Abstract
A sample of 194 patients whose dentofacial disharmonies were severe enough to warrant an orthognathic surgical treatment option completed the SCL-90-R, a 90-item assessment tool used to measure current level of psychological distress. Two global and nine primary dimension scores of psychological distress were computed. The average interpersonal sensitivity, psychoticism, and obsessive-compulsive dimension scores were higher than the nonpsychiatric patient population norms for both males and females, but the confidence intervals for these dimensions were still in the upper end of the normal range of functioning (< 1 SD above the normative mean). No statistically significant differences by gender or age group were observed. Over 15% of the patients were clinically elevated on obsessive-compulsive behavior, interpersonal sensitivity problems, hostility, paranoid ideation, and psychoticism; and 24.7% qualified as a positive diagnosis for a psychiatric disorder. It appears that a surprisingly large number of individuals with dentofacial disharmonies who are seeking treatment consultation are experiencing a level of psychological distress that warrants intervention.
Keywords: Orthognathic surgery, Symptom Checklist-90-R (SCL-90-R), Psychological factors
People with dentofacial disharmonies may encounter psychosocial stress, either directly from teasing or indirectly from sociocultural precepts or stereotyping. Dental anomalies have been reported to be the cause of teasing1 and "general playground harassment"2 among children and are associated with lowered social attractiveness.3 Although overt teasing does not generally continue past adolescence, adolescents and adults with dentofacial deformities may encounter significant discrimination in a variety of settings because of their appearance.4–8 Cultural evidence of this stereotyping can be found, for example, in cartoons: cartoonists typically use protruding upper incisors and long face height to depict individuals of low intellect, and the caricature of a witch features a deficient upper jaw and protruding chin. Facial attractiveness is an important variable in the formation of first impressions,3–5 and there is ample evidence that in the absence of other information, unattractive people are perceived as less socially competent, less popular, and less friendly.6 Social stereotyping based on facial appearance disproportionately affects adolescents and young adults, and can be a major factor in total life adjustment.7,8
In two separate studies in which orthognathic surgery patients were interviewed preoperatively, over 60% of the patients indicated that their facial appearance had negatively influenced their personal life, and over 40% had had their social life negatively affected.9,10 The relationship between a physical condition or limitation and psychological distress has been investigated in a variety of medical populations.11–12 Infertility researchers have proposed a conceptual model, the "psychological sequelae model,"11 in which a physical limitation may result in disruption of psychological functioning in specific dimensions. In a sample of 104 married couples who had experienced difficulty in achieving conception, the elevation on the psychoticism dimension, as measured with the symptom checklist-90-R (SCL-90-R), was dramatically reduced with the removal of just one item: "The idea that something serious is wrong with your body."11 Using a similar approach in evaluating patients with rheumatoid arthritis indicated that psychological distress related to depression and hostility was related to disease severity.12 Under this model, significant psychological distress does not necessarily warrant a psychiatric label and diagnosis if the symptomatology is caused by the medical condition and/or treatment.
In a recent study of 155 patients who were undergoing an initial dentofacial evaluation, approximately one-third reported that improving their self-confidence and feelings about self were important motivations for seeking treatment, and 10% to 15% cited motivations such as improving their social life, ease in socialization, and being in public.13 Given that patients with a facial skeletal disharmony express a desire for improvement in these areas, we might expect that they would experience negative emotional reactions such as depression, anxiety, interpersonal problems, or social discomfort prior to treatment. In fact, a recent study of dentofacial patients suggested a link between global self-concept and psychological distress, with lowered self-concept associated with higher levels of psychological distress.14
Despite its intuitive appeal, support for the notion that dentofacial disharmony results in psychological distress has not been supported by the literature. The available literature generally has concluded that orthognathic surgery patients are a psychologically stable, "normal," group.15–19 "Psychologically stable" implies no current, even temporary or of short duration, psychological or emotional distress as well as no chronic psychiatric disorder. These studies have primarily reported averages that, although valuable from a research and epidemiological viewpoint, do not necessarily imply that all patients are "normal. " For example, one study19 reported an "unexpected" prevalence of patients (over one-third) who rated high in personality disturbances even though the average fell in the normal range. Thus, the percentage of patients who exceed clinical criteria for symptom report of psychological or psychiatric problems is as important as the average score.
The apparent disparity between the conceptual expectations based on patient self-report and the conclusions from previous reports on psychological status may have occurred for several reasons. The published reports (Table 1) have focused on presurgery patients rather than patients in the process of seeking and deciding on treatment options. The treatment-seeking process may be particularly stressful because patients need to focus on the possible benefit/risks of treatment options and consider the perceived impact of the disharmony on their quality of life.
Table 1.
Personality psychological instruments used in previous studies on the psychological status of orthognathic surgery patients
| Senior | Instruments used | Purpose of |
|---|---|---|
| author | assessment | |
| Kiyak16,17 | Tennessee self-concept inventory | Self-assessment of |
| self-concept/selfesteem | ||
| Eysenck's personality inventory | Neuroticism and | |
| extroversion | ||
| Rotter's internality-externality scale | Locus of control | |
| Auerbach18 | Krantz health opinion survey | Attitudes toward |
| health care | ||
| SCL-90-R | Current psychological well-being | |
| Impact message inventory | Interpersonal style of | |
| reaction | ||
| Tennessee self-concept | Self-assessment of | |
| self-esteem and | ||
| indication of personality disturbances | ||
| Flanary19 | 16 personality factor questionnaire | Traits of suspicion, |
| apprehension, tension, undisciplined self-conflict | ||
| Eysenck's Personality Inventory | Neuroticism and | |
| extroversion | ||
| Tennessee self concept inventory | Self-assessment of | |
| self concept/selfesteem and indication of personality disturbance | ||
| Family environment scale | Perceptions of family | |
| and relationship of | ||
| self to family | ||
| Million behavioral health inventory | Health coping style |
Second, the majority of instruments used in previous studies assess personality characteristics (traits) that are considered to be relatively stable, patterned ways in which an individual thinks, feels, or behaves over a long period of time rather than indicators of current psychological distress (state) or psychopathology (Table 1). Auerbach et al.18 used the SCL-90-R and reported the average T-score values for a group of 30 presurgery patients; however, the averages were not compared with normative data, and the percentage of patients who exhibited psychological distress was not reported.
Finally, as noted by Laskin,20 there may have been a shift in the patient population from the 1970s and '80s to the 1990s as the availability of treatment and social acceptance of orthognathic surgery has increased. Thus, prior studies may inaccurately or inadequately describe the current dentofacial population.
The purpose of this project was to investigate psychological distress in a consecutive series of patients seeking a diagnostic evaluation for a dentofacial disharmony at an academic care center. The SCL-90-R, an assessment tool that emphasizes the patient's psychological well-being in terms of the current level of psychological distress (i.e., a "state" measure), was used to derive both global and dimension scores of psychological distress.
The SCL-90-R was designed primarily to reflect the psychological symptom patterns of psychiatric and medical patients.21 However, the psychological sequelae model would suggest that the interpretation of certain items may be confounded since endorsement of the item may reflect the medical condition itself,(i.e., the presence of a dentofacial disharmony or behaviors/feelings associated with consideration of a costly, lengthy, and face-changing treatment) rather than frank psychopathology. For example, endorsement of the item "feeling uncomfortable eating or drinking in public" might well be a normal reaction to the dentofacial disharmony and/ or the treatment-seeking process rather than a symptom of anxiety or paranoia. A psychological distress profile of individual SCL-90-R items was also constructed to investigate whether the psychological sequelae model was appropriate for patients with a dentofacial disharmony.
Materials and methods
Subjects
Subjects between 15 and 50 years of age who had developmental anteroposterior and/or vertical problems for which an orthognathic surgical treatment plan was recommended were eligible for inclusion in this study. Preprosthetic patients and those with congenital craniofacial anomalies, deformities due to acute trauma, or a primary complaint of temporomandibular joint problems were excluded from participation because their presenting problems result from different etiologies. In accordance with the Institutional Review Board, subjects seen for a pretreatment consultation in the Dentofacial Deformities Program at the University of North Carolina between January 1,1993 and December 31,1996 were asked to participate at the time of their initial evaluation. Demographic information as well as referral source was collected for each subject.
Instrument
During the diagnostic records appointment, subjects were given a self-administered questionnaire, the SCL-90-R. This is a 90-item self-report instrument used extensively in health-related research as an outcome measure and/or as a screening tool for psychological distress and possible psychological disorders.11,12, 22,23 Each item is rated using a five-point scale from "not at all (0)" to "extremely (4)" as a response to the question "Within the past 7 days, how much were you distressed by…?"
The subjects were told that the intent of the questionnaire was to provide information about how they felt about themselves, and they were given standardized instructions on how to complete the questionnaire. Subjects were asked to complete the SCL-90-R at the initial appointment. If subjects requested, they were allowed to take the questionnaire home to complete with instructions to bring the questionnaire with them to their next appointment.
Data analysis
Nine primary dimensions were calculated from the SCL-90-R items according to the instructions from the manual.21 Descriptions of these dimensions are given in Table 2. Published internal consistency measures for the dimensions range from .77 to .90. Test/retest reliability estimates range from .78 to .90. Cronbach's alpha computed for this sample for the nine dimensions ranged from .70 to .90. The raw scores of each dimension were converted, using the nonpsychiatric patient norms, to standardized T-scores that are specific for each sex. A T-score distribution has a median of 50 and a standard deviation of 10. T-scores are used for ease in interpretation and to control for the significant relationships between sex and levels of psychopathology.
Table 2.
Description of the global indices and primary dimensions of SCL-90-R
| Description | |
|---|---|
| Global indices | |
| Caseness/positive diagnosis | One or more criteria for psychiatric diagnosis |
| Global severity index (GSI) | Overall indicator of psychopathology |
| Primary dimensions | |
| Obsessive-compulsive (O-C) | Thoughts, impulses, and actions that are unwanted but are unremitting or irresistible to the individual |
| Interpersonal sensitivity (INT) | Feelings of personal inadequacy and inferiority |
| Depression (DEP) | Feelings reflective of the manifestations of clinical depression |
| Paranoid ideation (PAR) | Symptoms indicative of psychotic illness, including suspiciousness, grandiosity, fear, and hostility |
| Psychoticism (PSY) | Feelings of interpersonal alienation, symptoms of schizophrenia, withdrawn schizoid features |
| Anxiety (ANX) | Symptoms and signs associated with high levels of manifest anxiety (trembling, panic attacks, feelings of terror) |
| Somatization (SOM) | Distress arising from perceptions of bodily dysfunction |
| Hostility (HOS) | Thoughts, feelings, actions typical of anger |
| Phobic anxiety (PH) | Fear response to a stimulus that is disproportionate to the stimulus; avoidance or escape behavior |
Two global scores were also computed. The global severity index (GSI) is an overall psychological distress measure that provides a single summary measure that combines information on both the number of symptoms and the intensity of perceived distress. Another indication of the level of current psychological distress is represented by "caseness" or "positive diagnosis." Caseness is a measure developed as an epidemiological screening measure for psychiatric disorder. According to caseness criteria, an individual is considered to have a psychiatric diagnosis if the GSI is above a T-score of 63 or if any two dimension scores exceed T-scores of 63.
Separate 95% confidence intervals were calculated for each T-score dimension mean for males and females. Confidence intervals were used to provide an estimate of the average psychological status for male and female dentofacial deformity patients seeking treatment as well as an indication of the variability that could be expected in these mean estimates due to sampling.
Data were also examined in terms of the percentage of patients whose dimension scores were clinically elevated. For this study, a T-score that exceeded 63 in a given SCL-90-R dimension was considered to represent clinically significant psychological distress in that dimension. This cutoff was selected because the definition of caseness is based on the criterion of a T-score of at least 63.21 Fisher exact tests were used to compare frequencies of distressed patients for the SCL-90-R dimensions between males and females and between younger (25 and younger) and older patients. Level of significance was set at 0.025 to adjust for the multiple pairwise comparisons performed within each SCL-90-R dimension.
The authors subjectively reviewed each of the SCL-90-R items. Those items that the authors believed could be hypothesized as normal responses to a dentofacial disharmony and/or treatment-seeking are listed in Table 3. The percentage of participants who rated their distress as moderate (2) or greater was calculated for each of these items. Corrected subscale scores were calculated using the prorating methodology described in the SCL-90-R manual21 after these items had been removed. The intent was to assess whether these items were confounding the assessment of psychological distress.
Table 3.
SCL-90-R items with a possibly confounded interpretation for patients with a dentofacial disharmony
| Dimension | Item | % distressed* |
|---|---|---|
| O-C | Feeling blocked in getting things done | 17.2 |
| INT | Feeling very self-conscious with others | 15.6 |
| INT | Feeling uneasy when people are watching or talking about you | 13.4 |
| INT | Feeling others do not understand you or are unsympathetic | 11.4 |
| INT | Feeling uncomfortable about eating or drinking in public | 7.8 |
| PAR | Feeling that you are watched or talked about by others | 9.4 |
| PH | Feeling uneasy in crowds, such as shopping or at a movie | 7.7 |
| PSY | The idea that something serious is wrong with your body | 6.2 |
| PSY | Feeling lonely even when you are with people | 5.2 |
Frequency of subjects who rated their distress as moderate (2), quite a bit (3), or extreme (4)
Results
Subjects
Of the 222 eligible patients, 194 agreed to participate in this project and signed an informed consent form. One hundred twenty two (63%) were female and 80% were Caucasian. The mean age was 25.9 (std = 9.8 yr.) and 55% were 25 or younger at the consultation appointment. Thirty percent had had previous orthodontic treatment and 8% had undergone previous facial surgery. The primary referral source for these patients was an orthodontist or dentist (65%), but 35% were self-referred or referred by a friend or family member. Fifty-eight percent of these patients elected to proceed with the surgical treatment option, 15% chose camouflage orthodontic treatment only, and 19% elected not to have treatment. The remainder of the patients (8%) were undecided about treatment 6 months after the case presentation.
Psychiatric morbidity
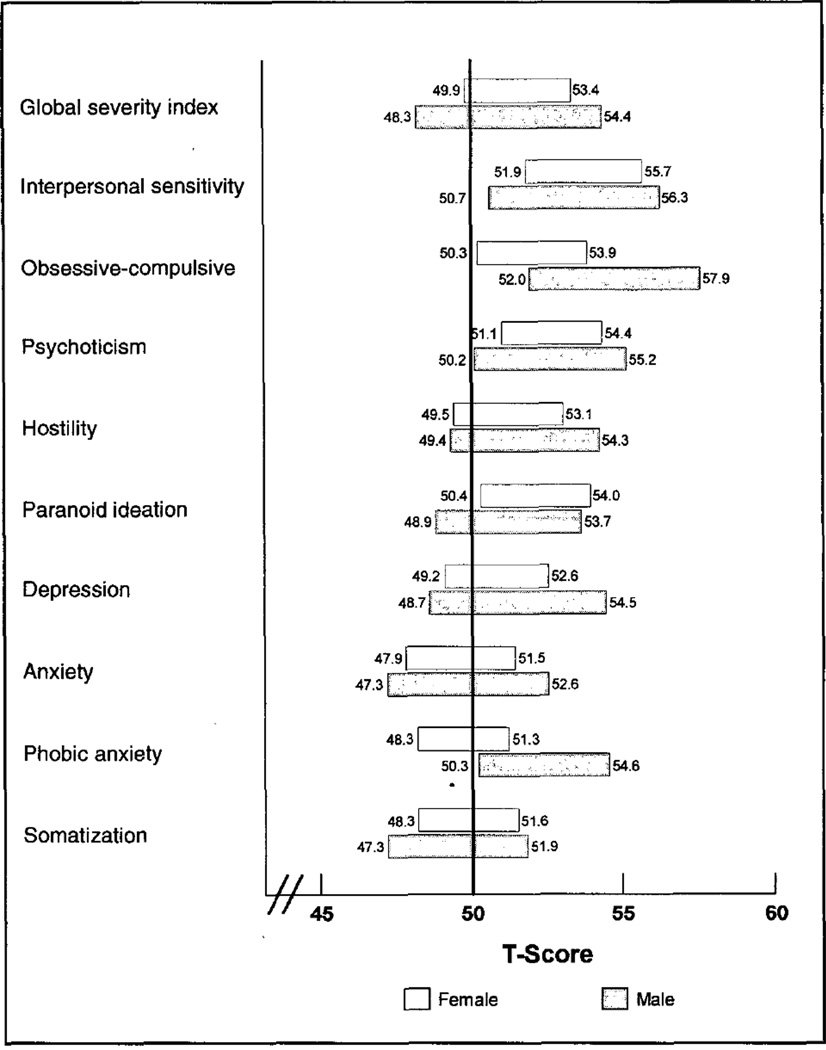
The 95% confidence intervals for the SCL-90-R scales for males and females seeking a diagnostic evaluation for a dentofacial disharmony are illustrated in Figure 1. The confidence intervals did not include, for either males or females, the nonpatient population norm (a T-score of 50)21 for the interpersonal sensitivity, psychoticism, or obsessive-compulsive dimensions. Thus, we are 95% sure that dentofacial disharmony patients are reporting higher than average distress on these dimensions than would a normative population. Compared with population norms, males were higher on the phobic anxiety dimension and females on the paranoid ideation dimension. For these five dimensions the confidence intervals indicate a mild elevation of distress. None of the upper confidence bounds exceeded the 60th percentile (1 standard deviation above the nonpsychiatric patient means) and were not indicative, on average, of psychiatric disorder in patients with a dentofacial disharmony seeking a treatment consultation.
Figure 1.
95% confidence intervals for the SCL-90-R dimensions for males and females. Lower and upper boundaries for each condifence interval are given outside the box. Since the intervals are given in T-scores, the normative population average for all dimensions is 50.
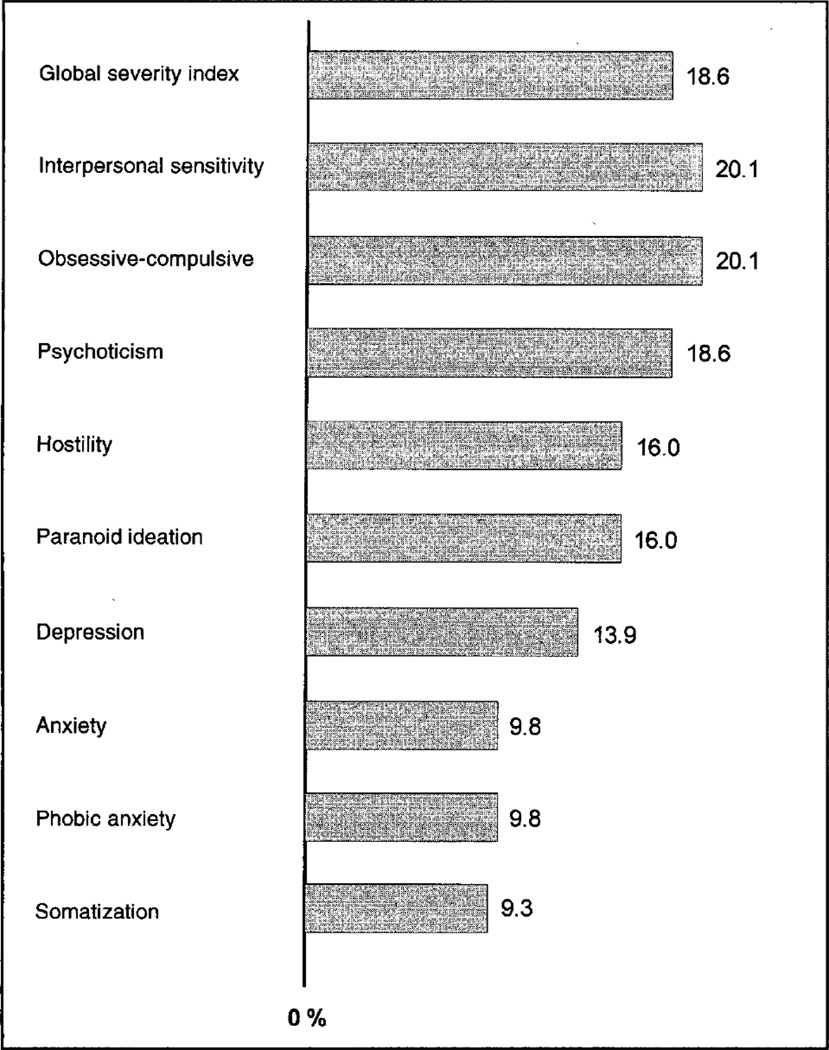
Over 15% of the patients had clinically elevated scores for obsessive-compulsive behavior, interpersonal sensitivity problems, hostility, paranoid ideation, or psychoticism (Figure 2). Sixteen percent of the patients had elevated scores on one scale, and 24.7% on two or more scales. Nineteen percent of the patients had an elevated GSI score, the most sensitive single indicator of psychological distress, and 24.7% of the patients met the criteria for a psychiatric diagnosis ("caseness").
Figure 2.
Percent of patients who exceeded a T-score of 63 on a SCL-90-R dimension
Although there were no statistically significant differences between younger and older patients (all p-values exceeded 0.05), a higher percentage of the younger patients were "distressed" on six of the nine dimensions. The difference in percentages ranged from 1% on obsessive-compulsive and phobic anxiety to 9% on the hostility dimension (25+: 11%; <=25:20%). A higher percentage of the younger patients had elevated GSI scores and had a positive diagnosis but the differences were small, 1% and 3%, respectively. There were no statistically significant differences between males and females (all p-values exceeded 0.05) in the percentages of distressed individuals although a higher percentage of males were distressed on seven of the dimensions. The difference in percentages ranged from 1 % on somatization to 8% on psychoticism (males: 24%; females: 16%). A higher percentage of males had elevated GSI scores (22% vs. 16%) and had a positive psychiatric diagnosis (31% vs. 21%). Even with a sample size of 194, there is insufficient power to detect statistically significant differences in proportions of these magnitudes.
Item analysis
The percentage of patients who endorsed the specific items listed in Table 3 ranged from 5.2% to 17.2%. The average T-score decreased dramatically for interpersonal sensitivity in both males and females (adjusted male mean, 41.0; adjusted female mean, 39.0) when dimension scores were recomputed after those items had been removed. But the average T-score for the other dimensions (paranoid ideation, psychoticism, obsessive-compulsive, and phobic anxiety) did not decrease. The percentage of patients with a positive diagnosis (caseness) was not substantially lowered (24.7% to 22.7%) when these nine items were removed.
The pattern of the most frequently endorsed items rated at least as moderately distressing indicates a profile of distress that was not expected. Only one of the theorized confounding items, "Feeling blocked in getting things done," appeared in the empirical profiles, and then only for males. Ten of the 15 items were common to both sexes (Tables 4 and 5).
Table 4.
Distress profile of female patients with a facial skeletal disharmony seeking a treatment consultation.
| Dimension | Item | % distressed |
|---|---|---|
| SOM | Headaches | 39.4% |
| DEP | Worrying too much about things | 34.5% |
| HOS | Feeling easily annoyed or irritated | 33.6% |
| DEP | Feeling low in energy or slowed down | 26.2% |
| INT | Your feelings being easily hurt | 19.8% |
| SOM | Pains in lower back | 20.5% |
| ANX | Nervousness or shakiness inside | 18.0% |
| O-C | Trouble remembering things | 18.8% |
| ANX | Feeling tense or keyed up | 18.0% |
| INT | Feeling critical of others | 16.4% |
| — | Trouble falling asleep | 17.4% |
| O-C | Trouble concentrating | 14.8% |
| — | Difficulty making decisions | 18.9% |
| O-C | Worried about sloppiness or carelessness | 19.7% |
| SOM | Soreness of your muscles | 17.2% |
The 15 most frequently endorsed SCL-90-R items that were rated at least at the moderately distressing level. For these 15 items, the percentage of subjects who rated their distress as moderate (2), quite a bit (3), or extreme (4)s presented as the percent distressed.
Table 5.
Distress profile of male patients with a facial skeletal disharmony seeking a treatment consultation.
| Dimension | Item | % distressed |
|---|---|---|
| HOS | Feeling easily annoyed or irritated | 23.7% |
| DEP | Worrying too much about things | 20.9% |
| O-C | Worried about sloppiness or carelessness | 20.9% |
| DEP | Feeling low in energy or slowed down | 18.1% |
| O-C | Feeling blocked in getting things done | 20.9% |
| SOM | Headaches | 15.3% |
| ANX | Feeling tense or keyed up | 22.5% |
| O-C | Having to check and double-check what you do | 18.3% |
| INT | Feeling critical of others | 13.9% |
| O-C | Trouble concentrating | 28.3% |
| O-C | Having to do things very slowly to insure correctness | 15.5% |
| O-C | Trouble remembering things | 13.9% |
| O-C | Repeated unpleasant thoughts that won't leave your mind | 16.6% |
| SOM | Pains in lower back | 18.1% |
| — | Feeling that people will take advantage of you if you let them | 14.1% |
The 15 most frequently endorsed SCL-90-R items that were rated at least at the moderately distressing level. For these 15 items, the percentage of subjects who rated their distress as moderate (2), quite a bit (3), or extreme (4) is presented as the percent distressed.
Discussion
Psychiatric morbidity
Examination of the 95% confidence intervals suggests a slight elevation in psychological distress, on average, in patients seeking a diagnostic consultation for a facial skeletal disharmony. These elevations do not indicate frank psycho-pathology for the group as a whole. Auerbach18 reported average T-scores that were, in fact, higher than those reported here, but no statistical comparison was made with "normative" values.
A quarter of the patients in this study had levels of psychological distress that warranted a positive psychiatric diagnosis using the SCL-90-R as a screening assessment. This criterion is used to identify individuals with sufficiently pronounced distress to warrant intervention. This proportion is slightly lower than that reported by Flanary et al.19 using a different instrument. But this rate is almost 1.5 times higher than that usually reported for the general population.24 Almost 20% of the patients had significantly elevated scores on the global severity index (GSI). Elevations on this index, the single most sensitive indication of psychological distress on the SCL-90-R, is particularly noteworthy since the GSI represents a composite of dimensions. Such multifaceted distress may require consultation, and possibly counseling, with a mental health specialist. This is particularly important to clinicians treating orthognathic surgery patients since the medical literature suggests that anxiety, depression, and body concerns are associated with exaggerated health complaints and poor adjustment to treatment.25–27
Sex differences
No statistically significant sex differences in the proportion of clinically distressed individuals were noted, although a larger proportion of males reported clinical levels of distress on seven of the dimensions and on the two global scores. Despite the fact that men and women, on average, reported comparable levels of elevated interpersonal sensitivity, a higher percentage of men who sought consultation for a dentofacial disharmony at UNC reported social reasons for seeking surgery compared with women.13 It may be that men report being more motivated by social concerns because they more readily expect social fulfillment to result from esthetic improvements. Support for this lies in one study's finding that facial attractiveness was more predictive of overall male social functioning than female.28
Psychological sequelae model
By eliminating "social discomfort" items that might be hypothesized to be associated with a skeletal disharmony, distress scores on interpersonal sensitivity dropped markedly. However, psychological distress in other dimensions remained surprisingly high, and the percentage of positive psychiatric diagnoses decreased by only 2%. Therefore, the psychological distress exhibited by these patients is not due primarily to interpersonal sensitivity issues. Obsessive-compulsive symptoms, psychoticism, paranoid ideation, and phobic anxiety are clearly signs of psychological distress, but not the types of distress reported in the literature on the effects of physical unattractiveness. In fact, even studies of adults and children with facial deformities due to cleft lip/palate have failed to uncover psychological symptoms apart from social anxiety/excessive shyness.29–30 The psychological sequelae model (whereby an impairment in physical functioning is expected to result in psychological distress) appears to be an appropriate conceptual model for patients with infertility problems11 or rheumatoid arthritis,12 but our results provide only mixed support for this conceptualization in the dentofacial population.
Clinical implications
Elevations on SCL-90-R dimensions and global indices should not be regarded as indications of major psychiatric disorders or negative personality traits that might contraindicate orthognathic surgery. In comparing the SCL-90-R with the DSM-III diagnostic criteria, the majority of SCL-90-R diagnoses were adjustment disorders, e.g., emotional problems, depressed mood, or anxious mood, rather than major psychiatric disorders.31 Elevations on the SCL-90-R would best be interpreted as psychological strain or discomfort that might well benefit from psychological intervention or extra attention and support from the clinician and staff.
Pogrel and Scott32 suggested that routine pre-operative psychological evaluation is not needed, but that certain types of patients (difficult patients, patients with excessive symptoms, and patients with poor support systems) should be referred for counseling. In fact, patients who were rated by their surgeon as submissive tended to have poorer immediate postsurgical adjustment, while those rated by their surgeon as dominant had higher psychological distress before and after surgery.18 In addition, patients who are uninvolved and disinterested in their treatment generally do not cope as well with problems and are more likely to become angry and hostile.33
It is difficult, if not impossible, to adequately screen patients for psychological distress in the course of a diagnostic interview or case presentation. Clinicians have several options. They can depend on their own interview and perceptive skills for evaluation, or they can ask patients to complete a standardized test and refer patients who have clinically elevated scores for diagnosis and counseling. If standardized tests are used, the clinician should establish a working relationship with a mental health professional who could review test profiles that indicate endorsement of extreme items.
A mental health referral is recommended for those patients experiencing a high level of psychological distress. Certainly patients who endorse items suggestive of psychotic illness (e.g., someone else controls their thoughts or they hear voices that others do not), overt hostility (urges to harm someone else), or suicide should be referred for psychological evaluation. Counseling, if viewed by the clinician as a constructive option for addressing life problems, can be recommended without offending the patient. Good patient management requires that a clinician assess whether a patient is cognitively competent to make a decision, is experiencing any stressors that may complicate or interfere with the progress of treatment and recovery from surgery, and has realistic expectations associated with treatment.
The prognosis for patients with clinically elevated psychological distress is unclear. Those patients may be the most pleased with the surgical change or they may be at increased risk for dissatisfaction. Neuroticism, a personality trait that indicates emotional lability and overreactivity, has been correlated with dissatisfaction, negative mood, and patient self-report of postsurgical swelling, pain, or paresthesia,17,34,35 although the association has not been observed consistently during recovery. Whether a patient who is experiencing high psychological distress or psychopathology before surgery will have a poorer postsurgical adjustment and increased dissatisfaction is not known.
Conclusions
The findings from this sample of patients with dentofacial disharmonies seeking a treatment consultation at an academic care center indicate that:
Males and females exhibit, on average, a mild increase in psychological distress on interpersonal sensitivity, obsessive-compulsive, and psychoticism dimensions, but this elevation is not indicative of psychopathology as a whole.
A quarter of the patients qualified as a positive diagnosis of a psychiatric disorder using the SCL-90-R criterion. Removal of items from the interpersonal sensitivity dimension that might be related to the presence of a moderate to severe dentofacial disharmony reduced the percentage of positive diagnoses by only 2%.
Orthodontists and oral and maxillofacial surgeons should be alert to symptoms reflecting psychological distress, as well as psychiatric morbidity, in patients with a dentofacial disharmony.
Acknowledgment
The authors gratefully acknowledge the assistance of Steven Dickens and Debora Price. This project was supported by NIH DE 10028 and NIH DE 05215.
Contributor Information
Ceib Phillips, Department of Orthodontics, School of Dentistry, University of North Carolina, Chapel Hill, North Carolina.
M. Elizabeth Bennett, Department of Orthodontics, School of Dentistry, University of North Carolina, Chapel Hill, North Carolina.
Hillary L. Broder, Division of Behavioral Sciences, University of Medicine and Dentistry of New Jersey, New Jersey Dental School, Newark, New Jersey.
References
- 1.Kilpelanien P, Phillips C, Tulloch JFC. Anterior tooth position and motivation for early treatment. Angle Orthod. 1993;63:171–174. doi: 10.1043/0003-3219(1993)063<0171:ATPAMF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Shaw WC, Meek S, Jones D. Nicknames, teasing, harassment and the salience of dental features among school children. Br J Orthod. 1980;7:75–80. doi: 10.1179/bjo.7.2.75. [DOI] [PubMed] [Google Scholar]
- 3.Shaw WC. The influence of children’s dentofacial appearance on their social attractiveness as judged by peers and lay adults. Am J Orthod. 1981;79:399–415. doi: 10.1016/0002-9416(81)90382-1. [DOI] [PubMed] [Google Scholar]
- 4.Tagiuri R. Person perception. In: Lindzey G, Aronson E, editors. The handbook of social psychology. 2nd edition. Reading, Mass: Addison-Wesley; 1969. [Google Scholar]
- 5.Goffman E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- 6.Bull R, Rumsey N. The social psychology of facial appearance. New York: Springer-Verlag; 1988. [Google Scholar]
- 7.Berscheid E. An overview of the psychological effects of physical attractiveness. In: Lucker GW, Ribbens KA, McNamara JA Jr, editors. Psychological aspects of facial form. Ann Arbor, Mich: Craniofacial Growth Series, Monograph # 11; 1980. pp. 1–23. [Google Scholar]
- 8.Adams G. The effects of physical attractiveness on the socialization process. In: Lucker GW, Ribbens KA, McNamara JA Jr, editors. Psychological aspects of facial form. Ann Arbor, Mich: Craniofacial Growth Series, Monograph # 11; 1980. pp. 25–47. [Google Scholar]
- 9.Barbosa ALB, Marcantonio E, Barbosa CEdM, Gabrielli MFR, Gabrielli MAC. Psychological evaluation of patients scheduled for orthognathic surgery. J Nihon Univ Scho Dent. 1993;35:l–9. doi: 10.2334/josnusd1959.35.1. [DOI] [PubMed] [Google Scholar]
- 10.Garvill J, Garvill H, Kahnberg KE, Lundgren S. Psychological factors in orthognathic surgery. J Cranio-Maxillo-Facial Surgery. 1992;20:28–33. doi: 10.1016/s1010-5182(05)80193-3. [DOI] [PubMed] [Google Scholar]
- 11.Berg BJ, Wilson FJ. Psychiatric morbidity in the infertile population: A reconceptualization. Fertility and Sterility. 1990;53:654–661. [PubMed] [Google Scholar]
- 12.Parker JC, Buckelew SP, Smarr KL, Buescher KL, Beck NC, Frank RG, Anderson SK, Walker SE. Psychological screening in rheumatoid arthritis. J Rheumatol. 1990;17:1016–1021. [PubMed] [Google Scholar]
- 13.Phillips C, Broder HL, Bennett ME. Dentofacial disharmony: Motivations for seeking treatment. Int J Adult Orthod Orthognath Surg. 1997;12:7–15. [PMC free article] [PubMed] [Google Scholar]
- 14.van Steenbergen E, Nanda R. Presurgical satisfaction with facial appearance in orthognathic surgery patients. Am J Orthod Dentofac Orthop. 1996;110:653–659. doi: 10.1016/s0889-5406(96)70078-1. [DOI] [PubMed] [Google Scholar]
- 15.Sachs RHJ. Assessment of readiness of patients desiring treatment of dentofacial anomalies. J Oral Surg. 1981;39:113–116. [PubMed] [Google Scholar]
- 16.Kiyak HA, McNeill RW, West RA, Hohl T, Bucher F, Sherrick P. Predicting psychologic responses to orthognathic surgery. J Oral Surg. 1982;40:150–156. doi: 10.1016/0278-2391(82)90046-5. [DOI] [PubMed] [Google Scholar]
- 17.Kiyak HA, McNeill RW, West RA, Hohl T, Heaton P. Personality characteristics as predictors and sequelae of surgical and conventional orthodontics. Am J Orthod. 1986;89:383–392. doi: 10.1016/0002-9416(86)90069-2. [DOI] [PubMed] [Google Scholar]
- 18.Auerbach SM, Meredity J, Alexander JM, Mercuri LG, Brophy C. Psychological factors in adjustment to orthognathic surgery. J Oral Maxillofac Surg. 1984;42:435–440. doi: 10.1016/0278-2391(84)90229-5. [DOI] [PubMed] [Google Scholar]
- 19.Flanary CM, Barnwell GM, VanSickels JE, Littlefield JH, Rugh AL. Impact of orthognathic surgery on normal and abnormal personality dimensions: A 2-year follow-up study of 61 patients. Am J Orthod Dentofac Orthop. 1990;98:313–322. doi: 10.1016/S0889-5406(05)81488-X. [DOI] [PubMed] [Google Scholar]
- 20.Laskin DM. What it takes to make a pretty face. J Oral Maxillofac Surg. 1990;48:1138. doi: 10.1016/0278-2391(90)90527-9. [DOI] [PubMed] [Google Scholar]
- 21.Derogatis LR. The SCL-90 administration, scoring and procedures manual. Baltimore: Johns Hopkins University Press; 1977. [Google Scholar]
- 22.Craig TJ, Jandorf L, Rubinstein J. Interrater and observer/self report correlation of psychopathology in routine clinical practice. Annals of Clinical Psychiatry. 1995;7:25–31. doi: 10.3109/10401239509149021. [DOI] [PubMed] [Google Scholar]
- 23.Kinney RK, Gatchel JR, Mayer TG. The SCL-90-R evaluated as an alternative to the MMPI for psychological screening of chronic low-back pain patients. Spine. 1991;16:940–942. doi: 10.1097/00007632-199108000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Weissman MM, Meyers JK. Affective disorders in a US urban community. Arch Gen Psychiatry. 1978;35:1304–1311. doi: 10.1001/archpsyc.1978.01770350030002. [DOI] [PubMed] [Google Scholar]
- 25.Kellnar R. Functional somatic symptoms and hypochondriasis. A survey of empirical studies. Arch Gen Psych. 1985;42:821–833. doi: 10.1001/archpsyc.1985.01790310089012. [DOI] [PubMed] [Google Scholar]
- 26.Croyule RT, Kuretsky MB. Effects of mood on self- appraisal of health status. Health Psych. 1987;6:239–253. doi: 10.1037//0278-6133.6.3.239. [DOI] [PubMed] [Google Scholar]
- 27.Lipowski ZJ. Somatization and depression. J Psychosom Med. 1990;31:13–18. doi: 10.1016/S0033-3182(90)72212-8. [DOI] [PubMed] [Google Scholar]
- 28.Reis H, Nezlek J, Wheeler L. Physical attractiveness in social interaction. J Person Soc Psych. 1980;38:604–617. [Google Scholar]
- 29.Bennett ME. The psychological and social consequence of facial disfigurement in children. Facial Plastic Surgery. 1195;11:76–81. doi: 10.1055/s-2008-1064521. [DOI] [PubMed] [Google Scholar]
- 30.Bennett ME, Stanton ML. Psychotherapy for persons with craniofacial deformities: Can we treat without theory? Cleft Palate Craniofacial J. 1993;30:406–410. doi: 10.1597/1545-1569_1993_030_0406_pfpwcd_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 31.Derogatis LR, Morrow GR, Fetting J, Penman D, Piasetsky S, Schmale AM, et al. The prevalence of psychiatric disorders among cancer patients. J Am Med Assoc. 1983;249:751–757. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 32.Pogrel MA, Scott P. Is it possible to identify the psychologically "bad risk" orthognathic surgery patient preoperatively? Int J Adult Orthod Orthognath Surg. 1994;9:105–110. [PubMed] [Google Scholar]
- 33.Flood AB, Lorence DP, Ding J, et al. The role of expecations in patients’ reports of post-operative outcomes and improvement following therapy. Medical Care. 1993;31:1043–1056. doi: 10.1097/00005650-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Kiyak HA, McNeill RW, West RA. The emotional impact of orthognathic surgery and conventional orthodontics. Am J Orthod. 1985;88:224–234. doi: 10.1016/s0002-9416(85)90217-9. [DOI] [PubMed] [Google Scholar]
- 35.Neal CE, Kiyak HA. Patient perception of pain, paresthesia, and swelling after orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1991;6:169–181. [PubMed] [Google Scholar]