenter phase II study. Diabetes Care 2010;33:2399–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soheilian M, Ramezani A, Bijanzadeh B, et al. Intravitreal bevacizumab (avastin) injection alone or combined with triamcinolone versus macular photocoagulation as primary treatment of diabetic macular edema. Retina 2007;27:1187–95 [DOI] [PubMed] [Google Scholar]
- 38.Nguyen QD, Brown DM, Marcus DM, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012;119:789–801 [DOI] [PubMed] [Google Scholar]
- 39.Cunningham ET, Jr, Adamis AP, Altaweel M, et al. A phase II randomized double-masked trial of pegaptanib, an anti-vascular endothelial growth factor aptamer, for diabetic macular edema. Ophthalmology 2005;112:1747–57 [DOI] [PubMed] [Google Scholar]
- 40.Sultan MB, Zhou D, Loftus J, et al. A phase 2/3, multicenter, randomized, double-masked, 2-year trial of pegaptanib sodium for the treatment of diabetic macular edema. Ophthalmology 2011;118:1107–18 [DOI] [PubMed] [Google Scholar]
- 41.Soheilian M, Ramezani A, Obudi A, et al. Randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus macular photocoagulation in diabetic macular edema. Ophthalmology 2009;116:1142–50 [DOI] [PubMed] [Google Scholar]
- 42.Sivaprasad S, Ockrim Z, Massaoutis P, et al. Posterior hyaloid changes following intravitreal triamcinolone and macular laser for diffuse diabetic macular edema. Retina 2008;28:1435–42 [DOI] [PubMed] [Google Scholar]
- 43.Pearson PA, Comstock TL, Ip M, et al. Fluocinolone acetonide intravitreal implant for diabetic macular edema: a 3-year multicenter, randomized, controlled clinical trial. Ophthalmology 2011;118:1580–7 [DOI] [PubMed] [Google Scholar]
- 44.Callanan D, Gupta S, Ciulla TA, et al. Efficacy and safety of combination therapy with dexamethasone intravitreal implant (DEX Implant) plus laser photocoagulation versus monotherapy with laser for treatment of diffuse diabetic macular edema (DDME) [abstract]. Invest Ophthalmol Vis Sci 2011;52:E-Abstract 3968 [Google Scholar]
- 45.Kim Y, Kang S, Yi CH. Three-year follow-up of intravitreal triamcinolone acetonide injection and macular laser photocoagulation for diffuse diabetic macular edema [abstract]. Invest Ophthalmol Vis Sci 2010;51:E-Abstract 4260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elman MJ, Bressler NM, Qin H, et al. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2011;118:609–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nguyen QD, Shah SM, Heier JS, et al. Primary end point (six months) results of the ranibizumab for edema of the mAcula in diabetes (READ-2) study. Ophthalmology 2009;116:2175–81 [DOI] [PubMed] [Google Scholar]
- 48.Ohji M, Ishibashi T. Sr, REVEAL study group Efficacy and safety of ranibizumab 0.5 mg as monotherapy or adjunctive to laser versus laser monotherapy in Asian patients with visual impairment due to diabetic macular edema: 12-month results of the REVEAL Study [abstract]. Invest Ophthalmol Vis Sci 2012;53:E-Abstract 4664 [Google Scholar]
- 49.Mitchell P, RESTORE extension study group 2-Year safety and efficacy outcome of ranibizumab 0.5 mg in patients with visual impairment due to diabetic macular edema (DME): an interim analysis of the RESTORE extension study [abstract]. Invest Ophthalmol Vis Sci 2012;53:E-Abstract 4667 [Google Scholar]
- 50.Do DV, Campochiaro PA, Boyer DS, et al. 6 month results of the READ 3 Study: ranibizumab for edema of the mAcula in diabetes [abstract]. Invest Ophthalmol Vis Sci 2012;53:E-Abstract 5282 [Google Scholar]
- 51.Jorge R, Nepomuceno AB, Takaki E, et al. A prospective randomized trial of intravitreal bevacizumab versus ranibizumab for the management of refractory diabetic macular edema [abstract]. Invest Ophthalmol Vis Sci 2012;53:E-Abstract 347 [Google Scholar]
- 52.Michaelides M, Fraser-Bell S, Hamilton R, et al. Macular perfusion determined by fundus fluorescein angiography at the 4-month time point in a prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (Bolt Study): report 1. Retina 2010;30:781–6 [DOI] [PubMed] [Google Scholar]
- 53.Faghihi H, Esfahani MR, Harandi ZA, et al. Intravitreal bevacizumab vs. combination of intravitreal bevacizumab plus macular photocoagulation in clinically significant diabetic macular edema: 6 months results of a randomized clinical trial. Iranian J Ophthalmol 2010;22:21–6 [Google Scholar]
- 54.Soheilian M, Garfami KH, Ramezani A, et al. Two-year results of a randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus laser in diabetic macular edema. Retina 2012;32:314–21 [DOI] [PubMed] [Google Scholar]
- 55.Lim JW, Lee HK, Shin MC. Comparison of intravitreal bevacizumab alone or combined with triamcinolone versus triamcinolone in diabetic macular edema: a randomized clinical trial. Ophthalmologica 2012;227:100–6 [DOI] [PubMed] [Google Scholar]
- 56.Oliveira Neto HL, Andrade RE, Casella M, et al. A randomized clinical trial to compare the efficacy and safety of isolated or combined intravitreal injection of triamcinolone acetonide and bevacizumab for diabetic macular edema ATEMD protocol—a Brazilian clinical trial [abstract]. Invest Ophthalmol Vis Sci 2011;52:E-Abstract 5331 [Google Scholar]
- 57.Adamis AP, Altaweel M, Bressler NM, et al. Changes in retinal neovascularization after pegaptanib (Macugen) therapy in diabetic individuals. Ophthalmology 2006;113:23–8 [DOI] [PubMed] [Google Scholar]
- 58.Do DV, Nguyen QD, Boyer D, et al. One-year outcomes of the DA VINCI Study of VEGF Trap-Eye in eyes with diabetic macular edema. Ophthalmology 2012;119:1658–65 [DOI] [PubMed] [Google Scholar]
- 59.Haller JA, Kuppermann BD, Blumenkranz MS, et al. Randomized controlled trial of an intravitreous dexamethasone drug delivery system in patients with diabetic macular edema. Arch Ophthalmol 2010;128:289–96 [DOI] [PubMed] [Google Scholar]
- 60.Campochiaro PA, Brown DM, Pearson A, et al. Sustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 Years in patients with diabetic macular edema. Ophthalmology 2012;119:2125–32 [DOI] [PubMed] [Google Scholar]
- 61.Beck RW, Edwards AR, Aiello LP, et al. Diabetic Retinopathy Clinical Research Network (DRCR.net) Three-year follow-up of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular edema. Arch Ophthalmol 2009;127:245–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ockrim ZK, Sivaprasad S, Falk S, et al. Intravitreal triamcinolone versus laser photocoagulation for persistent diabetic macular oedema. Br J Ophthalmol 2008;92:795–9 [DOI] [PubMed] [Google Scholar]
- 63.Bressler NM, Edwards AR, Beck RW, et al. Exploratory analysis of diabetic retinopathy progression through 3 years in a randomized clinical trial that compares intravitreal triamcinolone acetonide with focal/grid photocoagulation. Arch Ophthalmol 2009;127:1566–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Diabetic Retinopathy Clinical Research Network A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology 2008;115:1447–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ford JA, Elders A, Shyangdan D, et al. The relative clinical effectiveness of ranibizumab and bevacizumab in diabetic macular oedema: an indirect comparison. BMJ 2012;345:e5182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chakravarthy U, Harding SP, Rogers CA, et al. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology 2012;119:1399–411 [DOI] [PubMed] [Google Scholar]
- 67.Martin DF, Maguire MG, Fine SL, et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 2012;119:1388–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Campbell RJ, Gill SS, Bronskill SE, et al. Adverse events with intravitreal injection of vascular endothelial growth factor inhibitors: nested case-control study. BMJ 2012;345:e4203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Van der Reis MI, La Heij EC, De Jong-Hesse Y, et al. A systematic review of the adverse events of intravitreal anti-vascular endothelial growth factor injections. Retina 2011;31:1449–69 [DOI] [PubMed] [Google Scholar]
- 70.Fung AE, Rosenfeld PJ, Reichel E. The International Intravitreal Bevacizumab Safety Survey: using the internet to assess drug safety worldwide. Br J Ophthalmol 2006;90:1344–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Elbendary AM, Shahin MM. Intravitreal diclofenac versus intravitreal triamcinolone acetonide in the treatment of diabetic macular edema. Retina 2011;31:2058–64 [DOI] [PubMed] [Google Scholar]
- 72.Sfikakis PP, Grigoropoulos V, Emfietzoglou I, et al. Infliximab for diabetic macular edema refractory to laser photocoagulation: a randomized, double-blind, placebo-controlled, crossover, 32-week study. Diabetes Care 2010;33:1523–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Keech AC, Mitchell P, Summanen PA, et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet 2007;370:1687–97 [DOI] [PubMed] [Google Scholar]
- 74.PKC-DMES Study Group Effect of ruboxistaurin in patients with diabetic macular edema: thirty-month results of the randomized PKC-DMES clinical trial. Arch Ophthalmol 2007;125:318–24 [DOI] [PubMed] [Google Scholar]
- 75.PKC-DMES Study Group Effect of ruboxistaurin on visual loss in patients with diabetic retinopathy. Ophthalmology 2006;113:2221–30 [DOI] [PubMed] [Google Scholar]
- 76.Fong DS, Strauber SF, Aiello LP, et al. Comparison of the modified Early Treatment Diabetic Retinopathy Study and mild macular grid laser photocoagulation strategies for diabetic macular edema. Arch Ophthalmol 2007;125:469–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Health Canada Reports of eye inflammation, endophthalmitis, and Toxic Anterior Segment Syndrome (TASS) following off-label intravitreal use of Avastin (bevacizumab). 2008. [cited 24 Oct 2012]; http://www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/prof/_2008/avastin_4_hpc-cps-eng.php
- 78.Curtis LH, Hammill BG, Schulman KA, et al. Risks of mortality, myocardial infarction, bleeding, and stroke associated with therapies for age-related macular degeneration. Arch Ophthalmol 2010;128:1273–9 [DOI] [PubMed] [Google Scholar]
- 79.Gower EW, Cassard S, Chu L, et al. Adverse event rates following intravitreal injection of Avastin or Lucentis for treating age-related macular degeneration [abstract]. Invest Ophthalmol Vis Sci 2011;52:E-Abstract 6644 [Google Scholar]
- 80.General Medical Council. Prescribing medicines for use outside the terms of their licence (off-label). 2012 [cited 24 Oct 2012]; http://www.gmc-uk.org/guidance/ethical_guidance/prescriptions_faqs.asp#10.
- 81.U.S.Food and Drug Administration. Off-Label" and investigational use of marketed drugs, biologics, and medical devices—Information Sheet. 2011 [cited 24 Oct 2012]; http://www.fda.gov/RegulatoryInformation/Guidances/ucm126486.htm.
- 82.Alimera Sciences. Alimera Sciences’ ILUVIEN Receives Marketing Authorization in France for the Treatment of Chronic Diabetic Macular Edema. 2012 [cited 24 Oct 2012]; http://investor.alimerasciences.com/releasedetail.cfm?ReleaseID=692876.
- 83.Laidlaw DA. Vitrectomy for diabetic macular oedema. Eye 2008;22:1337–41 [DOI] [PubMed] [Google Scholar]
- 84.National Institute for Health and Clinical Excellence. Ranibizumab for the treatment of diabetic macular oedema:TA237. 2011 [cited 24 Oct 2012]; http://publications.nice.org.uk/ranibizumab-for-the-treatment-of-diabetic-macular-oedema-ta237.
- 85.Rajendram R, Fraser-Bell S, Kaines A, et al. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: report 3. Arch Ophthalmol 2012;130:972–9 [DOI] [PubMed] [Google Scholar]
- 86.Sivaprasad S, Dorin G. Subthreshold diode laser micropulse photocoagulation for the treatment of diabetic macular edema. Expert Rev Medical Devices 2012;9:189–97 [DOI] [PubMed] [Google Scholar]
- 87.Cho WB, Moon JW, Kim HC. Intravitreal triamcinolone and bevacizumab as adjunctive treatments to panretinal photocoagulation in diabetic retinopathy. Br J Ophthalmol 2010;94:858–63 [DOI] [PubMed] [Google Scholar]
- 88.Googe J, Brucker AJ, Bressler NM, et al. Randomized trial evaluating short-term effects of intravitreal ranibizumab or triamcinolone acetonide on macular edema after focal/grid laser for diabetic macular edema in eyes also receiving panretinal photocoagulation. Retina 2011;31:1009–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Faghihi H, Roohipoor R, Mohammadi SF, et al. Intravitreal bevacizumab versus combined bevacizumab-triamcinolone versus macular laser photocoagulation in diabetic macular edema. Eur J Ophthalmol 2008;18:941–8 [DOI] [PubMed] [Google Scholar]
- 90.Figueroa MS, Contreras I, Noval S. Surgical and anatomical outcomes of pars plana vitrectomy for diffuse nontractional diabetic macular edema. Retina 2008;28:420–6 [DOI] [PubMed] [Google Scholar]
- 91.Isaac DL, Abud MB, Frantz KA, et al. Comparing intravitreal triamcinolone acetonide and bevacizumab injections for the treatment of diabetic macular oedema: a randomized double-blind study. Acta Ophthalmol 2012;90:56–60 [DOI] [PubMed] [Google Scholar]
- 92.Paccola L, Costa RA, Folgosa MS, et al. Intravitreal triamcinolone versus bevacizumab for treatment of refractory diabetic macular oedema (IBEME study). Br J Ophthalmol 2008;92:76–80 [DOI] [PubMed] [Google Scholar]
- 93.Prager SG, Kriechbaum K, Mylonas G, et al. Comparison of intravitreally applied bevacizumab and triamcinolone on diabetic macular edema [abstract]. Invest Ophthalmol Vis Sci 2010;51:E-Abstract 4262 [Google Scholar]
- 94.Ozturk BT, Kerimoglu H, Bozkurt B, et al. Comparison of intravitreal bevacizumab and ranibizumab treatment for diabetic macular edema. J Ocul Pharmacol Ther 2011;27:373–7 [DOI] [PubMed] [Google Scholar]
- 95.Marey HM, Ellakwa AF. Intravitreal bevacizumab alone or combined with triamcinolone acetonide as the primary treatment for diabetic macular edema. Clin Ophthalmol 2011;5:1011–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shahin MM, El-Lakkany RS. A prospective, randomized comparison of intravitreal triamcinolone acetonide versus intravitreal bevacizumab (avastin) in diffuse diabetic macular edema. Middle East Afr J Ophthalmol 2010;17:250–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Loftus JV, Sultan MB, Pleil AM, et al. Changes in vision- and health-related quality of life in patients with diabetic macular edema treated with pegaptanib sodium or sham. Invest Ophthalmol Vis Sci 2011;52:7498–505 [DOI] [PubMed] [Google Scholar]
- 98.Ferrone PJ, Jonisch J. Ranibizumab dose comparison for the treatment of diabetic macular edema [abstract]. Invest Ophthalmol Vis Sci 2011;52:E-Abstract 5333 [Google Scholar]
- 99.Solaiman KA, Diab MM, Abo-Elenin M. Intravitreal bevacizumab and/or macular photocoagulation as a primary treatment for diffuse diabetic macular edema. Retina 2010;30:1638–45 [DOI] [PubMed] [Google Scholar]
- 100.Scott IU, Edwards AR, Beck RW, et al. Diabetic Retinopathy Clinical Research Network A phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edema. Ophthalmology 2007;114:1860–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lee SJ, Kim ET, Moon YS. Intravitreal bevacizumab alone versus combined with macular photocoagulation in diabetic macular edema. Korean J Ophthalmol 2011;25:299–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Audren F, Lecleire-Collet A, Erginay A, et al. Intravitreal triamcinolone acetonide for diffuse diabetic macular edema: phase 2 trial comparing 4 mg vs 2 mg. Am J Ophthalmol 2006;142:794–9 [DOI] [PubMed] [Google Scholar]
- 103.Audren F, Erginay A, Haouchine B, et al. Intravitreal triamcinolone acetonide for diffuse diabetic macular oedema: 6-month results of a prospective controlled trial. Acta Ophthalmol Scand 2006;84:624–30 [DOI] [PubMed] [Google Scholar]
- 104.Avitabile T, Longo A, Reibaldi A. Intravitreal triamcinolone compared with macular laser grid photocoagulation for the treatment of cystoid macular edema. Am J Ophthalmol 2005;140:695–702 [DOI] [PubMed] [Google Scholar]
- 105.Bandello F, Pognuz DR, Pirracchio A, et al. Intravitreal triamcinolone acetonide for florid proliferative diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 2004;242:1024–7 [DOI] [PubMed] [Google Scholar]
- 106.Bonini MA, Jorge R, Barbosa JC, et al. Intravitreal injection versus sub-Tenon's infusion of triamcinolone acetonide for refractory diabetic macular edema: a randomized clinical trial. Invest Ophthalmol Vis Sci 2005;46:3845–9 [DOI] [PubMed] [Google Scholar]
- 107.Cellini M, Pazzaglia A, Zamparini E, et al. Intravitreal vs. subtenon triamcinolone acetonide for the treatment of diabetic cystoid macular edema. BMC Ophthalmol 2008;8:5TN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cardillo JA, Melo LA, Jr, Costa RA, et al. Comparison of intravitreal versus posterior sub-Tenon's capsule injection of triamcinolone acetonide for diffuse diabetic macular edema. Ophthalmology 2005;112:1557–63 [DOI] [PubMed] [Google Scholar]
- 109.Chung EJ, Freeman WR, Azen SP, et al. Comparison of combination posterior sub-tenon triamcinolone and modified grid laser treatment with intravitreal triamcinolone treatment in patients with diffuse diabetic macular edema. Yonsei Medi J 2008;49:955–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Dehghan MH, Ahmadieh H, Ramezani A, et al. A randomized, placebo-controlled clinical trial of intravitreal triamcinolone for refractory diabetic macular edema. Int Ophthalmol 2008;28:7–17 [DOI] [PubMed] [Google Scholar]
- 111.Chew E, Strauber S, Beck RW, et al. Diabetic Retinopathy Clinical Research Network Randomized trial of peribulbar triamcinolone acetonide with and without focal photocoagulation for mild diabetic macular edema: a pilot study. Ophthalmology 2007;114:1190–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gil AL, Azevedo MJ, Tomasetto GG, et al. Treatment of diffuse diabetic maculopathy with intravitreal triamcinolone and laser photocoagulation: randomized clinical trial with morphological and functional evaluation. Arq BrasArquivos Brasileiros de Oftalmol 2011;74:343–7 [DOI] [PubMed] [Google Scholar]
- 113.Entezari M, Ahmadieh H, Dehghan MH, et al. Posterior sub-tenon triamcinolone for refractory diabetic macular edema: a randomized clinical trial. Eur J Ophthalmol 2005;15:746–50 [DOI] [PubMed] [Google Scholar]
- 114.Hauser D, Bukelman A, Pokroy R, et al. Intravitreal triamcinolone for diabetic macular edema: comparison of 1, 2, and 4 mg. Retina 2008;28:825–30 [DOI] [PubMed] [Google Scholar]
- 115.Jonas JB, Kamppeter BA, Harder B, et al. Intravitreal triamcinolone acetonide for diabetic macular edema: a prospective, randomized study. J Ocul Pharmacol Ther 2006;22:200–7 [DOI] [PubMed] [Google Scholar]
- 116.Joussen AM, Weiss C, Bauer D, et al. Triamcinolone versus inner-limiting membrane peeling in persistent diabetic macular edema (TIME study): design issues and implications. Graefes Arch Clin Exp Ophthalmol 2007;245:1781–7 [DOI] [PubMed] [Google Scholar]
- 117.Kaderli B, Avci R. Comparison of topical and subconjunctival anesthesia in intravitreal injection administrations. Eur J Ophthalmol 2006;16:718–21 [DOI] [PubMed] [Google Scholar]
- 118.Kang SW, Sa HS, Cho HY, et al. Macular grid photocoagulation after intravitreal triamcinolone acetonide for diffuse diabetic macular edema. Arch Ophthalmol 2006;124:653–8 [DOI] [PubMed] [Google Scholar]
- 119.Kim JE, Pollack JS, Miller DG, et al. ISIS-DME: a prospective, randomized, dose-escalation intravitreal steroid injection study for refractory diabetic macular edema. Retina 2008;28:735–40 [DOI] [PubMed] [Google Scholar]
- 120.Lam DS, Chan CK, Mohamed S, et al. A prospective randomised trial of different doses of intravitreal triamcinolone for diabetic macular oedema. Br J Ophthalmol 2007;91:199–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lee HY, Lee SY, Park JS. Comparison of photocoagulation with combined intravitreal triamcinolone for diabetic macular edema. Korean J Ophthalmol 2009;23:153–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Maia OO, Jr, Takahashi BS, Costa RA, et al. Combined laser and intravitreal triamcinolone for proliferative diabetic retinopathy and macular edema: one-year results of a randomized clinical trial. Am J Ophthalmol 2009;147:291–7 [DOI] [PubMed] [Google Scholar]
- 123.Massin P, Audren F, Haouchine B, et al. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of a prospective controlled trial. Ophthalmology 2004;111:218–24 [DOI] [PubMed] [Google Scholar]
- 124.Mohamed S, Leung GM, Chan CK, et al. Factors associated with variability in response of diabetic macular oedema after intravitreal triamcinolone. Clin Experiment Ophthalmol 2009;37:602–8 [DOI] [PubMed] [Google Scholar]
- 125.Nakamura A, Shimada Y, Horio N, et al. Vitrectomy for diabetic macular edema with posterior subtenon injection of triamcinolone acetonide. [Japanese]. Folia Ophthalmol Japonica 2004;55:958–62 [Google Scholar]
- 126.Spandau UH, Derse M, Schmitz-Valckenberg P, et al. Dosage dependency of intravitreal triamcinolone acetonide as treatment for diabetic macular oedema. Br J Ophthalmol 2005;89:999–1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tunc M, Onder HI, Kaya M. Posterior sub-Tenon's capsule triamcinolone injection combined with focal laser photocoagulation for diabetic macular edema. Ophthalmology 2005;112:1086–91 [DOI] [PubMed] [Google Scholar]
- 128.Verma LK, Vivek MB, Kumar A, et al. A prospective controlled trial to evaluate the adjunctive role of posterior subtenon triamcinolone in the treatment of diffuse diabetic macular edema. J Ocul Pharmacol Ther 2004;20:277–84 [DOI] [PubMed] [Google Scholar]
- 129.Wickremasinghe SS, Rogers SL, Gillies MC, et al. Retinal vascular caliber changes after intravitreal triamcinolone treatment for diabetic macular edema. Invest Ophthalmol Vis Sci 2008;49:4707–11 [DOI] [PubMed] [Google Scholar]
- 130.Yalcinbayir O, Gelisken O, Kaderli B, et al. Intravitreal versus sub-Tenon posterior triamcinolone injection in bilateral diffuse diabetic macular edema. Ophthalmologica 2011;225:222–7 [DOI] [PubMed] [Google Scholar]
- 131.Haller JA, Bandello F, Belfort R, Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology 2010;117:1134–46 [DOI] [PubMed] [Google Scholar]
- 132.Haller JA, Dugel P, Weinberg DV, et al. Evaluation of the safety and performance of an applicator for a novel intravitreal dexamethasone drug delivery system for the treatment of macular edema. Retina 2009;29:46–51 [DOI] [PubMed] [Google Scholar]
- 133.Kuppermann BD, Blumenkranz MS, Haller JA, et al. Randomized controlled study of an intravitreous dexamethasone drug delivery system in patients with persistent macular edema. Arch Ophthalmol 2007;125:309–17 [DOI] [PubMed] [Google Scholar]
- 134.Boyer DS, Faber D, Gupta S, et al. Dexamethasone intravitreal implant for treatment of diabetic macular edema in vitrectomized patients. Retina 2011;31:915–23 [DOI] [PubMed] [Google Scholar]
- 135.Campochiaro PA, Hafiz G, Shah SM, et al. Sustained ocular delivery of fluocinolone acetonide by an intravitreal insert. Ophthalmology 2010;117:1393–9 [DOI] [PubMed] [Google Scholar]
- 136.Gillies MC, Islam FM, Zhu M, et al. Efficacy and safety of multiple intravitreal triamcinolone injections for refractory diabetic macular oedema. Br J Ophthalmol 2007;91:1323–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gillies MC, Simpson JM, Gaston C, et al. Five-year results of a randomized trial with open-label extension of triamcinolone acetonide for refractory diabetic macular edema. Ophthalmology 2009;116:2182–7 [DOI] [PubMed] [Google Scholar]
- 138.Sutter FK, Simpson JM, Gillies MC. Intravitreal triamcinolone for diabetic macular edema that persists after laser treatment: three-month efficacy and safety results of a prospective, randomized, double-masked, placebo-controlled clinical trial. Ophthalmology 2004;111:2044–9 [DOI] [PubMed] [Google Scholar]
- 139.Brown DM, Nguyen QD, Rubio RG, et al. Ranibizumab for Diabetic Macular Edema (DME): 24-Month Efficacy and Safety Results of RISE—a phase 3 randomized controlled trial [abstract]. Invest Ophthalmol Vis Sci 2011;52:E-Abstract 6647 [Google Scholar]
- 140.Boyer D, Sy J, Rundle AC, et al. Ranibizumab (Anti-VEGF) for vision loss due to diabetic macular edema—results of two phase III randomized trials [abstract]. 71st Scientific Sessions June 24–28, 2011, San Diego Convention Center—San Diego, California, USA2011;Abstract No, 133-LBOR. [Google Scholar]
- 141.Soheilian M, Ramezani A, Yaseri M, et al. Initial macular thickness and response to treatment in diabetic macular edema. Retina 2011;31:1564–73 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.