Abstract
Background
Mental illness (MI) affects approximately one in five US adults, and is associated with oral disease and poor dental treatment outcomes. Little is known about dental utilization or unmet dental need in this population.
Methods
This study examined dental visits and unmet dental need in community-dwelling adults with MI in 2007 Medical Expenditure Panel Survey (MEPS) data. Differences between adults with and without MI were tested using multivariate logistic regression.
Results
Eighteen percent of adults (N=19,368) had MI; 5.5 percent had unmet dental need. Although individuals with MI were not significantly more likely to have a dental visit (46.3 percent) than those without MI (42.2 percent; OR=1.09, 95 percent CI=.97–1.23), they were significantly more likely to report unmet need (11.0 versus 5.3 percent; OR=2.00, 95 percent CI=1.67–2.41). Those with mood or anxiety disorders were most likely to report unmet need (Ps<.001).
Conclusions
While individuals with MI did not visit the dentist significantly more than adults without MI, their higher level of unmet need suggests current dental service use is not addressing their needs adequately.
Clinical Implications
Dentists should be familiar with MI conditions as these patients may have greater unmet dental need.
Keywords: Mental illness, dental need, utilization
INTRODUCTION
One in five US adults-- approximately 44 million people--have a diagnosable mental illness in any given year.1 The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-Text Revision)2 defines a mental illness as “a clinically significant behavioral or psychological syndrome or pattern…that is associated with present distress…or disability” (p. xxxi). Dental patients with a mental illness (MI) may present with a mood disorder, anxiety disorder, and sometimes schizophrenia or other psychotic disorder. These MI conditions may cause a significant impact on patients’ functioning, or may be managed with medication, psychotherapy, or a combination of therapeutic approaches with little impact on daily activities.3–8
MI has been found to be Mental illness (MI) can be associated with higher unemployment rates,9 lower income,10 and lack of preventive medical care.11 It is MI has also associated with such systemic diseases as cardiovascular disease and diabetes,12 which in turn can be related to poor oral health outcomes.13 MI has been linked with poor oral health, including increased tooth decay,14 untreated restorative needs,15 periodontal disease,16–17 and edentulism.18 Adults with MI are at increased risk for oral disease because of medication side effects,19–21 lack of access to dental care,22–23 and reduced motivation and ability to adequately complete oral self-care.24 In one of the few US studies, Stiefel and colleagues found significantly more dry mouth symptoms, soft tissue lesions, tooth decay, plaque and calculus in community-dwelling psychiatric patients with chronic MI compared with primary-care patients of similar age and gender.25
People with MI are often fearful of the dentist and dental treatment,26–27 yet dentists may be hesitant to use sedative medications because of uncertainty regarding medication interactions or the unpredictability of patients’ reactions to sedation.28 Additionally, some dentists are reluctant to treat individuals with symptoms of MI at all.29
Little is actually known about the oral health status and dental utilization of adults with psychiatric disorders in the US. Nevertheless, based on work outside of the US, it is likely that individuals with MI have greater need for dental care but are less able to afford it,30 suggesting the relationship between mental illness and poor oral health operates at least in part through lack of access to dental care. The aim of this study was to use data from the 2007 Medical Expenditure Panel Survey (MEPS) to compare differences in dental visits and unmet dental need in US adults with and without MI. We hypothesized that adults with MI, compared to those without MI, would be more likely to report unmet dental need but less likely to report having made dental visits. Further, it was hypothesized that individuals with MI who did receive care would be more likely to report receiving only non-preventive care than those without MI, and that those with MI conditions commonly perceived to be the most debilitating (e.g., schizophrenia) would report more unmet dental need than those without MI or with potentially less debilitating MI conditions (e.g., mood disorders).
METHODS
Data Source
We used examined data from the 2007 Medical Expenditure Panel Survey (MEPS).31 MEPS is a nationally representative health survey of the US community-dwelling population. Data for adults (age 21 and over) collected during 2007 from the Full Year Consolidated, Medical Conditions, and Dental Visit files were analyzed used for the current study.31 The University of Washington Institutional Review Board approved the study.
MEPS is made up of interview data. One key respondent from each participating family completes five in-person interviews at home over two years, with an interview occurring approximately every six months. Respondents provide information about medical conditions, healthcare utilization, hospitalizations, medication use, and personal characteristics for each non-institutionalized household member. Data from MEPS are de-identified and publicly available from the Agency for Healthcare Research and Quality (AHRQ) website. The MEPS data includes population weights to adjust for the complex sample design and to generate national population estimates.31
Variables
The associations between mental illness, dental utilization, and sociodemographic variables were examined. Selection of the the sociodemographic variables available in MEPSthe MEPS data was based on The Behavioral Model for Vulnerable Populations.32 Previous research has established the applicability of the Vulnerable Populations model to explain variation in oral health.33
Outcomes
We measured two outcomes:
Dental utilization: We defined dental utilization as the report of at least one dental examination in 2007. Non-preventive care was defined by a person receiving at least one procedure involving crowns; restorations; extractions; or treatment for abscess.34 We calculated whether participants had any dental utilization, and among those receiving care, whether they received only non-preventive care during 2007.
Unmet dental need: We defined unmet dental need as a report of one or more occurrences of being unable to receive necessary dental care or having experienced a delay in receiving necessary dental care. Two survey items asked (yes/no) if participants were unable to receive or were delayed in receiving dental care they or a dentist thought necessary for any reason in the prior 12 months. We combined these two variables into one, then dichotomized the combined variable into the presence or absence of unmet dental need.34
Sociodemographic Characteristics
Age was categorized into five comparably sized groups (see Table 1) for respondents age 21 or above as of December 31, 2007. Race/ethnicity was grouped into Hispanic, Non-Hispanic White, Non- Hispanic Black, and other. Education was categorized as less than high school, completed high school/General Educational Development (GED) degree, and more than high school. Employment was dichotomized into employed or unemployed, based on whether the individual was unemployed at any point during the prior 12-month period.
Table 1.
Comparisons of dental utilization and sociodemographic variables in adults by presence and absence of at least one mental illness (MI)
| Weighted percent (Standard Error) |
|||
|---|---|---|---|
| MI | No MI | ||
| 18.1 (0.4) | 81.9 (0.4) | Pp | |
| At least one dental visit in 2007 (n=7319) | 46.3 (1.0) | 42.2 (0.6) | NS |
| Non-Preventive visit only (n=907) | 12.0 (0.9) | 10.9 (0.5) | NS |
| Unmet Dental Need (n=1314) | 11.0 (0.6) | 5.3 (0.2) | <.001 |
| Age | |||
| 21–29 | 13.0 (0.9) | 18.7 (0.5) | <.001 |
| 30–39 | 17.6 (0.8) | 19.1 (0.4) | |
| 40–49 | 20.8 (0.9) | 19.9 (0.5) | |
| 50–59 | 21.3 (0.8) | 17.9 (.04) | |
| 60+ | 27.3 (1.0) | 24.4 (0.5) | |
| Sex | |||
| Male | 37.0 (0.8) | 50.7 (0.4) | <.001 |
| Female | 63.0 (0.8) | 49.3 (0.4) | |
| Race/ethnicity | |||
| Non-Hispanic White | 77.5 (0.9) | 67.2 (0.8) | <.001 |
| Non-Hispanic Black | 8.1 (0.5) | 11.9 (0.5) | |
| Other Non-Hispanic | 4.6 (0.5) | 6.8 (0.4) | |
| Hispanic | 9.8 (0.6) | 14.1 (0.6) | |
| Education | |||
| < High School | 15.1 (0.6) | 13.8 (0.4) | NS |
| HS/GED* | 49.8 (1.1) | 48.8 (0.6) | |
| > High School | 34.6 (1.1) | 36.6 (0.7) | |
| Missing | 0.5 (0.1) | 0.6 (0.1) | |
| Employment | |||
| Employed | 65.7 (1.1) | 65.4 (0.6) | NS |
| Unemployed | 34.3 (1.1) | 34.6 (0.6) | |
| Income (percent compared to poverty level) | |||
| High | 38.4 (1.1) | 43.1 (0.7) | <.001 |
| Middle | 28.7 (0.1) | 31.2 (0.6) | |
| Low | 13.9 (0.7) | 12.4 (0.4) | |
| Poor | 19.0 (0.8) | 13.2 (0.4) | |
| Dental Insurance | |||
| Yes | 40.0 (1.0) | 44.8 (0.6) | <.001 |
| No | 60.0 (1.0) | 55.2 (0.6) | |
| Health insurance | |||
| Any Private | 55.6 (1.1) | 56.4 (0.5) | NS |
| Public Only | 27.3 (0.9) | 27.4 (0.5) | |
| Uninsured | 17.1 (0.8) | 15.5 (0.5) | |
HS/GED = High school graduate/General Educational Development (GED) degree
We determined the presence of at least one mental illness (MI) using Clinical Classification (CC) codes 650-670.35 In each interview, interviewers asked the participant about all health conditions each household member experienced since the previous interview. Interviewers initially coded these conditions into ICD-9 codes36 that were then translated into CC codes.
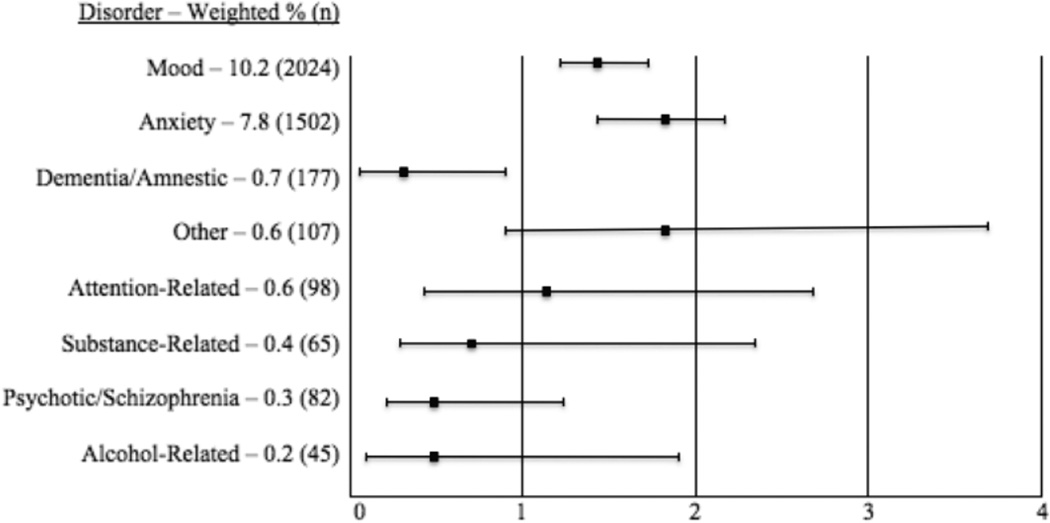
We identified the primary MI condition reported for each individual identified as having an MI, and all individuals with such a condition were included in the analysis. It was presumed that the first MI condition reported for each individual was the most salient. Among those with MI, most reported as the primary MI condition a mood disorder (10.2 percent), followed by anxiety (7.8 percent), dementia/amnestic (0.7 percent), miscellaneous/other (0.6 percent), attention-deficit hyperactivity/conduct/disruptive (0.6 percent), substance-related (0.4 percent), schizophrenia/other psychotic (0.3 percent), and alcohol-related disorder (0.2 percent).
For each MI condition reported, the respondent was asked if the condition resulted in a “serious impact” on the individual's overall health and well being. The impact was coded on a 4-point scale from “very seriously” to “not at all.” The presence of at least one serious MI condition (SMI) was indicated by a dichotomous variable (yes/no), where “yes” indicated that the mental illness condition either “very seriously” or “somewhat seriously” impacted the person’s overall health and well being. Among those with an SMI, unadjusted estimates found that most reported a mood disorder (38.3 percent), followed by anxiety (25.8 percent), dementia/amnestic (2.4 percent), attention-deficit hyperactivity/conduct/disruptive (1.8 percent), schizophrenia/other psychotic (1.2 percent), miscellaneous/other (1 percent), substance-related (0.6 percent), and alcohol-related disorder (0.6 percent).
Dental insurance was categorized as a dichotomous variable defined by whether or not an individual had any type of insurance coverage (including private or public) for dental procedures during 2007. Income was categorized into four groups based on the household income as a percentage of the Federal Poverty Level (ranging from $10,210 for a one-person household to $34,750 for an eight person household in 2007)37 as poor (up to 125 percent), low income (125 percent to less than 200 percent), middle income (200 percent to less than 400 percent), and high income (greater or equal to 400 percent). Medical insurance was defined as receiving assistance from only private insurance, any public insurance (Medicaid, Medicare, or other public sources), or being uninsured during 2007.
Data analyses
The frequencies presented are unweighted, as weighted frequencies do not have a very meaningful interpretation, and in order to provide both a clear representation of the proportion of the MEPS sample reporting mental illness conditions, dental visits, and unmet dental need. All analyses presented are weighted to provide a sense of the associations between these variables on a nationally representative scale. Weighted frequency distributions were examined and descriptive statistics were calculated for those reporting at least one MI compared to those without an MI (Table 1). Multivariate logistic regression analyses were used to examine the differences in presence of a dental visit and in unmet dental need between those with and without MI and between those with and without an SMI, adjusting for sociodemographic variables. Odds ratios (OR) and 95 percent confidence intervals (CIs) are presented to describe the strength of the adjusted associations between dental utilization, unmet need and MI. Chi-square analyses were used to examine differences in the presence of a dental visit in 2007 and unmet dental need between individuals without an MI and those with a specific MI condition (e.g., mood, anxiety disorders).
Data were analyzed using PASW version 18.0 Complex Samples (IBM Corporation, Somers, New York) that accounted for the complex sampling methods and population weights of MEPS data and to estimate confidence intervals.
RESULTS
The study population consisted of 19,368 adults. The mean age was 47.6 years (SE=0.2); 51 percent (SE=0.2) of the sample was female. Over 18 percent reported having at least one MI (n=3,525), while 6.5 percent of the sample (n=1,264) reported having at least one mental illness that seriously impacts their functioning (SMI).
Dental Utilization
Thirty-seven percent of all adults reported at least one dental visit for any reason in 2007. Individuals with MI were slightly more likely to report having had a dental visit (46.3 percent) than those without MI (42.2 percent; Table 1), and this association was not statistically significant when adjusted for the effects of sociodemographic variables (OR=1.09, 95 percent CI=.97–1.23). There was no significant difference in the probability of a dental visit for individuals with an SMI (44.1 percent) compared to those without an SMI (42.9 percent) when adjusted for the effects of sociodemographic variables (OR=1.05, 95 percent CI=.91–1.20).
Of those adults who reported a dental visit in 2007, 12.4 percent reported having only non-preventive visits (Table 1). There was no significant difference in receiving only non-preventive dental care between individuals with MI (12.0 percent) compared to those without MI (10.9 percent; OR=1.12, 95 percent CI=.86–1.42). Adults with SMI were just as likely to report having had only non-preventive dental visits (11.2 percent) as individuals without SMI (11.1 percent; OR=1.02, 95 percent CI=.81–1.82).
Unmet Dental Need
Overall, 6.8 percent of the adult sample reported having unmet dental need in 2007. Individuals with at least one MI (11.0 percent) were twice as likely to report unmet dental need in the previous 12 months compared to those without an MI (5.3 percent; OR=2.00, 95 percent CI=1.67–2.41, Table 1). When limiting the analysis to only those individuals with at least one SMI, those adults were still almost twice as likely to have unmet dental need (10.3 percent) than were those without a SMI (6.1 percent; OR=1.76, 95 percent CI=1.29–2.25) after adjusting for the impact of sociodemographic variables. Having at least one dental visit in 2007 did not alter this relationship (OR=1.81 for individuals with MI who reported at least one dental visit (95 percent CI=1.71–2.71); OR=1.91 for individuals with MI who did not have a dental visit (95 percent CI=1.86–2.79)).
Unmet Dental Need and MI Conditions
Figure 1 shows the odds ratios of unmet dental need among adults with various MI conditions. Individuals with a mood disorder had greater odds of reporting unmet dental need (12.0 percent) than were those without a mood disorder (5.7 percent; OR=1.4, 95 percent CI=1.2-1.7).. A similar pattern emerged for individuals with anxiety disorders (12.5 percent) compared with individuals without anxiety disorders (5.9 percent; OR=1.81, 95 percent CI=1.43 -2.12). Individuals with dementia were significantly less likely to report unmet dental need (2.1 percent) than those without dementia (6.4 percent; OR=0.32, 95 percent CI=0.08-0.91). There were no statistically significant differences in unmet need between those with and without attention disorders, developmental disorders, disorders diagnosed in childhood, schizophrenia or other psychotic disorders, alcohol- or substance-related disorders. The same patterns were seen for those with an SMI.
Figure 1. Adjusted odds ratios* for unmet dental need by most frequently reported types of mental illness.
*Adjusted for age, gender, race/ethnicity, education, income, employment, presence of dental and medical insurance. T-bars indicate standard 95 percent confidence intervals.
DISCUSSION
In contrast to the available literature, US adults with and without MI reported similar rates of dental visits as well as similar rates of receiving only non-preventive care. This pattern was the same for those with an SMI that had substantial impact on their health and well being. This was true even when other factors that might impact dental visits, such as dental insurance, were controlled for in the analyses. The levels of utilization overall were consistent with estimates for the US population from other sources, suggesting that the utilization rates found in this study are valid.38
As hypothesized, individuals with MI were more likely to report unmet dental need than those without MI. This was also true for individuals with an SMI that had an impact on their overall health and well being. Unmet dental need may be driven by need for dental treatment, an excessive level of dental disease, or the failure of treatment to address the level of dental disease adequately. Individuals with MI may experience greater levels of disease due to poor oral care or medication side effects.19–21, 24 They may also be unable to seek or receive adequate care because of cost, lack of insurance, or unwillingness of dentists to provide them with care.22–23, 28–29
Unmet dental need was assessed using a combination of two items: the need to delay needed care or not being able to receive care that the individual or a dentist thought was necessary. It is not possible to tease apart the individual’s perceived need from what they have been told by a dental provider; thus, the true nature of unmet dental need is unclear. Nonetheless, individuals in this vulnerable population perceive greater unmet need for dental care. Adults with MI, as well as those with an SMI, consistently reported more unmet dental need regardless of whether they had a dental visit in 2007.
Mental illness was determined by participants reporting having experienced at least one MI condition at any time during 2007, and was then broken down further by type of MI condition(s) experienced. Individuals with a mood or anxiety disorder were significantly more likely to report unmet dental need, while participants with dementia or other amnestic disorders were significantly less likely to report unmet dental need. This may initially seem counterintuitive, as individuals with mood or anxiety disorders are often able to function well with the assistance of psychotherapy and/or pharmacotherapy. Meanwhile, those with dementia often require more intensive assistance in their daily functioning. This assistance, however, may include help scheduling and attending regular dental appointments, and may not be available to those who are functioning more highly with mood or anxiety disorders.
One limitation of this study is that the presence or absence of MI in the MEPS sample, as for other variables, relies on self-report or the report of a family member. It may not give a full picture of the severity of the illness or the limitations it imposes on a person’s level of functioning. Individuals with MI whose family members are aware of and reporting on their dental status may have more familial and social support than others with MI. Therefore, not accounting for the dental needs of those without family support may lead to underestimates of dental utilization and unmet dental need in adults with MI.
The current study provides a piece of the puzzle about the associations between MI, dental utilization, and unmet dental need. There are, however, additional factors that are likely to play a role in these associations that are not addressed in the MEPS and other similar nationally representative health surveys. The Behavioral Model for Vulnerable Populations,32 used to predict health behaviors in homeless39 and other populations, includes demographic variables such as those included in the current study (age, gender, education, income) as well as social and behavioral characteristics not currently available in MEPS. Among the variables identified in the model are social support, health beliefs, and competing needs, as well as community-level variables such as availability of health and social services. Research is needed to assess the impact of MI on an individual’s functioning and how MI affects health-seeking behavior, particularly in the presence of barriers to care such as low income and lack of dental insurance. Community-level variables, such as the availability of dental and other health resources, must also be examined in order to put individuals’ health behaviors and needs into context. Further, as the two-year window allowed in MEPS data may not be enough to examine clearly examine treatment outcomes within the dental setting, longitudinal studies are needed to gain a clearer picture about the impact of individual- and community-level factors on effectiveness of treatment.
Friedlander and colleagues have written concise reviews concerning of the identification and dental management of patients with various mood and anxiety disorders.3–8 Including questions on the health history about these MI conditions will help open communication between dentists and their patients about the patients’ needs. In addition, resources are currently being developed to help dental providers better understand and care for adults and children with MI.40 Careful review of the patient’s health history, including current use of psychotropic medications (i.e., medications used to treat depression, anxiety, and/or attention disorders) and treatment by a mental health professional, is critical to determine a patient’s particular needs.28
Similar to other populations with special health care needs, individuals with MI are considered by the Special Care Dentistry Association to require special treatment considerations.41 While diagnosing and treating MI conditions falls outside the scope of dental practice, direct communication with the patient and his or her family physician or mental health professional can identify potential problems (e.g., severe dental fear or mistrust of healthcare professionals) that could hamper effective dental treatment. Setting realistic expectations for treatment goals, length of treatment, and special considerations -- such as shortening the duration of individual appointments while increasing their frequency -- is key to addressing the increased dental needs in this vulnerable population.
CONCLUSION
The current study gives us a view of dental visits and unmet dental need in people with mental illness at a national level. Yet, as with many studies employing secondary data, questions still remain that are best answered with studies directed specifically towards the population of interest. Nevertheless, individuals with MI experience more dental disease than those without MI.14–18 The results of this study strongly suggest that current dental service use does not fully address the dental needs of mentally ill patients.
ACKNOWLEDGEMENTS
This study was supported by the National Institutes of Health/National Institute of Dental and Craniofacial Research Grants 5K23DE019202-03 and U54DE019346.
Contributor Information
Lisa J. Heaton, Acting Assistant Professor, Department of Oral Health Sciences University of Washington, Seattle, Washington.
Lloyd A. Mancl, Research Associate Professor, Departments of Oral Health Sciences, Biostatistics and Pediatric Dentistry University of Washington, Seattle, Washington.
David Grembowski, Professor, Departments of Oral Health Sciences and Health Services, University of Washington, Seattle, Washington.
Jason M. Armfield, Senior Research Fellow, Australian Research Centre for Population Oral Health University of Adelaide School of Dentistry, Adelaide, Australia.
Peter Milgrom, Professor, Departments of Oral Health Sciences and Health Services University of Washington, Seattle, Washington.
References
- 1.U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General—Executive Summary. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. text rev. Washington: American Psychiatric Assoc; 2000. Print. [Google Scholar]
- 3.Friedlander AH, Mahler ME. Major depressive disorder. Psychopathology, medical management and dental implications. JADA. 2001;132(5):629–638. doi: 10.14219/jada.archive.2001.0240. [DOI] [PubMed] [Google Scholar]
- 4.Friedlander AH, Friedlander IK, Marder SR. Bipolar I disorder: psychopathology, medical management and dental implications. JADA. 2002;133(9):1209–1217. doi: 10.14219/jada.archive.2002.0362. [DOI] [PubMed] [Google Scholar]
- 5.Friedlander AH, Yagiela JA, Mahler ME, Rubin R. The pathophysiology, medical management and dental implications of adult attention-deficit/hyperactivity disorder. JADA. 2007;138(4):475–482. doi: 10.14219/jada.archive.2007.0199. [DOI] [PubMed] [Google Scholar]
- 6.Friedlander AH, Friedlander IK, Marder SR. Posttraumatic stress disorder: psychopathology, medical management, and dental implications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(1):5–11. doi: 10.1016/j.tripleo.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Friedlander AH, Freymiller EG, Yagiela JA, Eth S. Dental management of the adolescent with panic disorder. ASDC J Dent Child. 1993;60(4):365–371. [PubMed] [Google Scholar]
- 8.Friedlander AH, Marder SR, Sung EC, Child JS. Panic disorder: psychopathology, medical management and dental implications. JADA. 2004;135(6):771–778. doi: 10.14219/jada.archive.2004.0306. [DOI] [PubMed] [Google Scholar]
- 9.Shippee ND, Shah ND, Williams MD, Moriarty JP, Frye MA, Ziegenfuss JY. Differences in demographic composition and in work, social, and functional limitations among the populations with unipolar depression and bipolar disorder: results from a nationally representative sample. Health Qual Life Outcomes. 2011;13(9):90. doi: 10.1186/1477-7525-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levinson D, Lakoma MD, Petukhova M, Schoenbaum M, Zaslavsky AM, Angermeyer M, Borges G, Bruffaerts R, de Girolamo G, de Graaf R, Gureje O, Haro JM, Hu C, Karam AN, Kawakami N, Lee S, Lepine JP, Browne MO, Okoliyski M, Posada-Villa J, Sagar R, Viana MC, Williams DR, Kessler RC. Associations of serious mental illness with earnings: results from the WHO World Mental Health surveys. Br J Psychiatry. 2010;197(2):114–121. doi: 10.1192/bjp.bp.109.073635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salsberry PJ, Chipps E, Kennedy C. Use of general medical services among Medicaid patients with severe and persistent mental illness. Psychiatr Serv. 2005;56(4):458–462. doi: 10.1176/appi.ps.56.4.458. [DOI] [PubMed] [Google Scholar]
- 12.Juul SH, Nemeroff CB. Psychiatric epidemiology. Handb Clin Neurol. 2012;106:167–189. doi: 10.1016/B978-0-444-52002-9.00010-3. [DOI] [PubMed] [Google Scholar]
- 13.Babu NC, Gomes AJ. Systemic manifestations of oral diseases. J Oral Maxillofac Pathol. 2011;15(2):144–147. doi: 10.4103/0973-029X.84477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rekha R, Hiremath SS, Bharath S. Oral health status and treatment requirements of hospitalized psychiatric patients in Bangalore city: a comparative study. J Indian Soc Pedod Prev Dent. 2002;20(2):63–67. [PubMed] [Google Scholar]
- 15.Hede B. Oral health in Danish hospitalized psychiatric patients. Community Dent Oral Epidemiol. 1995;23(1):44–88. doi: 10.1111/j.1600-0528.1995.tb00196.x. [DOI] [PubMed] [Google Scholar]
- 16.Rudolph MJ, Chikte UM. Dental caries experience and periodontal disease in institutionalised male psychiatric patients. J Dent Assoc S Afr. 1993;48(8):451–454. [PubMed] [Google Scholar]
- 17.Velasco E, Bullón P. Periodontal status and treatment needs among Spanish hospitalized psychiatric patients. Spec Care Dentist. 1999;19(6):254–258. doi: 10.1111/j.1754-4505.1999.tb01394.x. [DOI] [PubMed] [Google Scholar]
- 18.Syrjälä AM, Ylöstalo P, Sulkava R, Knuuttila M. Relationship between cognitive impairment and oral health: results of the Health 2000 Health Examination Survey in Finland. Acta Odontol Scand. 2007;65(2):103–108. doi: 10.1080/00016350601083521. [DOI] [PubMed] [Google Scholar]
- 19.de Vries MW, Peeters FP. Dental caries with long-term use of antidepressants. Lancet. 1995;16(346):1640. doi: 10.1016/s0140-6736(95)91980-5. [DOI] [PubMed] [Google Scholar]
- 20.Peeters FP, de Vries MW, Vissink A. Risks for oral health with the use of antidepressants. Gen Hosp Psychiatry. 1998;20(3):150–144. doi: 10.1016/s0163-8343(98)00017-6. [DOI] [PubMed] [Google Scholar]
- 21.Little JW. Dental implications of mood disorders. Gen Dent. 2004;52(5):442–450. [PubMed] [Google Scholar]
- 22.Moon ZK, Farmer FL, Tilford JM. Attenuation of racial differences in health service utilization patterns for previously uninsured children in the Delta. J Rural Health. 2005;21(4):288–294. doi: 10.1111/j.1748-0361.2005.tb00097.x. [DOI] [PubMed] [Google Scholar]
- 23.Manski RJ, Macek MD, Moeller JF. Private dental coverage: who has it and how does it influence dental visits and expenditures? JADA. 2002;133(11):1551–1159. doi: 10.14219/jada.archive.2002.0087. [DOI] [PubMed] [Google Scholar]
- 24.Cutler C. Assessing patients' perception of self-care agency in psychiatric care. Issues Ment Health Nurs. 2003;24(2):199–211. doi: 10.1080/01612840305300. [DOI] [PubMed] [Google Scholar]
- 25.Stiefel DJ, Truelove EL, Menard TW, Anderson VK, Doyle PE, Mandel LS. A comparison of the oral health of persons with and without chronic mental illness in community settings. Spec Care Dent. 1990;10(1):6–10. doi: 10.1111/j.1754-4505.1990.tb01079.x. [DOI] [PubMed] [Google Scholar]
- 26.Pohjola V, Mattila AK, Joukamaa M, Lahti S. Anxiety and depressive disorders and dental fear among adults in Finland. Eur J Oral Sci. 2011;119(1):55–60. doi: 10.1111/j.1600-0722.2010.00795.x. [DOI] [PubMed] [Google Scholar]
- 27.Locker D, Poulton R, Thomson WM. Psychological disorders and dental anxiety in a young adult population. Community Dent Oral Epidemiol. 2001;29(6):456–463. doi: 10.1034/j.1600-0528.2001.290607.x. [DOI] [PubMed] [Google Scholar]
- 28.Heaton LJ, Hyatt HA, Huggins KH, Milgrom P. United States dental professionals’ perceptions of dental anxiety and need for sedation in patients with mental illness. SAAD Digest. 2012;28:23–30. [PMC free article] [PubMed] [Google Scholar]
- 29.Janardhanan T, Cohen CI, Kim S, Rizvi BF. Dental care and associated factors among older adults with schizophrenia. JADA. 2011;142(1):57–65. doi: 10.14219/jada.archive.2011.0029. [DOI] [PubMed] [Google Scholar]
- 30.Pratt LA, Dey AN, Cohen AJ. Characteristics of adults with serious psychological distress as measured by the K6 Scale: United States-2001–2004. Adv Data. 2007;382:1–18. [PubMed] [Google Scholar]
- 31.Agency for Healthcare Research and Quality 2007. Medical Expenditure Panel Survey. Accessed at http://www.meps.ahrq.gov/mepsweb/ on June 7, 2012. [PubMed]
- 32.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 33.Baker SR. Applying Andersen's behavioural model to oral health: what are the contextual factors shaping perceived oral health outcomes? Community Dent Oral Epidemiol. 2009;37(6):485–494. doi: 10.1111/j.1600-0528.2009.00495.x. [DOI] [PubMed] [Google Scholar]
- 34.Iida H, Lewis C, Zhou C, Novak L, Grembowski D. Dental care needs, use and expenditures among U.S. children with and without special health care needs. JADA. 2010;141(1):79–88. doi: 10.14219/jada.archive.2010.0025. [DOI] [PubMed] [Google Scholar]
- 35.Agency for Healthcare Research and Quality (AHRQ) The Healthcare Cost and Utilization Project (HCUP) Clinical Classifications Software. Accessed at http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp on June 7, 2012. [PubMed] [Google Scholar]
- 36.Practice Management Information Corporation (PMIC) vols. 1,2,3. Published Los Angeles, CA: PMIC, C2005. Edition Hospital edition; ICD-9-CM: international classification of diseases, 9th revision; clinical modification, 6th edition, 2006. [Google Scholar]
- 37.U.S. Department of Health and Human Services. The 2007 HHS Poverty Guidelines. Accessed at http://aspe.hhs.gov/poverty/07poverty.shtml on February 24, 2012.
- 38.Vargas CM, Dye BA, Hayes KL. Oral health status of rural adults in the United States. JADA. 2002;133(12):1672–1681. doi: 10.14219/jada.archive.2002.0120. [DOI] [PubMed] [Google Scholar]
- 39.Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Andersen Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20–30. doi: 10.1037/a0023643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.University of Washington. Special needs fact sheets for providers and caregivers. Accessed at http://www.dental.washington.edu/departments/omed/decod/special_needs_facts.php on March 4, 2012.
- 41.American Academy on Pediatric Dentistry Council on Dental Benifits Programs/Council on Clinical Affairs. Policy on model dental benefits for infants, children, adolescents, and individuals with special health care needs. Pediatr Dent. 2008–2009;30(7 Suppl):71–73. [PubMed] [Google Scholar]