Abstract
Objective
Computerized provider/physician order entry (CPOE) with clinical decision support (CDS) is designed to improve patient safety. However, a number of unintended consequences which include duplicate ordering have been reported. The objective of this time-series study was to characterize duplicate orders and devise strategies to minimize them.
Methods
Time series design with systematic weekly sampling for 84 weeks. Each week we queried the CPOE database, downloaded all active orders onto a spreadsheet, and highlighted duplicate orders. We noted the following details for each duplicate order: time, order details (e.g. drug, dose, route and frequency), ordering prescriber, including position and role, and whether the orders originated from a single order or from an order set (and the name of the order set). This analysis led to a number of interventions, including changes in: order sets, workflow, prescriber training, pharmacy procedures, and duplicate alerts.
Results
Duplicates were more likely to originate from different prescribers than from same prescribers; and from order sets than from single orders. After interventions, there was an 84.8% decrease in the duplication rate from weeks 1 to 84 and a 94.6% decrease from the highest (1) to the lowest week (75). Currently, we have negligible duplicate orders.
Conclusions
Duplicate orders can be a significant unintended consequence of CPOE. By analyzing these orders, we were able to devise and implement generalizable strategies that significantly reduced them. The incidence of duplicate orders before CPOE implementation is unknown, and our data originate from a weekly snapshot of active orders, which serves as a sample of total active orders. Thus, it should be noted that this methodology likely under-reports duplicate orders.
Keywords: Informatics, documentation, medication errors
1. Background
The benefits of computerized provider/physician order entry (CPOE) are well documented. CPOE, particularly with clinical decision support (CDS), has been shown to increase patient safety [1, 2, 3]. The Institute of Medicine (IOM) supports CPOE as a means to decrease prescriber error and improve safety and quality of care [4]. CPOE has also been reported to improve the utilization of health care services, decrease costs, reduce hospital length of stay, decrease medical errors, and improve compliance with guidelines [1]. CPOE systems improve legibility [5] and decrease errors relating to look-alike, sound-alike medications [6]. Reductions in medication errors have been noted for dosing, frequency, route, substitution, and allergies [7]. Improved prescribing practices with respect to use of proper drugs, dosing and timing have also been documented [8].
However, as with many new technologies, unintended consequences, including some that affect patient safety, may occur [9, 10, 11, 12, 13, 14]. The introduction of new technologies, including CPOE, may be disruptive [15]. The consequences may be anticipated or unanticipated, desirable or undesirable, and direct or indirect [13]. Unintended adverse consequences of CPOE include additional work demands, changes in workflow, infinite need for system changes, paper persistence, changes in communication, negative emotions, generation of new types of errors, changes in power structure and overdependence on technology [12]. The term “e-Iatrogenesis” was coined to describe patient harm caused “by the application of health information technology” [16]. One study describes 22 different categories of medication errors that were facilitated by CPOE [9]. Even in highly computerized hospitals, high rates of adverse drug events were noted after implementation of CPOE, particularly in the absence of CDS [10].
Duplicate orders related to CPOE have been previously noted in the literature. In an early study (1998) of “computer-assisted prescriptions” (CAP) vs. those that were handwritten, Evens et al note 11 duplicate errors in the CAP group vs. none in the “handwritten” group [17]. Koppel et al. [9] described “medication discontinuation failures” whereby physicians can add “new but duplicative medication.” Duplication errors were partly explained by the fact that ordering and discontinuing medications were separate processes. In addition, as many as 20 screens were required to view each patient’s medications, making it intrinsically difficult to spot duplicates. In a review of paper-based ICUs vs. computer-based ICUs, Colpaert et al. noted that although the incidence of intercepted medicine prescription errors were four times lower in the computer based ICUs, most of the errors were related to “double prescriptions” identified by nurses and pharmacists [18].
Ash et al. [14] surveyed 176 CPOE-enabled hospitals and found eight categories of undesirable and unintended consequences, including “overlapping medication orders.” In his review of medication related CDS in CPOE, Kuperman addressed several causes and also made recommendations for “best duplicate therapy checking practices” [19]. Spencer et al. [20] reported a significant increase in voluntary reports of medication errors attributed to CPOE implementation. Duplicate orders accounted for 4% of these errors. In their study comparing two institutions with varying use of CPOE, George and Austin-Bishop noted significant numbers of duplicate orders at both [21]. Fitzhenry et al. studied medication orders and found that significant omissions, delays and “dose shifting” occurred; which led to an increase in duplicate orders. These authors strongly advocated activating duplicate order alerts as a strategy toward reduction [22]. Schedlbauer et al. [23] performed a comprehensive review of the literature for studies on the efficacy of drug alerts and found that 23 of 27 studies demonstrated beneficial effects, although not specifically for duplicate orders. Reckmann et al. also call attention to this in their review of prescribing errors in hospital inpatients [24]. More recently, Wetterneck et al. evaluated duplicate orders before and after implementation of CPOE with CDS. They identified a number of contributing factors, and highlighted multiple “improvement activities” which may reduce them [25].
Duplicate medication orders are an example of a preventable use error with significant effects on patient care. While many papers describe the presence of duplicate orders, this paper describes the nature of these orders and the successful reduction of duplicate orders after implementing CPOE at an academic university affiliated hospital.
2. Objectives
The purpose of this report is to describe the nature of the duplicate orders, report our analysis of them and describe the methods used to reduce them.
3. Methods
We employed techniques described as “action research”, in which participants endeavored to both solve organizational problems in real time, as well as collect data as part of a research process.
3.1 Study Site
The Hospital for Special Surgery is a 205 bed facility in New York City devoted exclusively to the treatment of musculoskeletal and orthopedic conditions. It is affiliated with New York-Presbyterian Hospital and Weill-Cornell Medical College. It has residency and fellowship programs in multiple specialties. The staff includes both full time and consulting physicians, as well as physician assistants (PAs), nurse practitioners (NPs), and nurse anesthetists.
3.2 System characteristics
Our electronic medical record (EMR) went live on July 29, 2007 (Sunrise Clinical Management [SCM], version 4.5 sp 3, Eclipsys, Atlanta, GA [now Allscripts]). It included CPOE, limited documentation (height, weight, and allergies), basic flow sheets, and an electronic medication administration record (e-MAR). We confined duplicate alerts to those medications categorized as “high alert” by the Institute of Safe Medication Practices (ISMP) as well as the drugs most commonly prescribed at our hospital. ISMP notes 22 classes of High Alert drugs (such as antithrombotic and hypoglycemic drugs), as well as 10 other specific drugs such as nitroprusside and potassium chloride for injection (www.ismp.org accessed 6/24/12). Because of their frequent use at HSS, we also included corticosteroids, sedative hypnotics, 2nd generation antihistamines, cardiac medications in the same class, antibiotics in the same class, NSAID’s, PPI’s and H2 blockers and PCA’s (IV-IV and nerve block-nerve block).
3.3 Duplicate Orders: definition and method of quantification
An SQL query of all active orders in the SCM database was performed every Tuesday evening from September 19, 2007 through April 21, 2009, totaling 84 consecutive weeks. These data represent a “snap shot” of all duplicate orders taken at a particular time one day each week (ie a point prevalence study). To illustrate the effect across the 84-week time frame, we partitioned some subsequent analyses into Pre-interventions; the first five weeks of data, and Post-interventions; the final five weeks of data. The data were downloaded into an Excel spreadsheet (®Microsoft), and orders were grouped by patient to identify duplicates. All duplicate medication orders were noted and inspected by a single experienced clinical pharmacist trained in informatics (CP). Non-duplicate entries were manually removed from the spreadsheet after noting the total number of orders entered.
Duplicate medication orders (“duplicates”) were defined for the study as two or more active orders for the identical medication regardless of dose. The second order entered was labeled as the duplicate order. Certain orders were not considered to be duplicates and were excluded from analysis. These include:
-
1.
dose range ordering (e.g. acetaminophen: one pill for mild pain and two pills for severe pain),
-
2.
combination drug plus component (e.g. losartan/HCTZ plus HCTZ or Percocetv® plus acetaminophen,
-
3.
the same drug prescribed for different indications (e.g. acetaminophen for pain and acetaminophen for fever) and
-
4.
large volume parenterals.
The following variables were captured for each order: time of order, order details (e.g. drug, dose, route, and frequency), ordering prescriber, including position and role (e.g. Attending, Fellow, Resident, PA, NP etc), single order or part of an order set (and name of order set). Initial analysis led to a number of interventions devised to reduce the number of duplicate orders. These interventions included changes in order sets to avoid overlapping medications; changes in work-flow; additional training strategies; altering pharmacy procedure; and broadening duplicate warnings. These are described more fully in subsequent sections. All statistical analyses were conducted using SPSS version 17.0 or higher (PASW Statistics, SPSS, 2009) with SAS for verification purposes. Significant differences between percentages were performed through CHI-square or t-test for proportions, as appropriate. Thresholds for statistical significance were set at a minimum of p<0.05.
4. Results
4.1 Duplicate Order Rate
A total of 316,160 orders were captured during the 84 weeks, averaging 3,764 orders per weekly sampling period (range 1,121–5,163). There were 5,442 duplicate orders over this period, an average duplication rate of 1.8%. The highest rate was 5.0% (211/4,220) in week 1, and the lowest rate was 0.3% (8/2,667) in week 75. The duplication rate was 0.82% (32/3,888) in the last week (84) of the study. When the data were analyzed by regression, decline in duplicate orders represented a significantly decreasing linear slope (b = –0.9831, R2 = 0.4625, p<0.01, ►Figure 1).
Fig. 1.
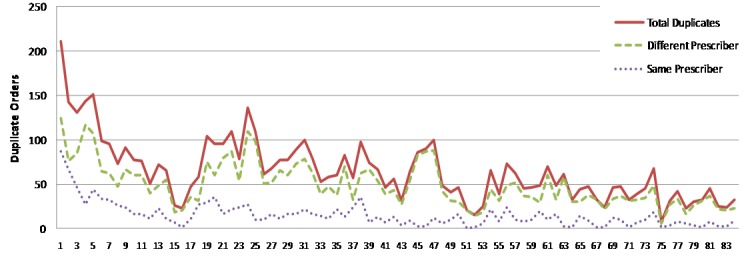
Duplicate orders by week: total, same prescriber, and different prescriber.
There was an 84.8% decrease in the duplication rate from week 1 (211 duplicates) to week 84 (32 duplicates), and a 94.6% decrease from the highest (week 1) to the lowest (week 75) (►Figure 1). The duplication rate of 3.7% Pre-interventions (780/21,081) was reduced to 0.9% Post-interventions (211/23,444); from nearly one duplicate for every 25 orders to fewer than nine in every 1,000, representing a decrease of 75.7% (p<0.01).
4.2 Duplicate Analysis by Drug
Over the 84 week period, 248 drugs were duplicated. However, only 23 drugs accounted for 80% of the duplications. Principal among these were hydromorphone (8.95%), acetaminophen (7.57%), ondansetron IV (7.26%), and oxycodone-acetaminophen 5/325 mg (6.63%).
4.2.1 General Interventions
Knowing which drugs were most commonly duplicated allowed us to design effective interventions. These included elimination from order sets, where appropriate; “un-defaulting“ previously defaulted medications on order sets; activating alerts on targeted drugs and allowing the pharmacy to censor certain medications.
4.2.2 Effectiveness of General Interventions
Some of our interventions met with significant success. For example, when we activated alerts for diphenhydramine and metoclopramide, the rates of duplication diminished to nearly zero. Other interventions were less successful. Authorizing our pharmacists to “censor” duplicate orders for specific medications did not significantly decrease duplicate orders for these medications. We attribute this to the fact that at the time of the study, pharmacists were using two different electronic systems, in addition to paper. Also, the alerts in the 2 electronic systems were not integrated.
Overall, the interventions worked very well. Before implementation of interventions, 73 drugs were involved in duplications, of which 16 accounted for 80% of the duplications. The ten most duplicated drugs, in decreasing order of frequency, were: hydromorphone IV, acetominophen, ondansetron IV, oxycodone-acetominophen 5mg-325mg, esomeprazole, metoclopramide IV, sodium phosphate/biphosphate, diphenhydramine, trimethobenzamide INJ and diphenhydramine IVPB. After implementation of interventions, 44 drugs were involved in duplications, of which 20 accounted for approximately 80% of the duplications. Twenty drugs were common to both the Pre-and Post-intervention periods. Of these twenty, seventeen demonstrated a significant reduction in duplicates.
4.3 Duplicate Orders by Source: Same vs. Different Prescriber
The data were analyzed to determine if each duplicate order was generated from the same versus different prescriber. For each week of the study, duplicates generated by different prescribers outnumbered the duplicates by the same prescriber (►Figure 1). Over the entire 84 weeks, there were 1,283 same prescriber duplicates (1,283/5,442; 23.6%) versus 4,159 different prescriber duplicates (4,159/5,442; 76.4%,) the latter occurring at a significantly higher rate (p<0.01).
4.3.1 Intervention Strategies: by Provider
We developed a number of strategies to reduce the number of same prescriber and different prescriber duplicates. These included individual training by a dedicated IT trainer for all individuals requesting one-on-one training, e-mails to prescribers after duplicate events were noted, reminders in staff conferences and other group meetings, CD and computer based re-training, weekly e-mails to the heads of residency and fellowship training programs, the PA supervisor and various service and division Chiefs, meetings with individual prescribers held by the Director of Resident Training, and various Chiefs of Service.
4.3.2 Effectiveness of intervention strategies by provider
Same prescriber duplicates fell 90.8% (p<0.01) from 271 (271/780, 34.7%) for the five weeks Pre-interventions to 25 (25/159 15.7%) for the five weeks Post-interventions. Same prescriber duplicates dropped from 87 in week 1 to 3 in week 83, a reduction of 96.6% (p<0.01, ►Figure 1).
The duplicate order rate for different prescribers was reduced by 73.7% (p<0.01) from 509 (509/780 65.3%) Pre-interventions to 134 (134/159 84.3%) Post-interventions and a drop from 124 in week 1 to 23 in week 84, an improvement of 81.5% (p<0.01, ►Figure 1). Although duplicate orders decreased significantly for both groups, there was a 96.6% reduction in same prescriber duplicates from the first week to the final week, versus an 81.5% reduction in duplicates from different prescribers.
4.4 Duplicate Orders by Source: Same vs. Different Prescriber Department
We next analyzed duplicates from the same department versus different departments (i.e. Anesthesia, Medicine, Orthopedics, Pediatrics, Radiology). Most duplicate orders originated from within the same department. Pre-Interventions, the ratio of same department to different department duplicates was 2.2:1.
4.4.1 Intervention Strategies: by Department
Intervention strategies targeting departments included lectures, departmental meetings, training sessions, and e-mails sent to the heads of departments that outlined specific instances of duplicate orders from members of their departments.
4.4.2 Effectiveness of intervention Strategies by Department
The result was a reduction of same department duplicates of 87.3% from Pre- to Post-interventions (p<0.01). This represents a reduction in same department duplicates from over 100 per week (536/5) to under 15 (68/5). Different department duplicates fell by 62.7% (p<0.01), representing a change in duplicates between departments from nearly 50 per week pre-interventions (244/5) to under 20 (91/5) post interventions.
4.5 Duplicate Orders by Source: by “Prescriber Group”
Eighteen different “prescriber groups” were identified (►Table 1). Before interventions, duplicates were caused by nine of the 18 prescriber groups (50%). Five of the nine groups accounted for 90.3% of all duplicates: anesthesia attendings had the biggest share of duplicate orders (24.6%), followed by physician assistants (20.3%), anesthesia fellows (17.9%), orthopedic fellows (15.0%) and orthopedic residents (12.4%). The data were also analyzed to determine the percent of all orders that were duplicates. Anesthesia fellows were highest: 11.3% of their 1,243 orders were duplicates. Anesthesia residents had a duplicate rate of 8.64% of 741 orders, followed by orthopedic attendings with a rate of 5.88 %. All other groups were under 5%.
Table 1.
Pre- and Post-Intervention Duplicate Order Rates by Prescriber Role/Credential and Department.
| Pre-Interventions | Post Interventions | Freq of Duplicates | Pct of Duplicates | Duplication Rate | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Department & Credential | Total Order Placed | Pct/Share of Orders Placed | Duplicates | Pct/Share of Duplicate Orders | Percent of Orders that are Duplicates: Rate | Total Order Placed | Pct/Share of Orders Placed | Duplicates | Pct/Share of Duplicate Orders | Percent of Orders that are Duplicates: Rate | Percent Change in Duplicate Frequency * | p-Val ue | Percent Change in Pct/Share of Duplicates * | p-Value | Change in Percent of Orders that are Duplicates * | p-Value |
| Anesth Resident | 741 | 3.56 | 64 | 8.21 | 8.64 | 380 | 2.08 | 15 | 9.43 | 3.95 | –76.6 | p<0.01 | 15.0 | p<0.01 | –54.3 | p<0.01 |
| Anesth Fellow | 1243 | 5.97 | 140 | 17.95 | 11.26 | 667 | 3.65 | 5 | 3.14 | 0.75 | –96.4 | p<0.01 | –82.5 | p<0.01 | –93.3 | p<0.01 |
| Anesth Attending | 6059 | 29.10 | 192 | 24.62 | 3.17 | 5238 | 28.70 | 20 | 12.58 | 0.38 | –89.6 | p<0.01 | –48.9 | p<0.01 | –88.0 | p<0.01 |
| Medicine Resident | 83 | 0.40 | 0 | 0.00 | 0.00 | 51 | 0.28 | 0 | 0.00 | 0.00 | ||||||
| Medicine Fellow | 2 | 0.01 | 0 | 0.00 | 0.00 | 11 | 0.06 | 0 | 0.00 | 0.00 | ||||||
| Medicine Attending | 248 | 1.19 | 10 | 1.28 | 4.03 | 129 | 0.71 | 6 | 3.77 | 4.65 | –40.0 | ns | ns | 15.3 | ns | |
| Ortho Resident | 3857 | 18.52 | 97 | 12.44 | 2.51 | 3014 | 16.51 | 28 | 17.61 | 0.93 | –71.1 | p<0.01 | 41.6 | p<0.01 | –63.1 | p<0.01 |
| Ortho Fellow | 3913 | 18.79 | 117 | 15.00 | 2.99 | 4478 | 24.53 | 41 | 25.79 | 0.92 | –65.0 | p<0.01 | 71.9 | p<0.01 | –69.4 | p<0.01 |
| Ortho Attending | 17 | 0.08 | 1 | 0.13 | 5.88 | 8 | 0.04 | 0 | 0.00 | 0.00 | ns | ns | ns | |||
| Peds Resident | 13 | 0.06 | 0 | 0.00 | 0.00 | 104 | 0.57 | 0 | 0.00 | 0.00 | ||||||
| Peds Fellow | 20 | 0.10 | 0 | 0.00 | 0.00 | 2 | 0.01 | 0 | 0.00 | 0.00 | ||||||
| Peds Attending | 3 | 0.01 | 0 | 0.00 | 0.00 | 9 | 0.05 | 0 | 0.00 | 0.00 | ||||||
| Radiology Resident | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | ||||||
| Radiology Fellow | 2 | 0.01 | 0 | 0.00 | 0.00 | 21 | 0.12 | 1 | 0.63 | 4.76 | ns | ns | ns | |||
| Radiology Attending | 7 | 0.03 | 0 | 0.00 | 0.00 | 1 | 0.01 | 0 | 0.00 | 0.00 | ||||||
| Nurse Pract | 174 | 0.84 | 1 | 0.13 | 0.57 | 335 | 1.84 | 4 | 2.52 | 1.19 | ns | ns | ns | |||
| Phys Asst | 4417 | 21.21 | 158 | 20.26 | 3.58 | 3700 | 20.27 | 39 | 24.53 | 1.05 | –75.3 | p<0.01 | 21.1 | p<0.01 | –70.5 | p<0.01 |
| Pharmacists | 25 | 0.12 | 0 | 0.00 | 0.00 | 105 | 0.58 | 0 | 0.00 | 0.00 | ||||||
| Total | 20824 | 100 | 780 | 100 | 3.75 | 18253 | 100 | 159 | 100 | 0.87 | –79.6 | p<0.01 | –76.7 | p<0.01 | ||
*Note: Blanks indicate inability to compute change due to a pre or post-Intervention zero value, or a computationally inappropriate value.
4.5.1 Intervention Strategies: by Prescriber Group
We used a similar approach to prescriber groups we used with individual prescribers, except the approach was directed towards the groups as a whole (see 4.3.1).
4.5.2 Effectiveness of Intervention Strategies by Prescriber Group
Post-interventions, the duplicate rates were again associated with a subset of prescribers: 9 of 14 groups. The top 5 accounted for over 90% of all duplicates. However, the percentage of all orders that were duplicates was under 5% for all categories.
Pre- versus Post-interventions duplication rates revealed statistically significant decreases in the frequency of duplicates, the percentage of duplicates and the duplication rate for six of the groups; all but one of the groups for which the change in rate was noteworthy. Collectively, the duplication rate for the groups fell by 76.7% (p<0.01).
4.6 Other Provider Factors
The data were also reviewed to determine if an increase in duplicate orders occurred when new residents arrived at the end of June or when they changed services. We found no obvious or statistically significant relationship between duplicate orders and rotation schedule for orthopedic and anesthesiology residents.
4.7 Order Sets versus Single Orders
We analyzed the duplicate orders with respect to their “origin” as follows:
-
1.
Both from the same order set
-
2.
Both from different order sets but containing overlapping orders
-
3.
The original was a single order, and the duplicate was from an order set
-
4.
The original was from an order set, and the duplicate was a single order
-
5.
Neither was from an order set: both original and duplicate were single orders
Duplicates originating from order sets included groups 1, 2, and 3. Duplicates originating from single orders included groups 4 and 5. As shown in ►Figure 2, for almost every week, there were more duplicate orders originating from order sets than from single orders.
Fig. 2.
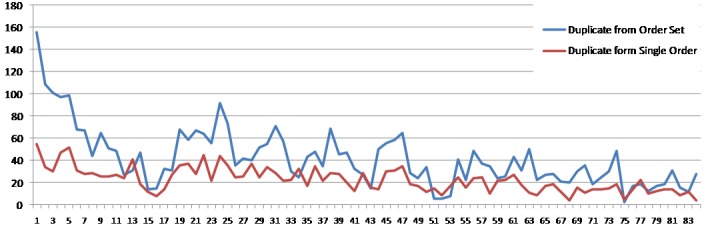
Weekly duplicate orders originating from order sets versus single order.
Most duplicates originated from either entering the same order set twice, or from different order sets which contained the same drugs (i.e. overlapping order sets). It was important to address duplicates originating from order sets; not only because of their numbers, but because the order set content could be changed by clinical governance. We were able to do this for a number of order sets.
Using these techniques, duplicate orders originating from order sets and from single orders were reduced from Pre-interventions to Post-interventions by 79.7% (p<0.01) and 79.3% (p<0.01) respectively (►Table 2 and ►Figure 2). Thus, duplicates from order sets fell from over 600 Pre-interventions to less than 100 duplicates Post-interventions. There was an equivalent decrease in duplicate originating from single orders: from 150 duplicates Pre-interventions to approximately 30 duplicates Post-interventions.
Table 2.
Pre- versus Post- Intervention Duplicate Orders by Source or Origination and Duplication.
| 84 Week | Pre-Interventions | Post-Interventions | Percent Change | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Duplicates | Pct | Duplicates | Pct | Duplicates | Pct | |||
| Same Order Set | 1311 | 24.1% | 302 | 38.7% | 44 | 27.7% | –85.4% | p<0.01 |
| Overlapping OS | 1539 | 28.3% | 224 | 28.7% | 36 | 22.6% | –83.9% | p<0.01 |
| Orig Single, Dup OS | 683 | 12.6% | 36 | 4.6% | 26 | 16.4% | –27.8% | ns |
| Duplicate from Order Set | 3533 | 64.9% | 562 | 72.1% | 106 | 66.7% | –81.1% | p<0.01 |
| Orig OS, Dup Single | 698 | 12.8% | 63 | 8.1% | 18 | 11.3% | –71.4% | p<0.05 |
| Both Original Orders | 1211 | 22.3% | 155 | 19.9% | 35 | 22.0% | –77.4% | p<0.05 |
| Duplicate from Single Order | 1909 | 35.1% | 218 | 27.9% | 53 | 33.3% | –75.7% | p<0.01 |
| Totals | 5442 | 780 | 159 | –79.6% | p<0.01 | |||
4.8 Order Sets and Workflow
Not all duplicate orders originating from overlapping order sets are amenable to simple changes in order sets, as changes in workflow are sometimes required. We noted that some duplicates originating from order sets were generated when a patient was admitted to the hospital as an emergency, and then subsequently undergoes surgery. Admitting orders are entered via the Orthopedic Admission Order Set, and after surgery, a post-op order set is used. If the admitting orders are not discontinued when post-op orders are entered, then multiple duplicates are created. Prior to go-live, the admission orders were discontinued by “protocol”. The Unit Registrar would simply remove the pre-operative paper orders from the order section when the patient went to surgery (effectively “discontinuing” them). In the current state pre-op orders must be actively discontinued; prescriber order management is required. We tracked these errors, and educated where necessary. Other duplicate orders were traced to the workflow in ambulatory surgery. For example, both the anesthesiologists and the orthopedists were entering post-op pain medications. When this workflow was clarified, duplicates diminished.
Following the strategies outlined above, we reduced the number of duplicates originating from order sets by 79.6% (p<0.01). Duplications were significantly reduced for four of the five categories of source and duplication (►Table 2 and ►Figure 3). The only category for which duplicates were not reduced significantly were duplicates from an order set for which the original was a single order. None-the-less, there was still a 27.8% reduction in duplicates (p<0.01).
Fig. 3.
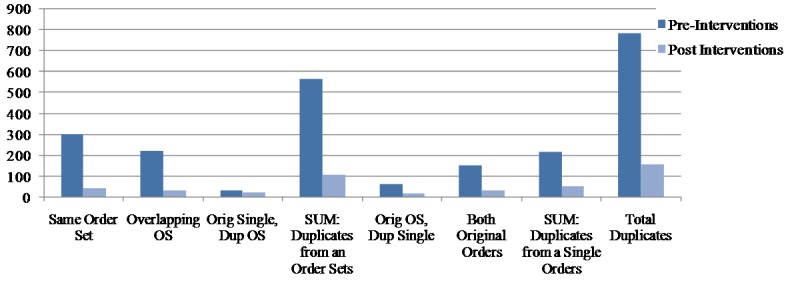
Pre- versus Post-intervention duplicate orders by source of originating and duplicate order.
4.9 Time Intervals for Duplication
We next focused on the time interval from the original order to the duplicate order. For each time frame analyzed, duplicates were more likely to be generated sooner rather than later. This holds true for duplicates generated within the first; 10 minutes; one hour; one day; and two weeks. For each time interval examined, more duplicates occurred earlier than later. (Data not displayed).
5. Discussion
The challenge of duplicate orders at Hospital for Special Surgery became obvious shortly after CPOE implementation. This paper reports the techniques we developed to analyze the duplicate orders so that we could design tactics to reduce them. Using this approach, we successfully decreased duplicate orders from 211 per week to 32 per week, a reduction of 84.8% (p<0.01). When fewer duplicates are entered, there are significant improvements in “downstream” effects for those involved in the medication management and administration chain. Our study both identifies the causes of duplicate orders and the effects of a successful strategy to reduce them.
As described above, our goals were to identify the drugs which were being duplicated most frequently and create strategies to reduce them. These strategies included the following interventions:
-
1.
many duplicated drugs were defaulted within order sets, wherever possible they were “un-defaulted”,
-
2.
many drugs were removed from order sets altogether (and now require a specific order to prescribe),
-
3.
additional duplicate alerts were activated for high-risk and high-frequency drugs, and
-
4.
the pharmacy was asked to discontinue certain duplicate orders.
Because our analysis demonstrated that most duplicates were associated with order sets, we paid particular attention to duplicates originating from order sets and were able to reduce them significantly.
After identifying the specific prescribers and groups responsible for most duplicate orders, we focused on retraining them. Strategies included individual counseling; e-mails to prescribers following duplicate events; reminders in staff meetings and other group meetings; CDs and Computer Based Training; and weekly e-mails to department heads.
We remained sensitive to striking a balance between helpful alerts and those that might contribute to alert fatigue [26, 27, 28]. In a review of drug safety alerts in CPOE, it was noted that clinicians override such gratuitous alerts 49–96% of the time [19]. (In that study there was no specific mention of duplicate order alerts.) On go-live, we decided not to activate duplicate alerts on all medications, but focused on high-risk and high-frequency drugs. Despite our literature-reinforced concerns, when we activated additional duplicate alerts, we were pleased to see that duplicates decreased significantly. We have since extended alerts to additional medications with similar success.
As with many types of unintended consequences, understanding workflow is a key to remediation. One example of this was cited by Campbell et al. [12]: duplicate orders for x-rays occurred because the “gatekeeper” function of the clerical staff was eliminated. We found similar issues in our patients whose existing pre-op orders were no longer being “discontinued” by the registrar after surgery. This can be attributed to a key difference between the electronic world and the paper world. With CPOE, the responsibility for “order maintenance” has moved forward, and placed on the prescriber. We believe this is as it should be. The best way to prevent order-entry errors is to stop these orders from being entered in the first place. Another workflow related example is that electronic orders can be placed simultaneously by different clinicians in different remote locations, a rare occurrence in paper-based processes.
Finally, we empowered our pharmacists to assist in reducing duplicate orders. A number of studies identify pharmacist interventions, some involving duplicate orders, after CPOE implementations [19]. In one study, pharmacists were given authority to change orders by methods including discontinuing duplicate orders for IV fluids and medications [28]. Another study reported that 14.8% of pharmacist interventions were performed because of duplicate orders. Interestingly, although both pharmacists and prescribers were presented with identical duplicate order warning screens, prescribers ignored these alerts more frequently than pharmacists did [29].
In contrast to these studies, our efforts to involve the pharmacy in censoring duplicates were unsuccessful. We believe this was due to a complex pharmacist workflow, which involved the use of two separate computer systems as well as paper. We have recently implemented a fully-computerized medication management system, which we believe will allow successful pharmacy interventions.
The first limitation to our study is that our method of identifying duplicates was to take weekly “snapshots” of all active orders at a single point in time. This method underestimates the total number of duplicates during the study period. However by expressing duplicates as a proportion of all orders, we feel that it is a valid representation of the problem. In addition, the time of the “snapshot” did not vary from week to week, and we believe that the prescribers present in the hospital, and the types of surgery performed on the “snapshot” day is representative of all weekdays. Creating a report that reflected the full range of duplicate order types was judged to be too time consuming, resource intensive, and beyond our capabilities during implementation.
Although there were clearly a large number of duplicate orders post-go-live, we do not know how many duplicate orders existed in the written world. It is possible that similar numbers of duplicates existed pre-CPOE. An extensive chart review would be needed to gain a better understanding of pre-CPOE duplicate orders.
A topic of interest is the number of duplicate orders that occurred at “time zero”. It has been documented that duplicate orders have been entered by a prescriber during a single ordering session – and many within 10 minutes of each other [22]. However, we believe that our findings may be an artifact related to activating post-op orders previously placed on hold. It seems impossible for a single prescriber, or different prescribers to duplicate an order in less than a second.
6. Conclusions
We implemented CPOE with CDS at the Hospital for Special Surgery to improve patient safety and enhance efficiency. Our CDS included dose range checking and alerts for drug interactions, drug allergies, and duplicate medication orders. It also included custom features designed specifically for orthopedic surgical patients [30]. We paid particular attention to alerts that are known to improve treatment and outcomes in hospitalized patients, such as drug condition alerts [23, 31]. However, we recognized that many of these alerts are ignored or “over-ridden” [32, 33]. Excessive alerting can lead to “decision support overload” and alert fatigue, where prescribers might ignore important messages [34]. It was therefore important to strike a balance between too many and too few alerts.
Upon go-live, many benefits, including elimination of illegibility and unapproved abbreviations and significant reductions in medication order turnaround time, were apparent. But we also noted an unintended and under-investigated negative consequence: duplicate medication orders.
By studying the specific drugs, the type and role of prescribers, the origin of the duplicate orders, and workflow, we were able to devise reduction strategies: changes in order sets to avoid overlapping medications; changes in work-flow; additional training strategies; altering pharmacy procedure, and broadening duplicate warnings. Using these methods, we were able to decrease duplicate orders significantly.
Sittig and Ash have recently published an authoritative volume entitled Clinical Information Systems; Overcoming Adverse Consequences [35]. They state that the goal of their book is to help organizations “… better understand and begin to deal with the inevitable, unintended, adverse events that may occur” (page xvii). With this goal in mind, we undertook this analysis of duplicate orders.
Clinical Relevance
Duplicate medication ordering is an example of a preventable use error with significant effects on patient care. While many papers describe the presence of duplicate alerts, this paper describes the nature of these orders and the successful reduction of duplicate orders after implementing CPOE at an academic university affiliated hospital. Understanding the sources and workflow-related causes of duplicate orders can lead to their reduction or elimination. Advanced clinical decision support can lead to reduction or elimination of duplicate orders. Attention to order set design can decrease duplicate orders. Education and training are important to reducing duplicate orders.
Conflict of Interest
Steven K. Magid and Christopher Forrer have no conflicts of interest. Steven Shaha is employed by the vendor of the computer information system Allscripts.
Human Subjects Protections
This study received Hospital for Special Surgery IRB approval as well as a waiver of informed consent and HIPAA authorization.
Acknowledgements
We would like to thank Melissa Honour for her help in analysis, Phyllis Tower for her research assistance and Staci Risman and Jaimie Lee for editorial assistance.
References
- 1.Kuperman GJ, Gibson RF. Computer physician order entry: benefits, costs, and issues. Ann Intern Med 2003; 139: 31–39 [DOI] [PubMed] [Google Scholar]
- 2.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes. A systematic review. JAMA 2005; 293: 1223–1228 [DOI] [PubMed] [Google Scholar]
- 3.Amarasingham R, Plantinga L, Diener-West M, Gaskin DJ, Powe NR. Clinical information technologies and inpatient outcomes: a multiple hospital study. Arch Intern Med 2009; 169: 108–114 [DOI] [PubMed] [Google Scholar]
- 4.Committee on Quality of Health Care in America, Institute of Medicine To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [Google Scholar]
- 5.Bates DW, Kuperman G, Teich JM. Computerized physician order entry and quality of care. Qual Manag Health Care 1994; 2: 18–27 [PubMed] [Google Scholar]
- 6.Institute of Safe Medical Practice. ISMP’s Guidelines for Standard Order Sets. Available at: http://www.ismp.org/Tools/guidelines/StandardOrderSets.pdf Accessed April 25, 2010.
- 7.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma'Luf N, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc 1999; 6: 313–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices Arch Intern Med 2000; 160: 2741–2747 [DOI] [PubMed] [Google Scholar]
- 9.Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005; 293: 1197–1203 [DOI] [PubMed] [Google Scholar]
- 10.Nebeker JR, Hoffman JM, Weir CR, Bennett CL, Hurdle JF. High rates of adverse drug events in a highly computerized hospital. Arch Intern Med 2005; 165: 1111–1116 [DOI] [PubMed] [Google Scholar]
- 11.Han YY, Carcillo JA, Venkataraman ST, Clark RSB, Watson RS, Nguyen TC, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 2005; 116: 1506–1512 [DOI] [PubMed] [Google Scholar]
- 12.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2006; 13: 547–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ash JS, Sittig DF, Dykstra RH, Guappone K, Carpenter JD, Seshadri V. Categorizing the unintended socio-technical consequences of computerized provider order entry. Int J Med Inform 2007; 76(suppl 1): S21–S27 [DOI] [PubMed] [Google Scholar]
- 14.Ash JS, Sittig DF, Poon EG, Guappone K, Campbell E, Dykstra RH. The extent and importance of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2007; 14: 415–423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McNutt RA, Abrams R, Arons DC; Patient Safety Committee. Patient safety efforts should focus on medical errors. JAMA 2002; 287: 1997–2001 [DOI] [PubMed] [Google Scholar]
- 16.Weiner JP, Kfuri T, Chan K, Fowles JB. “e-Iatrogenesis”: the most critical unintended consequence of CPOE and other HIT. Am Med Inform Assoc 2007; 14: 387–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans KD, Benham SW, Garrard CS. A comparison of handwritten and computer-assisted prescriptions in an intensive care unit. Crit Care 1998; 2(2): 73–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colpaert K, Claus B, Somers A, Vandewoude K, Robays H, Decruyenaere J. Impact of computerized physician order entry on medication prescription errors in the intensive care unit: a controlled cross-sectional trial. Crit Care 2006; 10(1): R21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuperman GJ, Bobb A, Payne TH, Avery AJ, Gandhi TK, Burns G, et al. Medication-related Clinical Decision Support in Computerized Provider Order Entry Systems: A Review. J Am Med Inform Assoc 2007; 14: 29–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spencer DC, Leininger A, Daniels R, Granko RP, Coeytaux RR. Effect of a computerized prescriber-order-entry system on reported medication errors. Am J Health Syst Pharm 2005; 15: 62(4)16–9 [DOI] [PubMed] [Google Scholar]
- 21.George D, Austin-Bishop N. Error rates for computerized order entry by physicians versus nonphysicians. Am J Health-Syst Pharm 2003; 60: 2250–2252 [DOI] [PubMed] [Google Scholar]
- 22.Fitzhenry F, Peterson JF, Arrieta M, Waitman LR, Schildcrout JS, Miller RA. Medication administration discrepancies persist despite electronic ordering. J Am Med Inform Assoc 2007; 14: 756–764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schedlbauer A, Prasad V, Mulvaney C, Phansalkar S, Stanton W, Bates DW, et al. What evidence supports the use of computerized alerts and prompts to improve clinicians’ prescribing behavior? J Am Med Inform Assoc 2009; 16: 531–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reckmann MH, Westbrook JI, Koh Y, Lo C, Day RO. Does computerized provider order entry reduce prescribing errors for hospital inpatients? A systematic review. J Am Med Inform Assoc 2009; 16(5): 613–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wetterneck TB, Walker JM, Blosky MA, Cartmill RS, Hoonakker P, Johnson MA, et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc 2011; 18(6): 774–782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuperman GJ, Reichley RM, Bailey TC. Using commercial knowledge bases for clinical decision support: opportunities, hurdles, and recommendations. J Am Med Inform Assoc 2006; 13: 369–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Sijs H, Aarts J, Vulto A, Berg M. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc 2006; 13: 138–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Senholzi C, Gottlieb J. Pharmacist interventions after implementation of computerized prescriber order entry. Am J Health Syst Pharm 2003; 60: 1880–1882 [DOI] [PubMed] [Google Scholar]
- 29.Fair MA, Pane F. Pharmacist interventions in electronic drug orders entered by prescribers. Am J Health Syst Pharm 2004; 61: 1286–1288 [DOI] [PubMed] [Google Scholar]
- 30.Magid SK, Pancoast PE, Fields T, Bradley DG, Williams RB. Employing clinical decision support to attain our strategic goal: the safe care of the surgical patient. J Healthc Inf Manag 2007; 21: 18–25 [PubMed] [Google Scholar]
- 31.Rind DM, Safran C, Phillips RS, Wang Q, Calkins DR, Delbanco TL, et al. Effect of computer-based alerts on the treatment and outcomes of hospitalized patients. Arch Intern Med 1994; 154: 1511–1517 [PubMed] [Google Scholar]
- 32.Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS. Physicians' decisions to override computerized drug alerts in primary care. Arch Intern Med 2003; 163: 2625–2631 [DOI] [PubMed] [Google Scholar]
- 33.Lin CP, Payne TH, Nichol WP, Hoey PJ, Anderson CL, Gennari JH. Evaluating clinical decision support systems: monitoring CPOE order check override rates in the Department of Veterans Affairs' Computerized Patient Record System. J Am Med Inform Assoc 2008; 15: 620–626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc 2004; 11: 104–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sittig DF, Ash JS, Clinical Information Systems; Overcoming Adverse Consequences, 1st ed. Sudbury, MA: Jones and Bartlett; 2011 [Google Scholar]


