Abstract
Objectives
To identify patient characteristics and surgical factors associated with patient-reported outcomes over 5 years following primary total hip replacement (THR).
Design
Prospective cohort study.
Setting
Seven hospitals across England and Scotland.
Participants
1431 primary hip replacements for osteoarthritis.
Main outcome measures
The Oxford Hip Score (OHS) was collected preoperatively and each year up to 5 years postoperatively. Repeated measures such as linear regression modelling are used to identify patient and surgical predictors of outcome and describe trends over time.
Results
The majority of patients demonstrated substantial improvement in pain/function in the first year after surgery—between 1 and 5 years follow-up, there was neither further improvement nor decline. The strongest determinant of attained postoperative OHS was the preoperative OHS—those with worse preoperative pain/function had worse postoperative pain/function. Other predictors with small but significant effects included: femoral component offset—women with an offset of 44 or more had better outcomes; age—compared to those aged 50–60, younger (age <50) and older patients (age >60) had worse outcome, increasing body mass index (BMI), more coexisting diseases and worse Short Form 36 mental health (MH) was related to worse postoperative pain/function. Assessment of change in OHS between preoperative and postoperative assessments revealed that patients achieved substantial and clinically relevant symptomatic improvement (change), regardless of variation in these patient and surgical factors.
Conclusions
Patients received substantial benefit from surgery, regardless of their preoperative assessments and surgical characteristics (baseline pain/function, age, BMI, comorbidities, MH and femoral component offset). Further research is needed to identify other factors that can improve our ability to identify patients at risk of poor outcomes from THR surgery.
Keywords: Epidemiology
Article summary.
Article focus
Total hip replacement (THR) is a common and successful surgical intervention, providing substantial relief from pain and improvement in function in patients with hip arthritis.
An important minority of patients continue to experience some pain and functional disability following surgery.
Relatively little work has been carried out to establish the predictors of patient reported outcomes after hip replacement, in particular the role of intraoperative surgical factors and how symptoms change over time in the mid-to-long term.
Key messages
The majority of patients achieved large improvement in symptoms of pain and function in the first year following surgery—there was no further improvement or decline between 1 and 5 years.
A new finding is that a larger femoral component offset is associated with better outcomes of THR in women—this finding requires confirmation in other large cohorts.
Small statistically significant differences in attained postoperative Oxford Hip Score (OHS) relating to patient (age, BMI, comorbidities and mental health (MH)) and surgical (femoral component offset) characteristics at the time of surgery are greatly outweighed by the substantial change in OHS achieved by these patients.
Strengths and limitations of this study
Strengths include the large sample size, repeated measures of a reliable, valid and responsive instrument for assessing outcomes of THR with data collected prospectively over 5 years with a good rate of follow-up.
Further strengths include the use of multiple imputation and bootstrapping as an internal validation technique, ensuring that the predictors identified are those most likely to be replicated in external validation studies.
Limitations are that other potential predictive variables were not available in this study, such as radiographic grade, pattern of osteoarthritis, patient expectations of surgery and the type and extent of joint damage.
Response bias may play a role, as responders were younger and had better preoperative Short Form 36 MH scores; hence, the true effects of these predictors may be underestimated.
Introduction
Total hip replacement (THR) surgery is a commonly performed and successful surgical intervention, providing substantial relief from pain and improvement in functional disability in patients with hip arthritis.1–4 Attention has turned from looking at the technical outcomes of surgery, such as prosthesis survival, to the use of patient reported outcome measures (PROMs) to see whether surgery has been successful from the patient's perspective.3 5 Through the use of PROMs, it has emerged that while on average the majority of patients improve after surgery, an important minority of patients continue to experience some pain and functional disability after THR, whereas some have no improvement or get worse.6–10
Relatively little work has been carried out to establish the predictors of good or bad patient-reported outcomes after THR.11 Several potential determinants of outcomes of THR have been identified within the literature including baseline levels of pain and function,8 12–16 severity of clinical disease,13 16 age,13 16 17 gender,13 15 18 radiographic grade,13 14 education,8 12 14 18 obesity,15 17 comorbidities,8 15 living alone,15 19 mental health (MH)16 and patient’s expectations of surgery.14 20 Little is known about the probable role of intraoperative surgical factors on patient-reported outcomes. In addition, the majority of prior research looks at short-term outcomes and few studies have examined how symptoms change over time in the longer term.
Using a large prospective cohort of patients receiving primary THR for osteoarthritis (OA) with repeated measures of patient-reported outcomes (as measured by the Oxford Hip Score (OHS)) at yearly intervals over a 5-year follow-up period, the aim of this study was to: (1) identify patient characteristics and intraoperative surgical factors associated with differences in attained postoperative levels of pain and function and (2) for variables identified as significant predictors of attained postoperative score to assess change (temporal trends) in symptoms of pain and function over time between preoperative and postoperative assessments.
Methods
We obtained information from the Exeter Primary Outcomes Study (EPOS). Details of the study have previously been published elsewhere.21–23 Patients were consecutively recruited between January 1999 and January 2002 at seven centres across England and Scotland. Patients underwent THR using a cemented Exeter femoral stem component (Stryker Howmedica Osteonics, Mahwah, New Jersey).24 A variety of cemented and uncemented acetabular components were used. Patients were included if they were undergoing primary hip replacement with an Exeter cemented femoral stem and were willing and able to give consent to participate in the study. The North Western Multiple Centre Research Ethics Committee and the local research ethics committees in all the participating centres gave ethical approval for conducting the study. All eligible patients were invited to participate in the study. Patient recruitment varied between the centres but was between 80% and 90% of eligible patients. The geographical area covered by the participating hospitals was wide and included both university teaching and district general hospitals that included urban and rural locations and represented both affluent and inner city suburbs. The catchment area of the four combined units included over a million people. There were 1375 patients (1431 hips) with a primary diagnosis of OA. The unit of analysis was the implant rather than the patient, of whom 56 had bilateral procedures. We examined 1431 THRs performed by consultant and non-consultant surgeons using anterolateral or posterior approaches.
An extensive range of patient and intraoperative surgical factors has been collected within the EPOS. A priori a reduced set of variables was selected for inclusion in the analysis, based on factors previously shown within the literature to be related to patient-reported outcomes of hip replacement, in addition to further variables that were considered potentially relevant—in particular, the intraoperative factors, as little is known within the literature on the possible role with patient outcomes. The final set of patient and surgical factors that were selected are described below.
Patient variables
At the preoperative assessment, information was collected on age, gender, height and weight (from which body mass index (BMI) was calculated), primary diagnosis and current occupation. Patients were asked whether they were using concomitant therapies such as oral anticoagulants, corticosteroids, non-steroidal anti-inflammatory drugs and other analgesics. Data were collected on coexistent diseases including whether the patient had ever had deep venous thrombosis and pulmonary embolism, whether there was any evidence of urinary tract infection in the 4 weeks prior to surgery, whether the patient had any other musculoskeletal disease, whether the patient suffers from neurological, respiratory, cardiovascular, renal and hepatic disease and whether the patient was currently receiving treatment for any other medical conditions. An ordinal variable was created of the number of coexistent diseases a patient had at the preoperative assessment. Fixed flexion range of motion recorded in degrees was obtained from the Charnley Modification of D'Aubigne-Postel Grade questionnaire.25 26 Patients completed a preoperative Short Form 36 (SF-36),27 which measures the quality of life generically through eight domains: physical function, bodily pain, general health, role physical, vitality, social function, role emotional and MH. The lowest score, 0, corresponds to the worst possible health and 100, to the best possible health.
Surgical variables
Detailed intraoperative information was collected for each patient. This included information on the grade of the operator (consultant, registrar and senior house officer), surgical approach (anterolateral and posterior) and patient position (supine and lateral). Data were available on whether or not a lavage system was used for the acetabular component, whether there was cement pressurisation for both the femoral and acetabular components, the type of cement used in both the socket (none, simplex, cmw1, palacos r and other) and the femur (simplex, cmw1, cmw3, palacos r and palacos lv), the type of polyethylene used (uhmwpe and cross-linked), whether the femoral head was made of stainless steel or ceramic, femoral head size (22, 26 or 28 mm) and the femoral component offset size (35, 37.5, 44, 50 mm offset). The duration of the operation was recorded in minutes.
Outcome variable
Prior to the surgery, patients completed an OHS questionnaire with follow-up questionnaires being filled in at 1, 2, 3, 4 and 5 years postsurgery. Preoperative and postoperative scores were completed independently by the patient prior to clinical examination. The OHS was introduced in 1996 predominantly for use in clinical trials.28 The score is joint specific and has been assessed for reliability and validity.29 The OHS consists of 12 questions asking patients to describe their hip pain and function during the past 4 weeks. Each question is on a Likert scale taking values from 0 to 4. An overall score is created by summing the responses to each of the 12 questions. A total score was created ranging from 0 to 48, where 0 is the worst possible score (most severe symptoms) and 48 is the best score (least symptoms).
Statistical methods
Stata V.11.1 (Stata, College Station, Texas, USA) was used for all statistical analyses. Potential prognostic variables included the patient and surgical variables described above. The cumulative effect of missing data in several variables often leads to exclusion of a substantial proportion of the original sample, causing a loss of precision and power. To overcome this bias we used multiple imputation, which allows for the uncertainty about missing data by creating several plausible imputed datasets and appropriately combining their results. We have performed this using the Imputation by Chained Equations (ICE) procedure in Stata30 and 10 imputed datasets created. We included all predictor variables in the multiple imputation process (as listed earlier), together with the outcome variable as this carries information about missing values of the predictors. We fitted two models to describe the association of the patient and surgical variables on the following outcomes:
Attained postoperative OHS at 1, 2, 3, 4 and 5 years follow-up: a repeated measures linear regression model was fitted where the outcomes were the OHS at 1, 2, 3, 4 and 5 years follow-up, adjusting for the preoperative OHS as a covariate in the model. Generalised estimating equation was used to account for clustering within the data using an exchangeable correlation matrix. This model estimates the impact of predictors on the average OHS over the five follow-up time points. Fractional polynomial regression modelling was used to explore evidence of non-linear relationships for continuous variables. Interaction terms were fitted between the predictor variable and time, to see if the association of the predictor on outcome changed between 1 and 5 years follow-up.
Change in OHS between baseline and 1, 2, 3, 4 and 5 years follow-up: for variables identified as significant predictors of attained postoperative OHS, the repeated measures linear regression model is fitted, where the outcome is expanded to include the preoperative and 1, 2, 3, 4 and 5 years postoperative OHS. Interaction terms are fitted between the predictor variable and time to describe the change in OHS over time31 across categories of the predictor variable, for example, in those who are obese versus not obese.
Model validation
The full regression model including all predictor variables is fitted to each of the imputed datasets and averaged together to give overall estimated associations with standard errors (SEs) calculated using Rubins rules.30 Given the extensive list of patient and surgical variables considered for inclusion in the model, we wanted to ensure that we minimised the possibility of making a type 1 error (rejecting the null hypothesis when it is true)—for example, the chance that a variable identified as being ‘significant’ in this dataset may not be replicated in other samples of patients. For internal validation of the model, we therefore used a combination of multiple imputation and bootstrapping32 33 (see online supplementary file). A total of 200 bootstrap samples are randomly drawn with replacement. An automatic backward selection procedure is applied to each of the 200 bootstrap samples of 10 imputed datasets using a Wald test with a stopping rule of α=0.157. Variables retained in the final regression model are those consistently selected across the re-samples at least 70% of the time. To assess model discrimination, we use the R2 statistic as a measure of explained variation.34
Results
Data are available on 1375 patients (1431 hips) receiving primary hip-replacement surgery between January 1999 and January 2002. Of these patients, 1281 (89.5%) completed a preoperative OHS questionnaire and at least one of the follow-up questionnaires and were included in the analysis. About 80% of patients completed the OHS at the 1 year follow-up and this declined to a 70% response rate by 5 years. Baseline demographic details are described in table 1. A comparison of the patients that did, and did not, respond to the 5-year follow-up questionnaire revealed that there were no differences in baseline pain and function as assessed by the OHS. Differences were observed where those that responded were younger, less likely to be unemployed/retired and had better preoperative SF-36 MH scores.
Table 1.
Descriptive statistics and comparison of those who did, and did not, complete the 5-year follow-up questionnaire
| Variable | Missing | Baseline (n=1431) | Non-responders at year 5 | Responders at year 5 | p Value* |
|---|---|---|---|---|---|
| Oxford Hip Score | |||||
| Preoperative | 70 (4.9%) | 16.4 (7.8) | 16.1 (8.2) | 16.5 (7.6) | 0.35 |
| 1 year postoperative | 274 (19.1%) | 43 (36, 46) | – | – | |
| 2 year postoperative | 316 (22.1%) | 43 (36, 47) | – | – | |
| 3 year postoperative | 368 (25.7%) | 43 (36, 47) | – | – | |
| 4 year postoperative | 430 (30.0%) | 44 (36, 47) | – | – | |
| 5 year postoperative | 396 (27.7%) | 43 (37, 47) | – | – | |
| Patient characteristics | |||||
| Age | 9 (1%) | 70.0 (63.9, 76.1) | 73.6 (66.2, 79.3) | 68.8 (62.7, 74.5) | <0.001 |
| BMI | 95 (7%) | 27.4 (4.9) | 27.1 (4.9) | 27.6 (4.8) | 0.077 |
| Gender | 7 (0%) | 0.46 | |||
| Male | 537 (38%) | 171 (39%) | 366 (37%) | ||
| Female | 887 (62%) | 266 (61%) | 621 (63%) | ||
| Occupation | 0 (0%) | 0.005 | |||
| Heavy manual | 41 (3%) | 8 (2%) | 33 (3%) | ||
| Light manual | 89 (6%) | 20 (5%) | 69 (7%) | ||
| Office/professional | 107 (7%) | 21 (5%) | 86 (9%) | ||
| Housewife | 187 (13%) | 67 (15%) | 120 (12%) | ||
| Unemployed/retired | 1007 (70%) | 325 (74%) | 682 (69%) | ||
| Number of coexisting diseases | 0 (0%) | 0.94 | |||
| 0 | 431 (30%) | 136 (31%) | 295 (30%) | ||
| 1 | 498 (35%) | 147 (33%) | 351 (35%) | ||
| 2 | 315 (22%) | 99 (22%) | 216 (22%) | ||
| 3 | 140 (10%) | 43 (10%) | 97 (10%) | ||
| 4 | 47 (3%) | 16 (4%) | 31 (3%) | ||
| Concomitant therapy used | 8 (1%) | 0.84 | |||
| No | 104 (7%) | 31 (7%) | 73 (7%) | ||
| Yes | 1319 (93%) | 406 (93%) | 913 (93%) | ||
| SF36 mental health score | 515 (36%) | 74 (60, 88) | 72 (52, 88) | 76 (60, 88) | 0.046 |
Cells represent either: number (percentage), mean (SD), median (IQR).
Where continuous variables were not normally distributed, a non-parametric t test (Kruskal-Wallis) was used.
Fisher’s exact test is used where the expected counts are less than 5.
*t Tests are used for continuous variables and χ2 tests for categorical variables.
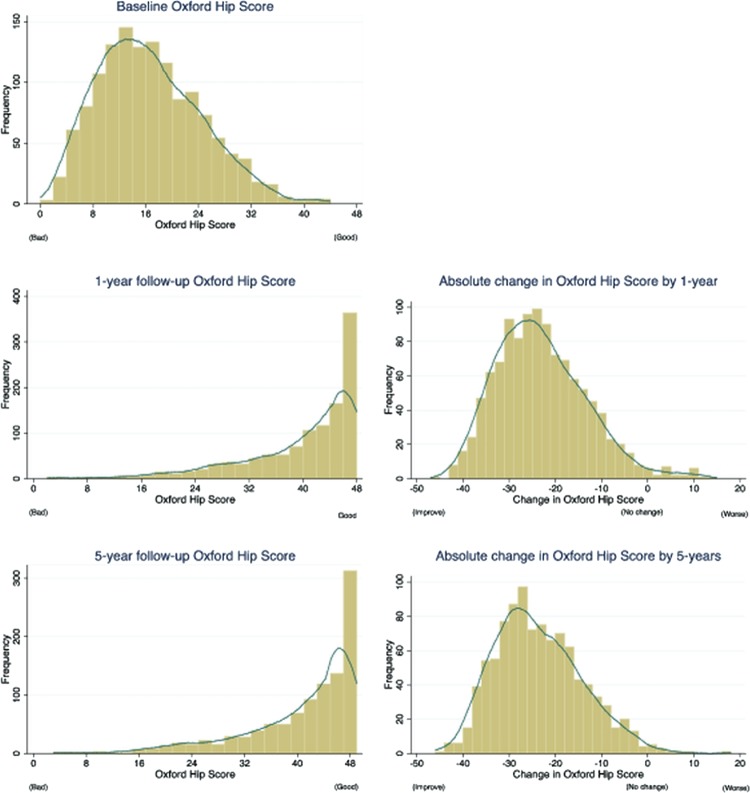
Histograms of the distribution of OHS at baseline and follow-up and the absolute difference in scores (figure 1) highlight that, at the 1-year and 5-year follow-ups, the score is negatively skewed to the left, suggesting that the majority of patients achieve improvement in pain and function. The histograms of the difference in scores highlight that almost all patients get better with only a small minority getting worse or receiving no improvement (2.3% by 1 year and 1.2% by 5 years). The change in OHS over time from the repeated measures regression model is displayed in figure 2. This demonstrates that regardless of the level of preoperative OHS, patients achieved substantial improvement in pain and function following surgery. Those with the worst preoperative scores achieved the greatest improvement (28.8 point change in those with preoperative OHS <5); however, patients with the best preoperative scores still achieved substantial improvement (change of 10.6 points in those with preoperative OHS >30). Interestingly, between the 1-year and 5-year follow-up, a steady state is reached where there is no further improvement or decline, with a non-significant trend between OHS and time (p=0.88).
Figure 1.
Distribution of Oxford Hip Score at baseline, follow-up and absolute difference in scores.
Figure 2.
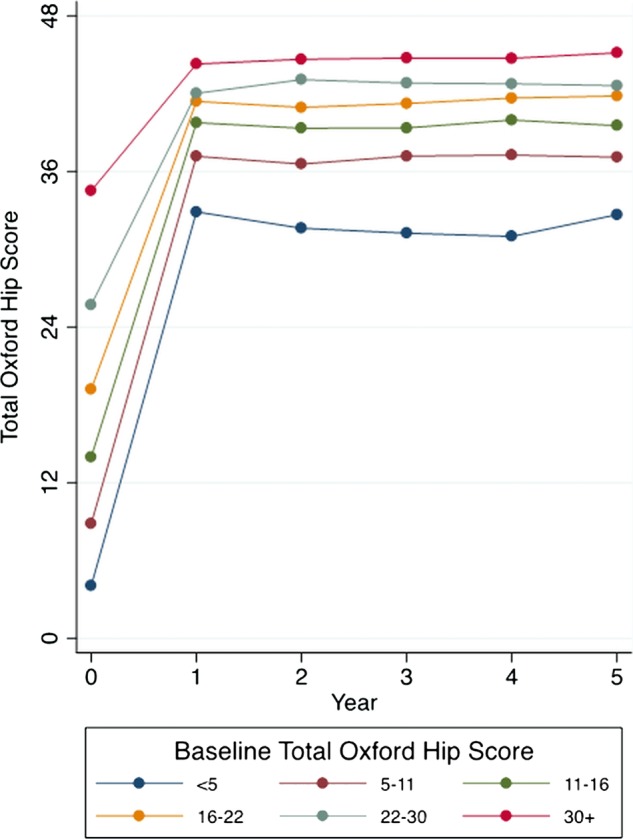
Change in Oxford Hip Score over time, stratified by baseline score.
A number of variables were identified as important predictors of attained postoperative OHS (table 2). The strongest determinant of outcomes was the baseline OHS. Increasing baseline OHS (better preoperative pain/function) was associated with increasing follow-up OHS (better postoperative pain/function). The effect of age was non-linear, where compared to those aged 50–60, younger patients (age <50) and older patients (age >60) had worse outcomes. Increasing BMI, patients with a greater number of coexisting diseases prior to surgery and those with worse preoperative SF-36 MH scores, also had worse outcomes. The surgical predictor we identified was femoral component offset, where patients with larger offset size (offset of 44 or more) had significantly better outcomes. We hypothesised that this may be explained by an interaction with gender, where a larger offset is used in men. A significant interaction was observed where no association was observed in men, while in women those with larger offsets had better outcomes. The effect of surgical approach was significant at the 1 year follow-up, where the anterolateral approach had better outcomes than the posterior approach (difference in 1 year OHS of 2.2 units 95% CI 1.1 to 3.3); however, the effect size attenuated over time and became no longer significant between 3-year and 5-year follow-up.
Table 2.
Repeated measures analysis of covariance models to identify predictors of the average Oxford Hip Score (OHS) between 1-year and 5-year follow-up
| Variable | Univariable Δ coefficient (95% CI) |
p Value | Multivariable Δ coefficient (95% CI) |
p Value |
|---|---|---|---|---|
| Patient variables | ||||
| Baseline total Oxford Hip Score (10 units) | 3.68 (3.16 to 4.20) | <0.001 | 2.68 (2.16 to 3.21) | <0.001 |
| Year | 0.02 (−0.10 to 0.13) | 0.77 | 0.01 (−0.11 to 0.13) | 0.88 |
| Age | ||||
| <50 | −1.44 (−3.92 to 1.03) | 0.25 | ||
| 50–60 | −0.96 (−2.27 to 0.35) | 0.15 | −1.87 (−3.22 to −0.53) | 0.006 |
| 60–70 | 0.00 (0.00 to 0.00) | – | 0.00 (0.00 to 0.00) | – |
| 70–80 | −0.37 (−1.20 to 0.46) | 0.38 | −1.49 (−2.37 to −0.61) | 0.001 |
| 80+ | −2.29 (−3.69 to −0.88) | 0.001 | −3.81 (−5.29 to −2.33) | <0.001 |
| BMI (10 units) | −1.14 (−2.05 to −0.22) | 0.02 | −1.54 (−2.45 to −0.64) | 0.001 |
| Number of coexisting diseases | −1.06 (−1.43 to −0.69) | <0.001 | −0.90 (−1.27 to −0.54) | <0.001 |
| SF-36 mental health score (10 units) | 0.80 (0.50 to 1.11) | <0.001 | 0.76 (0.46 to 1.07) | <0.001 |
| Surgical variables | ||||
| Femoral component offset size (mm offset) | 0.15 (0.04 to 0.26) | 0.01 | 0.17 (0.06 to 0.28) | 0.002 |
| R2 | 17.4% | |||
| Optimism | 0.8% | |||
| Bias-corrected R2 | 16.6% | |||
Δ: represents the average follow-up OHS between 1, 2, 3, 4 and 5 years follow-up.
Variables included in the final regression model are those that are retained in at least 70% of the 200 bootstrap backward selection regression models.
Univariable—each predictor in the model is adjusted for baseline OHS only.
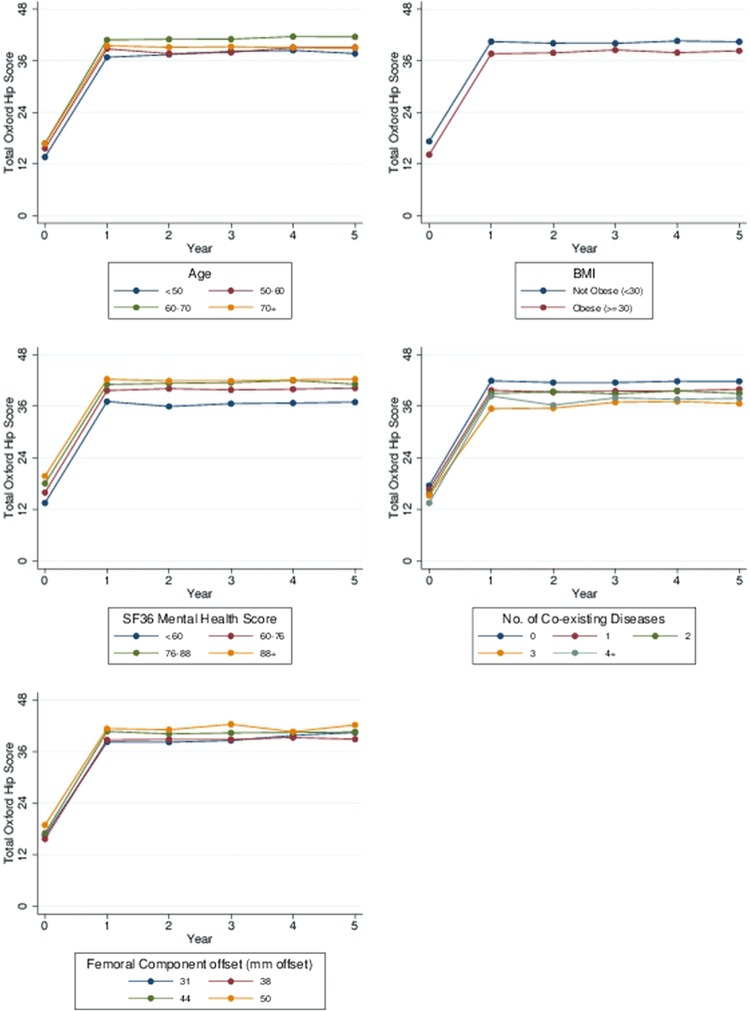
Figure 3 describes the change in OHS over time stratified according to each of the predictor variables we identified in this study. The graphs highlight that while there are small statistically significant differences in attained postoperative OHS relating to patient (age, BMI, comorbidities and MH) and surgical (femoral component offset) characteristics at the time of surgery, this is greatly outweighed by the substantial change in OHS achieved by these patients, regardless of whether they are old or young, obese or not obese. These patient groups still receive great benefit from surgery.
Figure 3.
Change in Oxford Hip Score over time, stratified by predictive variables.
Assessing the discriminatory ability of the final model including the baseline OHS alone explained 10.3% of the variability in outcome. The final predictive model including the patient and surgical variables explained 16.6%. This suggests that although we have identified significant patient and surgical predictors of the outcome, they have smaller effects and explain little of the variability in attained postoperative OHS above that of the baseline score.
Discussion
Main findings
Within a large prospective cohort of patients receiving primary THR in the UK, we identified a number of predictors of differences in attained postoperative pain and function. Determinants included: preoperative pain and function—those with worse preoperative pain/function had worse postoperative pain/function; femoral component offset—women with an offset of 44 or more had better outcomes, age—compared to those aged 50–60, younger patients (age <50) and older patients (age >60) had worse outcome, increasing BMI, a greater number of coexisting diseases and worse SF-36 MH at the time of surgery was related to worse postoperative pain and function. The strongest determinant of outcome was the baseline score with the patient and surgical variables contributing small but statistically significant effects.
Assessing the relationship of change in symptoms of pain and function between preoperative and postoperative assessments for predictor variables in the final model revealed that patients achieved large symptomatic improvement (change), regardless of differences in preoperative patient and surgical factors. The change in symptoms greatly outweighs any differences in attained postoperative score—patients achieved great benefit from surgery regardless of factors such as their age and BMI at the time of surgery. Exploring temporal trends in symptoms of pain and function over time demonstrated that there was neither little further improvement nor decline in the short-term to mid-term (between 1-yearand 5-year follow-up) where a steady symptomatic state was reached.
Strengths and limitations
The strength of this study lies in its large sample size and repeated measures of a reliable, valid and responsive instrument for assessing outcomes of THR,28 29 with data collected prospectively over 5 years with a good rate of follow-up. The use of multiple imputation and bootstrapping as an internal validation technique is a strength of this study, ensuring that the predictors we identified are those most likely to be replicated in external validation studies and not chance significant findings that are anomalies of our dataset. Within this study, the aim was to identify predictors of differences in attained postoperative pain and function—it should be noted that the predictors we identified of attained health state may not necessarily be the same as the predictors of improvement (change) in symptoms. It should be noted that it remains unclear which measure of the two outcomes of change in status or attained status is most appropriate for judging the value of surgery35—THR could either be viewed as intended to preserve the highest levels of pain function or alternatively to maximise the potential for symptomatic improvement. The limitations are that other potential predictive variables were not available in this study, predominantly radiographic factors such as x-ray grade and pattern of OA and other factors including patient expectations of surgery and the type and extent of joint damage. Response bias may play a role, as responders were younger and had better preoperative SF-36 MH scores; hence, the true effects of these predictors may be underestimated in this study.
Within this study, histograms of the absolute difference (change) in scores between preoperative and postoperative assessments highlight that almost all patients get better with only a small minority getting worse or receiving no improvement (2.3% by 1 year and 1.2% by 5 years). This is set in the context that data in the study come from seven high volume centres with skilled surgeons across England and Scotland and raise the possibility that outcomes in this study may be better than expected. Comparing this finding with data from other cohorts, in the European Collaborative Database of Cost and Practice Patterns of Total Hip Replacement (EUROHIP) study consisting of THR patients across 20 European orthopaedic centres, based on the change in Western Ontario and McMaster Universities Osteoarthritis score (WOMAC) score at 12 months, 58 (6.9%) of 845 patients had no change or a worsening of symptoms—although this varied by region— and in patients from the UK, only 4 (3.5%) of 111 patients had no change or got worse. In data from the Elective Orthopaedic Centre database that include primary hip replacements performed in four acute National Health Service trusts in the UK in South West London, 88 (5.1%) of 1711 patients symptoms got worse after 6 months based on the OHS, and in data from St. Helier district general hospital, Carshalton, UK, 14 (2.3%) of 619 patients had no change or a worsening in OHS at 12 months. Hence, while it is plausible that outcomes in the EPOS may be better than expected, the findings are consistent with other cohorts.
What is already known?
In our study, an important new finding was that a larger femoral component offset is associated with better outcomes of THR. We hypothesised that the effect of offset size may be explained by an interaction with gender, as men have larger offsets. A significant interaction was observed, where no association was observed in men, while in women those with larger offsets had better outcomes. The choice of offset can affect hip stability as well as abduction strength, potentially resulting in abnormal (trendelenburg) gait. Component offset may be preoperatively templated, although common offsets are often assumed (ie, 37.5 mm for females and 44 mm for males). There is greater potential to decrease offset in females, partly because of the above assumption, and it is sometimes difficult to use the larger offset components because a smaller femoral canal diameter precludes their use. The choice of offset for the femoral component has not changed since this study was conducted, and these findings are generalisable to clinical practice. We are not aware of any data in the literature describing the relationship of intraoperative surgical factors on patient-reported outcomes. Within the literature, data exist on the relationship between head size and failure of a THR, whereby a larger head size (40 mm vs 28 mm) with a ceramic-on-ceramic bearing surface was associated with lower 5 year revision rates.36 This is thought to be related to larger diameter heads increasing fluid-film lubrication, in turn reducing wear, and decreasing dislocation rates.36 However, femoral component offset and head size are independent factors that are unrelated to one another. Within this study, we found no association between head size and patient-reported outcomes—this is unsurprising since the head sizes used were 22, 26 and 28 mm and common to orthopaedic practice at the time this study took place. Thinner liners are now manufactured allowing larger head sizes to be used in acetabular components of the same size.
Consistent with other studies in the literature, we observed that worse preoperative MH was a predictor of poor outcome16 as were greater numbers of preoperative comorbidities.8 15 We found that older age and higher BMI were associated with worse patient-reported outcomes. Within the literature, while some authors conclude that older age and increasing BMI area were associated with worse outcomes, others have found no evidence of an association.7–9 12–19 31 37 This is in line with the conclusions of large literature reviews stating that such factors are not strong predictors of outcome.11 The findings are important for decision making as physicians often advise patients that they are too old or obese to receive THR.11 38 We can conclude that in relation to patient-reported outcomes of THR, even if some groups fare less well after THR, it does not mean these patients do not get benefit from surgery.11 Expectations of patients may also play a role;, for example, what a young person wants to achieve in functional rehabilitation is different from the wants of an older person, for whom a lower functional score may be perfectly acceptable. It is also well known within the literature that patients with better preoperative pain and function achieve better attained postoperative pain and function and that patients with worse preoperative pain and function get the greatest change (symptomatic improvement) between baseline and follow-up.8 12–16
While the effects of preoperative patient characteristics including age, BMI, coexisting diseases and MH may already be known within the existing literature, what is novel about this study is contrasting the effects of these factors on attained levels of postoperative scores with a graphical representation of change (improvement in scores). Our findings highlight that small but significant differences in attained scores are greatly outweighed by the fact that these patient groups get great benefit from surgery (in terms of substantial change in symptoms of pain and function), regardless of the differences in preoperative patient characteristics.
Within this study, although we examined a wide range of patient and intraoperative surgical factors, we were only able to explain around 17% of the variability in patient-reported outcomes of THR. Data were not available to us on other factors known within the literature to be predictive of outcomes of THR such as radiographic information and the presence of musculoskeletal disease in other joints. It has previously been shown that patients with pain in other joints39 have worse outcomes. Patients with worse preoperative x-rays are more likely to improve.13 14 Worse outcomes have been observed in patients who live alone,15 19 those with less social support31 and patients with lower educational attainment.8 12 14 18 Patients with greater preoperative expectations of surgery have been observed to have better outcomes.14 20 While inclusion of such factors would help to improve the predictive ability of the model, as individual factors of interest, it is quite likely that we would see the same pattern whereby small differences are seen in attained score but patients achieve benefit.
What this study adds?
Within this study, we have identified a number of patient and surgical predictors of attained postoperative pain and function following THR surgery. These predictors remain related to outcome over the short-to-midterm. An important new finding was that a larger femoral component offset was associated with better postoperative pain and function in women. This finding implies that greater consideration should be given to measuring and deciding upon the choice of offset in women as there is potential to undersize. While age, BMI, coexisting diseases, MH and femoral component offset were associated with small but significant differences in attained pain and function, analyses of change demonstrate that these patients still achieve substantial symptomatic benefit from surgery regardless of the differences in these preoperative factors. The findings will be important to inform patients and clinicians’ decisions regarding the likely outcomes of surgery for these patient groups. Although we have assessed a wide range of patient characteristics and intraoperative surgical factors, there is still uncertainty as to the cause of variation in outcomes of hip replacement. There is a need to focus on issues that remain unclear such as the effect of soft tissue and the severity and pattern of OA. Further research is needed using more detailed measures of existing predictive variables and identification of other factors beyond those observed in this study that explain a greater proportion of the variability in outcome to improve our ability to identify patients at risk of poor outcomes from THR surgery.
Supplementary Material
Footnotes
Collaborators: The following people are the main investigators of the Exeter Primary Outcomes Study (EPOS) group: Professor D Murray, Mr G Andrew, Mr P Gibson, Mr J Nolan, Mr A Hamer, Mr M Fordyce and Mr K Tuson. Dr DJ Beard is a member of the EPOS steering group and scientific advisor. The following people are study coordinators for the EPOS group: Anne Potter, Ann McGovern, Kathleen Reilly, Cathy Jenkins, Adele Cooper, Clare Darrah, Lynne Cawton, Praveen Inaparthy and Clare Pitchfork.
Contributors: AJ, NKA, RNB, GT, DB, MKJ, CC and DM were involved in: (1) substantial contributions to conception and design, analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content and (3) final approval of the version to be published.
Funding: This article presents independent research commissioned by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research funding scheme (RP-PG-0407–10064). The views expressed in this article are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. This study has been supported by Stryker Howmedica Osteonics (Newbury, UK). Support was also received from the Oxford NIHR Musculoskeletal Biomedical Research Unit, Nuffield Orthopaedic Centre, University of Oxford and the UK Medical Research Council, Medical Research Council Lifecourse Epidemiology Unit, University of Southampton.
Competing interests: All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that: AJ, RNB and GT have no conflicts of interest; MKJ, NKA, and CC have received honorariums, held advisory board positions (which involved receipt of fees) and received consortium research grants, respectively, from: Novartis and Alliance for Better Health and Lilly; Merck, Merck Sharp and Dohme, Roche, Novartis, Smith and Nephew, Q-MED, Nicox, Servier, GlaxoSmithKline, Schering-Plough, Pfizer, and Rottapharm; and Alliance for Better Bone Health, Amgen, Novartis, Merck Sharp and Dohme, Servier, Eli Lilly and GlaxoSmithKline; DB has held an independent consultancy with ICNet and Stryker and has been a grant holder on a Genzyme-funded study; DM has received royalties from Biomet and Wright Medical Technology, Inc and receives research support from DePuy, A Johnson & Johnson Company, Stryker, Zimmer and Wright Medical Technology, Inc; they have no other relationships or activities that could appear to have influenced the submitted work.
Ethics approval: Ethical approval was obtained from the Salford and Trafford Research Ethics Committee (Project No.98105—MREC 98/8/20 UK Multicentre Exeter Primary Outcome Study). Informed written consent was obtained from all the participants.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
Contributor Information
Collaborators: D Murray, G Andrew, P Gibson, J Nolan, A Hamer, M Fordyce, K Tuson, DJ Beard, Anne Potter, Ann McGovern, Kathleen Reilly, Cathy Jenkins, Adele Cooper, Clare Darrah, Lynne Cawton, Praveen Inaparthy, and Clare Pitchfork
References
- 1.Harris WH, Sledge CB. Total hip and total knee replacement (1). N Engl J Med 1990;323:725–31 [DOI] [PubMed] [Google Scholar]
- 2.Harris WH, Sledge CB. Total hip and total knee replacement (2). N Engl J Med 1990;323:801–7 [DOI] [PubMed] [Google Scholar]
- 3.Ethgen O, Bruyere O, Richy F, et al. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 2004;86:963–74 [DOI] [PubMed] [Google Scholar]
- 4.Cooper C, Arden NK. Excess mortality in osteoarthritis. BMJ 2011;342:d1407. [DOI] [PubMed] [Google Scholar]
- 5.Professor the Lord Darzi of Denham Kbe HonFREng FmedSci High quality care for All. NHS next stage review final report—summary: Department of Health, 2008
- 6.Williams O, Fitzpatrick R, Hajat S, et al. Mortality, morbidity, and 1-year outcomes of primary elective total hip arthroplasty. J Arthroplasty 2002;17:165–71 [DOI] [PubMed] [Google Scholar]
- 7.Nilsdotter AK, Petersson IF, Roos EM, et al. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis 2003;62:923–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacWilliam CH, Yood MU, Verner JJ, et al. Patient-related risk factors that predict poor outcome after total hip replacement. Health Serv Res 1996;31:623–38 [PMC free article] [PubMed] [Google Scholar]
- 9.Judge A, Cooper C, Williams S, et al. Patient-reported outcomes one year after primary hip replacement in a European Collaborative Cohort. Arthritis Care Res 2010;62:480–8 [DOI] [PubMed] [Google Scholar]
- 10.Hawker GA. Who, when, and why total joint replacement surgery? The patient's perspective. Curr Opin Rheumatol 2006;18:526–30 [DOI] [PubMed] [Google Scholar]
- 11.Santaguida PL, Hawker GA, Hudak PL, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg 2008;51:428–36 [PMC free article] [PubMed] [Google Scholar]
- 12.Fortin PR, Clarke AE, Joseph L, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum 1999;42:1722–8 [DOI] [PubMed] [Google Scholar]
- 13.Cushnaghan J, Coggon D, Reading I, et al. Long-term outcome following total hip arthroplasty: a controlled longitudinal study. Arthritis Rheum 2007;57:1375–80 [DOI] [PubMed] [Google Scholar]
- 14.Judge A, Cooper C, Arden NK, et al. Pre-operative expectation predicts 12-month post-operative outcome among patients undergoing primary total hip replacement in European orthopaedic centres. Osteoarthritis Cartilage 2011;19:659–67 [DOI] [PubMed] [Google Scholar]
- 15.Jones CA, Voaklander DC, Johnston DW, et al. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med 2001;161:454–60 [DOI] [PubMed] [Google Scholar]
- 16.Quintana JM, Escobar A, Aguirre U, et al. Predictors of health-related quality-of-life change after total hip arthroplasty. Clin Orthop 2009;467:2886–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Braeken AM, Lochhaas-Gerlach JA, Gollish JD, et al. Determinants of 6–12 month postoperative functional status and pain after elective total hip replacement. Int J Qual Health Care 1997;9:413–18 [DOI] [PubMed] [Google Scholar]
- 18.Rissanen P, Aro S, Sintonen H, et al. Quality of life and functional ability in hip and knee replacements: a prospective study. Qual Life Res 1996;5:56–64 [DOI] [PubMed] [Google Scholar]
- 19.Hopman WM, Mantle M, Towheed TE, et al. Determinants of health-related quality of life following elective total hip replacement. Am J Med Qual 1999;14:110–16 [DOI] [PubMed] [Google Scholar]
- 20.Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty 2009;24:716–21 [DOI] [PubMed] [Google Scholar]
- 21.Andrew JG, Palan J, Kurup HV, et al. Obesity in total hip replacement. J Bone Joint Surg Br 2008;90-B:424–9 [DOI] [PubMed] [Google Scholar]
- 22.Palan J, Beard D, Murray D, et al. Which approach for total hip arthroplasty: anterolateral or posterior? Clin Orthop 2009;467:473–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palan J, Gulati A, Andrew JG, et al. The trainer, the trainee and the surgeons’ assistant: clinical outcomes following total hip replacement. J Bone Joint Surg Br 2009;91-B:928–34 [DOI] [PubMed] [Google Scholar]
- 24.Hossain M, Parfitt D, Beard D, et al. Does pre-operative psychological distress affect patient satisfaction after primary total hip arthroplasty? BMC Musculoskelet Disord 2011;12:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br 1972;54-B:61–76 [PubMed] [Google Scholar]
- 26.D'Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 1954;36:451–75 [PubMed] [Google Scholar]
- 27.Ware JE. How to score the revised MOS Short Form Health Scales. Boston: The Health Institute, New England Medical Centre Hospital, 1988 [Google Scholar]
- 28.Murray DW, Fitzpatrick R, Rogers K, et al. The use of the Oxford Hip and Knee Scores. J Bone Joint Surg Br 2007;89-B:1010–14 [DOI] [PubMed] [Google Scholar]
- 29.Dawson J, Fitzpatrick R, Carr A, et al. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br 1996;78-B:185–90 [PubMed] [Google Scholar]
- 30.Royston P. Multiple imputation of missing values: update of ice. The Stata J 2005;5:527–36 [Google Scholar]
- 31.Fitzgerald JD, Orav EJ, Lee TH, et al. Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum 2004;51:100–9 [DOI] [PubMed] [Google Scholar]
- 32.Vergouw D, Heymans M, Peat G, et al. The search for stable prognostic models in multiple imputed data sets. BMC Med Res Methodol 2010;10:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heymans M, van Buuren S, Knol D, et al. Variable selection under multiple imputation using the bootstrap in a prognostic study. BMC Med Res Methodol 2007;7:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Royston P, Moons KG, Altman DG, et al. Prognosis and prognostic research: developing a prognostic model. BMJ 2009;338:b604. [DOI] [PubMed] [Google Scholar]
- 35.Losina E, Katz JN. Total knee replacement: pursuit of the paramount result. Rheumatology (Oxford) 2012;51:1735–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith AJ, Dieppe P, Vernon K, et al. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet 2012;379:1199–204 [DOI] [PubMed] [Google Scholar]
- 37.Harse JD, Holman CD. Charlson's index was a poor predictor of quality of life outcomes in a study of patients following joint replacement surgery. J Clin Epidemiol 2005;58:1142–9 [DOI] [PubMed] [Google Scholar]
- 38.Hawker G, Wright J, Coyte P, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am 1998;80:163–73 [DOI] [PubMed] [Google Scholar]
- 39.Judge A, Javaid MK, Arden NK, et al. A clinical tool to identify patients who are most likely to receive long term improvement in physical function after total hip arthroplasty. Arthritis Care Res 2012;64:881–9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.