Abstract
Background
This paper reports on work carried out to elicit information needs at a trans-disciplinary, nurse-managed health care clinic that serves a medically disadvantaged urban population. The trans-disciplinary model provides a “one-stop shop” for patients who can receive a wide range of services beyond traditional primary care. However, this model of health care presents knowledge sharing challenges because little is known about how data collected from the non-traditional services can be integrated into the traditional electronic medical record (EMR) and shared with other care providers. There is also little known about how health information technology (HIT) can be used to support the workflow in such a practice.
Objectives
The objective of this case study was to identify the information needs of care providers in order to inform the design of HIT to support knowledge sharing and distributed decision making.
Methods
A participatory design approach is presented as a successful technique to specify requirements for HIT applications that can support a trans-disciplinary model of care.
Results
Using this design approach, the researchers identified the information needs of care providers working at the clinic and suggested HIT improvements to integrate non-traditional information into the EMR. These modifications allow knowledge sharing among care providers and support better health decisions.
Conclusions
We have identified information needs of care providers as they are relevant to the design of health information systems. As new technology is designed and integrated into various workflows it is clear that understanding information needs is crucial to acceptance of that technology.
Keywords: Information needs, participatory design, requirements analysis and design, clinical information technology, nursing workflow, provider-provider communications
1. Introduction
Adoption of electronic medical records (EMRs) in ambulatory medical practices has lagged behind that of hospitals, and diffusion to non-traditional practices has been even slower [1–3]. Often these systems are poorly automated [4–5] and introduce unanticipated workflow issues [6–7]. Few settings experience this frustration more keenly than clinics that operate using a care delivery model that differs from the “normal” physician-centered, medical model initially designed to support inpatient care in a medical center or hospital [8–9]. While these non-traditional practices often attend to the behavioral, emotional, and spiritual aspects of the patients’ health as well as to the patients’ clinical needs, knowledge sharing among the care providers can be challenging. The traditional EMR makes capturing data that do not conform to a standard clinical model difficult because the data are usually not associated with measureable values or are captured as part of the history and/or physical exam. Because the majority of the research on the impact of EMRs has been done on systems in large hospital (primarily public and academic) settings [10], there is a danger in trying to compare these large settings with smaller clinics and practices [11], each of which has distinct cultures. However, data show that a well designed EMR can contribute significantly to decreased complications [12], improving quality [13], and improving efficiency [14].
This article presents the results from a participatory design project using the i* framework. The purpose of the project was to elicit system requirements for a customized EMR that captures inputs from multiple different types of activities, integrates them, and allows them to “talk to each other” so that all the care providers can share the same patient information. The results of the project suggest that the use of appropriate HIT applications can facilitate knowledge sharing among care providers and support better health decisions.
1.1 Trans-disciplinary care
The term “trans-disciplinary care” has recently been coined to refer to providers from different specialties working jointly using a shared conceptual framework that draws together concepts, theories, and approaches from its parent discipline [15–16]. While the term is often used interchangeably with interdisciplinary and multi-disciplinary, trans-disciplinary settings differ because they create new frameworks that often break down traditional barriers [17]. This holistic approach to ambulatory care lends itself well to delivery by nurse practitioners and other allied health practitioners. The healthcare team may include nurses, social workers, psychologists, dietitians, and physical therapists; the care rendered can also include pre- and post-natal care, dental services, as well as a variety of classes and activities, in addition to primary care services. Although the holistic approach to providing health care offers significant advantages to the patient, it also presents significant challenges to the use of a traditional EMR, since data about an individual patient may come from multiple care providers and often in multiple formats.
When working within the trans-disciplinary model of care, a basic re-orientation to data and information is needed. Because all care is integrated into a “one-stop shop” model, data about the patient should not have to come from multiple record systems; ideally, one record per patient should receive input from all care providers. This “unit record” should reflect the full spectrum of care that the patient receives, and all care providers should have access to it (except for data that are protected such as HIV/AIDS status, psychotherapy notes, and the like). In addition, data on an individual patient should include records of attendance at “healthy living” classes such as yoga, nutrition, and exercise that are offered at the clinic as part of their trans-disciplinary care. Another characteristic of the data and information used in the trans-disciplinary model is that all care providers should co-orient around the same record, adding and retrieving data based on their view of the patient. The ideal unit record should also enable a care coordinator to make referrals to other clinic services, and to follow up to determine if the patient has interacted with that service.
1.2 Information needs and knowledge sharing
While early studies of clinical information needs focused on physicians either working alone or in teams [18–19], more recent studies have found that nurses’ information needs differ from those of physicians [20–21]. Nursing responsibilities in healthcare organizations run the gamut from educating patients to medication administration to executing physician orders and ensuring safety [21]. Nurses are often required to manage and balance relationships with multiple individuals usually distributed by time and space.
In the trans-disciplinary care model, nurses’ information needs are complicated by the fact that data about an individual patient are coming from multiple sources and in multiple formats. Using HIT to aggregate all of these disparate data can help to support nurse decision making [22]. In fact, the use of HIT by nursing practices has become even more important as EMR implementations have struggled [23–24]. Furthermore, previous studies have found that nurses tend to be more receptive to technological interventions than other clinicians [25–26].
Knowledge sharing among nurses about individual patients has traditionally been accomplished through face-to-face communication or through written notes on a patient’s chart. Nurses have developed methods for ensuring that critical information is communicated during transitions of care [27]. Although the trans-disciplinary model involves a complex flow of information, demonstrated by the numerous interactions and dependencies between and among workers, knowledge management practices have not generally been well integrated into such clinical organizational processes [28]. However, sharing knowledge among the healthcare team about individual patients is essential in the trans-disciplinary model if appropriate interventions are to be administered.
1.3 Participatory Design
It has been generally acknowledged that an “early-phase” requirements analysis in the system development life cycle is crucial to successful development and deployment of any software system [33–35]. Having key stakeholders play an integral role in the development of information systems is an essential component of participatory design [29] and typically requires repeated interactions between the designers and the stakeholders. This process of iterative design has been demonstrated to lead to more successful implementations in a variety of information technology settings [30]. Increasingly, participatory design is becoming more prevalent in the development of health IT system design [31–32].
In the early stages of the analysis process, the emphasis is on understanding the “whys” that underlie system requirements, rather than on the precise and detailed specification of “what” the system should do [36]. Traditional requirements engineering usually begins with a set of statements expressing stakeholders’ wishes about what the system should do [37]. Software designers and engineers then apply a set of techniques to refine these often incomplete, inconsistent, and ambiguous statements.
The i* framework [38–39] was developed for analyzing early requirements by modeling and reasoning about the socio-technical environments in an organization. The framework consists of two main modeling components: the Strategic Dependency (SD) model and the Strategic Rationale (SR) model. The Strategic Dependency (SD) model is used to describe the dependency relationships among various actors in an organizational context. The SR model is used to describe stakeholder interests and concerns, and how they might be addressed by various configurations of systems and environments. In the SD model, actors are related to each other through intentional dependencies. In the SR model, a single actor is examined in more detail in terms of achieving their goals. A typical i* analysis uses primarily graphical representations that help non-technical stakeholders to express their intentions. Instead of using technical flowcharts, the i* model uses lines and circles to show dependencies and relationships.
While system analysts and designers usually focus on information content and processes that are to be embedded in automated systems, it is becoming increasingly important to analyze and model the social context and surrounding environment of systems such as the organizational culture. Capturing the social context and surrounding environment in system design process and modeling [it] enhances the system’s ability to adapt to the needs of stakeholders. In this paper, we argue that the i* method of requirements analysis is particularly suited to the trans-disciplinary model of care since understanding information needs of the interdependent care providers is difficult to capture using traditional task analysis techniques.
2. Methods
2.1 Setting
The setting for the study was a nurse-managed, primary care clinic that coordinates patient services from a variety of health care professionals and delivers patient-centered care to a predominantly medically disadvantaged population in Philadelphia. The clinic has been cited nationally for its trans-disciplinary approach to primary care, in which a variety of services aimed at encouraging healthy lifestyles is part of every care plan. The healthcare team includes nurses, social workers, psychologists, dietitians, and physical therapists. To understand the information needs of care providers at the trans-disciplinary clinic and model their social context and surrounding environment, we conducted a comprehensive analysis of their requirements focused on the strategic relationships and essential information shared among the 26 staff members responsible for the healthy living programs and primary care. Seven staff members, representing each specialty in the clinic, participated in the design process. These included the director of the center, three nurses, two behavioral health clinicians, and the wellness coordinator. The healthy living programs were the target of this analysis process because, the data from these non-traditional services are not currently tracked in an electronic form that is accessible within the existing EMR.
The existing EMR describes the patient as a collection of numbers, including lab results and physiological measures such as blood pressure. This collection of facts and figures does not adequately describe the patient as viewed by many of the trans-disciplinary team members. Moreover, the existing EMR does not support effective information integration and knowledge sharing. For example, information from team members responsible for the healthy living programs and facilities is usually scanned into the existing EMR system as an image without data that can be digitally manipulated. The scanned documents are not easily accessible to the team members and cannot be shared among them through a single unit record.
2.2 Analysis Process
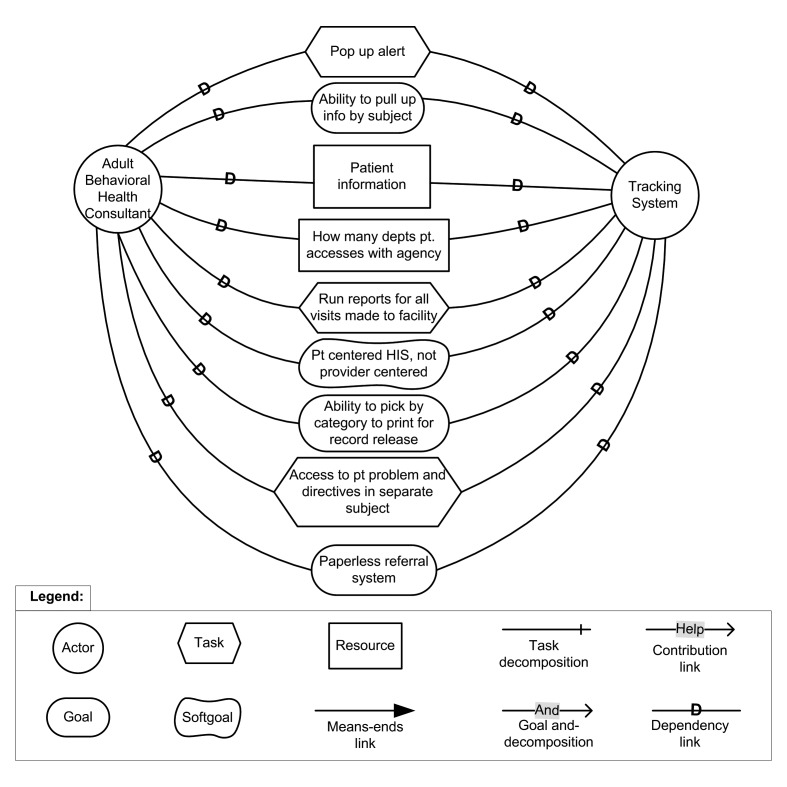
The i* star analysis was implemented at the site beginning with a series of three group sessions during which the clinic staff were given a set of simple tools to generate preliminary SD and SR diagrams. Each of the sessions lasted approximately two hours. After an explanation of the i* framework and the graphical techniques, the seven clinical staff members, who represented or were responsible for the healthy living programs, were asked to represent their tasks, the individuals with whom they interact to accomplish those tasks, and the information or data needed to accomplish the tasks. Over a series of sessions, the staff individually de-composed and articulated their goals, objectives, and tasks using basic representations such as lines and arrows captured on large sheets of paper. The sheets were then collected from the individuals and analyzed by the research team. As an example, ►figure 1 is what was presented back to the adult behavioral health consultant. After each team member documented the relationships, the figure was analyzed by the research team and presented back to them in a formal way. With each cycle, the research team and the stakeholders came closer to identifying commonly-held models (both SD and SR) specifying the tasks and the dependency relationships needed to accomplish an objective in the service of the overall goal – in this case, improved patient care.
Fig. 1.
Example diagram for the behavioral health staff member
The final result was a representation showing the consensus understand of the goals, objectives, and tasks.
3. Results
3.1 Summary of overall findings
Our requirements analysis verified that the existing EMR lacked the capacity to collect and report the full range of data available from the trans-disciplinary programs and to integrate them with traditional lab results and physiological measures. Furthermore, the analysis elucidated places in the current workflow where members of the healthcare team would like to have these healthy living data available from a single, integrated source to support decisions about further treatment programs. The requirements analysis substantiated and documented the need for an enhanced EMR that captures not only the medical facts about a patient but also the behavioral, emotional, and spiritual factors that influence physical health and disease. In addition, the requirements analysis demonstrated the key points where knowledge sharing and distributed decision making could be supported through HIT improvements.
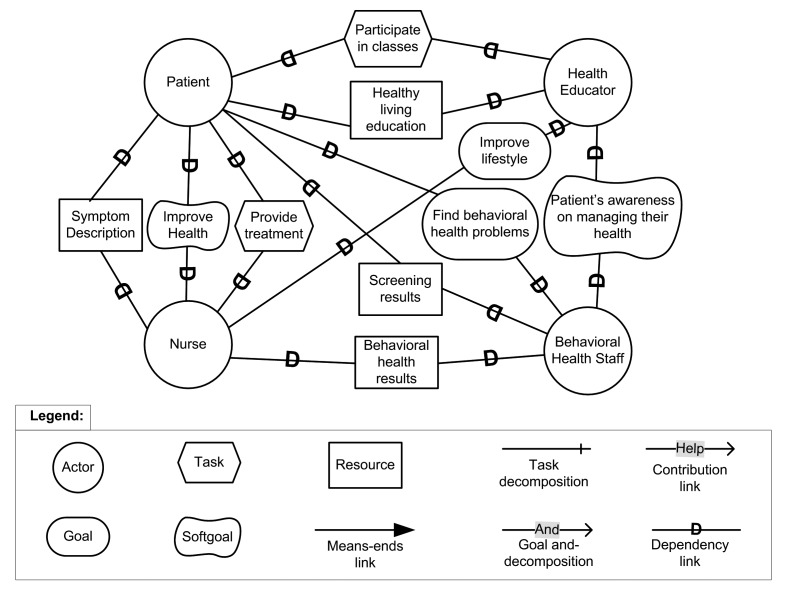
►Figure 2 is an example of a SD diagram generated for the collection of behavioral health data. The diagram also describes many other dependency relationships among the patient, health education coordinator, behavioral health specialist, and nurse practitioner. These diagrams were constructed for each key staff member involved in the processes.
Fig. 2.
A Strategic Dependency (SD) diagram.
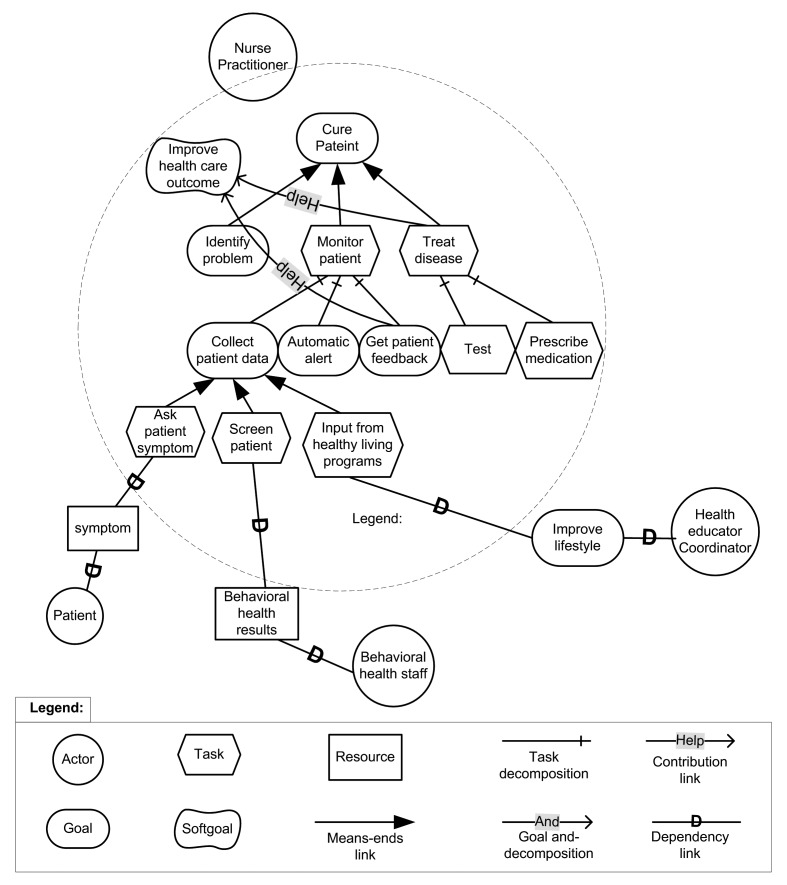
►Figure 3 shows an example of a SR diagram of the rationale of a nurse practitioner at the health center. In this example, the goal of the nurse is to care for the patient; the goal can be met by identifying the problems, treating the diseases, and monitoring the patient. The task of monitoring patients is decomposed into three sub-goals: collecting patient data, sending automatic alerts, and obtaining patient feedback. To collect patient data, three sub-tasks have been identified: asking the patient for symptoms, screening the patient, and obtaining input from the healthy living programs. Similar SR diagrams were made for each clinical staff position.
Fig. 3.
A Strategic Rationale (SR) diagram.
3.2 Process impacts
Absent the use the i* model to identify information needs associated with behavioral health programs, the complex interactions and dependencies between and among care providers would not have been as apparent. As a result of the requirements analysis, the research team was able to develop a customized module for the existing EMR that responds to these information needs and associates them with health outcomes. The patient wellness tracker (PWT) module captures inputs from multiple different types of activities, integrates them, and allows them to “talk to each other” so that all the care providers can share the information. Only with such an integrated EMR is it possible to track the relationships between and among the various types of services offered by the trans-disciplinary care model.
3.3 Outcomes
Ongoing testing of the PWT module suggests that appropriate HIT applications based on participatory design using an appropriate requirements analysis tool such as the i* framework can facilitate knowledge sharing among care providers and support better health decisions. For example, data collected in the PWT can track the number of patients completing quality of life surveys and associate those values with health outcomes (e.g. weight, blood pressure). The PWT captures data from a range of sources identified as being important to the care providers. These data can then be integrated with data from the existing EMR to describe a more complete picture of the patient than was available before implementation of the PWT. This more complete picture is the result of improved knowledge sharing among the care providers.
3.4 Results unique to the i* process
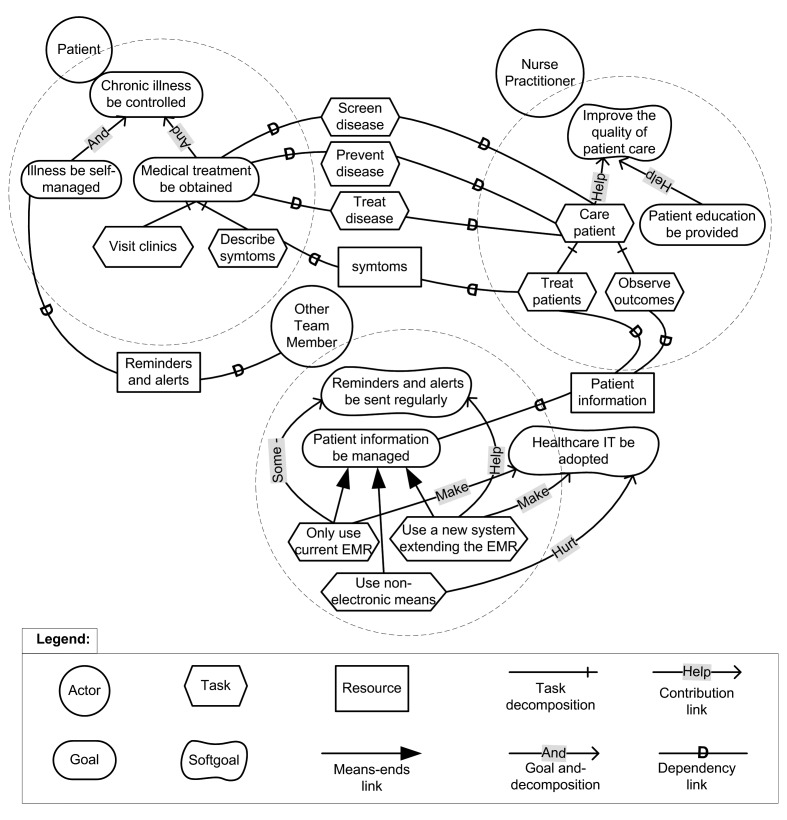
The tasks, dependencies, and relationships represented in the SD and SR diagrams reflect knowledge of specific content (e.g. what is a HbA1c value that is out of range?) as well as activity patterns (e.g. the clinic has to receive lab results before follow-up visit), and situational realities (e.g. patients may use “borrowed” insurance cards) that affect workflow and HIT system design. However, much of this knowledge is experiential or tacit. Tacit knowledge is notoriously difficult to elicit. One value of the i* framework is its recognition of the social context and environmental surroundings in which the HIT system operates (►Figure 4). The impacts of the social context is enumerated and documented on the figure. The fact that the i* model is able to elicit tacit knowledge from the stakeholders makes it possible for them to develop a better understanding of the resources available within the organization that can support better clinical decision making.
Fig. 4.
Representation of social context and environment.
4. Discussion and implications for future research
4.1 Health IT intervention
Our preliminary work suggests that the i* framework can be a successful technique to capture the information needs of care providers who work within a trans-disciplinary care model. The SD and SR diagrams can be refined until an actual design for templates emerges through which to capture the full array of care data. Following the conclusion of participatory design process, the SD and SR diagrams were used to direct the initial planning and programming of the PWT. Specifically, these models were used to develop the UML class diagrams to describe the software models. This then directed the software development. As healthcare continues to be transformed to a more patient-centric model, there is a critical need to make progress in identifying the information needs of care providers in non-traditional settings and to understand how appropriate HIT applications can integrate trans-disciplinary information more successfully. We believe that without a requirements analysis process such as the i* model, which captures tacit as well as explicit knowledge, the resulting PWT design would have been less successful.
4.2 Strengths and weaknesses of the health IT intervention
The strength of the i* model lies in the fact that it engages the key stakeholders in the requirements analysis process and builds both understanding and consensus around the process and the information needs involved in it. However, one weakness of the approach is that it is time-consuming and requires a slight learning curve for meaningful involvement. In a clinical setting such as the trans-disciplinary health center, care provider time is at a premium, and the investment in the requirements analysis can meet with resistance. However, for those care providers who made the investment in the process, the reward was increased clarity about information needs to support clinical decisions.
4.3 Significance and generalizability of the intervention
The i* model is an appropriate technique that can be used to identify system requirement in a wide range of settings. The specific significance of this study lies in its application of the i* model to a trans-disciplinary setting. The information needs of care providers in this type of setting are complex because of the multiple sources from which data are drawn and the multiple formats in which the data are presented. Creating a system that shares these disparate data effectively across the various disciplines is very challenging. Use of a participatory technique such as the i* model provides a structured approach for identifying these information needs. Although time consuming, the investment in the analysis process can yield significant results.
For a process such as the i* model to be effective, support must come for the top administrators of the organization. Most change literature points to the involvement and support of leadership as being essential to encouraging full participation of staff members. In addition, the participatory design technique has demonstrated success in encouraging users to participate and building support for systems as users are involved in the design. In this study, participation of the director of the center sent a strong message to others on the staff about the value of devoting time to the process. Without leadership support, knowledge management efforts often fail due to inadequate commitment to the process, both during the development and the implementation phases.
4.3.1 Future work
The research team is evaluating the potential of new graphic interfaces for the PWT data that will make integrating traditional clinical measures with behavioral measures more transparent to the care givers and ultimately to the patients. By sharing a fuller range of lab results and physiological measures among the various care providers, the new interface will allow for more distributed decisions about further treatment programs.
4.3.2 Extension to other workflows or situations
The i* model can be implemented as part of the requirements gathering process in a number of settings, in particular those where a complex workflow can be supported by HIT. For example, there is an increased interest in supporting the handoffs or transitions in care process with HIT. Handoffs between clinicians usually involve balancing competing goals and depend on the changing state of patients and care providers. Developing any HIT for this environment would be complicated by the fact that the process of handoffs can occur across several locations, timeframes, and individuals. The i* model captures dependencies and stakeholder interests so it would identify the competing goals and conflicts underlying the handoff process. Identifying the information needs of care providers will be crucial if the HIT is to support knowledge sharing and decision making among clinicians.
5. Conclusion
We have identified information needs of care providers as they are relevant to the design of health information systems. As new technology is designed and integrated into various workflows it is clear that understanding information needs is crucial to acceptance of that technology. Participatory design techniques and other requirement gathering have been demonstrated to be useful in understanding the needs of clinicians. In particular, the i* framework is proposed as a specific technique that is useful to capture underlying dependencies in the workflow of clinicians that must be supported by the technology. Presenting these findings to developers and clinicians who are responsible for selecting information tools to support clinical documentation is key in the development and procurement process.
Clinical Relevance Statement
The information needs of care givers documented in this report should be taken into consideration during the design process. Participatory design techniques take into account the various needs of key stakeholders. An awareness of these needs and methods to capture them provide support and direction to software designers and the clinicians that are making purchasing decisions.
Competing Interest
The authors do not declare any conflicts of interest.
Human Subject Research
The study was reviewed by the Drexel University Institutional Review Board.
Acknowledgments
This study was made possible by support from the exceptional staff of the 11th Street Family Health Center of Drexel University, led by Dr. Patricia Gerrity.
References
- 1.Bates DW. Physicians and ambulatory electronic health records. Health Affairs 2005; 24(5): 1180–1189 [DOI] [PubMed] [Google Scholar]
- 2.Berger RG, Kichak JP. Computerized physician order entry: Helpful or harmful? Journal of the American Medical Informatics Association 2004; 11: 100–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yarbrough AK, Smith TB. Technology acceptance among physicians. Medical Care Research and Review 2007; 64: 650–672 [DOI] [PubMed] [Google Scholar]
- 4.Karsh B-T. Beyond usability: designing effective technology implementation systems to promote patient safety. Quality & safety in health care 2004; 13(5): 388–394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan W.Increasing the success of physician order entry through human factors engineering. Journal of Heathcare Information Management 2002; 16(1): 71–79 [PubMed] [Google Scholar]
- 6.Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care – an interactive sociotechnical analysis. Journal of the American Medical Informatics Association 2007; 14(5): 542–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bates DW. Using information technology to reduce rates of medication errors in hospitals. BMJ 2000; 320: 788–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cogdill KW, et al. Information needs and information seeking in community medical education. Academic Medicine 2000; 75(5): 484–486 [DOI] [PubMed] [Google Scholar]
- 9.Wong FKY, Chung LCY. Establishing a definition for a nurse-led clinic: structure, process and outcome. Journal of Advanced Nursing 2006; 53(3): 358–369 [DOI] [PubMed] [Google Scholar]
- 10.Ash JS, et al. Categorizing the unintended sociotechnical consequences of computerized provider order entry. International Journal of Medical Informatics 2007; 76(Suppl. 1): S21–S27 [DOI] [PubMed] [Google Scholar]
- 11.Jerant AF, Hill DB. Does the use of electronic medical records improve surrogate patient outcomes in outpatient settings? The Journal of Family Practice 2000; 49(4): 349–357 [PubMed] [Google Scholar]
- 12.Amarasingham R, et al. Clinical information technologies and inpatient outcomes: a multiple hospital study. Arch Intern Med 2009; 169(2): 108–114 [DOI] [PubMed] [Google Scholar]
- 13.Chaudhry B, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006; 144: 742–752 [DOI] [PubMed] [Google Scholar]
- 14.Hillestad R, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Affairs 2005; 24: 1103–1117 [DOI] [PubMed] [Google Scholar]
- 15.Rosenfield PL. The potential of transdisciplinary research for sustaining and extending linkages between the health and social sciences. Social Science & Medicine 1992; 35(11): 1343–1357 [DOI] [PubMed] [Google Scholar]
- 16.Grey M, Connolly CA. Coming together, keeping together, working together: Interdisciplinary to transdisciplinary research and nursing. Nursing Outlook 2008; 56(3): 102–107 [DOI] [PubMed] [Google Scholar]
- 17.Mitchell PH. What’s In A Name?: Multidisciplinary, interdisciplinary, and transdisciplinary. Journal of Professional Nursing 2005; 21(6): 332–334 [DOI] [PubMed] [Google Scholar]
- 18.Gorman PN. Information needs of physicians. Journal of the American Society for Information Science 1995; 46(10): 729–736 [Google Scholar]
- 19.Reddy M, Dourish P.A finger on the pulse: Temporal rhythms and information seeking in medical care. In: Proceedings of ACM Conference on Computer Supported Cooperative Work CSCW’02, ACM, New York, 2002: 344–353
- 20.Xu X, et al. Understanding nurses’ information needs and searching behavior in acute care settings. AMIA Annu Symp Proc 2005: 839–843 [PMC free article] [PubMed] [Google Scholar]
- 21.Darbyshire P.Rage against the machine? Nurses’ and midwives’ experiences of using computerized patient information systems for clinical information. Journal of Clinical Nursing 2004; 13(1): 17–25 [DOI] [PubMed] [Google Scholar]
- 22.Randell R, et al. Supporting nurse decision making in primary care: Exploring use of and attitude to decision tools. Health Informatics Journal 2009; 15(1): 5 [DOI] [PubMed] [Google Scholar]
- 23.Poissant L, et al. The impact of electronic health records on time efficiency of physicians and nurses: A systematic review. Journal of the American Medical Informatics Association 2005; 12(5): 505–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee T.Nursing information: users’ experiences of a system in Taiwan one year after its implementation. Journal of Clinical Nursing 2008; 17(6): 763–771 [Google Scholar]
- 25.Ziegler J.Inching toward and info technology revolution. Business and Health 1999; 17(6): 51–55 10557391 [Google Scholar]
- 26.Gugerty B, Wooldridge P, Brennan M.The CISQ: A tool to measure staff involvement in and attitudes toward the implementation of a clinical information system. In: Proceedings of the American Medical Informatics Association; Los Angeles November 3–7, 2000. [PMC free article] [PubMed]
- 27.Patterson ES, Roth EM, Render ML. Handoffs during nursing shift changes in acute care. Proceedings of the Human Factors and Ergonomics Society 49th Annual Meeting. Santa Monica, CA :Human Factors and Ergonomics Society 2005.
- 28.Orzano AJ, et al. Family medicine practice performance and knowledge management. Health Care Management Review 2008; 33(1): 21 [DOI] [PubMed] [Google Scholar]
- 29.Irestig M, Eriksson H, Timpka T.The impact of participation in information system design: A comparison of contextual placements. Proceedings of the Eighth Conference on Participatory Design: Artful Integration: Interweaving Media, Materials and Practices, NewYork: ACM Press,. 2004: 102–111
- 30.Shneiderman B.Designing the user interface: Strategies for effective human-computer interaction. 3rd edn.Reading, MA:Addison-Wesley; 1998. [Google Scholar]
- 31.Sjoberg C, Timpka T.Participatory design of information systems in health care. Journal of the American Medical Informatics Association 1998; 5(2): 177–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weng C, et al. Participatory design of a collaborative clinical trial protocol writing system. International Journal of Medical Informatics 2007; 76(Suppl. 1): S245–S251 [DOI] [PubMed] [Google Scholar]
- 33.van Lamsweerde A.Goal-oriented requirements engineering: A guided tour. In: Proceedings of 5th IEEE International Symposium on Requirements Engineering, 2001.
- 34.Liu L, Yu E.Designing information systems in social context: A goal and scenario modelling approach. Information Systems 2004; 29(2): 187–203 [Google Scholar]
- 35.Elahi G, Yu E.A goal oriented approach for modeling and analyzing security trade-offs. Proc. 26th International Conference on Conceptual Modeling 2007: 375–390
- 36.Pfleeger SL, Atlee J.Software engineering: Theory and practice. New York: Pearson Prentice Hall., 2005. [Google Scholar]
- 37.Jackson M.The meaning of requirements. Annals of Software Engineering 1997; 3: 5–21 [Google Scholar]
- 38.Yu ESK, Liu L.Modelling trust for system design using the i* strategic actors framework. In the Proceedings of the workshop on Deception, Fraud, and Trust in Agent Societies held during the Autonomous Agents Conference: 2001: 175–194
- 39.An Y, et al. Collaborative social modeling for designing a patient wellness tracking system in a nurse-managed health care center. In the Proceedings of 4th International Conference on Design Science Research in Information Systems and Technology (DESRIST’09), 2009.