Abstract
Background
Growth chart recording is a key component of pediatric care. EHR systems could provide several growth charting functionalities compared to paper methods. To our knowledge, there has been no U.S. study exploring clinicians’ perceptions and practices related to recording of growth parameters as they adapt to electronic methods.
Objectives
To explore clinician practices regarding recording growth parameters as they adapt to electronic health records (EHR) and to investigate clinician perceptions of electronic growth charting using EHR.
Methods
An online survey of pediatricians and family practitioners in Kentucky inquiring about EHR usage, specifically use of growth charting with EHR, was conducted.
Results
Forty-six percent of respondents utilized EHRs, with pediatricians lagging family practitioners, and academic pediatricians lagging non-academicians. There was no consensus on EHR platforms being used. Almost a third of those who used EHR did not utilize electronic growth charting. Clinicians using EHR reported that electronic growth charts would improve clinician satisfaction and clinical efficiency as well as parent satisfaction and parent education. Only 12% of respondents provided copies of growth charts to parents at the end of their visit and discussed growth parameters with parents, with clinicians using EHR more likely to engage in these activities than non-EHR users.
Conclusion
Although Kentucky clinicians continue to slowly adopt EHRs, clinician perceptions and practices reflect enduring barriers to widespread use of electronic growth charting in pediatric and family practice. However, our results suggest that electronic growth charting has important benefits for both clinicians and patients, and greater adoption is expected as EHRs become standard across health care systems.
Keywords: Growth charts, pediatrics, family practice, electronic health record
Introduction & Background
Electronic health record (EHR) systems are becoming an increasingly central feature of clinical practice in the United States. The American Academy of Pediatrics (AAP) advocates realization of an electronic infrastructure with central coordination across all care settings. This organization also promotes vendor-neutral portability and financial support for implementation and development of such electronic systems [1]. Yet, physician perceptions of the impact of EHR implementation are not well understood. Qualitative research has revealed that some physicians believe that EHR systems improve and others believe that they worsen professional performance and efficiency [2]. Moreover, studies have shown that as clinicians become accustomed to EHR use, utilization of the system and efficiency of staff and physicians also increases [3, 4].
A central component of pediatric care is the assessment of growth as a measure of a child’s nutritional and general health status through the use of growth charts. As EHR systems are usually designed for adult care, special requirements for EHR systems in pediatrics have been identified and reviewed [5]. Standards for pediatric growth chart recommendations for software design in pediatric EHRs must include functionalities for growth and development data, special terminology and information for pediatric care and age-based normal ranges [6, 7]. The AAP provides performance standards that serve as quality measurements and data standards continue to evolve [8], although there are many areas where pediatricians should continue to be actively involved in pediatric EHR development [9].
Objectives
To our knowledge, there has been no U.S. study exploring how clinicians document growth parameters as they adapt to electronic methods. As a first step, this study was done with Kentucky clinicians to examine what practices are being used to monitor growth in children and adolescents; and to investigate types and utilization of electronic growth charting using EHR.
Methods
All procedures were reviewed and approved by University of Kentucky Office of Research Integrity.
Subjects
Using an online method, members of the Kentucky Chapter of American Academy of Pediatrics (KYAAP) and the Kentucky Academy of Family Physicians (KAFP) were electronically surveyed. Family practitioners were included with pediatricians in the sample due to their involvement with children’s healthcare, especially in Kentucky. The executive offices of both organizations sent out an e-mail with a survey link to the entire membership with 3 reminders sent out at 30-day intervals after the initial release of the survey. Survey data was collected between March and May 2011. Responses to the survey were anonymous and participants were informed that all data would be disclosed in aggregate. No incentives were provided and electronic submission only allowed one response per participant IP address, prohibiting multiple survey submissions by the same individual.
Survey Instrument
The instrument was designed by the authors and revised on Surveymonkey®, an online survey engine. The 39-question instrument (►Appendix 1 as Supplementary File) measures demographic data and practices and attitudes regarding EHRs and growth charting. The survey was reviewed and validated by an out-of-state clinician and a statistician who were not part of the study group prior to refining the final instrument. The demographics section contained questions on board certification, practice type and location, years in practice, patient insurance distribution, number of patients seen per week, and the age range for which growth was recorded in their clinic.
The section on electronic health record usage contained questions regarding the name of the electronic platform, preference of EHR to paper medical records, re-checks of EHR with paper copies of growth charts, utilization for plotting routine growth measurements, mechanisms of incorporating growth chart records into EHR, reliability of electronic growth charts compared to paper copies. It also asked about clinician beliefs regarding whether electronic growth charts would improve factors such as clinician satisfaction, parent satisfaction, clinical efficiency, reduction in medical errors, accuracy for special populations, education for parents, and transition between WHO and CDC charts.
Analysis
A statistical database was created using Microsoft® Excel, then data was imported into Stata 12 (Statacorp, LLP College Station, TX) for data analysis. To describe sample characteristics and responses, frequency distributions were provided on key variables. Bivariate measures of association (chi-square tests) were employed to identify significant relationships between variables. The p-value used to determine significance was 0.05. While corrections for multiple comparisons are often utilized in survey research (e.g., the Bonferroni method), we have opted not to make these adjustments, which reduce statistical power to detect significant effects [10, 11, 12]. Because the small sample size used here is associated with high likelihood of a Type II error (i.e., not rejecting the null hypothesis when it is actually false), this counterbalances the increased risk of a Type I error which may be associated with multiple testing1.
Results
A total of 173 members completed the survey. Response rate for KYAAP pediatricians was 13.4% (107/800) and 7.8% for KAFP 7.8% (66/850) family practitioners. Of the approximately 1700 distributed surveys to both pediatricians and family practitioners, 173 were returned (10.2%). Thirty-five respondents were excluded due to missing data on survey questions (20% of the sample). The final sample for analysis was 138. The excluded subset did not differ significantly from the analyzable subset on any respondent characteristics.
As shown in ►Table 1, 85 pediatricians and 53 family practitioners were represented from various practice types and practice locations. Board-certified and board-eligible practitioners represent 90% and 10% of respondents, respectively. About 28% of respondents were in an academic setting, 8% in a hospital-based group practice, 55% in a private group practice, and 9% in a private solo practice, mirroring the 2:3 ratio of Kentucky physicians in private and public practice. Thirty percent of respondents practiced in a rural area, 35% in a semi-urban area, and 35% in an urban area. Eighteen percent of respondents had been in practice for 0–5 years, 20% for 6–10 years, 15% for 11–15 years, and 47% for more than 15 years. Patient volume was less than 50 per week for 22% of respondents, 51–100 per week for 41% of respondents, 101–150 per week for 21% of respondents, and more than 150 per week for 16% of respondents. None of these sample characteristics differed significantly across pediatricians and family practitioners with the exception of practice setting and rural location. Pediatricians were more likely than family practitioners to be in academic settings (34% vs. 17%) and less likely to be in private solo practice (2% vs. 19%; X2 = 16.56, p<0.001). In addition, pediatricians were less likely than family practitioners to be located in rural areas (18% vs. 49%; X2 = 17.24, p<0.001).
Table 1.
Sample characteristics of respondents
| Analyzable Dataset (n = 137) | |
|---|---|
| Type of practitioner | |
| Pediatrician | 85 (62%) |
| Family Practitioner | 53 (38%) |
| Board status | |
| Non-board certified | 14 (10%) |
| Board certified | 124 (90%) |
| Type of setting | |
| Academic | 37 (28%) |
| Hospital-based group practice | 11 (8%) |
| Private group practice | 74 (55%) |
| Private solo practice | 12 (9%) |
| Location of clinical practice | |
| Rural | 41 (30%) |
| Semi-urban | 48 (35%) |
| Urban | 48 (35%) |
| Years of experience | |
| 0 – 5 years | 25 (18%) |
| 6 – 10 years | 27 (20%) |
| 11 – 15 years | 21 (15%) |
| More than 15 years | 64 (47%) |
| Number of patient per week | |
| 1 – 50 patients | 30 (22%) |
| 51 – 100 patients | 55 (41%) |
| 101 – 150 patients | 28 (21%) |
| More than 150 patients | 21 (16%) |
In all, 46% of respondents utilized EHRs. Forty percent of pediatricians and 57% of general practitioners reported using EHR, though this difference was non-significant (p = 0.06). As shown in ►Table 2 a significantly lower proportion of academic pediatricians vs. other types used EHR (X2 = 3.91, p<0.05). Among those who used EHR, most preferred this format to paper medical records (71% versus 29%). Among those who did not currently use EHR, nearly three-quarters reported that they were likely to adopt EHR in the next year (73%). Of the 39 respondents who currently used an EHR, 34 different platforms were used, with the most commonly used being EPIC, Centricity and Allscripts.
Table 2.
Cross-tabulation of use of medical records by type of practice.
| Pediatrician2 | Family Practitioner3 | |
|---|---|---|
| All settings1 | ||
| Uses EMR | 51 (60%) | 23 (43%) |
| Does not use EMR | 34 (40%) | 30 (57%) |
| Academic | ||
| Uses EMR | 7 (25%) | 7 (78%) |
| Does not use EMR | 21 (75%) | 2 (22%) |
| Non-Academic | ||
| Uses EMR | 30 (53%) | 23 (52%) |
| Does not use EMR | 27(47%) | 21 (48%) |
1 X2 =3 .62, p<0.10
2 Within pediatricians: X2 = 3.91, p<0.05
3 Within general practitioners: X2 = 1.99, p = 0.16
Of those who used EHR, 81% used electronic documentation for plotting routine growth parameters. Most physicians incorporated growth chart records into EHR using existing platform software (73%), although some scanned charts as an image (16%) or did not incorporate records electronically (11%). Nursing staff was most likely to complete growth charts (66%), followed by clinicians (56%). Among both respondents who used EHR and those who did not, 44% reported that electronically recorded growth charts are somewhat more reliable than paper charts, and 21% reported that they are much more reliable. A large percentage of respondents also believed that electronic growth charts would improve accuracy for special populations (82%) and would lead to a reduction in clinical errors (84%). However, clinicians using EHR did not differ statistically in their perceptions of the accuracy and efficacy of electronic growth charts (►Fig. 1).
Fig. 1.
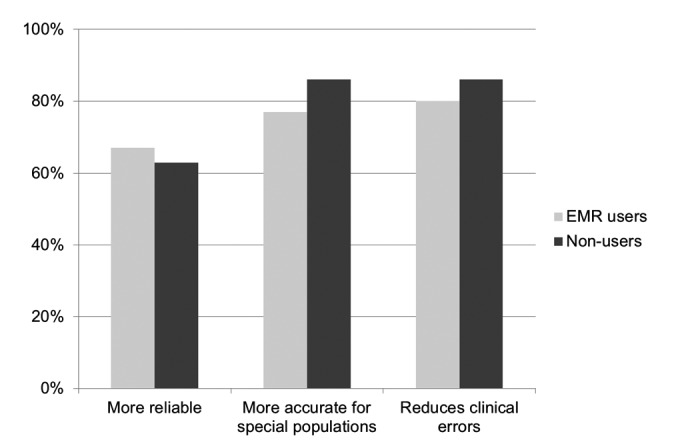
Frequency distributions on clinician attitudes towards the reliability and efficacy of electronic growth charts relative to paper charts.
Both EHR users and non-users reported on their perceptions of clinician experiences using electronic versus paper growth charts, with majority of clinicians agreeing that electronic growth charts would improve clinician satisfaction (80%) and improve clinical efficiency (83%). Ninety percent of those using EHR compared to 70% not using EHR reported that electronic growth charts would improve clinician satisfaction (X2 = 8.10, p<0.01). Also, 90% of those using EHR and only 77% of those not using EHR reported that electronic growth charts would improve clinical efficiency (X2 = 4.11, p<0.05) (►Fig. 2).
Fig. 2.
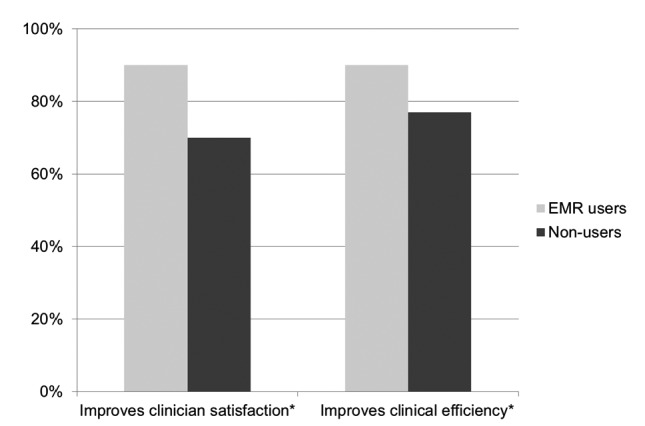
Frequency distributions on clinician attitudes toward clinician experiences using electronic growth charts (Note: *Users and non-users are significantly different at p<0.05 or less).
With respect to parent experiences, the majority of clinicians (66%) agreed that electronic growth charts would improve parent satisfaction. About 76% reported that electronic charts would also improve parent education. In all, 12% of respondents provided copies of growth charts to parents at the end of their visit, and a large majority of those who provided charts discussed body mass index, height, weight, head circumference, and nutritional status with parents.
In addition, respondents using EHR had more positive attitudes toward parent experiences and better clinical practices regarding parent education than non-users (►Fig. 3). Specifically, 80% of EHR users indicated that electronic growth charts would improve parent satisfaction compared to 53% of non-users (X2 = 10.35, p<0.001). In addition, 78% of EHR users indicated that electronic growth charts would improve parent education compared to 55% of non-users (X2 = 7.73, p<0.01). Finally, physicians using EHR were significantly more likely to share copies of growth charts with parents at the end of their visits (18%) than those who did not use EHR (5%; X2 = 5.82, p<0.05).
Fig. 3.
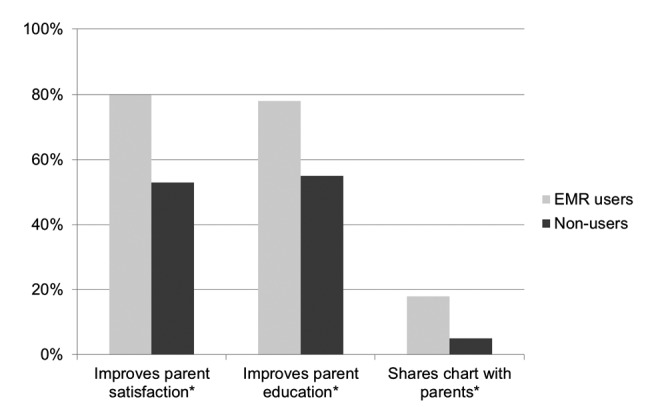
Frequency distributions on clinician practices and attitudes toward parent experiences with electronic growth charts (Note: *Users and non-users are significantly different at p<0.05 or less).
Discussion
We explored the practices of Kentucky clinicians in monitoring growth in children and adolescents in an age of Electronic Health Records (EHRs). Specifically, we investigated types of, and utilization of, electronic growth charting using EHRs. Less than half of clinicians surveyed utilize EHRs, but there was an encouraging trend towards adoption of EHRs with nearly three-quarters professing moving towards EHR adoption (compared to past studies with less than 50% adoption intent [13]). Family practitioner adoption rates in our survey were almost identical to rates in Washington State [14]. Pediatricians in our survey were more likely to have adopted EHR compared to past studies (13.7% in Florida and 21.3% nationally) [15, 16]. Consistent with other studies, pediatricians tended to have a lower adoption of EHR versus family practitioners [15] and academic clinicians had lower adoption rates than private community clinicians, contrary to most studies which have shown lower uptake in smaller group practices [17].
It is likely that cost, technical, organizational and other barriers [18] as well as limited pediatric-specific EHR options (specifically growth charting among the features) [19] are barriers to adoption of EHR among pediatricians. Additionally, there is no consensus adoption of EHRs with a variety of platforms being utilized. While we did not inquire what decision-process was followed in adoption of an EHR, we also did not find any studies that have explored determinants of EHR platform choice among practices. However, we suspect economics, leadership decision-making and functionality may be priorities for practitioners. The array of options can be confusing; there are 933 “complete
EHR” options for Ambulatory practice that are listed as “certified” under the Office of the National Coordinator for Health Information Technology (ONCHIT) [20]. The AAP’s Child Health Informatics Center (CHIC) aims to advocate for pediatrician-specific Health Information Technology (HIT) issues at the national level. It has attempted to increase education about pediatric-specific EHR adoption and implementation [21]. It has published reviews of 40 pediatric “friendly” platforms online, including specifically rating system ability to display growth data graphically, overlaying a standard age and gender-specific growth charts [22]. It is unclear to what extent clinicians utilize the guidance provided by CHIC while making decisions on adopting a specific platform.
While a majority of clinicians using EHRs did utilize electronic documentation for plotting growth parameters, mainly through existing platform software, a third of them still used paper charting systems, either scanning into the EHR or not including them in the electronic record. It is uncertain if these providers resorted to these activities due to lack of awareness of the EHR capability or because their platform did not support pediatric growth chart options. It is important to remember that “meaningful use” according to Centers for Medicare & Medicaid Services (CMS) which guides incentive payments for EHR use includes growth parameters as essential documentation [23].
Almost one third of clinicians felt that electronically recorded growth charts were less reliable than paper charts, though we are unable to discern the reasons for this perception. Most respondents believed that electronic growth charts would improve accuracy for special populations and would lead to a reduction in clinical errors.
Our study respondents using EHR had more positive attitudes toward the potential of electronic growth charts to improve clinical practice vis-a-vis clinician satisfaction and clinical efficiency. In this age of patient empowerment and move towards a personal health record, it is critical to share information with parents to enable them to be informed consumers. Moreover, growth recordings provide valuable information regarding nutritional status. This can both be reassuring (when in normal range) to worried parents, and encourage early intervention when abnormal. Most respondents in our study felt that electronic growth charts would improve parent satisfaction and improve parent education, with EHR users having more positive attitudes in this regard than non-users.
Communication with parents/caregivers about growth is highly recommended as they partner with physicians in children’s care [24]. With today’s concerns about rising obesity and the pivotal role that nutrition plays in caregivers’ perceptions of a child’s well-being, it is not unusual that almost two-thirds of parents in one study wanted to be shown a growth chart by a clinical provider [25]. In our study, providing copies of growth charts to parents at the end of the visit was uncommon, with only 1 in 8 clinicians doing so. Those who did also engaged in discussions about growth parameters and nutritional status with parents and caregivers. EHR-users were more likely to share copies of growth charts with parents at the end of their visits than non-users.
Limitations
We acknowledge that the small sample size and low response rate in our survey study are limitations. This is often seen with survey methodology not accompanied by incentives [26] and funding limitations precluded the use incentives for our study participants. Methods to increase e-survey response [27] were considered prior to design and execution of the study to improve response rate. Also, an almost 20% exclusion of respondents for non-completion of items occurred, but this subset did not significantly vary from analyzed respondents. Finally, because data on clinical practice sites were not collected in order to protect respondent confidentiality, we were unable to account for potential clustering of observations by site (i.e., multiple physicians in the same practice). While clustering does not affect sample estimation, it may lead to biased tests of significance. Consequently, additional research is needed to confirm the significance of relationships identified here.
We chose to survey members of the two large specialty practice organizations, KYAAP and KAFP, to reach the desired pediatricians and family practitioners who were most likely to encounter child and adolescent patients needing growth chart recording. While membership in organizations may not reflect all practicing clinicians, the two organizations represent about 70–80% of licensed practitioners in pediatrics and family practice in Kentucky. In addition, rural family practitioners were overrepresented in our sample, probably because FPs in urban areas are less likely to regularly see children than those in rural areas (due to limited access to pediatricians). Also, nurse practitioners were not included in this study, and they too are involved in child healthcare. We aim to be more inclusive in follow-up studies with these professionals in the future.
Additionally, this was a convenience sample of Kentucky clinicians, which may not be representation of physicians nationally. For pediatricians, Kentucky is comparable to other large American Academy of Pediatrics chapters, in terms of member initiatives, engagement activities, and other metrics [28]. For family practitioners, Kentucky reports a slightly higher “rurality” of members compared to other similar sized chapters [29]. In the future, we hope that findings presented here will be replicated and expanded to a nationally-representative sample in externally-funded follow-up studies.
Conclusions
In Kentucky, clinicians continue to slowly adopt Electronic Health Records, with pediatricians lagging family practitioners. There is still variability in EHR platforms being used, with some clinicians who use EHR still growth charting by paper means. Those clinicians who utilize EHRs have more favorable attitudes toward using EHRs, believe that electronic growth charting improves clinician and parent experiences, and communicate growth information to a greater extent than non-users of EHRs. There is a need for studies comparing accuracy of electronic growth charting to traditional methods before EHR growth charting becomes universal among clinicians who care for children and adolescents.
Clinical Relevance Statement
The work described in this manuscript reveals the continued low adoption of Electronic Health Records, particularly among pediatricians. There is still inconsistency of electronic growth charting even in EHR users, and skepticism about electronic growth chart accuracy. However, clinicians using EHRs capabilities for growth charting in children and adolescents communicate information to families about children’s growth, which makes for improved collaboration in children’s healthcare.
Conflict of Interest
The authors have no financial or other conflicts of interest related to the content or findings reported in this manuscript.
Protection of Human Subjects
All procedures used with human subjects in this study were approved by the University of Kentucky Office of Research Integrity, and in accordance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects.
Supplementary Material
Acknowledgments
The authors wish to acknowledge the assistance of Gerry Stover, Kentucky Academy of Family Physicians, and Mary York, Kentucky Chapter of American Academy of Pediatrics for disseminating the survey and for providing statistics regarding the organizations. No intramural or extramural funding was obtained in conducting this study.
Footnotes
1 The current sample has 91% statistical power to detect a difference in proportions of 0.20 (a large effect) between EHR users and non-users at an alpha level of 0.05. However, when the Bonferroni correction is applied, resulting in an alpha level of 0.0025, this sample has only 70% statistical power.
References
- 1.Council on Clinical Information Technology Health information technology and the medical home. Pediatrics 2011; 127(5): 978–982 [DOI] [PubMed] [Google Scholar]
- 2.Holden RJ. Physicians' beliefs about using EMR and CPOE: in pursuit of a contextualized understanding of health IT use behavior. Int J Med Inform 2010; 79(2): 71–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenbloom ST, Qi X, Riddle WR, Russell WE, DonLevy SC, Giuse D, Sedman AB, Spooner SA. Implementing pediatric growth charts into an electronic health record system. J Am Med Inform Assoc 2006; 13(3): 302–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samaan ZM, Klein MD, Mansour ME, DeWitt TG. The impact of the electronic health record on an academic pediatric primary care center. J Ambul Care Manage 2009; 32(3): 180–187 [DOI] [PubMed] [Google Scholar]
- 5.Task Force on Medical Informatics Special Requirements for Electronic Medical Record Systems in Pediatrics Pediatrics 2001; 108: 513 [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics: Task Force on Medical Informatics Special requirements for electronic medical record systems in pediatrics. Pediatrics 2001; 108(2): 513–515 [DOI] [PubMed] [Google Scholar]
- 7.Shiffman RN, Spooner SA, Kwiatkowski K, Brennan PF. Information Technology for Children's Health and Health Care, Journal of the American Medical Informatics Association 2001; 8(6): 546–551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spooner SA, Classen DC. Data standards and improvement of quality and safety in child health care. Pediatrics 2009; 123 (Suppl. 2): S74–S79 [DOI] [PubMed] [Google Scholar]
- 9.Gracy D, Weisman J, Grant R, Pruitt J, Brito A.Content barriers to pediatric uptake of electronic health records. Adv Pediatr 2012; 59(1): 159–181 [DOI] [PubMed] [Google Scholar]
- 10.Nakagawa S.A farewell to Bonferroni: The problems of low statistical power and publication bias. Behavioral Ecology 2004; 15: 1044–1045 [Google Scholar]
- 11.Bender R, Lange S.Adjusting for multiple testing- when and how? Journal of Clinical Epidemiology 2001; 54 (4): 343–349 [DOI] [PubMed] [Google Scholar]
- 12.Perneger T.What’s wrong with Bonferroni adjustments? British Medical Journal 1998; 316: 1236–1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simon SR, Kaushal R, Cleary P, Jenter C, Volk L, Poon E, Williams D, Orav E, Bates D.Correlates of electronic health record adoption in office practices: a statewide survey. Journal of the American Medical Informatics Association 2007; 14(1): 110–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stream GR.Trends in adoption of electronic health records by family physicians in Washington State. Inform Prim Care 2009; 17(3): 145–152 [DOI] [PubMed] [Google Scholar]
- 15.Menachemi N, Ettel DL, Brooks RG, Simpson L.Charting the use of electronic health records and other information technologies among child health providers. BMC Pediatr 2006; 6: 21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kemper AR, Uren RL, Clark SJ. Adoption of Electronic Health Records in Primary Care Pediatric Practices. Pediatrics 2006; 118; e20 [DOI] [PubMed] [Google Scholar]
- 17.Simon SR, McCarthy ML, Kaushal R, Jenter CA, Volk LA, Poon EG, Yee KC, Oray EJ, Williams DH, Bates DW. Electronic health records: which practices have them, and how are clinicians using them? Journal of Evaluation in Clinical Practice 2008; 14(1): 43–47 [DOI] [PubMed] [Google Scholar]
- 18.Boonstra A, Broekhuis M.Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res 2010; 10: 231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simpson LA, Peterson L, Lannon CM, Murphy SB, Goodman C, Ren Z, Zajicek A.Special challenges in comparative effectiveness research on children's and adolescents' health. Health Aff (Millwood). 2010; 29(10): 1849–1856 [DOI] [PubMed] [Google Scholar]
- 20.Office of the National Coordinator for Health Information Technology Available athttp://oncchpl.force.com/ehrcert?q=CHPL Accessed on May 30, 2012.
- 21.American Academy of Pediatrics (AAP) Child Health Informatics Center (CHIC) Available athttp://www2.aap.org/informatics/chic.html Accessed on May 30, 2012.
- 22.AAP COCIT EMR Product Reviews Available athttp://www.aapcocit.org/emr/readreviews.php?task=Compare_Feature&typefeat=GROWTH&filter=NAccessed on July 21, 2012
- 23.Centers for Medicare and Medicaid Services EHR Incentive Program Available athttps://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/EP-MU-TOC.pdfAccessed on June 4, 2012.
- 24.Canadian Paediatric Society & Dieticians of Canada Collaborative Public Policy Statement (2010). Promoting Optimal Monitoring of Child Growth in Canada: Using the New WHO Growth Charts Available athttp://www.cps.ca/english/statements/N/ExecSummary.pdf Accessed June 5, 2012. [DOI] [PubMed]
- 25.Ben-Joseph EP, Dowshe SA, Izenberg N.Do Parents Understand Growth Charts? A National, Internet-Based Survey. Pediatrics 2009; 124: 1100–1109 [DOI] [PubMed] [Google Scholar]
- 26.McMahon SR, Iwamoto M, Massoudi MS, Yusuf HR, Stevenson JM, David F, Chu SY, Pickering LK. Comparison of e-mail, fax, and postal surveys of pediatricians. Pediatrics 2003; 111(4 Pt 1): e299–e303 [DOI] [PubMed] [Google Scholar]
- 27.Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, Cooper R, Felix LM, Pratap S.Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009Jul 8; (3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Academy of Pediatrics (AAP) Department of Community, Chapter and State Affairs Available athttp://www.aap.org/Accessed September 14, 2012
- 29.American Academy of Family Physicians (AAFP) Available athttp://www.aafp.org/Accessed September 12, 2012 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


