Abstract
Background
There are no effective breast cancer education programs targeting Samoan women. We tested the effectiveness of a theory-guided, culturally appropriate breast cancer education program (the intervention) designed to increase mammography use among Samoan women.
Methods
This community-based participatory cluster-randomized controlled intervention trial used a parallel two-group design. The sample consisted of 776 women aged 42 and older who had not had a mammogram in the preceding two years. The primary outcome was self-reported mammogram use between pretest and posttest.
Results
Overall, there was no statistically significant intervention effect, although the odds of self-reported mammogram use were higher in the intervention than the control group (odds ratio [OR] 1.26, 95% CI [0.74, 2.14], p = 0.39). Exploratory subgroup analyses found that the intervention was effective only among women who were aware of mammograms but had never previously obtained one (OR 1.99, 95% CI [1.03, 3.85], p = 0.04). Low need for social support and lack of endorsement of culture-specific beliefs about breast cancer were associated with mammogram use in this group. In women unaware of mammography at pretest, high perceived susceptibility to breast cancer and endorsement of culture-specific beliefs were associated with mammogram use. For women who had previously obtained a mammogram, lower self-efficacy was associated with mammogram use. Intervention compared with control group women had significantly higher levels of knowledge of risk factors and lower endorsement of culture-specific beliefs at posttest.
Conclusions
Results suggest that a multifaceted education intervention may improve mammogram usage for certain subgroups of Samoan women.
Keywords: breast cancer screening, Samoan, Pacific Islander, minority, women’s health, community-based participatory research, mammography, education program, field trial, culture, behavior theory, education theory, education intervention
INTRODUCTION
Over the last two decades, there has been a steady increase in the use of mammography in the United States (1, 2). Improvements in breast cancer screening have contributed towards earlier stage at diagnosis (1, 3) and, in part, have resulted in better prognosis and longer survival. The increases in mammography use, however, have not accrued evenly across the U.S. population, as minority and recent immigrant populations still disproportionately underutilize breast cancer screening and early detection exams (2). Samoan women, the indigenous peoples of the U.S. Territory of American Samoa, are one such minority population. Regional surveys among Samoan women have documented disturbingly low rates of mammography use within the prior year, with rates of 22.4% and 24.4% for Samoan women 40 years and older residing in Hawaii and Los Angeles, respectively (4). In comparison, based on the 2000 National Health Interview Survey (2), rates of screening mammogram receipt within the prior two years by women 40 years and older ranged from 52.1% for American Indian/Alaska Native to 72.0% for non-Hispanic White. A similar rate for Pacific Islanders was not reported since, for confidentiality reasons, Pacific Islanders were coded with the “other’ category (2).
Breast cancer is the most common cancer among Samoan women. Indeed, breast cancer accounts for about 27% and 22%, respectively, of all cancers diagnosed among Samoan women in Los Angeles county and Hawaii (5, 6), a site-specific incidence comparable to that reported for non-Hispanic White women. Moreover, they have serious gaps in knowledge about breast cancer risk factors and harbor misconceptions regarding the cancer’s signs and symptoms (7, 8). In addition, in regional surveys, 42% of Samoan women 40 years and older had never heard about mammography (4). For Samoan women, important predictors for obtaining a mammogram include access to care (4), knowledge about risk factors (9) and screening guidelines (4), psychosocial factors (9), and culture-specific beliefs (9). For Samoans, culture-specific beliefs may also influence their health care utilization patterns, as such beliefs about disease etiology and treatment are associated with their use of indigenous healers (10).
There is evidence for the efficacy of various intervention models to enhance breast cancer screening, especially mammography utilization (11–18), among women of different ethnic/racial backgrounds and age ranges, and in different settings. No such intervention has, however, been tested among Samoan women. For Samoan women to achieve the Healthy People 2010 goal of regularly screening 70% of age-eligible women (19), it is imperative to design and test interventions to enhance age-appropriate breast cancer screening among these women. We present results of a community-based participatory intervention trial testing the effectiveness of a theory-guided, culturally appropriate breast cancer education program designed to increase mammography use among Samoan women.
MATERIALS AND METHODS
Data presented herein are from a community-based, collaborative field trial. The collaborative effort between a community partner (National Office of Samoan Affairs [NOSA]) and academic partners (University of California Irvine [UC Irvine] and University of California Los Angeles [UCLA]) used community-based participatory research (CBPR) principles (20–23) to guide its conceptualization, development, implementation, evaluation, and dissemination. The Institutional Review Boards of UC Irvine and UCLA and NOSA’s Human Subjects Review Committee approved the research protocol and the women signed written informed consent.
Study Design, Participants and Setting
The study was a cluster-randomized controlled intervention trial using a parallel two-group design. The study sites were Samoan-speaking churches in two contiguous southern California counties (Los Angeles and Orange), where approximately 45,000 Samoans reside (24). In all, 68 Samoan churches formed the sampling frame. Consenting churches were stratified on denominational category and congregation size and randomly assigned to either intervention or control condition. All eligible Samoan women within these churches were invited to participate. Eligibility criteria were Samoan (any-part) ancestry, age 42 years or older, and no mammogram within the past two years (all by self-report). Women aged 42 or older were included because screening mammograms are recommended once women reach the age of 40 (25).
Theoretical Frameworks
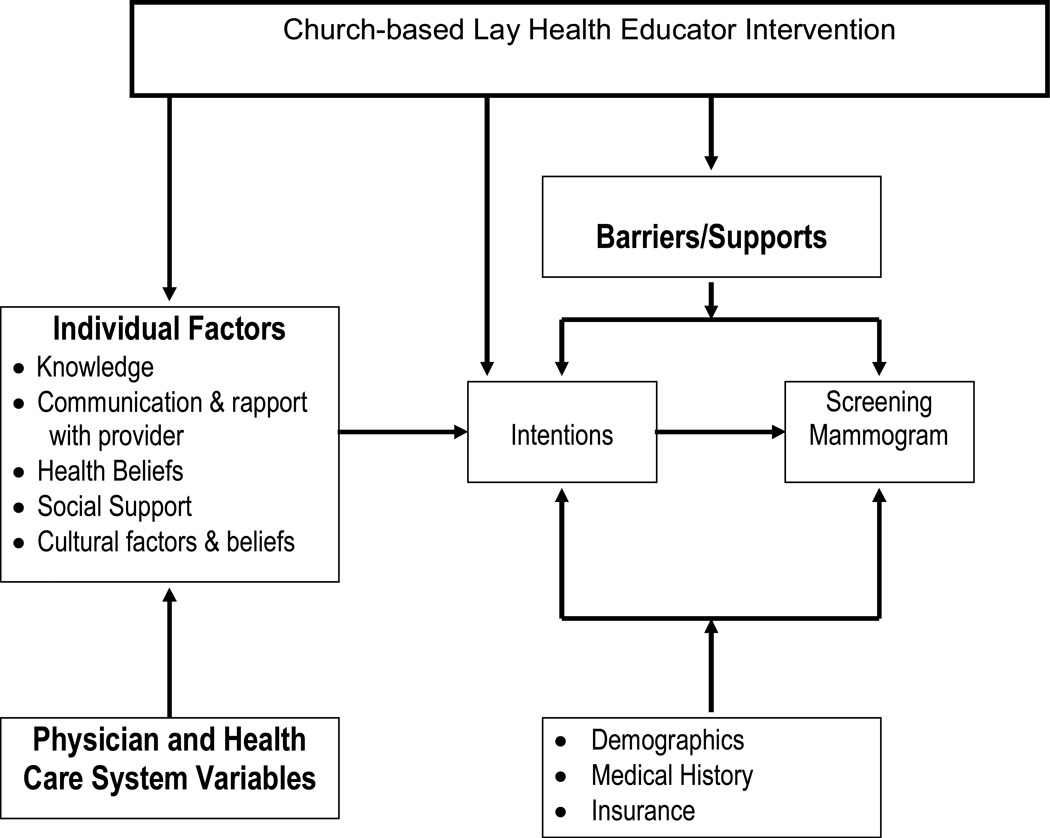
The Health Behavior Framework (HBF, Figure 1) (26–28) and Freire’s empowerment pedagogy (29, 30) guided the study. The HBF (previously referred to as the Adherence Model) represents a synthesis of some of the major theoretical formulations in the area of adherence and health behavior, and has been used to study antecedents of health behavior in diverse cancer control studies (e.g., (28, 31–37)). It is a general heuristic framework, which postulates that individual and health care system factors, and environmental and personal barriers jointly determine health behavior. For example, the Samoan women will have preexisting knowledge, health beliefs, social norms, past health behaviors, and cultural factors as a consequence of their place in society, migration history, and culturally determined beliefs. The education program was designed to influence the mutable individual level factors (e.g., knowledge, doctor-patient communications, perceptions of disease susceptibility and severity, cultural beliefs, self-efficacy), within the broader influences of health system factors over which there may be less control. It is postulated that the education program will positively influence beliefs and increase knowledge by framing and delivering its messages with a thorough understanding of the immutable factors that form the context within which individual behavior occurs. The final act of obtaining a mammogram represents the culmination of a complex chain of decision-making on the part of each woman. Our intervention was based on the premise that we can only influence such multi-faceted behavior using a multi-dimensional model derived from varying theoretical orientations.
Figure 1.
The Health Behavior Framework
Freire’s empowerment pedagogy provides a model to conduct education and nurture new behavioral skills by defining attributes of an ideal educational environment, the mode of effective education, and the incorporation of cultural and socio-ecological sensitivities within the educational context. The pedagogy, based on the problem posing method of learning, emphasizes dialogue and reciprocity (key CBPR components) (29, 30, 38). In this method, learners are presented with a particular situation as a problem to be solved by the group. Learners internalize and evaluate critically the information they receive in the course of participating in an open dialogue with those imparting the information, i.e., interactive exchange of knowledge. In addition, they are invited to introduce into the educational setting current environment and life circumstances that affect, in this study, their risk of breast cancer. The learners are empowered by the educator to make the problem of avoiding cancer their own problem instead of the educator’s problem. Through this strategy, educators involve themselves in an interactive process that allows them to gain more information about the beliefs and prevention of breast cancer while at the same time allowing the learners to be actively involved in a problem solving process that leads to improved health.
Breast Cancer Education Program (the Intervention)
Health education programs for minority populations need to be culturally targeted in terms of the program’s content, presentation format, medium of communication, and educators who are deemed credible and are culturally, linguistically, and socially acceptable and similar to the target audience (28, 35, 39, 40). Other important considerations are the inclusion of values, traditions, and experiences of the target audience. Samoans, similar to Native Hawaiians (41), have an oral tradition that values face-to-face interactions, trust building, collective decision-making, and experiential education through storytelling and role modeling.
The intervention consisted of three components: specially developed English- and Samoan language breast cancer educational booklets; skill building and behavioral exercises; and interactive group discussion sessions. The booklets along with the skill building and behavioral exercises (to model and role play new behaviors) supplemented the interactive group discussion sessions.
The intervention was culturally targeted as follows. The breast cancer educational booklets featured: Samoan artwork, scenery, and pictures of Samoans; Samoan words and phrases; and information about breast cancer, especially addressing culture-specific myths and beliefs harbored by Samoans. The booklets also addressed limitations in the readability, comprehension, and acceptability of standard breast cancer materials. The health educators: were Samoans with whom the women identified as being socially similar; conducted the sessions in the Samoan language; used terms and phrases which were familiar to the learners; before each session, recognized the social standing of learners bestowed with kinship-based traditional titles and/or their standing in the church hierarchy; approached delicate discussions about the female anatomy respectful of cultural and religious sensitivities; and engaged the learners in role play and skill building exercises mindful again of cultural and religious sentiments.
The intervention was designed around four modules, corresponding to four sessions, which operationalized Freire’s empowerment pedagogy and its problem posing method of education (38). Prior to the first session, the educator distributed the breast cancer education booklets. During the interactive sessions, the educator posed questions to the women designed to encourage thought and discussion about breast cancer’s potential impact on their lives, about their beliefs related to risk factors, signs and symptoms of the disease, about prevention and treatment. The educator then guided the group to come up with solutions to the problem of breast cancer control. After discussing a particular topic related to breast cancer, the learners were instructed to read appropriate sections from the booklet—thus reinforcing positive information. The interactive discussions coupled with review of printed information allowed the educator to mold the content and process of the intervention to the learners’ specific needs, characteristics and level of formal education, while encouraging a maximum degree of involvement—components thought to be vital to facilitate behavior change.
The first session (breast cancer: myths and facts) focused on the sessions’ procedural rules, reasons for staying healthy, what each learner already knew about breast cancer, and myths and facts regarding the disease. The establishment of procedural rules by the group was a major means for instituting group dynamics early in the process. This session also initiated entry into the interactive pedagogy and began the operationalization of important HBF constructs such as knowledge and perceived susceptibility and severity. By discussing knowledge and by learning myths and facts, the learners began to assess how much they knew. This stage assisted each learner to establish a baseline level of knowledge and efficacy against which she could assess the extent to which she “owned” the problem of breast cancer control. The second session (breast cancer risk factors and symptoms) focused on ways in which the learners were in control of their health, on learning about risk factors and symptoms of breast cancer and discussing early breast cancer detection examinations, including mammography. This session emphasized the efficacy of early detection. The learners also set goals in relation to the information presented, another step designed to elevate their own expectations of themselves. The third session (mammograms and follow-up) focused on what a mammogram is and how it is carried out; obtaining access to mammography in the community through lists of doctors and clinics providing mammograms; role playing for requesting mammograms; and the importance of following up on abnormal findings. This session also included a discussion on screening barriers (cost, fear of radiation, embarrassment, pain), navigation of the health care system, health insurance coverage, scheduling appointments, and follow-up visits. The learners designed a breast cancer screening action plan. The fourth session (review) summarized the information presented in the prior sessions with the learners reevaluating their perceptions of susceptibility, sense of control, and severity of the disease; and reinforcing their screening goals and action plan.
Two lay health educators (retired Samoan nurses) implemented the intervention. The educators were identified and recruited by Samoan community leaders based on their experience in community-based health education activities. The educators received about 20 hours of training on topics including, the intervention’s content, breast examinations, role-play and skills-enhancing techniques for navigating the health care system and doctor-patient communications, and effective strategies to facilitate interactive group discussions (e.g., establishing ground rules, use of verbal and non-verbal cues, use of pause and probe techniques, responding to questions, and involvement of all participants). After each session, two investigators (SIM, PHL) informally debriefed the educators about the group dynamics, discussion flow and depth, and the extent to which the discussion followed the session-specific script.
Between March 1999 and March 2000, to implement the intervention, we constituted 27 groups with 12–19 women/group. The women in these groups received the intervention over four weekly sessions between the pretest and posttest surveys. Each session lasted approximately two hours and was held either at the churches or at the project office. Women participating in the sessions received a token payment of $10 per session.
The control condition was usual care. Women in the control group were provided with the breast cancer educational materials after the posttest surveys.
Objectives and Outcomes
The primary objective was to increase mammogram usage among Samoan women. The primary outcome measure was self-reported mammogram use between the pretest and posttest surveys and was based on the response to the question, “Since the last time we interviewed you, have you had a mammogram?”
The pretest and posttest questionnaires also assessed demographics, ethnic identity, health status, health care access, and knowledge, attitudes and beliefs about breast cancer and mammography. The questionnaires were developed in English, translated into Samoan, and subsequently back-translated into English using standardized procedures (42). Reviewers from the community established face validity of the English and Samoan versions, which were pilot-tested and suitably revised.
We operationalized the HBF constructs by constructing measures from questionnaire items, as detailed in Table 1. Knowledge was scored as percent correct out of 10 items. Other HBF constructs were composed of 1–3 items. In the questionnaires, item response schema were tailored to item content (e.g., yes-maybe-no for screening barriers; a lot-somewhat-a little for belief in control over prevention; uncertain-somewhat certain-neither uncertain/certain-somewhat certain-very certain for self-efficacy items). To provide a unified approach across different item response schema and to facilitate use of the HBF constructs as both independent and dependent variables in logistic regressions, we first computed raw scores as means of multiple items (self-efficacy, ethnic identity) or by counting positive responses (perceived susceptibility, screening concerns, culture-specific beliefs), then dichotomized the raw scores into high/low categories. Responses for single-item HBF constructs (belief in control over prevention, belief in control over recovery, perceived severity, social support, divine intervention) were directly categorized as high/low. The HBF constructs were used as both secondary outcome measures and predictors in ancillary analyses.
Table 1.
Composition and scaling of the Health Behavior Framework constructs
| Construct and Questionnaire Items | Scaling |
|---|---|
Knowledge about breast cancer risk factors: “In your opinion, does ___ increase a woman’s risk of getting breast cancer?”
|
Percent correct derived from 4 response categories (strongly disagree, somewhat disagree, somewhat agree, strongly agree) |
Belief in control over getting breast cancer:
|
High/low belief derived from 3 response categories (a lot, somewhat, very little): high = a lot, low = somewhat or very little |
Belief in medical personnel’s control over recovery:
|
High/low belief derived from 3 response categories (a lot, somewhat, very little): high = a lot, low = somewhat or very little |
Perceived susceptibility:
|
High/low perception derived from 3 response categories (very, somewhat, not at all): high = one response “very” and other “very” or “somewhat,” low = otherwise |
Perceived severity:
|
High/low perception derived from 3 response categories (very, somewhat, not at all): high = not at all, low = very or somewhat |
Need for social support to obtain a mammogram:
|
High/low need derived from 3 response categories (yes, maybe, no): high = yes or maybe, low = no |
Screening concerns: “Are you concerned
|
High/low concerns derived from 3 response categories (yes, maybe and no); high = yes or maybe for 2 or more items, low = otherwise |
Self-efficacy: “How certain are you that you can
|
High/low self-efficacy derived from mean score of response categories (1 = uncertain, 2 = somewhat uncertain, 3 = neither uncertain/certain, 4 = somewhat certain, 5 = certain): high if mean ≥ 4, low if mean < 4. Cronbach’s α = 0.88 pretest, 0.91 posttest* |
Traditional Samoan ethnic identity:
|
High/low ethnic identity derived from mean score of response categories (1 = strongly disagree, 2 = somewhat disagree, 3 = neither disagree/agree, 4 = somewhat agree, 5 = strongly agree): high if mean ≥ 4, low if mean < 4. Cronbach’s α = 0.66 pretest, 0.68 posttest8 |
Endorsement of culture-specific beliefs:
|
High/low endorsement derived from 5 response categories (strongly disagree, somewhat disagree, neither disagree/agree, somewhat agree, strongly agree): high = agreement with one or both items, low = otherwise |
Agreement with divine intervention:
|
High/low agreement derived from 4 response categories: high = strongly agree or somewhat agree, low = strongly disagree or somewhat disagree |
Cronbach’s α was computed only for multi-item constructs with raw scores derived as means. Other constructs used single items (belief in control over prevention, belief in control over recovery, perceived severity, social support, divine intervention) or were scored using a counting approach (perceived susceptibility, screening concerns, culture-specific beliefs) or as percent correct (knowledge).
An additional predictor variable was mammography history. The women were categorized into three groups based on their awareness of mammograms and past history of mammography. Categorization was based on responses to the questions “Have you ever heard of a mammogram?” and “Have you ever had a mammogram?” in the pretest survey. The three groups were women unaware of mammography, women who were aware of but had never had a mammogram, and women with a previous mammogram.
Data Collection
Specially trained bilingual and bicultural Samoan women interviewers administered in-person the screening interview, and the pretest and posttest surveys. The interviewers screened and recruited eligible women at Samoan churches, place of residence, or during a Pacific Islander festival. As discussed elsewhere (9), we designed an elaborate validation system to identify and exclude duplicate interviews. Participants were administered a pretest questionnaire (before the intervention where applicable) and a posttest questionnaire approximately 8 months after pretest. The pretest and posttest surveys took approximately 25 and 10 minutes, respectively. The interviewers were blind to the study group status. Most of the surveys were conducted during weekday evenings and Saturdays. The women received a token payment of $5 for completing each survey.
Analysis
We compared the intervention and control groups on pretest demographics, mammogram history, and HBF constructs using chi-square tests for categorical variables and ANOVA for continuous variables. We compared the three subgroups defined by mammogram history using the same approach.
Because the intervention was allocated at the church level rather than individually, we used analytical methods for all outcome analyses that accounted for the correlation of responses of women within church (43). In particular, we used the GENMOD procedure in SAS for Windows Version 9.1, which fits models to correlated responses using generalized estimating equations (GEE), with an exchangeable working correlation structure, corresponding to compound symmetry within church.
The analyzed sample consisted of all women who completed the pretest and posttest surveys, consisting of 96% of the originally randomized sample (see Results). Analysis of outcomes compared women in the groups to which they were assigned regardless of treatment actually received. Intervention-control group comparisons of rates and reasons for loss to follow-up and demographic characteristics of dropouts indicated there was minimal potential for bias due to loss to follow-up; thus women with missing outcome data were excluded from the analyses.
For the primary outcome, self-reported mammogram use between pretest and posttest, we used GEE with a logit link, corresponding to logistic regression with standard errors adjusted for correlated data. Ancillary analyses were performed to (1) identify bivariate predictors of mammogram use, regardless of intervention assignment; (2) assess changes in secondary outcomes; (3) identify moderators, corresponding to subgroups, in which the intervention was differentially effective; and (4) develop multivariate models, which focused on the effectiveness of the intervention in subgroups and the association of HBF constructs with mammogram receipt.
We evaluated bivariate associations between self-reported mammogram use (dependent variable) and each of the demographic variables, mammogram history, and HBF constructs (independent variables) by entering each independent variable into the model singly. These analyses used GEE with a logit link.
To determine the intervention effect on the secondary outcomes, we compared the intervention and control groups on posttest measurements of the HBF constructs using GEE with a logit link, with the exception of knowledge, for which we used an identity link (linear regression).
To identify subgroups in which the intervention was differentially effective, we conducted exploratory moderator analysis by fitting models stratified by subgroups, with subgroups defined by pretest demographics and mammogram history variables.
All multivariate models included intervention group assignment as well as age (≥65 years vs. <65 years), education (>12 years vs. ≤12 years), marital status (currently married vs. not), employment (employed vs. other) and annual family income (≥$20,000 vs. <$20,000) in order to adjust for potential confounders. We began with models that additionally included all HBF constructs and pruned constructs from the model by backward elimination, in which the variable with the largest p-value is eliminated first, to sequentially remove constructs that did not exhibit a statistically significant association with the outcome. Constructs with p-values ≤.05 were retained in the models. Intervention group assignment and the potential confounders were retained regardless of statistical significance. Models were built separately for each subgroup.
The moderator analyses and multivariate models were exploratory analyses conducted in order to elucidate HBF predictors of mammogram receipt in this population and generate hypotheses for evaluation in other studies.
Sample size for the study was based on power analyses which concluded that a sample size of 300 women per study arm would have over 80% power to detect a 15% difference in the primary outcome, given an intraclass correlation of 0.1.
RESULTS
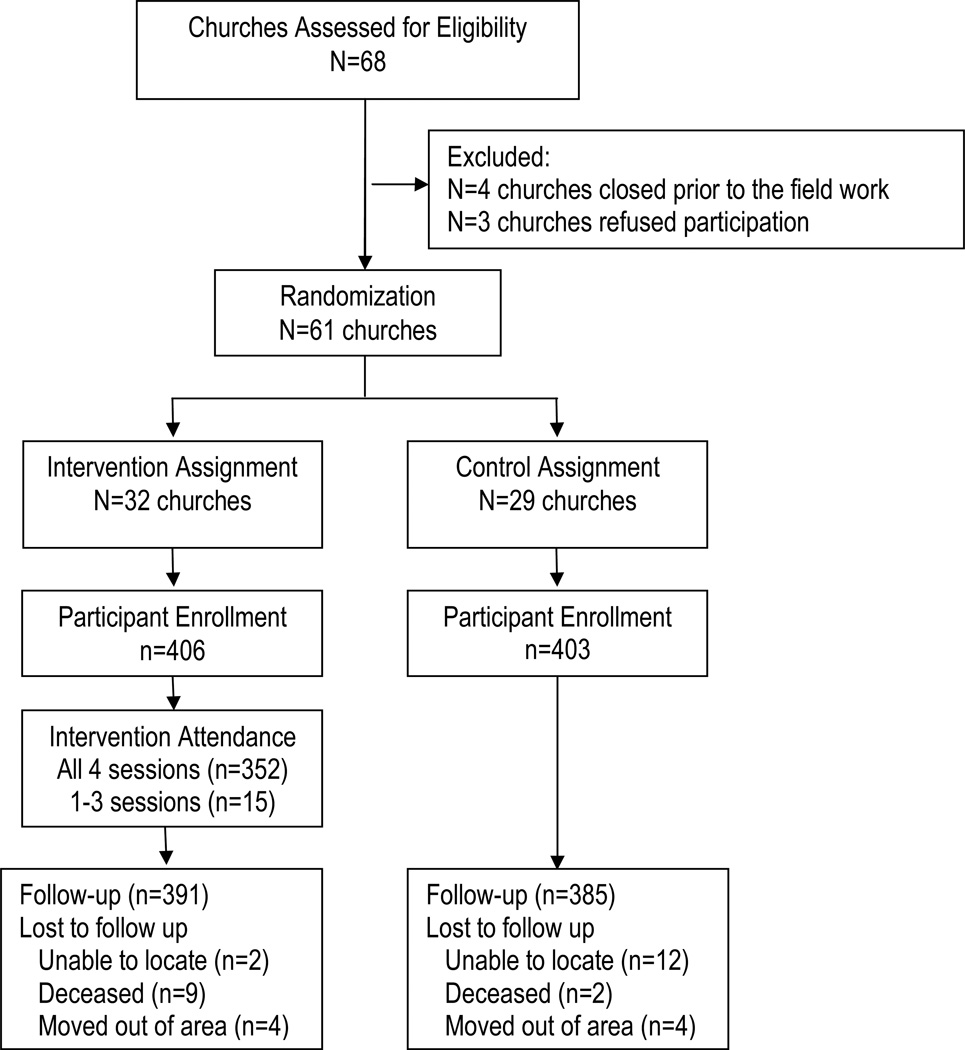
We conducted the study between July 1998 and June 2001, with recruitment and follow-up occurring between March 1999 and October 2000. We recruited 809 eligible Samoan women from 61 churches, with congregational sizes ranging from 20 to 400. Figure 2 provides the participant flow diagram. The panel with data from both pretest and posttest assessments was made up of 776 women (391 and 385, respectively, in the intervention and control groups), a retention rate of 96% in both groups. The demographic characteristics of the 33 women lost to attrition were similar in the control and intervention groups (data not shown). Of the 391 intervention group women, 90.0% (n=352) participated in all four education sessions, and 1.3% (n=5), 1.8% (n=7), 0.8% (n=3), and 6.1% (n=24) participated in 3, 2, 1 or 0 sessions, respectively.
Figure 2.
Participant flow through the trial
Women’s Characteristics at Pretest
At pretest, the control and intervention groups were similar on demographics and all HBF constructs (data not shown). About one-third (34%) of the women had not heard of mammography and an additional 25% of the women had heard of mammography but never received one (Table 2). Among women who had had a mammogram in the past; the most recent mammogram was 2–5 years before the pretest survey for 234 women and over 5 years before the pretest survey for 90 women. There were significant differences in demographic characteristics, access to care measure, and HBF constructs among the three subgroups (Table 2).
Table 2.
Pretest characteristics of the women in the Breast Cancer Education Program for Samoan Women, Southern California, 1998–2001
| Mammogram History Subgroups* | |||||
|---|---|---|---|---|---|
| Characteristic | Total study sample (n=776) |
Unaware of mammography (n=262) |
Aware but never had mammogram (n=190) |
Had previous mammogram (n=324) |
P for subgroup differences |
| Intervention group | 50% (391/776) | 52% (136/262) | 47% (89/190) | 51% (166/324) | .525 |
| Age (mean ± sd) | 55 ± 11 (n=776) | 58 ± 12 (n=262) | 52 ± 10 (n=190) | 54 ± 9 (n=324) | <.0001 |
| Born in American Samoa | 59% (460/775) | 58% (153/262) | 58% (110/190) | 61% (198/324) | .711 |
| Samoan interview language | 87% (672/775) | 95% (249/262) | 84% (160/190) | 81% (264/324) | <.0001 |
| Currently married | 66% (506/773) | 57% (148/260) | 70% (133/190) | 69% (225/324) | .002 |
| Employed | 32% (246/775) | 18% (48/262) | 37% (71/190) | 39% (127/324) | <.0001 |
| Education level | |||||
| More than 12 years | 17% (132/767) | 6% (15/256) | 21% (39/188) | 24% (78/324) | <.0001 |
| 9–12 years | 67% (517/767) | 68% (173/256) | 70% (132/188) | 65% (212/324) | |
| 8 years or less | 15% (118/767) | 27% (68/256) | 9% (17/188) | 10% (34/324) | |
| Annual family income | |||||
| $20,000 or more | 30% (221/731) | 18% (43/243) | 32% (58/180) | 39% (120/309) | <.0001 |
| $10,000–$19,999 | 30% (221/731) | 24% (59/243) | 39% (71/180) | 29% (91/309) | |
| Under $10,000 | 40% (289/731) | 58% (141/243) | 28% (51/180) | 32% (98/309) | |
| Health insurance status | |||||
| Insured | 79% (609/775) | 73% (190/262) | 74% (141/190) | 86% (279/324) | <.0001 |
| Uninsured | 21% (166/775) | 27% (72/262) | 26% (49/190) | 14% (45/324) | |
| Knowledge about risk factors (mean percent correct ± sd) | 47 ± 16 (n=776) | 47 ± 17 (n=262) | 44 ± 15 (n=190) | 48 ± 15 (n=324) | .019 |
| High belief in control over prevention | 41% (312/769) | 40% (103/258) | 37% (69/189) | 43% (140/322) | .291 |
| High belief in medical personnel’s control over recovery | 29% (221/773) | 26% (68/261) | 26% (49/190) | 32% (104/322) | .156 |
| High perceived susceptibility | 31% (238/776) | 35% (90/262) | 27% (51/190) | 30% (97/324) | .217 |
| High perceived severity | 18% 136/774) | 15% (38/262) | 29% (56/190) | 13% (42/322) | <.0001 |
| High need for social support to obtain a mammogram | 23% (175/774) | 37% (95/260) | 15% (28/190) | 16% (52/324) | <.0001 |
| High screening concerns | 65% (504/776) | 84% (219/262) | 57% (108/190) | 55% (177/324) | <.0001 |
| High self-efficacy | 55% (423/776) | 38% (99/262) | 59% (112/190) | 65% (212/324) | <.0001 |
| High traditional Samoan ethnic identity | 88% (680/776) | 91% (239/262) | 83% (158/190) | 87% (283/324) | .036 |
| High endorsement of culture-specific beliefs | 27% (212/776) | 35% (91/262) | 23% (44/190) | 24% (77/324) | .004 |
| High agreement with divine intervention | 75% (578/768) | 86% (221/258) | 67% (127/190) | 72% (230/320) | <.0001 |
Sample sizes are denoted parenthetically
Effectiveness of intervention on primary and secondary outcomes
Although rates of self-reported mammogram use were higher in the intervention than the control group (Table 3), the difference was not statistically significant. Rates of self-reported mammogram use in the intervention versus control group for the three mammogram history sub-groups were: 29% (40/136) vs. 23% (29/126) for women unaware of mammograms; 52% (46/89) vs. 36% (36/100) for women who were aware but never had one; and 60% (99/166) vs. 53% (83/158) for women with a previous mammogram. The strongest predictor of mammogram use was mammogram history at pretest (p<.0001). Women with a previous mammogram were the most likely to obtain a mammogram between pretest and posttest, followed by women who had heard of mammograms but never gotten one. Women unaware of mammography at pretest were the least likely to obtain one during follow-up. Other significant predictors of mammogram use were being married, being employed, higher income, and being insured.
Table 3.
Bivariate associations between pretest characteristics and self-reported mammography use between pretest and posttest
| Association with Self-Reported Receipt of Mammogram Between Pre- and Posttest |
|||
|---|---|---|---|
| Pretest characteristic | Mammogram receipt rates* |
Odds ratio (95% CI) |
P |
| Study group | |||
| Intervention group | 47% (185/391) | 1.26 (0.74, 2.14) | .390 |
| Control group† | 39% (148/384)‡ | ||
| Mammogram history at pretest | |||
| Had a mammogram in past | 56% (182/324) | 2.82 (1.99, 4.01) | <.0001 |
| Aware of mammograms but never had one | 43% (82/189) | 1.72 (1.23, 2.41) | <.0001 |
| Unaware of mammography† | 26% (69/262) | ||
| Age | |||
| 42–49 years | 44% (127/287) | 1.21 (0.82, 1.80) | .337 |
| 50–64 years | 44% (146/334) | 1.29 (0.90, 1.86) | .171 |
| 65 years or older† | 39% (60/154) | ||
| Country of birth | |||
| American Samoa | 43% (196/460) | 1.19 (0.82, 1.74) | .365 |
| Other† | 44% (137/315) | ||
| Education level | |||
| More than 12 years | 49% (65/132) | 1.55 (0.98, 2.45) | .063 |
| 9–12 years | 43% (220/517) | 1.19 (0.88, 1.60) | .259 |
| 8 years or less† | 37% (44/118) | ||
| Marital status | |||
| Currently married | 46% (231/506) | 1.31 (1.01, 1.70) | .041 |
| Currently single† | 38% (102/267) | ||
| Employment status | |||
| Employed | 51% (126/246) | 1.48 (1.15, 1.13) | .005 |
| Other† | 39% (207/529) | ||
| Annual family income | |||
| $20,000 or more | 48% (106/221) | 1.53 (1.10, 2.12) | .012 |
| $10,000–$19,999 | 46% (101/221) | 1.30 (0.91, 1.85) | .143 |
| Under $10,000† | 36% (104/289) | ||
| Language of interview | |||
| Samoan | 42% (279/672) | 0.75 (0.52, 1.06) | .106 |
| English† | 52% (54/103) | ||
| Insurance status | |||
| Insured | 45% (272/609) | 1.21 (0.92, 1.97) | .125 |
| Uninsured† | 37% (61/166) | ||
Sample sizes are denoted parenthetically
Reference group
Sample size reduced from 385 to 384 due to nonresponse on mammogram use for one women in the control group.
The intervention group women had significantly higher levels of knowledge about risk factors (62±17 (mean±SD) for intervention vs. 54±16 for control, p=0.003) and lower endorsement of culture-specific beliefs (12% [47/391] for intervention vs. 22% [85/385] for control, p=0.014) at posttest. Comparisons for other HBF constructs were largely in a direction suggestive of the effectiveness of the intervention but were not statistically significant (data not shown).
Moderator analysis
In moderator analyses, mammogram history at pretest, age, interview language and employment status were identified as potential moderators of the intervention effect, with p<0.100 for one or more subgroups. Mammogram history was selected for subgroup analysis by stratifying on this variable in the multivariate analysis since it was highly predictive of mammogram use and strongly associated with the other variables.
Multivariate models of mammogram use by subgroup
Table 4 presents multivariate logistic regression models for self-reported mammography use in the three subgroups defined by mammogram history at pretest. Because the three subgroups differed markedly in demographic and other pretest characteristics, stratification effectively controlled for many of these variables and allowed for better focus on HBF correlates of mammogram receipt within subgroup. Potential confounders (age, education, marital status, employment and insurance status) were also included in each model for added clarity. The odds of mammogram use were significantly higher in the intervention group for women who were aware of mammograms but had never had one at pretest (p=.040), but not for the other two subgroups. For this subgroup, high need for social support and endorsement of culture-specific beliefs about breast cancer were associated with lower odds of obtaining a mammogram. For women unaware of mammography at pretest, higher odds of mammogram use were associated with high perceived susceptibility to breast cancer, and high endorsement of culture-specific beliefs. For women with a previous mammogram, higher self-efficacy was associated with lower odds of obtaining one during the pretest-posttest interval. The addition of an acculturation measure (language of interview) to each of the models did not significantly change the results (data not shown).
Table 4.
Multivariate predictors of self-reported mammogram use between pretest and posttest, by participant mammogram history at pretest
| Mammogram History at Pretest | ||||||
|---|---|---|---|---|---|---|
| Unaware of mammography (n=262) |
Aware but never had a mammogram (n=189)‡ |
Had previous mammogram (n=324) |
||||
| Predictors (pretest) | Odds ratio (95% CI) |
P | Odds ratio (95% CI) |
P | Odds ratio (95% CI) |
P |
| Intervention vs. control group | 1.58 (0.73, 3.44) | .246 | 1.99 (1.03, 3.85) | .040 | 1.02 (0.51, 2.05) | .955 |
| High vs. low perceived susceptibility | 3.49 (1.60, 7.62) | .002 | ||||
| High vs. low endorsement of culture-specific beliefs | 2.14 (0.99, 4.63) | .053 | 0.35 (0.15, 0.81) | .014 | ||
| High vs. low need for social support | 0.29 (0.10, 0.86) | .025 | ||||
| High vs. low self-efficacy | 0.52 (0.32, 0.85) | .009 | ||||
All odds ratios are adjusted for age (65 or older vs. under 65), education (more than 12 years vs. 12 or fewer years), marital status (currently married vs. not), employment (employed vs. other) and annual family income ($20,000 or more vs. under $20,000).
Sample size reduced from 190 to 189 due to nonresponse on mammogram use for one woman in the control group.
DISCUSSION
To the best of our knowledge, this is one of the first breast cancer education programs developed and tested for Samoan women. Despite implementation of a theoretically driven, culturally competent, community-based intervention program, this study was not able to demonstrate an overall effect of the intervention. Although the rate of self-reported mammogram use between the pretest and posttest was higher in the intervention than the control group, the difference was not statistically significant. Exploratory moderator and multivariate analyses revealed effects of the education program on certain sub-groups of women based on prior mammogram history. The exploratory analyses suggest that the intervention was only effective for Samoan women who had heard of mammography but had never previously received one, doubling their odds of obtaining a mammogram compared to the control group. The intervention was also associated with higher, but not statistically significant, rate of mammogram receipt in women unaware of a mammography at pretest. There was no effect of the intervention on women who had a prior mammogram. Participation in the intervention also significantly increased knowledge and lowered endorsement of culture-specific beliefs about breast cancer.
In the multivariate model predicting mammogram use in women with a previous mammogram, higher self-efficacy was associated with lower odds of obtaining a mammogram during follow-up. The negative association between self-efficacy and mammogram use could be attributed to the incomplete measure of this construct. Our measure of self-efficacy was limited to four scaled items. It is quite likely that measurement of important aspects of self-efficacy such as ability to make and keep an appointment with a doctor, issues of child care and transportation, and ability to obtain follow-up care could have provided results in the expected direction. Another explanation for the negative association could be that these women, although scoring high on self-efficacy, were less certain about their ability to obtain follow-up care for an abnormal mammogram—and thus decided not to obtain a mammogram.
The study was designed to have 80% power to detect a 15% difference in mammography receipt between the intervention and control groups. However, we were only able to achieve an 8% intervention-control difference, which did not reach statistical significance. Several circumstances in the implementation of the study may have contributed to a reduction in the project effect size. The rate of mammogram use in the control group was at the high end of the anticipated range. The Samoan community in southern California is closely-knit, with extended family and church members networking on a regular basis. It is quite plausible that the intervention group women may have discussed their participation in the education program, and even shared information and experiences with the control group women, thus prompting the latter to obtain a mammogram. The intraclass correlation coefficient, measuring the degree to which outcomes of women within the same church are more concordant than outcomes of women from different churches, was 0.19, almost twice the anticipated value of 0.1. Given these circumstances, it would have been necessary to have a total sample size of about 1900, more than twice the actual study size, in order to detect an intervention effect after adjustment for the correlation. In addition, it is possible that the educators did not deliver the intervention in the intended manner or extent, thus reducing its effectiveness.
This study has implications for future research. First, despite the implementation circumstances discussed above, there was an overall positive but non-statistically significant intervention-control difference in mammography use at the posttest. This finding argues for a replication of the trial, which incorporates the methodological and implementation lessons learned in this study. It would be important to understand the cognitive, normative, psychological and structural triggers that may or may not contribute to a change (or lack thereof) in mammogram use among women exposed to the intervention. Insights into these factors would help strengthen the current intervention. Furthermore, it would be interesting to understand whether different aspects of the education program have a null, multiplicative, or additive effect on mammogram use. The different aspects of the education program would include: cultural and linguistic targeting; role play and behavioral exercises to alleviate fear and embarrassment about breast exam procedures and enhance skills for effective doctor-patient communications; the Freirian empowerment pedagogy to actually facilitate learning and enhance mammogram use; and the effects of group-based dynamics and positive reinforcement which may be inherent within peer groups such as those recruited through churches.
Second, our exploratory analyses suggest that the education program may improve mammogram use for certain sub-groups of women based on their mammogram history. Besides the need to validate this exploratory finding, future research needs to examine whether the null effect of the education program on women with a prior mammogram use history was an artifact or that the education program indeed has a differential effect based on their mammogram use history. A differential effect of the education program may be due to varying levels of readiness to take action among women. It is also possible that women who have had a previous mammogram may not feel the same level of urgency to the ones who have heard about a mammogram but have not obtained one.
The study has several strengths. It was based on prior research among Samoan women (4, 8) and the education program specifically targeted Samoan women. The study successfully balanced implementation of CBPR principles without compromising scientific fidelity and rigor. Moreover, for an 8-month prospective study, very few women were lost to attrition. There are some limitations of this study. There is no information on who declined to participate, which limits the generalizabilty of the findings. The data on mammogram use are self-report and could conceivably be biased. There is also potential sampling bias due to non-inclusion of eligible women within a church and Samoan women not affiliated with Samoan churches. It is not know how these women differed from those included in the study. Previous research (4, 8) suggests that nearly 85% of Samoans in Los Angeles and Orange counties are affiliated with Samoan churches. Furthermore, it is likely that the women excluded may be more assimilated into the “Westernized” culture that is different from traditional Samoan values and beliefs. If these assumptions are correct, they are less likely to benefit from culturally targeted cancer education programs.
In conclusion, findings from this study suggest that a multifaceted breast cancer education intervention may improve knowledge about breast cancer and increase mammogram usage in certain sub-groups of Samoan women based on their prior mammogram history. The findings also reveal the correlates of behavior change and how they differ depending on past mammogram history, and provide information for future micro-targeting of subpopulations with low mammogram utilization rates.
ACKNOWLEDGMENTS
We gratefully acknowledge the Samoan traditional and community leaders, Samoan church leaders and their congregations, and the Samoan health educators and interviewers who participated in this research.
Grant support: This research was supported in part by grants from the California Breast Cancer Research Program of the University of California (grant number 4BB-1400) and the National Center for Minority Health and Health Disparities (P60MD000532). The contents of the article are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies.
REFERENCES
- 1.Smigal C, Jemal A, Ward E, et al. Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin. 2006;56(3):168–183. doi: 10.3322/canjclin.56.3.168. [DOI] [PubMed] [Google Scholar]
- 2.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97(6):1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 3.Sassi F, Luft HS, Guadagnoli E. Reducing racial/ethnic disparities in female breast cancer: screening rates and stage at diagnosis. Am J Public Health. 2006;96(12):2165–2172. doi: 10.2105/AJPH.2005.071761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mishra SI, Luce PH, Hubbell FA. Breast cancer screening among American Samoan women. Prev Med. 2001;33(1):9–17. doi: 10.1006/pmed.2001.0845. [DOI] [PubMed] [Google Scholar]
- 5.Mishra SI, Luce-Aoelua P, Wilkens LR, Bernstein L. Cancer among American-Samoans: site-specific incidence in California and Hawaii. Int J Epidemiol. 1996;25(4):713–721. doi: 10.1093/ije/25.4.713. [DOI] [PubMed] [Google Scholar]
- 6.Mishra SI, Luce-Aoelua PH, Wilkens LR. Cancer among indigenous populations. The experience of American Samoans. Cancer. 1996;78(7 Suppl):1553–1557. [PubMed] [Google Scholar]
- 7.Mishra SI, Luce-Aoelua PH, Hubbell FA. Identifying the Cancer Control Needs of American Samoans. Asian Am Pac Isl J Health. 1998;6(2):277–285. [PubMed] [Google Scholar]
- 8.Mishra SI, Aoelua PL, Hubbell FA. Knowledge of and attitudes about cancer among American Samoans. Cancer Detect Prev. 2000;24(2):186–195. [PubMed] [Google Scholar]
- 9.Mishra SI, Bastani R, Huang D, Luce PH, Baquet CR. Mammography screening and Pacific Islanders: role of cultural and psychosocial factors. J Cancer Educ. 2007;22(1):32–36. doi: 10.1007/BF03174372. [DOI] [PubMed] [Google Scholar]
- 10.Mishra SI, Hess J, Luce PH. Predictors of indigenous healer use among Samoans. Altern Ther Health Med. 2003;9(6):64–69. [PubMed] [Google Scholar]
- 11.Bowie JV, Curbow BA, Garza MA, Dreyling EK, Benz Scott LA, McDonnell KA. A review of breast, cervical, and colorectal cancer screening interventions in older women. Cancer Control. 2005;12(Suppl 2):58–69. doi: 10.1177/1073274805012004S09. [DOI] [PubMed] [Google Scholar]
- 12.Curbow B, Bowie J, Garza MA, et al. Community-based cancer screening programs in older populations: making progress but can we do better? Prev Med. 2004;38(6):676–693. doi: 10.1016/j.ypmed.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Yabroff KR, O'Malley A, Mangan P, Mandelblatt J. Inreach and outreach interventions to improve mammography use. J Am Med Womens Assoc. 2001;56(4):166–173. 88. [PubMed] [Google Scholar]
- 14.Yabroff KR, Mandelblatt JS. Interventions targeted toward patients to increase mammography use. Cancer Epidemiol Biomarkers Prev. 1999;8(9):749–757. [PubMed] [Google Scholar]
- 15.Snell JL, Buck EL. Increasing cancer screening: a meta-analysis. Prev Med. 1996;25(6):702–707. doi: 10.1006/pmed.1996.0109. [DOI] [PubMed] [Google Scholar]
- 16.Mandelblatt JS, Yabroff KR. Effectiveness of interventions designed to increase mammography use: a meta-analysis of provider-targeted strategies. Cancer Epidemiol Biomarkers Prev. 1999;8(9):759–767. [PubMed] [Google Scholar]
- 17.Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomarkers Prev. 2002;11(1):59–71. [PubMed] [Google Scholar]
- 18.Meissner HI, Breen N, Coyne C, Legler JM, Green DT, Edwards BK. Breast and cervical cancer screening interventions: an assessment of the literature. Cancer Epidemiol Biomarkers Prev. 1998;7(10):951–961. [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Healthy People 2010. Washington, DC: U.S. Department of Health and Human Services; 2000. Jan, (Conference Edition, in Two Volumes). [Google Scholar]
- 20.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 21.Israel BA, Schulz AJ, Parker EA, Allen AJ, Guzman JR. Critical issues in developing and following community based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 22.Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 23.Bowser BP, Mishra SI, Reback CJ, Lemp GF, editors. Preventing AIDS: Community-Science Collaborations. Binghamton, NY: The Haworth Press; 2004. [Google Scholar]
- 24.U.S. Census Bureau. The Native Hawaiian and Other Pacific Islander Population: 2000. Washington, DC: U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2001. [Google Scholar]
- 25.US Preventive Services Task Force. Screening for breast cancer: summary of recommendations. [Accessed May 6, 2005];2002 Feb; Available at: http:www.ahcpr.gov/clinic/uspstf/uspsbrca.htm.
- 26.Bastani R, Maxwell AE, Bradford C, Das IP, Yan KX. Tailored risk notification for women with a family history of breast cancer. Prev Med. 1999;29(5):355–364. doi: 10.1006/pmed.1999.0556. [DOI] [PubMed] [Google Scholar]
- 27.Curry SJ, Emmons KM. Theoretical models for predicting and improving compliance with breast cancer screening. Annals of Behavioral Medicine. 1994;16(4):302–316. [Google Scholar]
- 28.Maxwell AE, Bastani R, Vida P, Warda US. Results of a randomized trial to increase breast and cervical cancer screening among Filipino American women. Prev Med. 2003;37(2):102–109. doi: 10.1016/s0091-7435(03)00088-4. [DOI] [PubMed] [Google Scholar]
- 29.Freire P. Cultural action and conscientization. Harvard Educational Review. 1977;40:452–477. [Google Scholar]
- 30.Freire P. Education as cultural action: an introduction. In: Colonnese LM, editor. Conscientization for Liberation. Washington, DC: Division of Latin Studies, U.S. Catholic Conference; 1971. [Google Scholar]
- 31.Bastani R, Marcus AC, Maxwell AE, Das IP, Yan KX. Evaluation of an intervention to increase mammography screening in Los Angeles. Prev Med. 1994;23(1):83–90. doi: 10.1006/pmed.1994.1012. [DOI] [PubMed] [Google Scholar]
- 32.Bastani R, Maxwell AE, Carbonari J, Rozelle R, Baxter J, Vernon S. Breast cancer knowledge, attitudes, and behaviors: a comparison of rural health and non-health workers. Cancer Epidemiol Biomarkers Prev. 1994;3(1):77–84. [PubMed] [Google Scholar]
- 33.Glenn B, Bastani R, Reuben D. How important are psychosocial predictors of mammography receipt among older women when immediate access is provided via on-site service? Am J Health Promot. 2006;20(4):237–246. doi: 10.4278/0890-1171-20.4.237. [DOI] [PubMed] [Google Scholar]
- 34.Maxwell AE, Bastani R, Vida P, Warda US. Strategies to recruit and retain older Filipino-American immigrants for a cancer screening study. J Community Health. 2005;30(3):167–179. doi: 10.1007/s10900-004-1956-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tai E, Yu Y-Y, Luce PH, Baquet CR, Mishra SI. Improving cervical cancer control among Pacific Islanders: evaluation of a theory-based education program. J Assoc Acad Minority Physicians. 2006;17:16–23. [Google Scholar]
- 36.Taylor VM, Yasui Y, Burke N, et al. Hepatitis B testing among Vietnamese American men. Cancer Detect Prev. 2004;28(3):170–177. doi: 10.1016/j.cdp.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tu SP, Taylor V, Yasui Y, et al. Promoting culturally appropriate colorectal cancer screening through a health educator: a randomized controlled trial. Cancer. 2006;107(5):959–966. doi: 10.1002/cncr.22091. [DOI] [PubMed] [Google Scholar]
- 38.Freire P. Creating alternative research methods: Learning to do it by doing, it. In: Hall BL, Gillette A, Tandon R, editors. Creating knowledge: A monolopy? Toronto: Participatory Research Network; 1982. pp. 29–37. [Google Scholar]
- 39.Mishra SI, Conner RF. Evaluation of an HIV prevention program among Latino farmworkers. In: Mishra SI, Conner RF, Magana JR, editors. AIDS Crossing Borders: The Spread of HIV Among Migrant Latinos. Boulder, CO: Westview Press; 1996. pp. 157–181. [Google Scholar]
- 40.Mishra SI, Chavez LR, Magana JR, Nava P, Burciaga Valdez R, Hubbell FA. Improving breast cancer control among Latinas: evaluation of a theory-based educational program. Health Educ Behav. 1998;25(5):653–670. doi: 10.1177/109019819802500511. [DOI] [PubMed] [Google Scholar]
- 41.Braun KL, Fong M, Kaanoi ME, Kamaka ML, Gotay CC. Testing a culturally appropriate, theory-based intervention to improve colorectal cancer screening among Native Hawaiians. Prev Med. 2005;40(6):619–627. doi: 10.1016/j.ypmed.2004.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hendricson WD, Russell IJ, Prihoda TJ, Jacobson JM, Rogan A, Bishop GD. An approach to developing a valid Spanish language translation of a health-status questionnaire. Med Care. 1989;27(10):959–966. doi: 10.1097/00005650-198910000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Cochran WG. Sampling Techniques. New York, NY: W. W. Wiley; 1977. [Google Scholar]