A 29-year-old right-handed G1P1 Caucasian woman presented with acute bifrontal headache (which resolved within 1 day), confusion, and difficulty using her right hand on postpartum day 10. She did not report nausea, vomiting, or visual complaints. The patient was previously healthy except for her recent preeclampsia, which required emergent cesarean section. On examination, the patient was afebrile, awake, alert, and apathetic. She was able to follow few one-step midline commands (e.g., eye opening and closing) inconsistently but not appendicular commands. Her neurologic deficits were remarkable for expressive aphasia, intermittent receptive aphasia, and hyperreflexia with bilateral extensor plantar responses. No meningismus or other focal neurologic deficits were present. Routine laboratory testing including urine toxicology screen was normal. C-reactive protein was 23 mg/L (reference range: <5 mg/L), and erythrocyte sedimentation rate (ESR) was 38 mm/h (reference range: 0–20 mm/h). Rheumatologic panel was negative. Brain MRI showed extensive non-contrast-enhancing T2/fluid-attenuated inversion recovery hyperintensities involving periventricular and deep white matter, especially the centrum semiovale, corpus callosum, bilateral anterior temporal lobes, bilateral caudate nucleus, and globus pallidus (figure, A–C). No evidence of acute or previous stroke was found. CT angiogram and venogram revealed no cerebral sinus thrombosis or large vessel vasculitis. Lumbar puncture opening pressure was 18.5 cm H2O. CSF showed normal cell counts, protein, and glucose levels without oligoclonal bands. EEG recorded in awake, drowsy, and sleep state was normal. Dilated ophthalmic examination showed no microangiopathy or retinal branch arterial occlusion. Audiologic examination was normal.
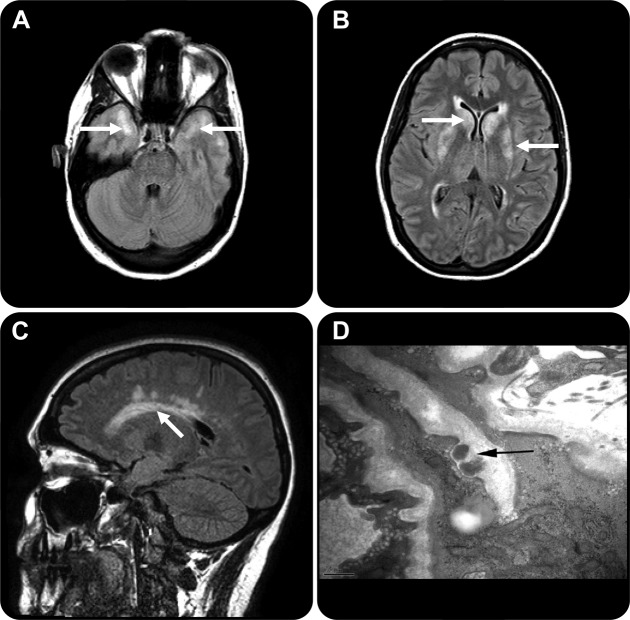
Figure. Brain MRI and biopsy results.
(A) Axial brain MRI fluid-attenuated inversion recovery (FLAIR) imaging shows white matter hyperintensities involving bilateral anterior temporal lobes (arrows). (B) Axial brain MRI FLAIR imaging shows white matter hyperintensities involving bilateral basal ganglia (arrows). This is an important radiographic distinction from multiple sclerosis, a frequent mimic of cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). (C) Sagittal brain MRI FLAIR imaging shows white matter hyperintensities involving corpus callosum and periventricular areas (arrow). (D) Electron micrograph of sample dural vessel wall shows extracellular deposits of granular osmiophilic material (GOM) (arrow) characteristic of CADASIL in the basal lamina of smooth muscle cells. GOM could not be assessed in the white matter sample due to the lack of blood vessel large enough to contain smooth muscle cells. Aside from the subtle spongy/microvacuolar change suggestive of focal edema, there was no other degenerative vascular or parenchymal abnormality (data not shown). Scale bar (bottom left): 0.5 μm.
Due to the rapid deterioration of her mental status, empiric IV Solu-Medrol 1 g/d was initiated for presumed cerebral vasculitis.
Although denying any relevant family history upon admission, the patient's family revealed 2 days later a history of genetically confirmed cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) in one maternal uncle, and stroke in age 40s in the mother, maternal grandmother, and great-grandmother. To diagnose definitively, stereotactic brain biopsy was performed on day 2 of Solu-Medrol. Subtle spongy/microvacuolar change, suggestive of focal edema, was found in white matter sample from an area of MRI signal abnormality. In the dural sample, granular osmiophilic material characteristic of CADASIL was identified in the basal lamina of smooth muscle cells in vessel walls using electron microscopy (figure, D). Genetic testing for the Notch3 gene showed a T>C transition at nucleotide 241, resulting in the substitution of cysteine by arginine, a disease-related mutation. Interestingly, by day 3 of Solu-Medrol, the patient's encephalopathy began to dramatically subside such that she was able to effectively communicate and follow commands. At 1-month follow-up, she was essentially back to her normal baseline.
DISCUSSION
CADASIL is the most common form of hereditary cerebral angiopathy due to mutation in Notch3 gene on chromosome 19.1 Cardinal clinical features include migraine with aura, subcortical ischemic events, mood disturbance, apathy, and progressive cognitive impairment.2 Here we report a patient with CADASIL presenting with acute encephalopathy that improved dramatically following IV Solu-Medrol therapy.
Postpartum acute headache and encephalopathy may result from many etiologies, including postpartum eclampsia, encephalitis, postpartum cerebral angiopathy, venous sinus thrombosis, acute disseminated encephalomyelitis, Susac syndrome, and posterior reversible leukoencephalopathy syndrome. Here, the patient did not have any previous migraine or stroke, but important clues to CADASIL are family history and topographic brain MRI findings. It has been shown that white matter changes involving the anterior temporal lobe has a sensitivity of 95% and specificity of 80% for diagnosing CADASIL.3
Typical symptoms of CADASIL usually develop insidiously and progressively. Acute neuropsychological impairment has rarely been documented.4,5 One study reported 6 patients with CADASIL, all with chronic migraine with aura, who developed reversible acute encephalopathy, headache, fever, seizure, and even coma, that lasted 7–14 days.6 In contrast, our patient did not have fever, seizures, or any history of migraine.
In retrospect, the patient's preeclampsia could also be related to CADASIL. It has been reported that preeclampsia is common in women with CADASIL. The first manifestation of CADASIL may occur during puerperium.7
The mechanism of corticosteroid improving the acute encephalopathy in CADASIL is not clear. The elevated C-reactive protein and ESR here likely represent a nonspecific reaction due to the postpartum/cesarean section state, rather than any CNS autoimmune process. Since electron microscopy reveals change of focal edema, we speculate that the steroids might have improved the condition by alleviating cerebral edema, thus improving blood perfusion. One caveat is that steroid might be irrelevant and the patient's improvement simply reflects the natural course.
DISCLOSURES
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/cp for full disclosures.
REFERENCES
- 1.Tournier-Lasserve E, Joutel A, Melki J, et al. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy maps to chromosome 19q12. Nat Genet 1993;3:256–259. [DOI] [PubMed] [Google Scholar]
- 2.Chabriat H, Joutel A, Dichgans M, Tournier-Lasserve E, Bousser MG. CADASIL. Lancet Neurol 2009;8:643–653. [DOI] [PubMed] [Google Scholar]
- 3.O'Sullivan M, Jarosz JM, Martin RJ, Deasy N, Powell JF, Markus HS. MRI hyperintensities of the temporal lobe and external capsule in patients with CADASIL. Neurology 2001;56:628–634. [DOI] [PubMed] [Google Scholar]
- 4.Ducray F, Ritzenthaler T, Cho TH, et al. Acute headache followed by focal neuropsychological impairment in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). J Stroke Cerebrovasc Dis 2010;19:75–76. [DOI] [PubMed] [Google Scholar]
- 5.Sathe S, DePeralta E, Pastores G, Kolodny EH. Acute confusional migraine may be a presenting feature of CADASIL. Headache 2009;49:590–596. [DOI] [PubMed] [Google Scholar]
- 6.Schon F, Martin RJ, Prevett M, Clough C, Enevoldson TP, Markus HS. “CADASIL coma”: an underdiagnosed acute encephalopathy. J Neurol Neurosurg Psychiatry 2003;74:249–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roine S, Poyhonen M, Timonen S, et al. Neurologic symptoms are common during gestation and puerperium in CADASIL. Neurology 2005;64:1441–1443. [DOI] [PubMed] [Google Scholar]