Abstract
Background
Frail older inpatients are at risk of unintended adverse events while in hospital, particularly falls, functional decline, delirium and incontinence.
Objective
The aim of this pragmatic trial was to pilot and evaluate a multi-component knowledge translation intervention that incorporated a nurse-initiated computerized clinical decision support tool to reduce harms in the care of older medical inpatients.
Methods
A stepped wedge trial design was conducted on six medical units at two hospitals in Calgary, Alberta, Canada. The primary quantitative outcome was the rate of order set use. Secondary outcomes included the number of falls, the average number of days in hospital, and the total number of consults ordered for each of orthopedics, geriatrics, psychiatry and physiotherapy. Qualitative analysis included interviews with nurses to explore barriers and facilitators around the implementation of the electronic decision support tool.
Results
The estimated mean rate of order set use over a 2 week period was 3.1 (95% CI 1.9–5.3) sets higher after the intervention than before. The estimated odds of a fall happening on a unit over a 2-week period was 9.3 (p = 0.065) times higher before than after the intervention. There was no significant effect of the intervention on length of hospital stay (p = 0.67) or consults to related clinical services (all p <0.2). Interviews with front-line nurses and nurse managers/educators revealed that the order set is not being regularly ordered because its content is perceived as part of good nursing care and due to the high workload on these busy medical units.
Conclusions
Although not statistically significant, a reduction in the number of falls as a result of the intervention was noted. Frontline users’ engagement is crucial for the successful implementation of any decision support tool. New strategies of implementation will be evaluated before broad dissemination of this knowledge translation intervention.
Keywords: Computerized order set, falls, older inpatients, knowledge translation
1. Background
Current models of hospital care often put a frail older individual at risk of falling, declining in function, becoming delirious, and ultimately being discharged to a long-term care facility [1–3]. Several hospital-related factors can increase these risks including the use of physical restraints, malnutrition and dehydration, the use of urinary catheters, the addition of new medications, and iatrogenic events [1, 4].
Falls occur in 1–2% of hospitalized older patients [1] and 1 in every 3 older adults is discharged from hospital at a higher level of disability than when they were admitted [2]. There is evidence available to guide us on fracture prevention that includes conducting falls prevention risk assessments [5] and initiating therapy with calcium, vitamin D, and drugs that treat osteoporosis [6]. There is less robust evidence to support multi-component falls prevention strategies [7–9]. However, interventions that include delirium prevention strategies, regular toileting routines, adjusting bed height, addressing postural hypotension and consulting physiotherapy can be implemented in hospital among those older in-patients determined to be at risk of falling.
Delirium occurs in 25–65% of hospitalized older patients [3, 10, 11] and has been associated with death, longer length of hospital stay, increased hospital-acquired complications, persistent cognitive deficits and increased discharge rates to long-term care [12–15]. Multiple factors usually contribute to the development of delirium and randomized trials have shown multi-component preventative strategies to be most effective [16]. The evidence supporting management strategies once delirium has occurred is less robust [16]. However, delirium management strategies must include measures to improve its detection [17].
The prevalence rate of urinary incontinence is up to 55% among older women and 35% among older men [18]. There is high quality evidence to support the diagnosis and management of urinary incontinence in hospitalized older patients (e.g. behavioral interventions such as prompted voiding or timed toileting) [19, 20].
2. Objectives
Clinical decision support provided to physicians has been found to improve practitioner performance and possibly patient outcomes [21–23]. The impact on nursing practice is less clear. The objective of this study was to evaluate the impact of a nurse-initiated computerized clinical decision support system that incorporated evidence-informed point of care strategies for preventing falls, functional decline and delirium among hospitalized older patients. This pragmatic trial focused on piloting and evaluating the implementation of a multi-component knowledge translation (KT) intervention that incorporated a clinical decision support tool to reduce harms in the care of older medical inpatients. The intervention targeted the care nurses provide to older medical patients in acute care hospitals. We used two frameworks to inform this activity, the MRC framework for complex interventions and the Knowledge to Action Cycle [24, 25]. This multi-component KT intervention utilized computerized clinical decision support, along with several different continuing education strategies [26]. The objective of this trial was to explore usage rates of the KT intervention, its impact on nursing practice, and the barriers and facilitators to its use.
3. Methods
A stepped wedge trial design [27] was conducted on six medical units at two hospitals in Calgary, Alberta, Canada. The intervention was sequentially rolled out (i.e. in-serviced) on a new unit every two weeks for a total of 12 weeks of study. All six units received the intervention, although the order in which units received the intervention was staggered. Until the intervention was rolled out on a unit, it acted as a control unit for purposes of analysis. Due to practical and scheduling issues within these active clinical units we were unable to randomize the units in terms of rollout order. However, all the units involved were medical units with similar staffing structures and all had previously shown a desire to work with the geriatric team. The intervention involved three components:
-
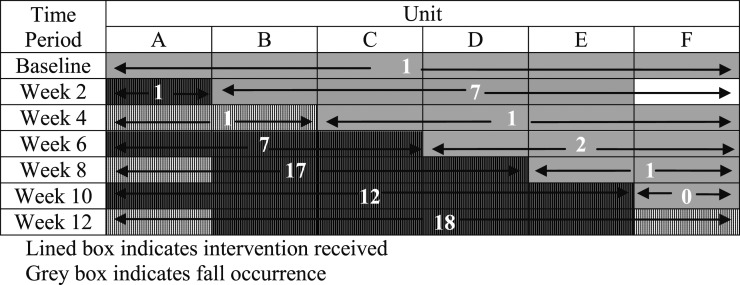
1.
An electronic nurse-initiated order set (e.g. delirium and fall risk screening; regular reorientation, ambulation and toileting protocols; feeding assistance; bowel routines; falls prevention strategies; non-pharmacological sleep routines; pain monitoring; encouragement of independence in activities of daily living) orderable by nurses from within a menu of common order sets for medical patients (►Fig. 1),
-
2.
educational in-servicing (e.g. education about relevant age related changes and evidence-informed strategies to provide optimal care to the older in-patient), and
-
3.
a binder of geriatric resource materials (e.g. cognitive and depression screening; behavioural mapping; non-pharmacologic delirium prevention strategies; falls screening and prevention; normal age related changes).
Figure 1.
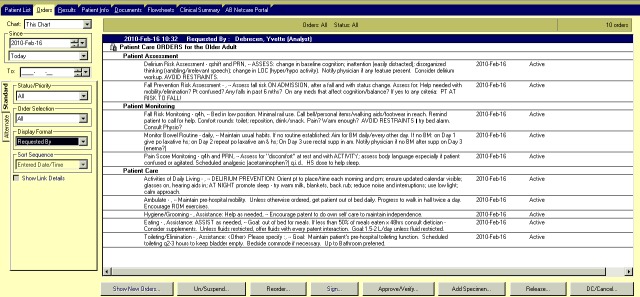
Electronic nurse-initiated order set
The electronic nurse-initiated geriatric order set was developed by a multi-disciplinary team using evidence obtained from published clinical trials, systematic reviews and practice guidelines [3, 6–9, 16, 20, 28–30]. The order set incorporates the current best evidence aimed at addressing delirium, falls, continence promotion, and optimal nutrition and hydration. Issues of workflow impact and sustainability were considered during development. The order set was made available within the hospitals’ electronic medical record, after it was vetted by frontline nurses, nurse educators and managers, local professional practice leaders, nursing council and clinical informaticians. The research team and local geriatric clinical nurse specialists developed standardized educational materials containing information that supported the electronic order set and the overall care of the older medical inpatient. The brief in-servicing (i.e. 15 minutes) was conducted on a new unit at the start of every 2-week study period. It was offered multiple times on each unit in order to help ensure the majority of unit nurses had the opportunity to attend, and it was kept brief in order to allow nurses to attend during a work shift. At the start of the 12-week rollout, the order set was available to all users of the electronic medical record but the unit nurses were not informed about its presence until the educational in-servicing.
We used a mixed methods approach to analysis. Data was collected from the electronic medical record of all patients 65 years of age or older who were residing on the study units on the days of data collection (ranging from 17–44 patients per unit per data collection period), which were at baseline and then once at the end of every 2-week study period over the 12-weeks of study. The primary quantitative outcome was the rate of use of the order set, as determined by the number of patients 65 years or older with the order set on their electronic medical record compared to the total number of patients 65 years or older on the units at the time of data collection. This process outcome was chosen in order to help determine how effectively the evidence-based strategies were incorporated into routine clinical care.
Secondary outcomes included the number of falls as documented on incidence reports, the average number of days in hospital, and the total number of consults ordered for each of orthopedics, geriatrics, psychiatry and physiotherapy. Given that incidence reports do not identify the patient, and therefore several fall reports could be generated by one person who falls frequently within an assessment period, the outcome of falls was considered as either no incidence reports versus one or more incidence reports within a given assessment period. Data was extracted from the electronic medical record using data queries based on unit and age. The unit of analysis was the medical unit. Given data was collected at the unit level and included no individual identifying data, and the fact that the intervention was considered usual best evidence clinical care the Ethics Board waived the need to obtain individual patient consent. The data were first explored with descriptive statistics including means and medians for continuous variables and frequencies for categorical data.
Repeated measures models were used to assess a time by intervention effect on outcomes using transformations as needed to meet model assumptions. Upon finding no evidence of a time effect, straightforward linear regression and logistic models were used to test for the effect of the intervention, while adjusting for number of patients and testing covariate effects of average age, average length of stay, percentage of female patients and unit [31].
The qualitative analysis included interviews that were conducted approximately six months after the completion of the 12 week roll out. Nursing staff from four of the six medical units agreed to participate in interviews. Interviews were conducted on each unit during a time approved by the unit nurse manager (i.e. when the manager and/or educator were available on the unit to be interviewed). Unit nurses were recruited with the assistance of the unit nurse managers and using snowball sampling, although the numbers were limited by nurse availability on these busy medical units. Frontline nurses, unit nurse managers and educators were interviewed in order to explore issues around the implementation of the KT intervention. Interviews were delayed until six months after roll out in order to help identify potential issues with sustainability of the intervention. Participation was considered as implied consent. An experienced interviewer, after providing participants with information sheets outlining the purpose of the study, conducted semi-structured interviews using a standardized list of questions. Domains of inquiry included impact on workload, perceived impact on patient care and barriers and facilitators to use. Responses were transcribed from audio recordings and merged with the notes taken in situ. No personal identifying data was collected. Two investigators independently analyzed the data using a content analysis approach. Common themes were identified, agreed upon and categorized. This study received ethical approval from the University of Calgary Conjoint Health Research Ethics Board.
4. Results
During the 12 weeks of study, the electronic order set was ordered a total of 68 times between the 6 units (►Fig. 2). The estimated mean rate of order set use over a 2 week period was 3.1 (95% CI 1.9–5.3) sets higher after the intervention was implemented than before, after adjusting for patient number and unit. Post hoc usage measurement revealed that the order set has been ordered 246 times during the 11 months since it was first made available on the electronic medical record of the three hospitals in Calgary.
Figure 2.
Number of order sets ordered and fall occurrence by time period and intervention phase in stepped wedge design
The estimated odds of a fall happening on a unit over a 2-week period was 9.3 times higher before than after the intervention was implemented (95% CI 0.9–100; p = 0.065), after adjusting for patient number. There was no significant effect of the intervention on the average length of hospital stay on the units (Median before = 42days vs. after = 45days; p = 0.67) or consults to related clinical services (total consults before = 278; total consults after 262; all p <0.2).
Seven unit nurses and six nurse managers/educators were interviewed. Most felt the order set was good basic nursing care and therefore many unit nurses were not ordering it but thought it could be a useful resource for new nurses. The perceived main barrier to the use of the order set was the high workload on these busy medical units and that there was a need for more staff or volunteer support to help in the care of older inpatients. Many of those interviewed reported that the order set was too wordy and contained long paragraphs. Both unit nurses and nurse managers/educators were unfamiliar with the geriatric resource binder and reported that is was not being used. Several nurse managers/educators felt Internet resources would more likely be used. The three interviewed unit nurses who attended the brief educational in-servicing felt the information provided was good basic nursing care. Among the four interviewed nurse managers/educators whom attended the in-servicing, two felt the information could be included in the future unit nurse teaching.
5. Discussion
We conducted a pragmatic trial evaluating a multi-component intervention that incorporated a clinical decision support tool (electronic order set) targeted for use by the nurses providing care to older medical inpatients within acute care hospitals. Not surprisingly the rate of use of the order set was higher after the intervention was rolled out (i.e. in-serviced) on a unit. Order set usage continued within the three Calgary-area hospitals over the eight months following the roll out on the six intervention units, suggesting modestly successful dissemination and implementation.
Issues around engagement of front line nurses included high workloads on busy medical units and a perception that the order set was already part of good basic nursing care. Although not measured, organizational issues and generational differences among the nursing staff may have had some influence as well [32, 33].
Although not statistically significant, we saw a reduction in the number of falls as a result of the intervention. This encourages us to continue to adapt this KT intervention to help overcome the identified barriers to its use. We could not demonstrate any reduction in the length of hospital stay, although we know that multiple extraneous factors could be impacting this indicator (e.g. acute medical issues; time to complete investigations; availability of sub-acute and long term care beds). There was no impact on the use of physiotherapy and geriatric services. We expected that consults to these services might have increased due to the increased attention to mobility and other geriatric related issues. We were unable to measure changes in delirium rates as this information is not contained within the electronic medical record.
Successful knowledge translation strategies utilize an iterative approach, viewing the process as a cycle[24]. This may involve modification of the intervention post-implementation, based on assessment of barriers and facilitators. It also requires ongoing engagement of the end users. Currently the geriatric in-patient consultation services within the local acute care hospitals have taken to using the order set as part of their suggested care plan for many of the patients they consult on, increasing the exposure of other units to the order set and helping to facilitate its spread. Other local initiatives that may impact future KT strategies include plans to expand the current medical record, which is currently a mixed electronic and paper record, to include electronic clinical nursing documentation. This may provide the opportunity to refocus the intervention away from an order set into a more broadly applied care pathway.
One of the limitations to this study was the fact that we were unable to randomize the units in terms of the timing of the rollout. Therefore we are unable to entirely exclude the possibility that units who received information about the order set early on were also more likely to take up the intervention. However, we suspect this was not the case based on the rates of order set use on the various units over time. Another limitation was the relatively small number of units studied and the study duration, which could have impacted the number of outcome events recorded.
Potential limitations with the qualitative interviews included the fact that the nurse managers on two of the six units declined interviews. Additionally, the research associate conducted the interviews on the units at times that were selected by the nurse managers/educators. However, analysis of the interviews revealed common recurring themes and the responses from the front line nurse differed from those of the unit managers/educators, suggesting that selection bias was unlikely a factor. Additionally, for pragmatic reasons we were limited in the number of nurses available for interviews. However, we feel that despite this limitation we reached saturation of potential themes.
Clinical decision support may be yet another strategy to incorporate into multi-component prevention and management approaches aimed at addressing common geriatric issues (e.g. falls; delirium; incontinence), given the documented improvement clinical decision support has had on adherence to care processes [21–23, 34, 35]. However, such strategies require further study given that earlier trials have not always demonstrated a clear benefit to clinical decision support in the care of older adults, have focused primarily on physician responses, and have not consistently demonstrated improved patient outcomes [21–23, 36].
6. Conclusions
Translation of evidence based strategies into the every day care of older hospitalized patients through the use clinical decision support showed mixed results, with a promising although not significant statistically decline in the rate of falls. Frontline user engagement is crucial for the successful implementation and sustainability of such clinical decision support tools.
7. Clinical Relevance
This Knowledge Translation intervention targeted front line nurses and their care of older medical inpatients to prevent common and sometimes catastrophic adverse events such as falls, delirium, and declining function while in hospital. We learned a few lessons around the barriers to implementing this tool, therefore in the next cycle we will focus on the rewording of the order set, on better targeting end-users, and on appropriate placement of the tool within the electronic medical record. We will also explore automatic promoting of the user to use the decision support tool in an effort to improve performance [21].
Conflicts of Interest
The authors declare that they have no conflicts of interest in the research.
Human Subjects
This study received ethical approval from the University of Calgary Conjoint Health Research Ethics Board. Given data was collected at the unit level and included no individual identifying data, and the fact that the intervention was considered usual best evidence clinical care the Ethics Board waived the need to obtain individual patient consent.
Acknowledgements
The authors would like to acknowledge the contributions of Mollie Cole, Margaret Wylie, Dr. Karen Fruetel, Virginia Meyer, Kelly McDonald and Jane Bankes in helping to develop the order set and resource binder, and the Alberta Health Services PCIS Order Set team for helping build the electronic version of the order set. The educational in-servicing was conducted by Rishma Jessa and Kelly McDonald. We also thank the Alberta Health Services Survey & Evaluation Services, Data Integration, Measurement & Reporting for helping conduct and transcribe the interviews. Additionally, the authors appreciate the support of the nurse managers, educators and front line nursing staff on the medical units that participated in the project.
References
- 1.Rothschild JM, Bates DW, Leape LL. Preventable medical injuries in older patients. Arch Intern Med 2000; 160(18): 2717–2728 [DOI] [PubMed] [Google Scholar]
- 2.Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 2003; 51(4): 451–458 [DOI] [PubMed] [Google Scholar]
- 3.Inouye SK, Bogardus ST, Jr., Charpentier PA, Leo-Summers L, Acampora D, Holford TR, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999; 340(9): 669–676 [DOI] [PubMed] [Google Scholar]
- 4.Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA 1996; 275(11): 852–857 [PubMed] [Google Scholar]
- 5.Schmid N. Federal Nursing Service Award Winner. Reducing patient falls: a research-based comprehensive fall prevention program. Mil Med 1990; 155: 202–207 [PubMed] [Google Scholar]
- 6.Brown JP, Josse RG. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 2002; 167(10 Suppl): S1-S34. [PMC free article] [PubMed] [Google Scholar]
- 7.Gates S, Fisher JD, Cooke MW, Carter YH, Lamb SE. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. BMJ 2008; 336(7636): 130–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ 2004; 328(7441): 680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2009(2): CD007146. [DOI] [PubMed] [Google Scholar]
- 10.Inouye SK. Delirium after hip fracture: to be or not to be? J Am Geriatr Soc 2001; 49(5): 678–679 [DOI] [PubMed] [Google Scholar]
- 11.Williams-Russo P, Urquhart BL, Sharrock NE, Charlson ME. Post-operative delirium: predictors and prognosis in elderly orthopedic patients. J Am Geriatr Soc 1992; 40(8): 759–767 [DOI] [PubMed] [Google Scholar]
- 12.Francis J, Kapoor WN. Prognosis after hospital discharge of older medical patients with delirium. J Am Geriatr Soc 1992; 40(6): 601–606 [DOI] [PubMed] [Google Scholar]
- 13.Gustafson Y, Berggren D, Brannstrom B, Bucht G, Norberg A, Hansson LI.et al. Acute confusional states in elderly patients treated for femoral neck fracture. J Am Geriatr Soc 1988; 36(6): 525–530 [DOI] [PubMed] [Google Scholar]
- 14.Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med 1998; 13(4): 234–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Keeffe S, Lavan J. The prognostic significance of delirium in older hospital patients. J Am Geriatr Soc 1997; 45(2): 174–178 [DOI] [PubMed] [Google Scholar]
- 16.Holroyd-Leduc JM, Khandwala F, Sink KM. How can delirium best be prevented and managed in older patients in hospital? CMAJ 2010; 182(5): 465–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990; 113(12): 941–948 [DOI] [PubMed] [Google Scholar]
- 18.Thom D. Variation in estimates of urinary incontinence prevalence in the community: effects of differences in definition, population characteristics, and study type. J Am Geriatr Soc 1998; 46(4): 473–480 [DOI] [PubMed] [Google Scholar]
- 19.Holroyd-Leduc JM, Tannenbaum C, Thorpe KE, Straus SE. What type of urinary incontinence does this woman have? JAMA 2008; 299(12): 1446–1456 [DOI] [PubMed] [Google Scholar]
- 20.Holroyd-Leduc JM, Straus SE. Management of urinary incontinence in women: scientific review. JAMA 2004; 291(8): 986–995 [DOI] [PubMed] [Google Scholar]
- 21.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA 2005; 293(10): 1223–1238 [DOI] [PubMed] [Google Scholar]
- 22.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 2005; 330(7494): 765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shojania KG, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev 2009(3): CD001096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof 2006; 26(1): 13–24 [DOI] [PubMed] [Google Scholar]
- 25.Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007; 334(7591): 455–459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forsetlund L, Bjorndal A, Rashidian A, Jamtvedt G, O’Brien MA, Wolf F, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2009(2): CD003030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown CA, Lilford RJ. The stepped wedge trial design: a systematic review. BMC Med Res Methodol 2006; 6: 54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc 2001; 49(5): 516–522 [DOI] [PubMed] [Google Scholar]
- 29.Lundstrom M, Olofsson B, Stenvall M, Karlsson S, Nyberg L, Englund U, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res 2007; 19(3): 178–186 [DOI] [PubMed] [Google Scholar]
- 30.Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 1994; 331(13): 821–827 [DOI] [PubMed] [Google Scholar]
- 31.Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemp Clin Trials. 2007; 28(2): 182–191 Epub 2006 Jul 7 [DOI] [PubMed] [Google Scholar]
- 32.Kramer LW. Generational diversity. Dimens Crit Care Nurs 2010; 29(3): 125–128 [DOI] [PubMed] [Google Scholar]
- 33.Richardson A, Storr J. Patient safety: a literature [corrected] review on the impact of nursing empowerment, leadership and collaboration. Int Nurs Rev 2010; 57(1): 12–21 [DOI] [PubMed] [Google Scholar]
- 34.Shojania KG, Jennings A, Mayhew A, Ramsay C, Eccles M, Grimshaw J. Effect of point-of-care computer reminders on physician behaviour: a systematic review. CMAJ 2010; 182(5): E216-E225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Durieux P, Trinquart L, Colombet I, Nies J, Walton R, Rajeswaran A, et al. Computerized advice on drug dosage to improve prescribing practice. Cochrane Database Syst Rev 2008(3): CD002894 . [DOI] [PubMed] [Google Scholar]
- 36.Gurwitz JH, Field TS, Rochon P, Judge J, Harrold LR, Bell CM, et al. Effect of computerized provider order entry with clinical decision support on adverse drug events in the long-term care setting. J Am Geriatr Soc 2008; 56(12): 2225–2233 [DOI] [PubMed] [Google Scholar]