Abstract
Objective
Previous research has found a longitudinal relationship between sleep problems and suicidal behavior while controlling for depression and other important covariates in a high risk sample of adolescents and controls. In this paper, we replicated this longitudinal relationship in a national sample and examined whether the relationship was partially mediated by depression, alcohol-related problems and other drug use.
Methods
Study participants were 6504 adolescents from the National Longitudinal Study of Adolescent Health (ADD HEALTH).
Results
In bivariate analyses, sleep problems (i.e., having trouble falling asleep or staying asleep) at Wave 1 were associated with suicidal thoughts and suicide attempts at Waves 1, 2, and 3 (W1, 2 and 3). In multivariate analyses, controlling for depression, alcohol problems, illicit drug use, and important covariates such as gender, age, and chronic health problems, sleep problems at a previous wave predicted suicidal thoughts and suicide attempts at a subsequent wave. In mediation analyses, W2 depression significantly mediated the effect of W1 sleep problems on W3 suicide thoughts. Moreover, W2 suicidal thoughts also significantly mediated the effect of W1 sleep problems on W3 suicidal attempts.
Conclusions
Sleep problems appear to be a robust predictor of subsequent suicidal thoughts and attempts in adolescence and young adulthood. Having trouble falling sleeping or staying asleep had both direct and indirect effects (via depression and suicidal thoughts) on suicidal behavior. Future research could determine if early intervention with sleep disturbances reduces the risk for suicidality in adolescents and young adults.
Keywords: Sleep problems, Suicidal thoughts, Suicide attempts, Adolescence
1. Introduction
Suicide is the third leading cause of death in the 15–24 year-old age group (Cash and Bridge, 2009). Sleep disturbances appear to be a robust risk factor for suicidality. A consistent and strong association between sleep disturbances and suicidality has been reported in both adults (Agargun et al., 2007; Fawcett et al., 1990; Sjostrom et al., 2007) and adolescents (Bailly et al., 2004; Goldstein et al., 2008; Nrugham et al., 2008).
In clinical samples of adults, insomnia was associated with suicidal attempts in patients with a major affective disorder (Fawcett et al., 1990) and depressed outpatients (Agargun et al., 2007). Moreover, those who were diagnosed with a sleep disorder had a significantly higher risk of death due to suicide (Wallander et al., 2007). Sleep disturbances and nightmares were common among suicide attempters (Sjostrom etal., 2007). In community and population samples, the association between sleep problems and suicidality was also reported. In a community study of older adults, poor sleep quality was predictive of completed suicides (Turvey et al., 2002). In the National Comorbidity Survey Replication Study, a nationally representative population study in the U.S., the presence of any sleep problems (i.e., difficulty initiating sleep, difficulty maintaining sleep, and early morning awakening) was significantly associated with concurrent suicidal thoughts, planning, and suicide attempts (Wojnar et al., 2009).
Among adolescents, sleep problems has been linked to suicidal thoughts (Bailly et al., 2004; Barbe et al., 2005; Choquet and Menke, 1990), suicidal attempts (Bailly et al., 2004; Nrugham et al., 2008), and completed suicides (Goldstein et al., 2008). Similarly, nightmares have been linked to both suicidal thoughts (Choquet et al., 1990; Liu, 2004) and attempts (Liu, 2004). These relationships have been found in both general populations (Liu, 2004; Nrugham et al., 2008) and clinical samples (Barbe et al., 2005). However, most of the existing studies were cross-sectional in design. Very few studies have examined the relationship between sleep disturbances and longitudinally, thus limiting our ability to understand the nature of their relationship. Moreover, many studies did not control for depressive symptoms when assessing the relationship between sleep problems and suicidality. As sleep problems are common among depressed individuals and depression is an important risk factor for suicidal behavior (Kessler et al., 1999; Pena et al., 2012), it is unclear whether the association between sleep problems and suicidal behavior may be due to depression.
To our knowledge, there were three prospective studies examining the relationships between sleep problems and suicidality in adolescence. In one study, 26515-year-old students in Norway were studied for a period of five years (Nrugham et al., 2008). Bivariate analyses showed that sleep problems at age 15 predicted suicide attempts between ages 15–20. However, in multivariate analyses, controlling for baseline suicidal thoughts and depressive symptoms, sleep problems did not significantly predict suicide attempts. The authors cautioned that a 70% follow-up rate and a small number of boys (N = 61) in the sample might have biased the results. Yet these findings underscore the importance of controlling for depressive symptoms when examining the relationship between sleep problems and suicidal behavior, as the association between depression and suicide attempts in adolescents is well-established (Kovacs et al., 1993; Lewinsohn et al., 1994).
Another prospective study reported a longitudinal relationship between sleep problems and suicidal behavior in a community sample of children of alcoholics and controls (N = 392; 280 boys, 112 girls; (Wong et al., 2010b)). Controlling for gender, parental alcoholism, parental suicidal thoughts, depressive symptoms, nightmares, aggressive behaviors, substance-related problems, as well as suicidal thoughts and self-harm behaviors at ages 12–14, having trouble sleeping at ages 12–14 significantly predicted suicidal thoughts and self-harm behaviors at ages 15–17. Children of alcoholics did not differ from controls on rates of sleep problems or suicidal behavior. When compared to the Nrguham et al. study, this study has a higher percentage of boys than girls and a higher follow-up rate (approximately 85%).
A third prospective study reported data from the National Longitudinal Study of Adolescent Health (ADD HEALTH) (Roane and Taylor, 2008). Adolescent insomnia symptoms were associated with concurrent report of suicide thoughts and attempts. Moreover, insomnia symptoms also prospectively predicted suicide thoughts and attempts at a subsequent wave. In the longitudinal analyses, adolescents who reported depression, suicide thoughts or attempts at a previous wave were excluded from the analyses. Thus, the longitudinal results suggested that insomnia symptoms predicted a new incidence of suicidal thoughts and suicide attempts. However, the analyses did not statistically control for important covariates such as substance use, even though data in the study suggested that sleep problems prospectively predicted alcohol, cannabis, and other drug use. Previous epidemiological research showed a consistent relationship between substance use disorder and suicidal behavior (Borges et al., 2000; Kessler et al., 1999; Wilcox et al., 2004). Moreover, the study excluded cases reporting depression based on one item, i.e., participants who marked often or every day to the question “How often have they felt depressed in the last week?” Excluding these cases based on one item is not equivalent to statistically controlling for the effect of depressive symptoms, as the study has 18 items on depression (Harris et al., 2009).
The prospective studies discussed above highlight the importance of sleep problems as a risk factor of suicidal behavior, even after controlling for other important correlates. At least two issues, however, remain to be addressed. First, with the exception of the study by Roane & Taylor (Roane et al., 2008), the existing longitudinal data on sleep problems and suicidal behavior focus on relatively small samples of adolescents. Studies on bigger samples are necessary to replicate previous findings. Second, the Roane and Taylor (2008) study did not statistically control for the effect of substance use, depressive symptoms, and other important covariates (e.g., chronic health problems that may affect sleep) in the analyses. Moreover, the study only analyzed data from two waves (Waves 1 and 3).
The current study extends past findings in two ways. First, we examined the relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescence (ADD Health) across three waves, while controlling for the effects of important covariates including depression and substance use. Second, we examined whether the longitudinal relationship between sleep problems and suicidal behavior were mediated (explained) by three well known risk factors of suicidal behavior, i.e., depression, alcohol-related problems, and use of illicit drugs (Kessler et al., 1999; Pena et al., 2012).
2. Methods
2.1. Participants
Participants in the study were 6504 adolescents and young adults who were in the publicly accessible database of the National Longitudinal Study of Adolescent Health (ADD HEALTH; (Harris et al., 2009)). ADD HEALTH is a nationally representative sample of U.S. adolescents. It is the largest study on adolescents conducted in the U.S. The study was designed to examine health-related behaviors, social contexts, and health-related outcomes in adolescents and young adults. The publicly accessible database included one-half of the core sample who completed an in-home interview and an oversample of African-American adolescents who had a parent with a college degree. Wave 1 of data collection took part in 1994–1995 (mean age = 15.99 years, SD = 1.75). Wave 2 occurred one year later, in 1996 (mean age = 16.02 years, SD = 1.62). Wave 3 took part five years after Wave 2, in 2001–2002 (mean age = 21.82 years, SD = 1.81) (Harris et al., 2009). Informed consent was obtained from the participants and their parents. This secondary data analysis project was approved by the Institution Review Board at Idaho State University.
2.2. Measures
This study analyzed data on sleep problems, suicidal behavior, and important covariates (e.g., depression, substance use) from Waves 1, 2, and 3 (W1, W2, and W3). Demographics characteristics (e.g., age, gender) were obtained by an in-school questionnaire at W1. Data on sleep problems, suicidal behavior, depression, substance use, and physical health status of all three waves were obtained by in-home interviews using a laptop computer. For less sensitive topics, the interviewer read the questions aloud and entered the participants' answers on the computer. For more sensitive topics, participants listened to pre-recorded questions over earphones and answered the questions directly on the computer.
Sleep problems was measured by one question, “Please tell me how often you have had each of the following conditions in the past 12 months? – trouble falling asleep or staying asleep” Responses were given on a rating scale, 1 = a few times, 2 = once a week, 3 = almost every day, 4 = every day. Suicidal thoughts were measured by the following question, “During the past 12 months, did you ever seriously think about committing suicide?” (0 = no, 1 = yes). Suicide attempt status were measured by one question, “During the past 12 months, how many times did you actually attempt suicide?” Responses were recoded to a dichotomous response: 0 = no attempt, 1 = one or more attempts.
Covariates that may be associated with sleep problems or suicidal behavior were controlled for in the analyses. Depressive symptoms were measured by the 18-item version of the Center for Epidemiologic Study-Depression Scale (CES-D). This version of CES-D is a valid instrument for both junior-high and high school students (Radloff, 1991). To avoid overlap between depressive symptoms and sleep problems, we obtain the sum of all CES-D items except one sleep item. Information on alcohol-related problems was obtained by five questions from the substance use section. Subjects were asked to indicate whether and how often they had the following problems over the last 12 months due to their drinking, i.e., got into trouble with parents, had problems at school or with school work, had problems with friends, had problems with someone they were dating, and got into a physical fight. They were asked to select one of the five choices, “never,” “once,” “twice,” “3–4 times,” or “5 or more times.” Data on all five questions were later recoded into a dichotomous variable, alcohol-related problem (0 = no; 1 = yes). Data on lifetime illicit drug use (0 = no; 1 = yes) were obtained from four questions from the substance use section – “During your life, how many times have you used marijuana?” The same question was used to obtain information on other drugs by substituting the word marijuana with three other drugs, i.e., cocaine, inhalants, or other kinds of illegal drugs (e.g., LSD, speed, and heroin). Lastly, demographics variables including gender (1 = male, 2 = female), age, race (0 = non-Caucasian, 1 = Caucasian), parents' poverty (0 = did not receive public assistance, 1 = received public assistance) and chronic health problems including allergies, asthma, migraines, diabetes or obesity (0 = no; 1 = yes) were statistically controlled for.
2.3. Analytic plan
In order to examine the longitudinal relationships between sleep problems and suicidal behavior, we first examined the concurrent relationship between sleep problems and suicidal behavior at each wave using chi-square analyses and bivariate logistic regression models. Next we tested the longitudinal relationships between sleep problems and suicidal behavior. Multivariate logistic regression models were used to predict suicidal thoughts and suicide attempts at W2 and 3. Sleep problems at a previous wave was the primary predictor of interest. For instance, if the outcome was suicidal thoughts at W2, sleep problems at W1 was used as a predictor. If the outcome was suicidal thoughts at W3, sleep problems at W2 was used as a predictor. Other predictors included suicidal thoughts or suicidal attempts, depressive symptoms, alcohol-related problems, and illicit drug use at a previous wave. Additionally, gender, age, ethnicity, school grade, poverty and chronic health problems were used in the analyses as statistical controls.
In order to find out whether W2 depression, alcohol-related problems and illicit drug use mediated (explained) the longitudinal relationship between W1 sleep problems and W3 suicidal behavior, we conducted mediation analyses using the product of coefficient approach (MacKinnon, 2008; MacKinnon et al., 2002). We first tested the mediated effect by the traditional Sobel Z statistic (Sobel, 1982). This statistic tested whether the coefficient αβ/Sαβ is significantly different from zero by comparing the coefficient to critical cut off values of a z-distribution (i.e., ±1.96 for p < .05); α′s are the effects of W1 sleep problems on the W2 mediators and β′s are the effects of W2 mediators on W3 suicidal thoughts and attempts; Sαβ is the standard error of αβ. However, as αβ is often not normally distributed, the Sobel Z statistic often has a small Type 1 error and low statistical power (MacKinnon et al., 2002). We therefore used a second method to test for mediation. The asymmetric confidence interval (CI) of αβ has an accurate Type 1 error and higher statistical power than the Sobel Z statistic (MacKinnon, 2008). The method tested whether the 95% asymmetric CI of αβ includes 0 (H0: αβ = 0) by using the PRODLIN program (MacKinnon et al., 2007). The mediator is considered significant at p < .05 if the 95% CI of αβ does not include 0.
Two sets of mediation analyses were done, one for W3 suicidal thoughts and one for W3 suicidal attempts. In each set of analyses, we first examined whether W1 sleep problems predicted W2 mediators (e.g., W2 depression) in separate logistic and multiple regression models. Logistic regression models were used to analyze whether sleep problems predicted dichotomous mediators such as alcohol-related problems and illicit drug use. Multiple regression models were used to analyze whether sleep problems predicted the continuous mediator, i.e., depression. W1 data for the mediators (e.g., W1 depression) and demographic covariates were controlled for in these analyses. We then examined whether W1 sleep problems and W2 mediators predicted W3 suicidal behavior while controlling for demographic covariates in logistic regression models.
3. Results
3.1. Concurrent relationships between sleep problems and suicidality
We first examined the concurrent relationship between sleep problems and suicidality at each wave. Having trouble falling asleep or staying asleep every day or almost every day in the last twelve months was significantly associated with suicidal thoughts and suicide attempts at W1, 2, and 3 (Table 1). Those who had sleep problems every day or almost every day in the last twelve months were approximately 2–3 times more likely to have suicidal thoughts (W1: Odds Ratio (OR) = 2.90, p < .001; W2: OR = 2.09, p < .001; W3: OR = 1.95, p < .01) and approximately 2–4 times more likely to have made suicide attempts (W1: OR = 3.95, p < .001; W2: OR = 2.30, p < .001; W3: OR = 1.99, p < .05).
Table 1.
The relationship between sleep problems and suicidality in the National Longitudinal Study of Adolescent Health.
| Wave 1 | Wave 2 | Wave 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||
| Thoughts | Attempts | Thoughts | Attempts | Thoughts | Attempts | ||||||||
| Trouble falling asleep (T1) | N | % | N | % | N | % | N | % | N | % | N | % | |
| No (N = 5875) | 657/5826 | 11.3 | 166/5871 | 2.8 | 434/4326 | 10.0 | 155/4357 | 3.6 | 254/4297 | 5.9 | 58/4413 | 1.3 | |
| Yes (N = 621)a | 164/609 | 26.9 | 64/621 | 10.3 | 89/471 | 18.9 | 37/473 | 7.8 | 49/450 | 10.9 | 12/464 | 2.6 | |
| χ2 | p-value | 121.36 | .000 | 91.91 | .000 | 34.35 | .000 | 20.33 | .000 | 16.890 | .000 | 4.80 | .023 |
| Odds ratio | 95% CI | 2.9 | 2.38–3.53 | 3.95 | 2.92–5.34 | 2.09 | 1.63–2.69 | 2.30 | 1.59–3.34 | 1.95 | 1.41–2.69 | 1.99 | 1.06–3.74 |
Note: All chi-square tests and logistic regression models are significant at p < .05.
Trouble falling asleep or staying asleep in the last twelve months every day or almost every day.
3.2. Longitudinal relationships between sleep problems and suicidality
Next we examined whether sleep problems at a previous wave prospectively predicted suicidal thoughts and attempts at the next wave in logistic regression models. The results are presented in Table 2.
Table 2.
The longitudinal relationship between sleep problems and suicidality in the National Longitudinal Study of Adolescent Health.
| Thoughts | Attempts | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Wald χ2 | Odds ratio | 95% CI | Wald χ2 | Odds ratio | 95% CI | |
| Wave 2 | ||||||
| Gender | 39.85 | 2.03*** | 1.63–2.53 | 27.28 | 2.69*** | 1.86–3.90 |
| Age | 1.33 | 1.09 | .94–1.26 | 1.17 | 1.13 | .90–1.43 |
| Race-ethnicity | 2.91 | 1.23 | .97–1.57 | .19 | .92 | .64–1.33 |
| Education | 7.89 | .80* | .68–.93 | 9.32 | .68** | .53–.87 |
| Poverty status | .61 | .88 | .63–1.22 | 1.94 | .66 | .37–1.18 |
| Chronic health conditions | 2.25 | 1.17 | .95–1.45 | .90 | 1.17 | .84–1.63 |
| Alcohol problems (previous wave) | 11.92 | 1.62*** | 1.23–2.13 | 12.74 | 2.07*** | 1.39–3.09 |
| Drug use (previous wave) | 33.19 | 1.98*** | 1.57–2.50 | 23.06 | 2.44*** | 1.70–3.51 |
| Depression (previous wave) | 34.26 | 1.06*** | 1.04–1.09 | 29.12 | 1.08*** | 1.05–1.12 |
| Sleep problems (previous wave) | 14.57 | 1.20*** | 1.09–1.32 | 7.79 | 1.22** | 1.06–1.41 |
| Wave 3 | ||||||
| Gender | 2.23 | .80 | .60–1.07 | 1.97 | 1.55 | .84–2.87 |
| Age | 2.59 | .84 | .69–1.04 | .24 | .90 | .60–1.36 |
| Race-ethnicity | 4.23 | 1.43* | 1.02–2.0 | 1.73 | .67 | .37–1.22 |
| Education | .36 | .93 | .75–1.17 | .76 | .82 | .52–1.28 |
| Poverty status | .10 | .93 | .60–1.45 | .04 | 1.07 | .52–2.20 |
| Chronic health conditions | 2.55 | 1.27 | .95–1.69 | .20 | 1.14 | .64–2.02 |
| Alcohol problems (previous wave) | .05 | .95 | .63–1.44 | .44 | .73 | .29–1.84 |
| Drug use (previous wave) | 3.11 | 1.35 | .97–1.88 | 1.12 | 1.43 | .74–2.78 |
| Depression (previous wave) | 18.59 | 1.07*** | 1.04–1.10 | 2.09 | 1.04 | .99–1.11 |
| Sleep problems (previous wave) | 7.77 | 1.23** | 1.06–1.43 | .04 | 1.03 | .76–1.40 |
Note. p < .05,
p < .01,
p < .001.
3.2.1. Wave 2 suicidal thoughts and attempts
Controlling for W1 suicidal thoughts, depressive symptoms, alcohol-related problems, and drug use, and demographics covariates, W1 sleep problems significantly predicted W2 suicidal thoughts. As sleep problems at W1 increased by one unit, adolescents were 20% more likely to report having suicidal thoughts at W2 (OR = 1.20, p < .001). Additionally, adolescents who were depressed, reported alcohol-related problems, and used illicit drugs at W1 were more likely to report suicidal thoughts at W2. Moreover, girls and those who were in lower grade were more likely to report suicidal thoughts at W2.
Controlling for W1 suicidal attempt status, depressive symptoms, alcohol-related problems, illicit drug use, and other demographic covariates, W1 sleep problems had a significant relationship with W2 suicide attempts. As sleep problems at W1 increased by one unit, the odds of having one or more suicide attempts at W2 increased by 22% (OR = 1.22, p < .01). Adolescents who had depressive symptoms, reported alcohol-related problems, and used illicit drugs at W1 were also more likely than their counterparts to report suicidal attempts at W2. Girls were more likely than boys to have attempted suicides. Adolescents in lower grades were more likely than those in higher grades to report one or more suicide attempts.
3.2.2. Wave 3 suicidal thoughts and attempts
Controlling for W2 suicidal thoughts and demographic covariates, W2 sleep problems again significantly predicted W3 suicidal thoughts. As sleep problems increased by one unit, the odds of reporting suicidal thoughts at W3 increased by 23% (OR = 1.23, p < .01). Adolescents who were depressed at W2 were also more likely to report suicidal thoughts at W3.
Controlling for W2 suicidal attempt status and covariates, W2 sleep problems had no significant relationship with W3 suicide attempt status. None of the covariates were significant predictors. To understand more about W2 variables and W3 suicide attempt status, we performed post hoc analyses adding W2 suicidal thoughts to the logistic regression model. W2 suicidal thoughts significantly predicted the risk of reporting a suicide attempt at W3 (OR = 3.53, p < .05). The odds of reporting a suicide attempt at W3 were three and a half times higher among those who had suicidal thoughts at W2 compared to those without suicidal thoughts.
3.3. Indirect effect of sleep problems and suicidality via depression, alcohol-related problems, and illicit drug use
The above results showed that depression, alcohol-related problems, and illicit drug use predicted both suicidal thoughts and suicide attempts. Here we examined whether sleep problems had an indirect effect on suicide thoughts and attempts via these three variables.
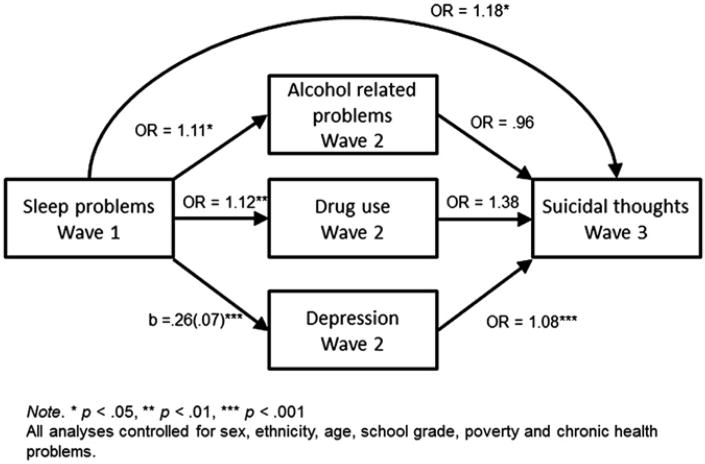
As shown in Fig. 1, W1 sleep problems directly predicted W3 suicidal thoughts. Additionally, W1 sleep problems also significantly predicted W2 depression, which significantly predicted W3 suicidal thoughts. This indirect effect was statistically significant (Sobel Z = 2.86, p < .01; 99% asymmetric CI = .01–.04, p < .01). W1 sleep problems also predicted W2 alcohol-related problems and illicit drug use. However, controlling for other variables in the model, alcohol-related problems and illicit drug use were not related to W3 suicidal thoughts.
Fig. 1.
Sleep problems as a longitudinal risk factor for suicidal thoughts.
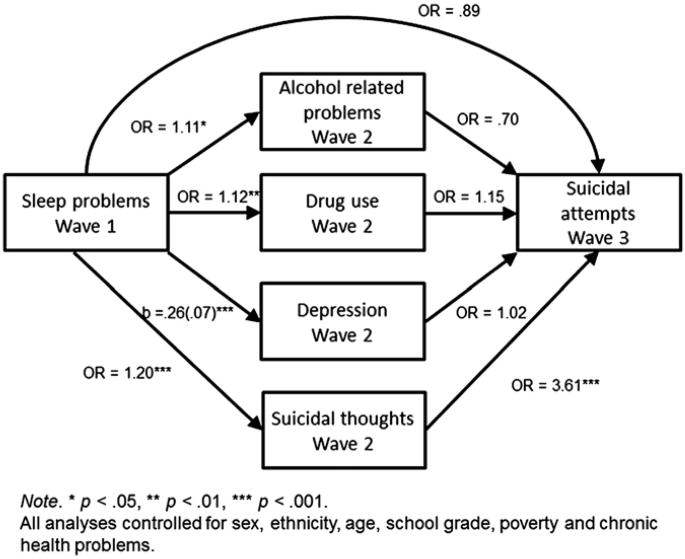
In the analyses on W3 suicide attempt status, W2 suicidal thoughts were included in the model as a predictor. Post hoc analyses in the above section found that it significantly predicted the outcome. W1 sleep problems predicted W2 suicidal thoughts, which in turn predicted W3 suicide attempt status. The indirect effect of sleep problems on suicide attempts at W3 was significant (Sobel Z = 2.65, p < .01; 99% asymmetric CI = .05–.51, p < .01). No other variable significantly predicted the odds of reporting suicidal attempt at W3 (Fig. 2).
Fig. 2.
Sleep problems as a longitudinal risk factor for suicide attempts.
To understand more about the relationships between sleep problems and the three mediators, we conducted additional analyses examining whether sleep problems predicted changes in mediators over time. We used sleep problems at a previous wave to predict depression, alcohol-related problems, and illicit drug use at a subsequent wave. In each set of analyses, we controlled for the scores of these three variables in the previous wave. So essentially, we examined whether sleep problems predicted changes of depression, alcohol-related problems and illicit drug use across waves. As shown in Table 3, sleep problems longitudinally predicted changes in all three variables in both W2 and W3.
Table 3.
Sleep problems as a longitudinal risk factor for alcohol problems, drug use, and depression.
| Alcohol-related problems | Illicit drug use | Depression | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| Wald χ2 | Odds ratio | 95% CI | Wald χ2 | Odds ratio | 95% CI | B | se | |
| Wave 2 | ||||||||
| Gender | .08 | 1.03 | .85–1.24 | 1.23 | 1.10 | .93–1.30 | 1.05*** | .13 |
| Age | .31 | 1.04 | .91–1.18 | .66 | .95 | .85–1.07 | .16 | .09 |
| Race-ethnicity | 7.70 | 1.37** | 1.10–1.69 | .29 | .96 | .79–1.14 | −.34* | .15 |
| Education | 2.42 | 1.12 | .97–1.29 | 1.28 | 1.08 | .95–1.22 | −.05 | .10 |
| Poverty status | .20 | .94 | .71–1.24 | .23 | .95 | .75–1.19 | .33 | .18 |
| Chronic health conditions | .40 | .94 | .78–1.13 | .39 | 1.06 | .89–1.25 | .15 | .13 |
| Alcohol problems (previous wave) | 350.48 | 7.09*** | 5.77–8.70 | – | – | – | – | – |
| Drug use (previous wave) | – | – | – | 861.12 | 13.15*** | 11.01–15.61 | – | – |
| Depression (previous wave) | – | – | – | – | – | – | .38*** | .01 |
| Sleep problems (previous wave) | 5.95 | 1.11* | 1.02–1.22 | 7.46 | 1.12** | 1.03–1.21 | .26*** | .07 |
| Wave 3 | ||||||||
| Gender | 58.29 | .49*** | .41–.59 | 48.08 | .58*** | .50–.68 | .34*** | .08 |
| Age | 3.68 | .88 | .78–1.00 | 17.67 | .79*** | .71–.88 | −.03 | .06 |
| Race-ethnicity | 23.60 | 1.71*** | 1.38–2.12 | 29.77 | 1.63*** | 1.37–1.94 | −.01 | .09 |
| Education | 1.24 | 1.08 | .94–1.24 | 2.01 | 1.09 | .97–1.23 | −.07 | .06 |
| Poverty status | .84 | .87 | .65–1.17 | 2.58 | .82 | .64–1.05 | .02 | .11 |
| Chronic health conditions | 1.49 | .90 | .75–1.07 | .46 | .95 | .82–1.11 | .03 | .08 |
| Alcohol problems (previous wave) | 61.08 | 2.41*** | 1.93–3.00 | – | – | – | – | – |
| Drug use (previous wave) | – | – | – | 202.09 | 3.46*** | 2.92–4.12 | – | – |
| Depression (previous wave) | – | – | – | – | – | – | .12*** | .01 |
| Sleep problems (previous wave) | 5.76 | 1.12* | 1.02–1.23 | 2.86 | 1.07 | .99–1.16 | .14*** | .05 |
Note. p < .05, p < .01, p < .001.
Note. p < .05,
p < .01,
p < .001.
4. Discussion
In a nationally representative sample of adolescents, we found that sleep problems at a previous wave significantly predicted suicidality at a subsequent wave, while controlling for depression, alcohol-related problems, illicit drug use, and a number of demographic covariates. Specifically, W1 sleep problems predicted W2 suicidal thoughts and suicide attempts. Similarly, W2 sleep problems also predicted W3 suicide thoughts. However, W2 sleep problems had no direct effect on W3 suicide attempts. W1 sleep problems had both direct and indirect effects (via W2 depression) on W3 suicidal thoughts. Moreover, W1 sleep problems had an indirect effect (via W2 suicidal thoughts) on W3 suicidal attempts. To our knowledge, this is the first prospective study showing such a relationship in a nationally representative sample. Past longitudinal studies reported findings from relatively small samples or did not adequately control for important covariates such as depression and substance use.
Generally, the relationships between W1 predictors and W2 outcomes are stronger than the relationships between W2 predictors and W3 outcomes. For instance, no W2 predictors (other than W2 suicide thoughts) predicted W3 suicide attempts. This could be due to the longer time lapse between W2 and W3 than between W1 and W2. W1 and W2 is one year apart from one another, whereas W2 and W3 are five years apart. Nevertheless, in most of our analyses, sleep problems at a previous wave was either a direct or indirect predictor (via depression, suicide thoughts) of subsequent suicidal behavior. Moreover, sleep problems longitudinally predicted changes in alcohol-related problems, illicit drug use, and depression. Our results showed that W2 depression was the only significant mediator of the relationship between W1 sleep problems and W3 suicidal thoughts. However, as alcohol-related problems and illicit drug use are well known risk factors for suicidal behavior (Kessler et al., 1999; Pena et al., 2012), sleep problems may increase the risk of suicidal behavior via these two variables later in life (i.e., beyond W3).
Taken as a whole, results from this study and past research indicate that sleep problems is an important risk factor for suicidal thoughts and suicide attempts in adolescence. National data have indicated that sleep problems and sleep deprivation are prevalent among adolescents. In a recent national study, 51% of 6th–12th graders reported feeling tired or sleepy and 31% reported having difficulty staying asleep at night at least once in week in the last two weeks (National Sleep Foundation, 2006). The active use of technology (e.g., computer with 24/7 internet access, cellular phone, video games) also have a significant impact on sleep in this age group. One study showed that among adolescents between the age of 13–18, 55% surfed the web every night or almost every night during the hour before going to bed and 56% sent or received text messages every night or almost every night before sleeping (National Sleep Foundation, 2011). The same study also found that one in five adolescents was “sleepy” during the day and about one third (30%) said they drove while drowsy at least once in the past month.
Given the prevalence of sleep problems and sleep deprivation, prevention programs for adolescent suicide could include discussions of the importance of sleep, sleep hygiene, and the management of sleep problems and other sleep problems. The potential effect of technology use before bedtime on sleep and alertness is also an important topic of discussion. The frequent and habitual use of technology with “interactive” properties (e.g., computer use, video games, texting) may have both short- and long-term consequences on sleep and changes of circadian rhythms. The effectiveness of including sleep-related issues in adolescent suicide prevention programs is a topic for future research.
This study also has several clinical implications. The relationship between sleep disturbances and suicidal behavior underscores the importance of assessing sleep problems among adolescents who are at risk for suicide. An assessment of sleep disturbances should be included in the evaluation of suicidal risk, regardless of whether the adolescent has any prior history of psychiatric problems that may cause sleep problems. Adolescents may be more willing to discuss issues related to sleep than more sensitive topics such as depression and substance use. Sleep problems in these patients should be treated and such treatment may have a positive effect on the prevention of suicidal behavior. Future research could determine if early intervention with sleep disturbances reduces the risk for suicidality in adolescents.
The longitudinal relationship between sleep problems and suicidal behavior does not explain why this relationship exists. Recent research found that sleep problems may negatively affect mood and inhibitory processes, which may increase the risk of suicidal behavior. A meta-analytic study found that sleep deprivation had the greatest negative effect on mood, followed by cognitive tasks and motor tasks (Pilcher and Huffcutt, 1996). Participants in one study reported less positive affect, experience more anxiety in a catastrophizing task, and rated the likelihood of potential catastrophes as higher when sleep deprived, compared to when rested (Talbot et al., 2010). A fMRI study found that that a lack of sleep inappropriately modulates the brain response to emotionally aversive stimuli (Yoo et al., 2007). Longitudinal studies have found that childhood sleep problems predicted depression and anxiety disorders in adolescence (Ong et al., 2006) and adulthood (Gregory et al., 2005). Thus, negative mood and depression may partially mediate the effects of sleep problems on suicidal behavior, which is consistent with past research on adolescent suicidality (Nrugham et al., 2008) and the results of this study. More longitudinal research on the relationships among sleep problems, mood regulation, and suicidal behavior is necessary to understand how these variables reciprocally affect one another over time. A current review of studies on sleep problems and emotions indicate that they might have a bidirectional relationship – while heightened emotional arousal might contribute to the maintenance of sleep problems, dysfunction in the sleep–wake regulating neural circuitries might also reinforce emotional disturbances (Baglioni et al., 2010).
Existing studies also indicate that sleep deprivation adversely affects inhibition or processes related to inhibition among adults (Chuah et al., 2006; Harrison and Horne, 2000; Tsai et al., 2005). Among children, sleep deprivation negatively affected (Randazzo et al., 1998) and sleep extension positively affected (Sadeh et al., 2003) executive function tasks, i.e., tasks that require sustained attention and inhibitory processes. Finally, overtiredness in childhood predicted lower response inhibition in adolescence (Wong et al., 2010a). Sleep problems may have a negative impact on inhibition and impulse control, which may increase the risk of suicidal behavior. Future research could examine how sleep problems and deprivation affect inhibitory processes and impulse control and whether such relationships increase the risk for suicidality among adolescents.
This study has several limitations. First, all measures were based on self-report which are subject to response and recall bias. No objective measures of sleep such as polysomnography or actigraphy were included. No information about individual sleep schedules or neurobiological parameters (e.g., structural and functional brain abnormalities) were analyzed in the study. Future studies need to include both subjective and objective assessment of sleep problems. Second, suicidal behavior and sleep problems were measured by single items. Although these items have face validity, the reliability of these measures is unknown. Future studies should use multiple items to measure these variables and estimate measurement error by doing latent variable analyses. Third, responses to the suicide items were recoded dichotomously. These items provided limited information on the underlying psychic states and psychological processes associated with suicidal thoughts and suicide attempts. Including other suicide items (e.g., severity of intent, frequency of attempts) could potentially reveal a more complex relationship between sleep problems and suicidal behavior. Fourth, other important predictors of adolescent suicidality (e.g., impulsivity, sexual abuse, physical abuse) were not included in the analyses. It was impossible to include these variables in the longitudinal analyses as they were measured only once. These variables should be included in future research. Fifth, a wide range of psychiatric disorders were not assessed. Most psychiatric disorders were associated with sleep difficulties or irregularities. The relationships between sleep problems and suicidal behavior reported in this paper could be due to the presence of psychiatric disorders (e.g., bipolar disorders, anxiety disorders). Future studies need to assess and statistically control for the presence of psychiatric disorders, especially those that are highly comorbid with sleep disorders and suicidal behavior.
In summary, among a nationally representative sample of adolescents, controlling for depression, alcohol problems, illicit drug use, and important covariates such as gender, age, and chronic health problems, sleep problems at a previous wave predicted suicidal thoughts (W2 and W3) as well as suicide attempts (W2) at a subsequent wave. Moreover, sleep problems longitudinally predicted depression, which significantly mediated the effect of sleep problems on suicidal thoughts.
Acknowledgments
This research uses data from ADD Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the ADD Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Role of funding source: This research was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism to M. M. Wong (R21 AA016851) and K. J. Brower (K24 AA00304).
The NIAAA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Contributors: Drs. Brower and Wong managed the literature searches. Drs. Brower and Wong wrote the manuscript. Dr. Wong conducted all the statistical analyses for the study. She also made all the tables and figures for the study.
Conflict of interest: The two authors have no conflict of interests.
References
- Agargun MY, Besiroglu L, Cilli AS, Gulec M, Aydin A, Inci R, et al. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. Journal of Affective Disorders. 2007;98:267–70. doi: 10.1016/j.jad.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Medicine Reviews. 2010;14:227–38. doi: 10.1016/j.smrv.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Bailly D, Bailly-Lambin I, Querleu D, Beuscart R, Collinet C. Sleep in adolescents and its disorders. A survey in schools Encephale. 2004;30:352–9. doi: 10.1016/s0013-7006(04)95447-4. [DOI] [PubMed] [Google Scholar]
- Barbe RP, Williamson DE, Bridge JA, Birmaher B, Dahl RE, Axelson DA, et al. Clinical differences between suicidal and nonsuicidal depressed children and adolescents. Journal of Clinical Psychiatry. 2005;66:492–8. doi: 10.4088/jcp.v66n0412. [DOI] [PubMed] [Google Scholar]
- Borges G, Walters E, Kessler R. Association of substance use, abuse and dependence with subsequent suicide behavior. American Journal of Epidemiology. 2000;151:781–9. doi: 10.1093/oxfordjournals.aje.a010278. [DOI] [PubMed] [Google Scholar]
- Cash SJ, Bridge JA. Epidemiology of youth suicide and suicidal behavior. Current Opinion in Pediatrics. 2009 doi: 10.1097/MOP.0b013e32833063e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choquet M, Menke H. Suicidal thoughts during early adolescence: prevalence, associated troubles and help-seeking behavior. Acta Psychiatrica Scandinavica. 1990;81:170–7. doi: 10.1111/j.1600-0447.1990.tb06474.x. [DOI] [PubMed] [Google Scholar]
- Chuah YML, Venkatraman V, Dinges DF, Chee MWL. The neural basis of interindividual variability in inhibitory efficiency after sleep deprivation. Journal of Neuroscience. 2006;26:7156–62. doi: 10.1523/JNEUROSCI.0906-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DC. Time-related predictors of suicide in major affective disorder. The American Journal of Psychiatry. 1990;147:1189–94. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. Journal of Consulting and Clinical Psychology. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory AM, Caspi A, Eley TC, Moffitt TE, O'Connor TG, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. Journal of Abnormal Child Psychology. 2005;33:157–63. doi: 10.1007/s10802-005-1824-0. [DOI] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, et al. The National Longitudinal Study of Adolescent Health: research design. 2009 WWW Document.
- Harrison Y, Horne JA. The impact of sleep deprivation on decision making: a review. Journal of Experimental Psychology: Applied. 2000;6:236–49. doi: 10.1037//1076-898x.6.3.236. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–26. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Goldston D, Gatsonis C. Suicidal behaviours and childhood-onset depressive disorders: a longitudinal investigation. Journal of American Academy of Child and Adolescent Psychiatry. 1993;32:8–20. doi: 10.1097/00004583-199301000-00003. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial risk factors for future adolescent suicide attempts. Journal of Consulting and Clinical Psychology. 1994;62:297–305. doi: 10.1037//0022-006x.62.2.297. [DOI] [PubMed] [Google Scholar]
- Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27:1351–8. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. New York, NY: Taylor & Francis Group/Lawrence Erlbaum Associates; 2008. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: program PRODLIN. Behavior Research Methods. 2007;39:384–9. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Sleep Foundation Sleep in America poll: teens and seep. Washington, DC: National Sleep Foundation; 2006. [Google Scholar]
- National Sleep Foundation Sleep in America poll: technology use and sleep. Washington, DC: National Sleep Foundation; 2011. [Google Scholar]
- Nrugham L, Larsson B, Sund AM. Specific depressive symptoms and disorders as associates and predictors of suicidal acts across adolescence. Journal of Affective Disorders. 2008;111:83–93. doi: 10.1016/j.jad.2008.02.010. [DOI] [PubMed] [Google Scholar]
- Ong SH, Wickramaratne P, Tang M, Weissman MM. Early childhood sleep and eating problems as predictors of adolescent and adult mood and anxiety disorders. Journal of Affective Disorders. 2006;96:1–8. doi: 10.1016/j.jad.2006.05.025. [DOI] [PubMed] [Google Scholar]
- Pena JB, Matthieu MM, Zayas LH, Masyn KE, Caine ED. Co-occurring risk behaviors among White, Black, and Hispanic US high school adolescents with suicide attempts requiring medical attention, 1999–2007: implications for future prevention initiatives. Social Psychiatry and Psychiatric Epidemiology. 2012;47:29–42. doi: 10.1007/s00127-010-0322-z. [DOI] [PubMed] [Google Scholar]
- Pilcher JJ, Huffcutt AJ. Effects of sleep deprivation on performance: a meta-analysis. Sleep. 1996;19:318–26. doi: 10.1093/sleep/19.4.318. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–66. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Randazzo AC, Muehlbach MJ, Schweitzer PK, Walsh JK. Cognitive function following acute sleep restriction in children ages 10–14. Sleep. 1998;21:861–8. [PubMed] [Google Scholar]
- Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–6. [PMC free article] [PubMed] [Google Scholar]
- Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Development. 2003;74:444–55. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- Sjostrom N, Waern M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30:91–5. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- Sobel M. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010 doi: 10.1037/a0020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai LL, Young HY, Hsieh S, Lee CS. Impairment of error monitoring following sleep deprivation. Sleep. 2005;28:707–13. doi: 10.1093/sleep/28.6.707. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, et al. Risk factors for late-life suicide: a prospective, community-based study. American Journal of Geriatric Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- Wallander MA, Johansson S, Ruigomez A, Garcia Rodriguez LA, Jones R. Morbidity associated with sleep disorders in primary care: a longitudinal cohort study. Primary Care Companion to the Journal of Clinical Psychiatry. 2007;9:338–45. doi: 10.4088/pcc.v09n0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug and Alcohol Dependence. 2004;76:S11–9. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. Journal of Psychiatric Research. 2009;43:526–31. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Nigg JT, Zucker RA. Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcoholism: Clinical and Experimental Research. 2010a;34:1033–44. doi: 10.1111/j.1530-0277.2010.01178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. Journal of Psychiatric Research. 2010b doi: 10.1016/j.jpsychires.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo S, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep – a prefrontal amygdala disconnect. Current Biology. 2007;17:R877–8. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]