To the Editor:
C-reactive protein (CRP) is a marker of systemic inflammation and cardiovascular disease.1–3 Based on findings from recent clinical trials, CRP has been recommended as an adjunct screening tool to stratify cardiovascular risk in the general population4. However, evidence regarding within-person variability of CRP in the general population is limited. Short-term variability in CRP has important implications for its use an interpretation in clinical practice and research studies. Thus, the objective of this study was to evaluate the short-term, within-person variability in CRP measurements and to quantify the impact of repeat testing on CRP-based cardiovascular risk classification.
Methods
Study Population
We included 541 participants aged 16–69 years who completed repeat examinations of the 2001–02 National Health and Nutrition Examination Survey (NHANES). Briefly, a 5% nonrandom sample of 2001–02 NHANES participants were recruited for the second examination, occurring approximately 2.5 weeks after the original examination. Participants represented a uniform distribution of individuals by age, sex, and race/ethnicity. The study design and methods for NHANES are detailed elsewhere.5
High-sensitivity serum CRP was measured using latex-enhanced nephelometry5. We used a cut-point of ≥1 mg/dL to define elevated CRP, based on the NHANES laboratory reference values and AHA/CDC recommendations.1 We also conducted sensitivity analyses using a higher cut-point (CRP ≥2 mg/dL).
Statistical Analyses
The Spearman’s and intra-class correlation (ICC) coefficients, and the within-person coefficient of variation (CVw) were used to characterize short-term within-person variability6. Persistently elevated CRP was defined as CRP ≥1 mg/dL at both examinations. We used scatterplots and Bland-Altman plots to visually display measurement variability6. Finally, we calculated the percentage of participants whose risk category was reclassified due to repeat testing.
Results
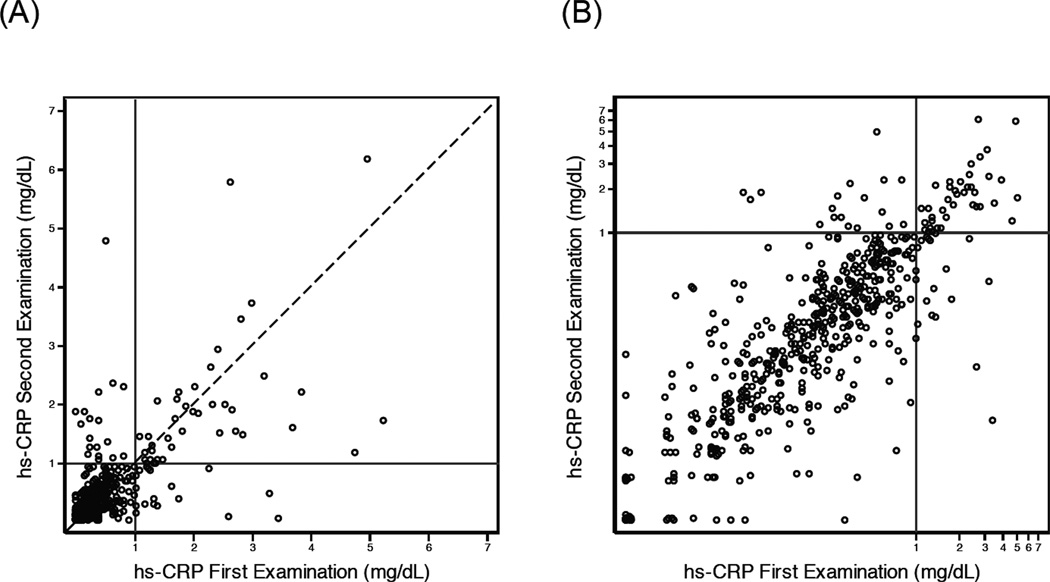
The mean age of participants was 38 years (SD, 16.5). Fifty percent of the study population was female and 48% were of non-Hispanic white race/ethnicity. The mean time between examinations was 18.9 days. Mean CRP was 0.45 mg/dL (95% CI: 0.39–0.51) at the first examination and 0.43 mg/dL (95% CI: 0.38–0.49) at the second examination (p-for-difference=0.45). The Spearman’s correlation between visits was 0.65, the ICC was 0.77 (95% CI: 0.69–0.84), and the CVw was 46.2% (95% CI: 42.9–49.3%). The high variability in CRP can be seen visually on the scatterplot (Figure 1), although the Bland-Altman plot shows that most of the discordance between examinations occurred at higher values (>1.0 mg/dL) (eFigure 1). The variability was particularly high among persons with CRP >2.0 mg/dL.
Figure 1. Scatterplot of CRP measurements in a subsample of NHANES 2001–2002.
Repeat measurements occurred ~19 days apart. Figure 1A is plotted on the arithmetic scale; Figure 1B is plotted on the natural logarithm scale. Solid lines are placed on the x-axis and y-axis where CRP = 1 mg/dL.
The prevalence of elevated CRP ≥1 mg/dL was 10.5% at the first examination and 10.4% at the second; 7.2% of participants had persistently elevated CRP (eTable 1). Of those with normal CRP at the first examination, only 3.5% had CRP ≥1 mg/dL at the second. Of those with CRP ≥1 mg/dL at the first examination, 32% were reclassified as having CRP <1 mg/dL at the second. The prevalence of CRP ≥2 mg/dL at the first examination was 4.3% and was 2.8% at the second; 1.5% of participants had CRP ≥2 mg/dL at both examinations, representing an approximately 65% decrease in prevalence.
Comment
In this sample of the general population, we observed significant short-term (~2.5 weeks) within-person variability in CRP, particularly at high values. Approximately one third of persons with elevated CRP were reclassified as having normal CRP after repeat testing. Our results are consistent with previous studies conducted in small selected populations (e.g., patients with ischemic heart disease) or where measurements were months or years apart.7,8 Of note, we observed greater variation at higher values where clinicians are most likely to intervene.
The 2010 American College of Cardiology Foundation/American Heart Association guidelines for the assessment of cardiovascular risk in asymptomatic adults includes recommendations for CRP to select patients for statin therapy when LDL cholesterol concentration is <130 mg/dL.9 Our results suggest that use of a single CRP measure for risk stratification may lead to substantial misclassification. Recommendations for repeat testing to confirm elevations in CRP prior to altering medical decision-making may be warranted, particularly among those with CRP values near the risk cut points.
Supplementary Material
Acknowledgements
JKB and SPJ were supported by NIH/NHLBI grant T32 HL007024.
Footnotes
Author Contributions
Dr. Bower had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study design and concept: Bower, Lazo, Selvin. Analysis and interpretation of data: Bower, Lazo, Juraschek, Selvin. Drafting of manuscript: Bower. Review and editing of the manuscript: Bower, Lazo, Juraschek, Selvin.
Financial Disclosures
None.
References
- 1.Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003 Jan 28;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 2.Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003;107(3):363–369. doi: 10.1161/01.cir.0000053730.47739.3c. [DOI] [PubMed] [Google Scholar]
- 3.Willerson JT, Ridker PM. Inflammation as a Cardiovascular Risk Factor. Circulation. 2004 Jun 1;109(21 suppl 1):II-2–II-10. doi: 10.1161/01.CIR.0000129535.04194.38. 2004. [DOI] [PubMed] [Google Scholar]
- 4.Spatz ES, Canavan ME, Desai MM. From Here to JUPITER / CLINICAL PERSPECTIVE. Circulation: Cardiovascular Quality and Outcomes. 2009 Jan 1;2(1):41–48. doi: 10.1161/CIRCOUTCOMES.108.832592. 2009. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey Data 2001–2002. [Accessed September 28, 2011]; http://www.cdc.gov/nchs/nhanes/nhanes2001-2002/nhanes01_02.htm.
- 6.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- 7.de Maat MP, de Bart AC, Hennis BC, et al. Interindividual and intraindividual variability in plasma fibrinogen, TPA antigen, PAI activity, and CRP in healthy, young volunteers and patients with angina pectoris. Arterioscler Thromb Vasc Biol. 1996 Sep;16(9):1156–1162. doi: 10.1161/01.atv.16.9.1156. [DOI] [PubMed] [Google Scholar]
- 8.Bogaty P, Brophy JM, Boyer L, et al. Fluctuating inflammatory markers in patients with stable ischemic heart disease. Arch Intern Med. 2005 Jan 24;165(2):221–226. doi: 10.1001/archinte.165.2.221. [DOI] [PubMed] [Google Scholar]
- 9.Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010 Dec 21;122(25):e584–636. doi: 10.1161/CIR.0b013e3182051b4c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.