Abstract
Based on positive deviance (examining the practices of successful individuals), we identified five primary themes from 36 strategies that help to maintain long-term weight loss (weight control) in 61 people. We conducted in-depth interviews to determine what successful individuals did and/or thought about regularly to control their weight. The themes included weight-control practices related to (a) nutrition: increase water, fruit, and vegetable intake, and consistent meal timing and content; (b) physical activity: follow and track an exercise routine at least 3×/week; (c) restraint: practice restraint by limiting and/or avoiding unhealthy foods; (d) self-monitor: plan meals, and track calories/weight progress; and (e) motivation: participate in motivational programs and cognitive processes that affect weight-control behavior. Using the extensive data involving both the practices and practice implementation, we used positive deviance to create a comprehensive list of practices to develop interventions for individuals to control their weight.
Keywords: interviews, semistructured, obesity / overweight, weight management
Long-term weight control is a goal for many Americans; however, weight loss and maintenance remain significant challenges (National Heart, Lung, and Blood Institute [NHLBI], 2000; Wadden, Butryn, & Wilson, 2007). Currently, 66% of Americans are overweight, with a body mass index (BMI) > 25 kg/m2, or obese, with a BMI > 30 kg/m2 (Ogden, Carroll, McDowell, & Flegal, 2007). Being overweight or obese increases the risks of many chronic medical conditions, including type 2 diabetes, heart disease, and stroke (NHLBI, 1998). One of the major difficulties of weight control for many Americans is that it represents a lifelong process. Successful weight control is increasingly viewed as a chronic medical condition, similar to diabetes and hypertension, which needs ongoing treatment (Ely et al., 2008; Logue et al., 2005; Rhodes, Bookstein, Aaronson, Mercer, & Orringer, 1996).
Behavioral interventions, through the combination of nutrition and exercise education and behavioral strategies, are the cornerstone of obesity treatment today (Burke et al., 2009; NHLBI, 2000; Wadden et al., 2007). The Diabetes Prevention Program (DPP) is an example of a behavioral intervention conducted with 3,200 overweight individuals (Knowler et al., 2002). Participants received 16 individual treatment sessions, conducted by registered dietitians, focusing on curricula designed to increase physical activity and decrease caloric intake. Participants in the lifestyle intervention lost an average of 5.6 kg, significantly more weight than the first-line oral drug of choice for type 2 diabetes treatment (metformin) or the control groups. In addition to the DPP, a recent review on the effectiveness of worksite nutrition and physical interventions for overweight and obese employees was conducted. The review included 47 studies (using mostly informational and behavioral strategies) in which there was a modest, pooled improvement in weight status (Anderson et al., 2009). The Internet has also been utilized successfully as a delivery mode for promoting health behavior change and eliciting weight loss (Krukowski, West, & Harvey-Berino, 2009; Webb, Joseph, Yardley, & Michie, 2010).
The most appropriate diet to recommend for weight loss has long been debated by nutritional experts, particularly in terms of macronutrient composition (Gardner et al., 2007; Sacks et al., 2009). Researchers from the A to Z Weight Loss Study, a randomized controlled trial of 311 overweight/obese women, found that participants assigned to the Atkins diet (characterized by low carbohydrate intake) lost more weight than those assigned to follow the Zone, Ornish, or LEARN diets (Gardner et al.). However, in a more recent study of 811 overweight adults assigned to one of four diets with varying compositions of fat, protein, and carbohydrates, researchers found that any reduced-calorie diet produced clinically meaningful weight loss (Sacks et al.). Secondary data analysis of the A to Z Weight Loss Study was conducted, and researchers again concluded that weight change was greater in the most adherent as compared to the least adherent participants, regardless of dietary group assignment (Alhassan, Kim, Bersamin, King, & Gardner, 2008).
Although both nutritional and behavioral approaches for weight control lead through a final common pathway of limiting caloric intake and/or increasing caloric expenditure, the number of potential practices used to achieve these ends are numerous and varied. Much of what is known about the weight-control practices that aid in weight loss maintenance has come from studies of subjects in the National Weight Control Registry (NWCR). The NWCR is a long-term study of more than 6,000 adults who have maintained a weight loss of at least 30 pounds for at least 1 year. The NWCR has been used, for example, to learn that those who are more successful tend to weigh themselves more often (Butryn, Phelan, Hill, & Wing, 2007), eat breakfast more often (Wyatt et al., 2002), self-monitor their intake and activity more often, exercise more (McGuire, Wing, Klem, Lang, & Hill, 1999), eat a lower-fat diet (McGuire et al.; Wyatt et al., 1999), eat a limited variety of food groups (Raynor, Jeffery, Phelan, Hill, & Wing, 2005), and watch less television (Raynor, Phelan, Hill, & Wing, 2006).
The design of the NWCR, specifically the lack of qualitative research used to inform the list of weight-control practices, has limited its ability to identify the full range of effective weight-control practices. However, qualitative research has been conducted in the area of weight control. The first published report of a community sample of successful dieters dates back to the studies of Colvin and Olson, which included qualitative interviews but did not identify a comprehensive set of weight-control practices (Colvin & Olson, 1983, 1984). Another qualitative study, the Successful Dieters Research Project, was designed to explore and describe successful dieters using an open-ended, semistructured interview (Brink & Ferguson, 1998). That study included successful dieters, defined as now normal-weight individuals who had lost at least 20% of initial body weight and maintained this loss for at least one year, contrasted with unsuccessful dieters. The decision to lose weight and the reasons for this decision, namely health and appearance, were similar between groups. Actual weight loss activities were not explored. A naturalistic field study with intensive interviewing techniques by Tyler and colleagues included 40 African American and 40 Euro American women (Tyler, Allan, & Alcozer, 1997). All 80 study participants reported trying to lose weight at some point in their life, and a total of 20 types of weight-loss methods were identified. The methods were divided into three categories: lifestyle work, head work, and professional services. Both African American and Euro American women reported using similar types and numbers of methods. However, the weight loss methods were not evaluated in terms of successful or unsuccessful dieters, but rather as a descriptive analysis of use in general (Tyler et al.). Additional qualitative work by Allan described the process of weight management in women, defining five stages: appraising, deemphasizing, mobilizing, enacting, and maintaining (1991). In a more recent study, Byrne and colleagues also performed qualitative interviews with successful individuals but focused on the psychological characteristics of successful individuals, and similarly did not seek to identify a comprehensive set of weight-control practices (Byrne, Cooper, & Fairburn, 2003). In addition, none of these qualitative studies included in-situ observation of individuals, an important qualitative method to identify commonly used practices (Baptiste, 2001; Byrne et al.; Colvin & Olson, 1983, 1984). As a result, research focused on identifying effective weight-loss practices does not typically include behaviors generated by people successful at weight control, but rather those behaviors determined to be important by experts in the field.
Several studies have been conducted to determine factors that influence weight control (Booth, Blair, Lewis, & Baek, 2004; Harvey-Berino, 1999; Qi & Dennis, 2000; Wing et al., 2007). Booth and colleagues determined that the behavior with the greatest influence on year-long weight loss was avoiding calorie-containing drinks and foods at the ends of and between meals (snacking). In a 24-week behavioral weight-loss program (Harvey-Berino), researchers similarly found a greater decrease in the percentage of body fat and resting metabolic rate for a low-calorie intake group and persistent decreases in body fat at 18 months. The important message was that calories do count in weight control. Likewise, Qi and Dennis studied eating behaviors conducive to weight loss in a 6-month behavior modification, dietary, low-intensity walking, weight-loss program. Those who were successful increased their total eating behavior score by 20% and improved the adoption of 14 positive eating behaviors, which was more than twice that of those who did not lose weight. Maintaining a weight graph and weighing daily also were important strategies. Reporting on the STOP Regain clinical trial (Wing et al.), researchers reported that increases in daily self-weighing were associated with successful weight-loss maintenance.
Several measures have been created to identify successful practices for short-term weight loss, such as the Eating Behaviors Inventory (EBI); however, none of these has been created by studying individuals successful at losing weight (Jeffery & French, 1996, 1999; Nothwehr, Dennis, & Wu, 2007; Nothwehr & Peterson, 2005; O’Neil et al., 1979). The EBI is used to sample the domain of behaviors that have been theoretically implicated in weight loss in behavioral weight-loss programs selected from a survey of treatment manuals (O’Neil et al., 1979). Only one study in the weight loss literature was used to assess dietary, exercise, and social practices specified by individuals from a study population for health or weight control (Blair, Lewis, & Booth, 1994), even though the merits of using respondents’ own wording in questionnaire items has long been recommended (Booth et al., 2004; Fishbein & Ajzen, 1975).
Over the past 20 years, an approach has emerged in which intensive qualitative research is used to learn the behaviors of those who have succeeded, and to later disseminate these behaviors. This approach is called positive deviance and has been used to improve many different problems, including business practices (Collins, 2001), infection rates (Hopkins & Withers, 2002), immunization programs (Naimoli, Challa, Schneidman, & Kostermans, 2008), and teaching skills (Reid, 1999). Positive deviance differs from the approach used by the National Weight Control Registry (NWCR) and similar measures that are employed in a “top-down” manner. In a top-down approach, professionals create the list of practices, whereas in positive deviance a “bottom-up” approach is used through qualitative inquiry to identify those practices (Awofeso, Irwin, & Forrest, 2008; Friedman, Mateu-Gelabert, Sandoval, Hagan, & Des Jarlais, 2008). The purpose of this article is to describe how the use of positive deviance was effective in identifying 36 practices used in successful weight control, which also will be used to guide future weight-loss interventions.
Conceptual Framework
Positive deviance is an inductive approach to determine successful practices of individuals who succeed where most tend to fail. The method includes examining the practices and behaviors of individuals within a community who, with the same resources, have achieved better results than their peers (Fowles, Hendricks, & Walker, 2005). Researchers who use the established principle of positive deviance in health care take an inductive, rather than deductive, framework to determine practices for weight control. In an inductive framework, specific observations lead to broader generalizations and theories, also known as a bottom-up approach. The central premise of positive deviance is that solutions to a problem that face a population often exist within that population, and that members possess experience that can be generalized to improve the performance of other members. Positive deviance is inductive and qualitative in nature because it uses the experiences of individuals who have better health outcomes than the majority, and analyzes their behaviors to determine what practices they used to promote successful outcomes (Timmerman, 2007).
Although positive deviance has been applied to health outcomes for 35 years (Smith, 1975), to our knowledge this is the first study published in Qualitative Health Research in which researchers have used positive deviance to explain the determination of successful practices. Several researchers have used inductive approaches in the study of weight control, including the analysis of food journals (Burke, Swigart, Warziski Turk, Derro, & Ewing, 2009), the examination of immigrant parents’ responses to existing public health educational materials and strategies for weight control (Ferrari, Tweed, Anneke Rummens, Skinner, & McVey, 2009), and the experiences of women who were classified as overweight while they participated in a physical activity intervention (Sabiston, McDonough, Sedgwick, & Crocker, 2009), but none cited the use of positive deviance to examine the practices of successful individuals.
Positive deviance has been used by researchers to identify and disseminate effective methods for purposes as varied as improving smoking cessation programs in Australia (Awofeso et al., 2008), improving methods for teaching students to read (Reid, 1999), decreasing hepatitis C transmission (Friedman et al., 2008), dealing with barriers to health-promotion interventions to improve behavior change in underserved women (Timmerman, 2007), reducing parasite infection (Hopkins & Withers, 2002), improving immunization programs in Africa (Naimoli et al., 2008), and improving birth weight in Egypt (Ahrari et al., 2006). In a study of the long-term avoidance of infection in drug users, the participants identified multiple goals that contributed to remaining uninfected, including balancing the need for drugs and income, developing ways to avoid drug-withdrawal sickness, avoiding situations in which other drug users share drugs, and avoiding HIV (Friedman et al.). In the application of positive deviance to a population of low-income pregnant women (n = 18), Fowles and colleagues (2005) determined that those with nutritionally adequate diets (as defined using the food pyramid scale and dietary recall) knew to eat balanced meals, had family support, were willing to prepare foods that were different than other family members, and ate at home more frequently than women with inadequate diets. The transcripts and field notes were used to identify nutritional behaviors and practices of women with adequate vs. inadequate dietary scores. Six of the 18 women had a dietary score of 19 or greater, indicating they had a nutritionally adequate diet and were classified as positive deviants. In a specific example, the positive deviants consumed a variety of foods from all the food groups, whereas the women who did not consume a balanced diet typically ate foods from one or two food groups, such as meat and bread, but not from the fruit and vegetable groups. Positive deviance practices are based on proven, successful implementation of behaviors within the community, rather than concepts that are deduced from theoretical principles.
Methods
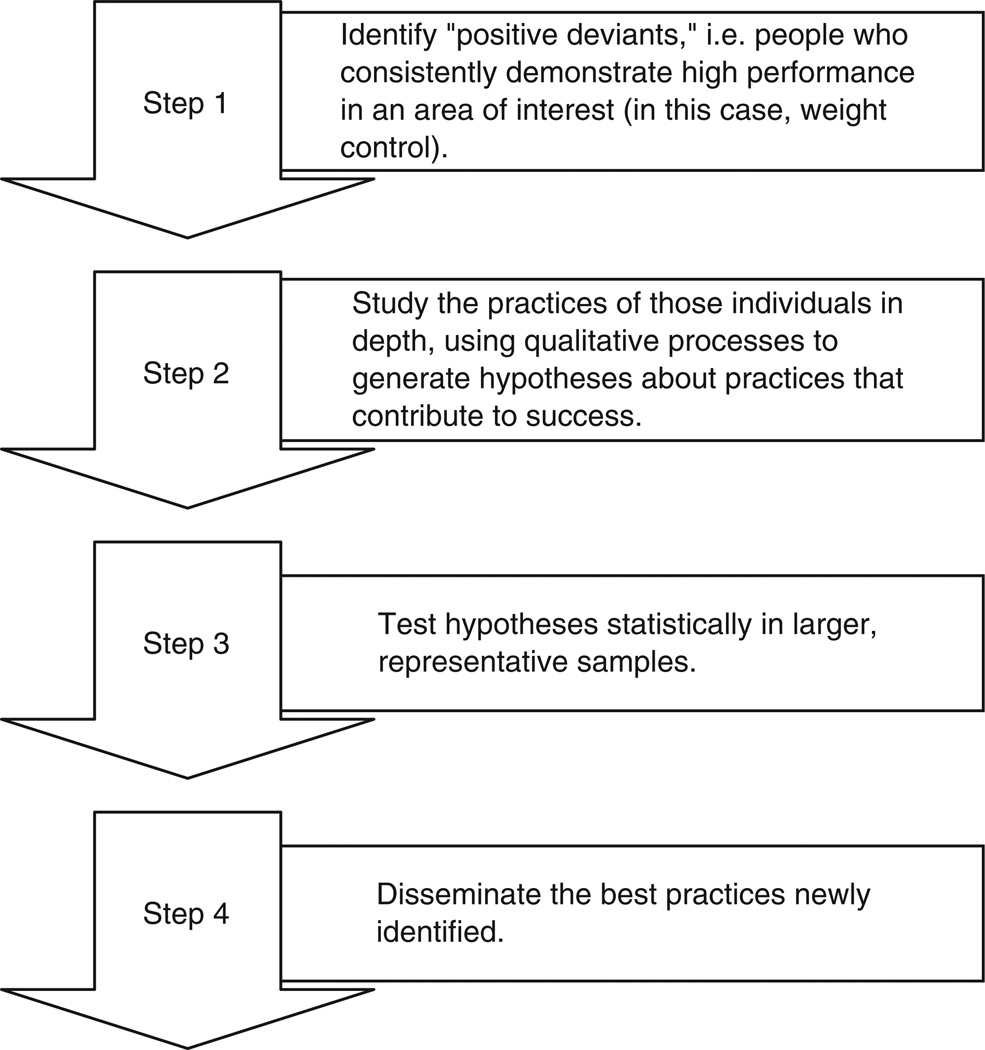
The application of positive deviance involves four steps (see Figure 1), including (a) sampling strategy, (b) qualitative data collection and analysis, (c) testing in a representative sample, and (d) dissemination of best practices (Bradley et al., 2009). The first step, the sampling strategy, is included in the Methods section of this article. The second step, qualitative data collection and analysis, is listed in the Results section. The purpose of this article is to examine how the qualitative data contribute to what is known about the practices implemented by those successful in weight control and, therefore, the second step is emphasized. However, we have plans for steps (c) testing and (d) dissemination of our research. We are currently running a randomized controlled trial (n = 100) to determine if adding and setting goals for each of the successful practices identified in this study will assist in weight control in a larger population, and the results will be disseminated upon completion.
Figure 1.
Four steps of positive deviance (Bradley et al., 2009)
Participants (Sampling Strategy)
Positive deviance requires the identification of positive deviants (i.e., people who consistently demonstrate exceptionally high performance in an area of interest). Our purposeful sampling strategy included recruiting individuals who were successful with long-term weight control, using inclusion criteria similar to that used by the NWCR (Klem, Wing, McGuire, Seagle, & Hill, 1997). The participants (n = 61) were screened for eligibility using the following criteria: (a) lost 30 pounds or more and maintained the weight loss for 1 year or more; (b) age greater than 21; (c) not pregnant; (d) English speaking, and (e) did not have bariatric surgery. The majority of participants were women (72%), White (79%), and well educated (90% had at least some college). Nearly half were single (never married, widowed, or divorced), and the majority reported their general health as “fair” (52%). Eighty-five percent (85%) of the participants lost all of their weight intentionally, and 12% lost most of it intentionally; all participants maintained the loss for at least 1 year. Approval for the research was obtained from the Pennsylvania State University College of Medicine Institutional Review Board.
Qualitative Data Collection
The in-depth examination of a participant’s behaviors, attitudes, and barriers typically requires the collection of inductive, qualitative data (Patton, 2002). In line with the principles of positive deviance, we developed an in-depth interview script based on open-ended questions about successful practices and cognitions that were used to control weight. The two primary questions were based on principles of cognitive-behavioral therapy (Beck, 1979), and included, “What do you do regularly that you think helps you to lose weight or to maintain a healthy weight?” and “What do you think about or remind yourself regularly that you think helps you lose weight or to maintain a healthy weight?”
A 20-minute telephone call was conducted with the 61 participants who were successful at losing and maintaining weight, using the script to develop a comprehensive list of overall practices that were used. Interviewers probed for the what, when, where, and how of each practice. Because self-aware responses to questions of “why?” are more difficult to access, questions relating to the reasons a respondent engaged in a practice were probed with at least 2 to 3 follow-up questions (Rubin & Rubin, 2004). Additionally, interviewers were vigilant to listen for causal statements in respondents’ statements. This ensured that the description of each practice would be clear enough to tell someone else exactly how to use this practice. Interviewers attempted to learn of as many practices as possible from each participant. We anticipated that different people would use different words to describe the same behavior, so we believed that information regarding intent would allow us to combine practices mentioned by more than one individual into a common theme. The in-depth interviews were audiotaped, saved on a digital file in a deidentified form, and transcribed verbatim. Three expert reviewers independently checked the accuracy of transcripts with the original audio files. After correcting any transcription errors and assuring accuracy, the reviewers commenced with coding each individual transcript to identify practices used to successfully maintain long-term weight loss.
Data Analysis
An inductive qualitative analysis was conducted to identify practices for successful weight control and explore themes linking these practices (see Figure 2). First, from each individual interview transcript, phrases that related to weight-control practices were identified and listed in a computer spreadsheet. More than 95 different practices for maintaining weight control were identified from approximately 90 hours of audiotaped, transcribed responses. Responses ranged from “participating in a weight-loss program” to “thinking about your goal for a healthy weight.” Analogous responses were considered for conceptual similarity and, if the expert reviewers determined the practice to be conceptually similar but described differently, the phrases were combined and assigned a discrete practice label. For example, the statements “I control my portions” and “I limit the amount I eat at each meal” were considered conceptually similar. The expert reviewers incorporated both statements into this particular practice and labeled it “Control your portions or limit the amount of food you eat at each meal.”
Figure 2.
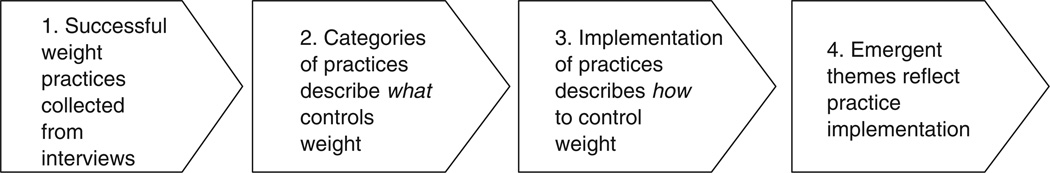
Inductive process of data analysis
Another example of response assignment is when responses indicated a similar practice, but indicated varied frequency of use; e.g., “I weigh myself every day” and “I weigh myself often” were combined into the practice labeled “weighing yourself.” These responses were collapsed into one practice because we believed the individual variability in frequency (daily, weekly, and so forth) was less important than the general act of self-monitoring (“weigh yourself”). Some responses indicated extremely different practices, and this required us to assign the responses to mutually exclusive practices or create a new practice to reflect the described behavior (e.g., “follow a consistent exercise regimen” and “do different types of exercise”). The data were not forced into preconceived themes, but instead an open-coding approach of emergence was employed so that interview data guided the creation of the categories (Creswell, 1998). Saturation of each category was important so as to account for all responses to the interview question. All coding decisions were discussed with an independent researcher and a consensus agreement was maintained. Practices used by at least 10% of the individual participants were included in the final list of 36 practices (see Table 1) to balance the scope of the practices with subject burden of repeatedly answering long survey instruments.
Table 1.
Five Themes and 36 Practices That Contribute to Weight Loss and Maintenance
| Theme | Use Often/ Occasionally (%) |
|---|---|
| Theme:1: Nutrition | |
| Drink plenty of water | 97 |
| Read nutrition labels | 97 |
| Eat plenty of fruits or vegetables | 93 |
| Eat healthy snacks | 93 |
| Eat plenty of low-fat sources of protein, such as fish, chicken, or beans | 92 |
| Avoid skipping a meal, including breakfast, or going too long without food | 87 |
| Eat about the same thing at each meal or snack | 80 |
| Theme 2: Physical Activity | |
| Do exercises that you enjoy | 92 |
| Follow a consistent exercise routine | 87 |
| Try to fit exercise into your lifestyle (walking/biking instead of driving, taking the stairs instead of an elevator) | 87 |
| Walk for exercise | 87 |
| Do different kinds of exercises | 79 |
| Exercise with other people | 70 |
| Write down how much you exercise each day | 41 |
| Theme 3: Restraint | |
| Limit the amount of sugar you eat or drink, such as cookies, desserts, sweets, or soda | 100 |
| Replace high-calorie foods or drinks with those that have fewer calories | 93 |
| Limit the amount of unhealthy food in your home | 92 |
| Control your portions or limit the amount of food you eat at each meal | 92 |
| Think about not overeating while you are eating a meal | 87 |
| Allow yourself to eat a small amount of some unhealthy foods, such as sweets, that you really like | 85 |
| Limit the amount of carbohydrates or “carbs” you eat, such as breads, pasta, rice, potatoes, and crackers | 72 |
| Avoid eating or drinking too much while eating out | 62 |
| Theme 4: Self-Monitoring | |
| Plan what you’ll buy before you get to the grocery store | 97 |
| Plan what you’ll eat ahead of time | 82 |
| Weigh yourself | 69 |
| Write down what you eat and drink | 48 |
| Theme 5: Motivation | |
| Remind yourself why you need to control your weight | 97 |
| Notice how many people are overweight | 97 |
| Think about your goal for a healthy weight | 93 |
| Think about how much progress you’ve made already losing weight | 87 |
| Think about how much better you feel when you are thinner | 90 |
| Think about the clothes you would like to fit into | 77 |
| Look for information about weight loss, nutrition, or exercise | 74 |
| Reward yourself for sticking to your diet or exercise plan | 66 |
| Look at older pictures of yourself to motivate you to stick to your diet or exercise plan | 62 |
| Participate in a weight-loss program, such as Jenny Craig, Weight Watchers, or others | 25 |
Second, two research assistants from our staff were trained in coding the interviews using a dichotomous categorization system. This system consisted of identifying the presence or absence of dichotomous yes/no classifications for each practice. For example, if the participant mentioned eating apples at lunch, the response was coded as “1” for the practice “eating plenty of fruits and vegetables.” The lead investigator (first author) and two research assistants negotiated the emergent interpretation for clarification and verifiability of the categories (Lincoln & Guba, 1985). Because we used consensus agreement, it is not appropriate to report kappa statistics. We maintained confirmability by recording the data analysis process and keeping a record of all stages of analysis (Patton, 2002).
Third, after determining core practices for the weight-control items, we examined practices for themes. Themes are abstractions allowing us to categorize and group types of practices. These themes are exhaustive, which means they account for all identified practices. Themes were identified by utilizing several features of significance. These included (a) repetition of the central idea within and across interviews, and (b) connections between specific practices and the meanings ascribed to them by study participants (Love, 1994). The five recurring categories of weight control included nutrition, exercise, restraint, self-monitoring, and motivation. The themes were exhaustive, but not mutually exclusive. To determine agreement of the themes, three additional reviewers coded all of the practices into the existing themes; full agreement was reached. Participants were asked two open-ended questions regarding what helped them lose weight or maintain a healthy weight by (a) what they did regularly, and (b) what they thought about or reminded themselves of regularly. The themes describing each of these categories are discussed below.
Results
Overall, the participants in this study found that limiting caloric intake and/or increasing caloric expenditure contributed to their weight control. Additionally, cognitive practices or thought patterns motivated them to continue with their weight loss and maintenance. The themes included (a) nutrition: increase water, fruit, and vegetable intake, and be consistent with both the timing and content of meals; (b) physical activity: at least three times per week, follow and track an exercise routine that brings variety and enjoyment; (c) restraint: practice restraint by limiting and/or avoiding unhealthy foods; (d) self-monitor: plan meals, and track calories/weight-loss progress; and (e) motivation: participate in motivational programs and cognitive processes (thoughts and reminders) that affect weight-control behavior. The specific practices that relate to each theme are shown in Table 1. In the descriptions of each theme, below, representations of the practices related to the theme are included. Each individual practice is not discussed separately because of space limitations.
Theme 1: Nutrition
Increasing water, fruit, and vegetable intake, and having consistency with both the timing and content of meals were nutritional factors that contributed to weight-control success. Although we know that eating fruits and vegetables and limiting unhealthy food is an important part of weight loss and maintenance, qualitative data allow researchers to examine not only what, but also how others have adopted the practice into their lives. Examples of how participants made healthy choices and increased their fruit and vegetable intake include quotes such as (a) “I just stay in the produce aisle․… That is all good stuff․… It works for me․… I have maintained my weight for 12 years”; (b) “Eating salad can make me full in my head, but not in my stomach․… I have to have a salad with lunch and dinner”; (c) “I eat yogurt, strawberries, and fruit”; (d) “I only buy foods that are healthy for me. Even if I snack, it is raw or dried fruits, or maybe raw vegetables”; and (e) “I eat a lot of Cheerios, Frosted Mini Wheats, Raisin Bran, Kashi Go Lean, Grape Nuts.” Participants (n = 4) also mentioned the practice of limiting their caloric intake while eating out, noting that they chose healthier choices such as fish or poultry, and salad instead of pasta, or used low-fat menus, such as Weight Watchers. One gentleman in military service said, “I avoid eating what is fried. Even at the Army, I try to watch what I eat.”
Another practice was to avoid processed foods and to eat organic, whole foods; natural foods; and fruits and vegetables (n = 5). Examples included drinking skim milk and eating light yogurt, using Splenda or other artificial sweeteners instead of sugar, using low-fat butter, eating a large amount of vegetables to fill up before dinner, and filling cabinets with healthy foods. Last, participants used the practice of eating about the same thing every day (n = 5), as reflected in the following comments: (a) “I shop for similar foods every time I go to the store”; (b) “I consistently eat the same thing for breakfast․… It does not change. Lunch is grilled chicken from McDonald’s with no mayo [mayonnaise] … diet soda”; (c) “I eat about the same thing every day. This way I know the calories in my meals and snacks”; and (d) “I eat breakfast, lunch, dinner, and three snacks regularly. I keep a schedule of eating․… I don’t just eat when I am hungry. I know this works because I lost the weight and have kept it down.”
Several participants chose to increase their water intake (n = 9) to have more energy, and to fill up on water to avert cravings. Several (n = 7) also read nutrition labels on food packages to limit their carbohydrates; to look for fiber content; and to determine fat, calorie, carbohydrates, sodium, whole wheat/grain, and protein content. One person kept “proteins and fats around 40% and carbs [carbohydrates] around 20% to 30%” to help with weight maintenance.
Theme 2: Physical Activity
Participants found that following and tracking an exercise routine that brought variety and enjoyment at least three times per week was important for weight control. A variety of responses about how physical activity could be incorporated into a daily routine were discussed. The responses were divided nearly equally between those who exercised at home (n = 9), worked out at a gym (n = 9), and walked outside for exercise (n = 8). The home exercisers typically used a treadmill, hand weights, and exercise videos, and said things such as (a) “I exercise about 3 to 5 times a week. I run on the treadmill at my house, about 3 days a week․… I work out for 30 minutes a day when I’m trying to maintain my weight and about 60 minutes when I am trying to lose weight”; (b) “I work out from 10:30 to 11:00 with a ‘Fit TV’ program called ‘Gilad’”; (c) “I do an abdominal video every day”; (d) “I have a rebounder [a mini trampoline] at home. I do it 30 to 60 minutes 3 times a week for muscle and cardio.”
Those who worked out at a gym (n = 6) typically chose cardio equipment (elliptical, treadmill, stair–treadmill) rather than an organized exercise class: (a) “Every day, even for 20 minutes, I work out alone. I do 20 to 30 minutes of treadmill, or elliptical, or stair–treadmill”; (b) “I go to the gym at least three times a week, for about 60 to 90 minutes․… I do combined cardio and a nautilus circuit”; and (c) “I go to the gym three times a week. I swim and use the treadmill for about 1.5 hours․… I go with a couple of friends.”
The outside walkers (n = 5) followed a regular exercise routine, ranging from one mile to three miles per day. One woman walked three times a week for three miles, usually early in the morning. She said, “I started walking to lose weight. I continued because it was taking off inches, and it takes my appetite away.” Another said that she walked every day, “even on Sunday.” Others responded: (a) “I walk my dog three times a day”; (b) “I try to walk 10,000 steps a day with a pedometer”; and (c) “I walk almost everywhere. I walk to work and at work․… I walk every day for 40 minutes to one hour, to and from work.” Another woman responded,
I walk regularly. I try for daily, at least 6 days a week. I walk a mile every day, alone or with someone or with my dog. In the summer, I walk all along the lake (more than a mile). My dog gets exercise and I do, too. Walking is free and the nearest health club is about 60 miles.
Most participants exercised by themselves, but some reported that it was helpful to work out with other people (n = 6). One man who always exercised with someone else said, “My brother works out with me Monday, Wednesday, Friday, a coworker is with me Tuesday and Thursday, and I may have clients working out with me any day during the week.” Some worked out with their families, such as a man who took his daughter with him to the gym on the weekends, or one who took his two young sons (ages 4 and 6) with him to the basement for a workout as his wife walked beside him on the treadmill. Having a workout partner seemed to be a form of accountability, as well as making the exercise more enjoyable. If people found an exercise routine they enjoyed doing, they were more likely to stick with the plan; for example, “I really enjoy exercising․… I like how it makes me feel. I like that I am doing my body good, burning calories, and keeping my muscle tone up.” One person summed it up this way: “I am always trying to improve. I keep reaching for more by diversifying and changing things. I keep my core of exercises constant but add reps [repetitions] and modify it to challenge myself.”
Theme 3: Restraint
Participants found that not only did they need to engage in new behaviors and thoughts to change their weight, but they also needed to practice restraint in their meal patterns by limiting and/or avoiding unhealthy foods. The majority found that limiting carbohydrates helped them achieve this goal. Some replaced high-calorie foods or drinks with those that have fewer calories, such as choosing “sherbet over ice cream,” or peanuts over candy bars; for example, “I keep peanuts around the house. I use them for a snack. They are high calories, but are better than a candy bar.” Another participant agreed that “nuts are good fats and protein that will keep you from getting hungry.” Other examples of limiting carbohydrates and fat were: (a) “I stay away from all white products … no flour, bagels, pasta. I eat spinach pasta”; (b) “Instead of putting four sugars in my coffee, I put two”; (c) “I used to eat Fruity Pebbles or Cocoa Puffs for breakfast; now I eat healthier”; (d) “I used to eat out often, but I stopped. The food is fattening”; (e) “Avoiding eating out helps me maintain my weight … when you make your own food, you know what is in it”; and (f) “I used to eat a whole pizza, but now I occasionally have a slice or two.” Some participants used the practice of limiting the amount of unhealthy food in the home to avoid slipping into previous patterns of unhealthy behavior (n = 7). Comments included: (a) “I might have soda if we go out, but I do not keep soda in the house. If it is not there, I can’t have it”; (b) “I avoid the snack aisle [in the grocery store]. I won’t bring bad food into the house”; and (c) “Because I am single, if I bake a cake, I have to get it out of the house.”
Participants (n = 14) allowed themselves to eat small amounts of some unhealthy foods, but practiced restraint so as to maintain weight. One participant previously drank six or seven sodas per day and three cups of cappuccino, but she replaced those poor practices with eating Lean Cuisine (a brand of low-fat, low-carbohydrate frozen entrees) and drinking water instead. Other participants said, (a) “I don’t deny myself if I want something badly. I ‘pick my battles’ with food”; (b) “I splurge on pumpkin pie, but avoid whipped cream on the side”; (c) “I like chocolate, so I allow myself to have some every now and then. I might eat one Hershey’s Kiss, or a few M&Ms [two different kinds of chocolate candies]”; (d) “Once in a while, I have steak if I crave red meat․… I know it is fine to have a treat․… I know it works because my cholesterol and blood pressure are great and I haven’t gained weight”; (e) “I try to eat well Monday through Thursday, then I can eat what I want Friday to Sunday. I don’t deprive myself of things I enjoy”; and (f) “German chocolate cake is my favorite … I have one small slice․… I don’t deny myself.”
Last, a common practice that participants used to practice restraint was portion control (n = 12). By eating smaller portions throughout the day, these individuals were able to maintain their weight. One woman who lost and maintained a loss of 125 pounds said,
I weigh and measure everything I eat. Everything … because it is all about portion control. I am broken and I don’t work like you do, like a normal person does, and I don’t stop when I am full. Four ounces is a drop in the bucket; it means nothing. I could eat a 25-ounce steak every day and not be full.
Others had additional strategies for restricting their portions, such as: (a) “I buy 100-calorie packs”; (b) “I put portions on a smaller plate and use smaller portions so that I don’t eat as much, but I think I have more food”; (c) “I snack periodically throughout the day. I rarely have a big meal․… I’m an artist, and I’m usually working on a lot of things at once”; and (d) “If I want to eat something that is unhealthy, I eat it slowly and with small bites.” One participant controlled portions by using the palm of his hand as a reference size for steak, fish, and chicken. He adjusted his portions to eat until he was full, but not overstuffed, and said, “This worked for me and it was not extreme. It was a change and I stopped overeating. I know it worked because I lost the weight and maintained the weight loss without perpetual exercise or starving myself.” A woman stressed the importance of portion control in snacking by saying,
I never bring a full package of anything out of the kitchen. I have chips in the house because my husband eats them. If I need to have some, I will just take a handful and bring it out of the kitchen. I will not bring the whole bag with me.
Another woman mentioned that she did not clean her plate at every course, and said, “I do not allow the food on my plate to be touching, because if it is touching, I have too much on my plate.” These practices helped participants practice control with their eating patterns.
Theme 4: Self-Monitoring
The focus of self-monitoring was planning for meals, as well as tracking calories and tracking progress toward the desired weight goal. Related to portion control, participants reported that they planned their meals for the day in advance to avoid impulsive behavior. Having a system of planning ahead for meals and before grocery shopping was important to monitoring weight. Some individuals (n = 5) mentioned preparing food in advance or taking food with them, planning for meals to avoid overeating. One man planned what he was going to eat in advance by preparing a large quantity of food on weekends and freezing it in meal-sized portions. One woman planned her meals in advance by thinking about her next meal. She said,
After I eat breakfast, I am thinking about my next meal. Do I want a protein shake or something like nuts, or cheese and crackers? I’m always thinking about my next meal. I try to stay ahead of it, so I don’t wait for the last minute and grab something that is not as good for me. I pack my lunch the night before so that it is already prepared when I get to work.
To help with planning for shopping at the grocery store, participants (n = 6) used the following practices: (a) “I go grocery shopping after dinner․… I mentally prepare to see food I can’t buy—junk foods like candy bars and black licorice. I avoid ‘impulse’ grocery shopping”; and (b) “To shop well at the grocery store, I have to keep my daughter at home [because] she puts sweets in the cart.” On woman spoke of her weekly trips to the grocery store, where she watched what other people were putting into their cart that might be appealing—especially the fruits. She took her time (about 30 to 45 minutes) when going grocery shopping, and looked for low-calorie or low-fat selections.
Included in this theme is also the need to monitor the number of calories eaten at each meal, and to keep track of weight-loss progress (n = 10). Participants tracked the number of calories to become aware of what they were eating and to improve their eating practices. Writing tools included journals, food diaries, calendars, and computer logs in which participants recorded daily food intake and weekly weight. One participant explained:
I write a lot. I document my exercises․… I write what I did during the day with the date and time. I document what I eat․… If I had a bad interaction with someone, I document that. I document almost everything. I will write “Don’t eat sweets for the next three days.” If I go back and read it, I know I can’t have it.
Other participants discussed how they kept track of what they ate and the importance of keeping a journal to give them time to “stop and think” and review what they had consumed (food and water) for the day. One participant used a journal to keep track of the amount of water she drank each day. Another woman said,
I gauge the amount of certain nutrients: proteins, carbs, fat, and calories. I write it all down daily when I am trying to lose weight․… It makes me very focused on my portions and amounts. I am conscious of things that go into my mouth. If I don’t focus on writing it, my weight stays the same.
To keep track of weight-loss progress, participants weighed themselves between three and seven times per week. One woman kept the scale in her kitchen, which made it convenient for her to weigh herself regularly. Weight control required monitoring of meals and weight to keep a healthy balance. A participant summarized: “If I see increased weight … I will pay a little more attention to what I’m eating over the next couple of days, or not have sweets, or take the dog for a 10-minute-longer walk each time.”
Theme 5: Motivation
Motivation was a contributing factor to success in losing and maintaining weight, and this theme could be divided into two categories: (a) participating in motivational programs, and (b) engaging in a cognitive process (thoughts and reminders) that affected weight-control behavior. Programs mentioned included Weight Watchers, Jenny Craig, LA Weight Loss, TOPS (Take Off Pounds Sensibly), and Nutrisystem, and participants (n =4) found that accountability kept them motivated through group support. Participants (n = 4) also looked for information in television shows (i.e., the Biggest Loser), on the Internet (Weight Watchers), and in magazines (GNC, Fitness, Shape) for inspiration and ideas on how to maintain weight. However, the most reported practice for maintaining motivation was through cognitive processes (n = 44), which affected weight-control behavior. Participants often reminded themselves how much better they felt because they were contributing to their health. They reported that they wanted to keep their weight under control to reduce cholesterol levels, blood sugar, and blood pressure. Some (n = 15) enjoyed more energy and took pride in their health, which kept them motivated, as expressed in these statements: (a) “When I am energized in the morning, and I don’t need a nap all day, I think about that this is how I want to continually feel․… Energy is a motivator to keep me on track”; (b) “I feel empowered and proud of myself because I am in charge of my health. I feel better physically and emotionally. I used to feel weighed down at the end of the day”; (c) “I think about how much happier I am now that I’ve lost the weight․… It motivates me and makes me feel good”; and (d) “It is a gift to be able to put anything in my closet on at any moment. I like that I can walk up and down stairs without passing out. I have more energy from my weight loss.” One woman who was previously embarrassed about her weight said,
I remind myself of the things I could not physically do that I can do now, like paint my toenails. Not being able to do that made me feel old and worthless․… I was afraid to ice skate because I thought I might fall and not be able to get up.
To motivate themselves to keep their weight under control, some participants (n = 9) said they looked at previous pictures of themselves or thought about how they used to look when they were at an unhealthy weight. One example is,
I think about my self-esteem, my image in the mirror. I think about it every day when I’m shaving or combing my hair. You see a picture of yourself: “Do I look better now in the mirror or in the picture?” If I look better now, then I am doing the right thing.
Examples of other things said by participants include: (a) “I think of the way I used to look and how I was not happy”; (b) “I have bad memories of my body image, or not feeling comfortable when I was heavy, and when I’m tempted to eat more or not go to the gym. I keep those things in mind”; (c) “I took a few Polaroids [photographs] each month … to see how much weight I had at the start and the end of the month”; and (d) “I was thin when I was younger, so I look at my pictures from when I was thin. I look at them to remind myself what I want to get back to before I had four kids. I think about being happy back then.”
Related to this practice, participants also thought about fitting into fashionable clothes, and were motivated by the thought of fitting into a smaller size (n = 9). One woman who was pleased with her new size said, “Nothing feels as good as fitting into your clothes.” Others expressed similar motivations: (a) “I go to the mall and look at smaller sizes, and think I want to fit in petite. I’m motivated because the petite clothes look better than women’s, and I want to fit into them. I am motivated to work harder”; (b) “I think about fitting into my favorite pair of jeans. I felt great when I fit into them. The size that I fit in now makes me feel good about myself”; and (c) “I say to myself, ‘If I don’t do good, then I can’t buy that.’ It is really fun to try on the clothes and fit into a regular size. I use it as a motivator.”
To help keep diet and exercise goals in mind, participants thought about people who were overweight as a self-reminder to keep their own weight under control (n = 6). One said,
Seeing people who are overweight is a reminder [to stay on track]․… It is heartbreaking to think about being so overweight. I am grateful that I was able to make changes to get out of it. I remember how it felt. It makes me conscious that I do not want to go back there, and it helps me stay on my goal. I feel bad for them.
Seeing others who were unhealthy was a motivator for some to eat well and exercise, as expressed in the following statements: (a) “When I see big people in the supermarket, even big kids, I am reminded to take my time and put healthy items in my cart”; (b) “Everyone averts their eyes from an obese person. I cry when I see them … because I know they are in so much pain, and that is part of me”; and (c) “I work around a lot of obese people, and when I look at them, it triggers me to stick to my plan.”
Finally, participants thought about what they were eating to help them stay with their plan (n = 5). Many used this strategy, particularly when they were making plans to eat out. They reminded themselves to stay away from fast food, which is unhealthy. It was important for them to eat healthy and not to overeat, especially avoiding desserts or skipping appetizers. A participant who ate out socially said, “I have to remind myself to eat well.” Some participants became aware of what they were eating before putting the food into their mouths; for example, one woman who used this weight-loss strategy consistently said she became more “mentally aware of what I’m eating․… I care more than I used to. I didn’t realize before that I needed to lose weight.” Another example was, “I think about what I eat. Am I really hungry, or am I eating just because I am bored?” A motivated participant summarized that she stayed engaged by thinking of losing weight in increments. She said, “I didn’t lose 140 pounds. I lost one pound 140 times.”
Innovative Implementation of Practices
In line with positive deviance, we not only reviewed the themes, but also looked for specific deviation in implementation of practices within the themes. Some responses differed from conventional experience in the first theme (nutrition). One person did “not pay attention to fat content, just sugar and flour.” Another said that before she lost weight, she was a vegetarian and ate a lot of pasta and carbohydrates, but at the time of interview she was eating more meats. Other innovative responses that related to nutrition included: (a) “I never eat cereal”; (b) “Reading labels was too stressful, so I eat what I want to … good fresh fish, lean chicken breast”; (c) “I drink beet, carrot, celery, honey bells [a type of orange] smoothies”; (d) “I like Dean Ornish’s cookbook, can eat unlimited amounts of his foods, and won’t gain weight”; (e) “I eat a lot of egg whites … I will eat a dozen at a time and sometimes add a whole egg or two”; (f) “I take a piece of dessert and eat it standing up”; (g) “I imagine that hunger pains are “Pac Men” [animated characters in a video game] eating away at his fat”; (h) “[I] had to give up bubble gum because … I would need to buy more, which brought me to the candy aisle”; (i) “At a restaurant, I tell the wait staff that I am allergic to sugar, flour, and vinegar and ask what I can eat”; and (j) “I freeze Sprite Zero [a type of carbonized soft drink] in ice cubes and I mash them and suck on them when I read at night. Some participants (n = 2) tried some innovative tricks to prevent themselves from overeating. One person placed her food in a cereal bowl, “like pasta—you can really pile it up on a plate․… It tricks your eye to thinking you have more because it is piled up more,” whereas another tore her food into little pieces, “like break a burger into five pieces. Eating it like that, you start to feel full even before you finish a burger.” She said it tricked her mind into thinking she was eating more, which stopped her from going back for second or third servings of food.
Several unexpected practices were also noted as being innovative regarding physical activity that helped some individuals lose and maintain weight: (a) “If I’m watching a movie, I just walk through the whole thing․… I don’t have a treadmill, I just walk”; (b) “I bought a push [lawn] mower and I push mow the yard”; (c) “I work out in front of a mirror to get positive reinforcement to continue”; (d) “I have post-its [sticky note papers] around my desk that tell me to do stomach exercises while I sit there”; (e) “I have started to do Wii [a home video game console with a unique controller that detects movement] activities in our basement—Wii tennis—I played yesterday for two hours․…It feels like real tennis because you have to get your body into it”; (f) “I bring a notepad to the gym to follow the different workouts my trainer taught me”; (g) “I walk at a faster pace at the grocery store. I cut wood for nonaerobic exercise in winter”; (h) “When I exercise outdoors in cold weather, I lose more”; and (i) “I will wash a car myself, rather than take it to a car wash.” These strategies were not mentioned in other literature, such as the NWCR, or on the EBI.
Other participants (n = 4) used imagery in unique ways to keep their weight under control. One woman visualized family members who had diabetes, high blood pressure, and cancer, so she tried to “take a proactive role in breaking the cycle.” Another participant used imagery to “imagine my weight in amounts like bags of sugar and flour. I visualize I have lost “a bag of flour” when I lose 5 pounds, and I don’t have to carry it around anymore.” One woman imagined candy bars as cigarettes, because that made them unattractive to her. Another participant said, “I think of dressing like a coat. If you put on a coat, you weigh more. I pick the lightest coat they have.” Last, by reading “Fast Food Nation” (Schlosser, 2002), and watching the film about the local and global influence of the United States fast food industry, a participant found that fast food was not as appealing as it had been previously. She shared the film with her daughters and husband, and then the family did not eat fast food. These innovative practices helped participants lose weight and maintain their weight loss, despite the difficulties and barriers encountered.
Discussion
We used positive deviance to identify those who were successful at weight control and to investigate the implementation of weight-loss practices. Through this approach, we found that the findings were similar to others identified in the weight-control literature (Harvey-Berino, 1999; Qi & Dennis, 2000; Wing et al, 2007). We found that those who are more successful tend to weigh themselves, eat breakfast, self-monitor their food intake and activity, eat a lower-fat diet, and eat a limited variety of food groups. Our results are discussed in comparison with the NWCR, because this is the closest study in terms of determining weight-loss practices used by successful individuals. In the NWCR, 98% of registry participants reported that they modified their food intake to lose weight, compared to the 91% (average) in the present study. The most reported use of a practice in our study was limiting the amount of sugar consumed (cookies, desserts, sweets, sodas), because 100% of study participants noted this as something they used (very often, often, or occasionally). This is in agreement with Booth and colleagues (2004), who found that decreased snacking was associated with success at maintaining weight lost after an intervention. Booth and colleagues’ study methods were similar to our research methods (positive deviance), because they interviewed successful individuals to determine 27 weight-control practices. We did note some differences in practices identified by our study as compared to other weight-control studies. For example, the NWCR does not specifically include the practice of drinking water; however, 97% of participants in our study noted this as an important practice to use.
Self-monitoring has been described as the fundamental aspect of behavioral treatment (Wadden, 1993). Our work supports this description because the majority of participants in our study described self-monitoring through the use of self-weighing (69%). The NWCR lists weighing oneself as a primary strategy for weight loss. In the STOP Regain trial, Wing and colleagues (2007) showed that daily self-weighing was associated with a decreased risk of regaining weight. Qi and Dennis (2000) also found that maintaining a weight graph and weighing daily were associated with a higher likelihood of successful weight loss in a weight-loss intervention.
Other self-monitoring behaviors have also been shown to be important. Harvey-Berino (1999) showed a change in behaviors associated with successful weight loss; specifically, greater monitoring of food quantity eaten, recording the type and quantity of food consumed, planning meals and snacks, and keeping eating separate from other activities. Boutelle and Kirschenbaum (1998) found that the most-consistent self-monitors lost more weight than the least-consistent self-monitors. In our study, 97% of participants reported the use of planning what they would buy before going to the grocery store, and 82% reported planning what they would eat ahead of time. Approximately half (48%) of the individuals in our study recorded what they ate or drank.
Exercise is an important component of weight-loss maintenance, and researchers have shown a strong dose-response relationship with regular physical activity (O’Neil et al., 1979; O’Neil & Rieder, 2005). Those who successfully maintained their weight in the NWCR averaged 175 minutes of physical activity—primarily walking—per week. Although we did not measure the amount of physical activity engaged in by the study participants, we found that participants used a variety of strategies to implement physical activity (exercising consistently, finding an exercise they enjoyed, working out with others). Rather than concentrating on the amount of physical activity, the participants revealed a large variety in the implementation of this practice into their daily lives.
Although behavioral domains have been measured in other studies, the diversity of behaviors and cognitions associated with these behaviors have not been well researched. Our study included thoughts and cognitions associated with successful weight-loss maintenance. Tyler and colleagues (1997) also identified cognitive methods of weight loss, referred to as “head work,” in their study of interviews of 40 African American and 40 Euro American women. However, these methods were not exclusive to those who had been successful at weight loss, and included any method that had been tried. To our knowledge, only one other study (Barnes et al., 2007) had a similar methodology and included thoughts and cognitions in the survey instrument. However, the participants were African American, whereas the participants in our study were almost exclusively White, and the Barnes findings related to social support and perceived body image were different based on cultural norms. From these cultural differences, we learn that including positive-deviance practices from multiple racial and ethnic groups is essential in providing a range of weight-control practices.
Using positive deviance, we conclude that weight-control practices in successful individuals include a variety of nutritional, physical activity, restraint, self-monitoring, and motivational practices, with cognitive practices related to motivation. Although the themes in this study are not notably different from others, the study of positive deviance did produce novel implementation of themes from a population that was successful in weight control. These innovative practices are likely transferable to similar types of individuals, but would need to be examined in a larger population and reviewed by a medical professional to ensure their safety with general health practices. However, the unique practices have the potential to widen the number of successful weight-loss practices that could inform the design of a weight-loss intervention.
Limitations and Strengths
We recognize several limitations in this study. First, the qualitative interviews were retrospective, and it is possible the respondents’ answers did not reflect what they had actually done. External validation with objective measures, such as a food frequency questionnaire and accelerometer data, would be a next step for confirmation of some practices related to nutrition and exercise. Second, it is possible that additional in-depth exploration at multiple longitudinal time points would result in a wider variety of responses. Observation of participants would give us the opportunity to obtain in-situ behavioral information about practices of individuals who have been successful with weight loss and maintenance to reduce the possibility of recall error.
Third, it is possible that the participants might have used practices previously and were successful, so they were no longer using them at the time of interview. It is also possible that those who maintained their weight loss changed their practices over time based on social or contextual situations, and our interview was only a snapshot of their present practices. Longitudinal studies would improve the reliability of the responses received. Fourth, it was assumed that the participants were truthful in their successful weight loss and maintenance. Fifth, we did not explore the psychological factors that might serve as barriers to these practices, nor what served as motivation to maintain these practices. Additional research will include this aspect within the study to determine the psychological components of the positive deviants and why they were successful when others were not.
Sixth, the audiotapes were reviewed by two independent reviewers, and comparative analysis technique for clarification was utilized to determine verifiability. Despite this, misinterpretation of the wording of the practices described on the audiotapes might have resulted in misclassification of practices. The major limitation of assessing the agreement of the subjects’ responses with the reviewers’ interpretations is that we are relying on subjective interpretations. In future research, we recommend the use of qualitative computer software to manage large volumes of data and analysis of the transcripts. Additionally, we did not perform member checks or thematic accuracy checks with participants in this study. We recommend checking interpretations with participants to demonstrate interpretive validity. Last, the themes related to practices that contributed to both weight loss and weight-loss maintenance over time; therefore, we did not isolate the variables to determine whether the practices were related to one or both weight-control practices. In future qualitative studies, we will research the practices that contribute to only short-term and long-term weight maintenance (separate from weight loss).
Conclusion
We used positive deviance in this study to describe how successful individuals practice weight control. Using a qualitative research method was an appropriate approach to determine the weight-control practices that centered on the general categorical themes of nutrition, physical activity, restraint, self-monitoring, and motivational (cognitive) behaviors. The main findings of the successful weight-control practices were similar to those available in the current literature; however, the interesting point of this article is the use of positive deviance to determine weight-control practices to determine novel and innovative approaches to weight control. Using patient experiences of successful weight control gives a variety and depth of responses that contribute to our existing knowledge of the implementation of practices in weight loss and maintenance. Ongoing and future studies will determine if using positive deviance to assist in determining practices will assist in others’ adoption of the practices for weight control. Specifically, future weight-loss interventions can focus on participant behavior change to adopt proven weight-loss practices. Given the steady increase in obesity and programs to lose weight, we believe that future interventions using the advice from people who have found success might have a significant impact on weight control, as well as other health conditions.
Acknowledgments
We thank our research coordinators, Jolene Esposito and Aja Binette, as well as our project manager, Jennifer Poger, for their invaluable contributions to the study. We acknowledge the 61 participants who made this work in understanding weight-control practices possible.
Funding
The authors disclosed receipt of the following financial support for the research and/or authorship of this article: This work was supported by the Pennsylvania Tobacco Settlement Funds and Highmark, grant #4100042746.
Biographies
Heather L. Stuckey, DEd, is an assistant professor in the Department of Medicine at Penn State Hershey College of Medicine in Hershey, Pennsylvania, USA.
Jarol Boan, MD, is an associate professor in the Department of Medicine at Penn State Hershey Medical Center in Hershey, Pennsylvania, USA.
Jennifer L. Kraschnewski, MD, MPH, is an assistant professor in the Departments of Medicine and Public Health Sciences at Penn State Hershey Medical Center in Hershey, Pennsylvania, USA.
Michelle Miller-Day, PhD, is an associate professor in the Department of Communication Arts and Sciences at the Pennsylvania State University in University Park, Pennsylvania, USA.
Erik B. Lehman, MS, is a biostatistician in the Department of Public Health Sciences at Penn State Hershey College of Medicine in Hershey, Pennsylvania, USA.
Christopher N. Sciamanna, MD, MPH, is a professor in the Departments of Medicine and Public Health Sciences and is chief of the Division of General Internal Medicine at Penn State Hershey Medical Center in Hershey, Pennsylvania, USA.
Footnotes
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- Ahrari M, Houser RF, Yassin S, Mogheez M, Hussaini Y, Crump P, Levison FJ. A positive deviance-based antenatal nutrition project improves birth-weight in Upper Egypt. Journal of Health, Population and Nutrition. 2006;24(4):498–507. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17591347. [PMC free article] [PubMed] [Google Scholar]
- Alhassan S, Kim S, Bersamin A, King AC, Gardner CD. Dietary adherence and weight loss success among overweight women: Results from the A to Z weight loss study. International Journal of Obesity. 2008;32(6):985–991. doi: 10.1038/ijo.2008.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan JD. To lose, to maintain, to ignore: Weight management among women. Health Care for Women International. 1991;12(2):223–225. doi: 10.1080/07399339109515943. [DOI] [PubMed] [Google Scholar]
- Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, Johnson DB, Katz DL. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. American Journal of Preventive Medicine. 2009;37(4):340–357. doi: 10.1016/j.amepre.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Awofeso N, Irwin T, Forrest G. Using positive deviance techniques to improve smoking cessation outcomes in New South Wales prison settings. Journal of Health Promotion Australia. 2008;19(1):72–73. Retrieved from http://www.positivedeviance.org/pdf/smokingnewwales.pdf. [PubMed] [Google Scholar]
- Baptiste I. Qualitative data analysis: Common phases, strategic differences. Qualitative Social Research. 2001;2(3) Article 22. Retrieved from http://www.qualitative-research.net/index.php/fqs/article/view/917. [Google Scholar]
- Barnes AS, Goodrick GK, Pavlik V, Markesino J, Laws DY, Taylor WC. Weight loss maintenance in African-American women: Focus group results and questionnaire development. Journal of General Internal Medicine. 2007;22(7):915–922. doi: 10.1007/s11606-007-0195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: Penguin Books; 1979. [Google Scholar]
- Blair AJ, Lewis VJ, Booth DA. Influences on food choice and intake. Commentary from the 1st and 2nd food choice conferences. Prediction of success at weight loss from behaviour, attitudes, emotional eating and self-efficacy. Appetite. 1994;23(1):87–89. doi: 10.1006/appe.1994.1037. [DOI] [PubMed] [Google Scholar]
- Booth DA, Blair AJ, Lewis VJ, Baek SH. Patterns of eating and movement that best maintain reduction in overweight. Appetite. 2004;43(3):277–283. doi: 10.1016/j.appet.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obesity Research. 1998;6(3):219–224. doi: 10.1002/j.1550-8528.1998.tb00340.x. Retrieved from http://grande.nal.usda.gov/ibids/index.php?mode2=detail&origin=ibids_references&therow=379007. [DOI] [PubMed] [Google Scholar]
- Bradley E, Curry L, Ramanadhan S, Rowe L, Nembhard I, Krumholz H. Research in action: Using positive deviance to improve quality of health care. Implementation Science. 2009;4:25–36. doi: 10.1186/1748-5908-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brink PJ, Ferguson K. The decision to lose weight. Western Journal of Nursing Research. 1998;20(1):84–102. doi: 10.1177/019394599802000106. [DOI] [PubMed] [Google Scholar]
- Burke LE, Styn MA, Glanz K, Ewing LJ, Elci OU, Conroy MB, Sevick MA. SMART trial: A randomized clinical trial of self-monitoring in behavioral weight management-design and baseline findings. Contemporary Clinical Trials. 2009;30(6):540–551. doi: 10.1016/j.cct.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Swigart V, Warziski Turk M, Derro N, Ewing LJ. Experiences of self-monitoring: Successes and struggles during treatment for weight loss. Qualitative Health Research. 2009;19:815–828. doi: 10.1177/1049732309335395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: A key component of successful weight loss maintenance. Obesity. 2007;15(12):3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- Byrne S, Cooper Z, Fairburn C. Weight maintenance and relapse in obesity: A qualitative study. International Journal of Obesity Related Metabolic Disorders. 2003;27(8):955–962. doi: 10.1038/sj.ijo.0802305. [DOI] [PubMed] [Google Scholar]
- Collins J. Good to great: Why some companies make the leap … and others don’t. New York: Collins Business; 2001. [Google Scholar]
- Colvin RH, Olson SB. A descriptive analysis of men and women who have lost significant weight and are highly successful at maintaining the loss. Addictive Behaviors. 1983;8(3):287–295. doi: 10.1016/0306-4603(83)90024-2. [DOI] [PubMed] [Google Scholar]
- Colvin RH, Olson SB. Winners revisited: An 18-month follow-up of our successful weight losers. Addictive Behaviors. 1984;9(3):305–306. doi: 10.1016/0306-4603(84)90025-x. [DOI] [PubMed] [Google Scholar]
- Creswell JW. Qualitative inquiry and research design: Choosing among five traditions. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Ely AC, Banitt A, Befort C, Hou Q, Rhode PC, Grund C, Ellerbeck E. Kansas primary care weighs in: A pilot randomized trial of a chronic care model program for obesity in 3 rural Kansas primary care practices. Journal of Rural Health. 2008;24(2):125–132. doi: 10.1111/j.1748-0361.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- Ferrari M, Tweed S, Anneke Rummens J, Skinner HA, McVey G. Health materials and strategies for the prevention of immigrants’ weight-related problems. Qualitative Health Research. 2009;19:1259–1272. doi: 10.1177/1049732309344181. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Fowles ER, Hendricks JA, Walker LO. Identifying healthy eating strategies in low-income pregnant women: Applying a positive deviance model. Healthcare for Women International. 2005;26(9):807–820. doi: 10.1080/07399330500230953. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Mateu-Gelabert P, Sandoval M, Hagan H, Des Jarlais DC. Positive deviance control-case life history: A method to develop grounded hypotheses about successful long-term avoidance of infection. BMC Public Health. 2008;8:94–104. doi: 10.1186/1471-2458-8-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, King AC. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: The A TO Z Weight Loss Study. Journal of the American Medical Association. 2007;297(9):969–977. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J. Calorie restriction is more effective for obesity treatment than dietary fat restriction. Annals of Behavioral Medicine. 1999;21(1):35–39. doi: 10.1007/BF02895031. Retrieved from http://www.springerlink.com/content/q1kj2v650162l15p/fulltext.pdf. [DOI] [PubMed] [Google Scholar]
- Hopkins DR, Withers PC., Jr Sudan’s war and eradication of dracunculiasis. Lancet. 2002;360:s21–s22. doi: 10.1016/s0140-6736(02)11806-x. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, French SA. Socioeconomic status and weight control practices among 20- to 45-year-old women. American Journal of Public Health. 1996;86(7):1005–1010. doi: 10.2105/ajph.86.7.1005. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1380443/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, French SA. Preventing weight gain in adults: The pound of prevention study. American Journal of Public Health. 1999;89(5):747–751. doi: 10.2105/ajph.89.5.747. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1508711/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. American Journal of Clinical Nutrition. 1997;66(2):239–246. doi: 10.1093/ajcn/66.2.239. Retrieved from http://www.ajcn.org/cgi/reprint/66/2/239. [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krukowski RA, West DS, Harvey-Berino JJ. Recent advances in Internet-delivered, evidence-based weight control programs for adults. Journey of Diabetes Science and Technology. 2009;3(1):184–189. doi: 10.1177/193229680900300122. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2769852/pdf/dst-03-0184.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln Y, Guba E. Naturalistic inquiry. New York: Sage; 1985. [Google Scholar]
- Logue E, Sutton K, Jarjoura D, Smucker W, Baughman K, Capers C. Transtheoretical model—Chronic disease care for obesity in primary care: A randomized trial. Obesity Research. 2005;13(5):917–927. doi: 10.1038/oby.2005.106. [DOI] [PubMed] [Google Scholar]
- Love JG. The hermeneutics of transcript analysis. Qualitative Report. 1994;2(1) para. 7. Retrieved from http://www.nova.edu/ssss/QR/BackIssues/QR2-1/love.html. [Google Scholar]
- McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? Journal of Consulting and Clinical Psychology. 1999;67(2):177–185. doi: 10.1037//0022-006x.67.2.177. [DOI] [PubMed] [Google Scholar]
- Naimoli JF, Challa S, Schneidman M, Kostermans K. Toward a grounded theory of why some immunization programmes in sub-Saharan Africa are more successful than others: A descriptive and exploratory assessment in six countries. Health Policy and Planning. 2008;23(6):379–389. doi: 10.1093/heapol/czn028. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, MD: National Institutes of Health; 1998. [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute. The practical guide: Identification, evaluation and treatment of overweight and obesity in adults. Bethesda, MD: National Institutes of Health; 2000. [Google Scholar]
- Nothwehr F, Dennis L, Wu H. Measurement of behavioral objectives for weight management. Health Education Behavior. 2007;34(5):793–809. doi: 10.1177/1090198106288559. [DOI] [PubMed] [Google Scholar]
- Nothwehr F, Peterson NA. Healthy eating and exercise: Strategies for weight management in the rural Midwest. Health Education Behavior. 2005;32(2):253–263. doi: 10.1177/1090198104272328. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States—No statistically significant change since 2003–2004. National Center for Health Statistics Data Brief. 2007;1:1–8. Retrieved from http://65.162.96.74/resources/Other/1005-cdcobesityreport.pdf. [PubMed] [Google Scholar]
- O’Neil PM, Currey HS, Hirsch AA, Malcom RJ, Sexauer JD, Riddle FE, Taylor CA. Development and validation of the Eating Behavior Inventory. Journal of Behavioral Assessment. 1979;1(2):123–132. [Google Scholar]
- O’Neil PM, Rieder S. Utility and validity of the Eating Behavior Inventory in clinical obesity research: A review of the literature. Obesity Reviews. 2005;6(3):209–216. doi: 10.1111/j.1467-789X.2005.00192.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16045636. [DOI] [PubMed] [Google Scholar]
- Patton M. Qualitative research & evaluation methods. 3rd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Qi BB, Dennis KE. The adoption of eating behaviors conducive to weight loss. Eating Behaviors. 2000;1(1):23–31. doi: 10.1016/s1471-0153(00)00003-9. [DOI] [PubMed] [Google Scholar]
- Raynor DA, Phelan S, Hill JO, Wing RR. Television viewing and long-term weight maintenance: Results from the National Weight Control Registry. Obesity. 2006;14(10):1816–1824. doi: 10.1038/oby.2006.209. [DOI] [PubMed] [Google Scholar]
- Raynor HA, Jeffery RW, Phelan S, Hill JO, Wing RR. Amount of food group variety consumed in the diet and long-term weight loss maintenance. Obesity Research. 2005;13(5):883–890. doi: 10.1038/oby.2005.102. [DOI] [PubMed] [Google Scholar]
- Reid E. Improving low-performing high schools. Washington, DC: American Federation of Teachers; 1999. [Google Scholar]
- Rhodes KS, Bookstein LC, Aaronson LS, Mercer NM, Orringer CE. Intensive nutrition counseling enhances outcomes of National Cholesterol Education Program dietary therapy. Journal of the American Dietetic Association. 1996;96(10):1003–1010. doi: 10.1016/S0002-8223(96)00268-4. [DOI] [PubMed] [Google Scholar]
- Rubin HJ, Rubin IS. Qualitative interviewing: The art of hearing data. 2nd ed. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- Sabiston CM, McDonough MH, Sedgwick WA, Crocker PR. Muscle gains and emotional strains: Conflicting experiences of change among overweight women participating in an exercise intervention program. Qualitative Health Research. 2009;19:466–480. doi: 10.1177/1049732309332782. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. New England Journal of Medicine. 2009;360(9):859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlosser E. Fast food nation: The dark side of the all-American meal. New York: Houghton Mifflin; 2002. [Google Scholar]
- Smith DL. Positive deviance and organizational health. Hospital Administration in Canada. 1975;17(8):19–23. [PubMed] [Google Scholar]
- Thomas J, McLaren M, Linklater R. Fast food nation. United States: Fox Searchlight Pictures; United Kingdom: Tartan Films; 2006. (Producers), (Director). [Motion Picture]. [Google Scholar]
- Timmerman GM. Addressing barriers to health promotion in underserved women. Family and Community Health. 2007;30:S34–S42. doi: 10.1097/00003727-200701001-00006. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17159630. [DOI] [PubMed] [Google Scholar]
- Tyler DO, Allan JD, Alcozer FR. Weight loss methods used by African American and Euro-American women. Research in Nursing and Health. 1997;20(5):413–423. doi: 10.1002/(sici)1098-240x(199710)20:5<413::aid-nur5>3.0.co;2-r. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9334795. [DOI] [PubMed] [Google Scholar]
- Wadden TA. The treatment of obesity. In: Stunkard AJ, Wadden TA, editors. Obesity: Theory and therapy. New York: Raven; 1993. pp. 197–217. [Google Scholar]
- Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology. 2007;132(6):2226–2238. doi: 10.1053/j.gastro.2007.03.051. [DOI] [PubMed] [Google Scholar]
- Webb TL, Joseph J, Yardley L, Michie S. Using the Internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research. 2010;12(1):e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, Machan J. STOP regain: Are there negative effects of daily weighing? Journal of Consulting & Clinical Psychology. 2007;75(4):652–656. doi: 10.1037/0022-006X.75.4.652. [DOI] [PubMed] [Google Scholar]
- Wyatt HR, Grunwald GK, Mosca CL, Klem ML, Wing RR, Hill JO. Long-term weight loss and breakfast in subjects in the National Weight Control Registry. Obesity Research. 2002;10(2):78–82. doi: 10.1038/oby.2002.13. Retrieved from http://www.nature.com/oby/journal/v10/n2/pdf/oby200213a.pdf. [DOI] [PubMed] [Google Scholar]
- Wyatt HR, Grunwald GK, Seagle HM, Klem ML, McGuire MT, Wing RR, Hill JO. Resting energy expenditure in reduced-obese subjects in the National Weight Control Registry. American Journal of Clinical Nutrition. 1999;69(6):1189–1193. doi: 10.1093/ajcn/69.6.1189. Retrieved from http://www.ajcn.org/cgi/reprint/69/6/1189. [DOI] [PubMed] [Google Scholar]