Summary
Impulse control disorders (ICD) (most commonly pathologic gambling, hypersexuality, and uncontrollable spending) and compulsive behaviors can be triggered by dopaminergic therapies in Parkinson disease (PD). ICD are especially prevalent in patients receiving a dopamine agonist as part of their treatment regimen for PD, and have also been reported when dopamine agonists are used for other indications (e.g., restless legs syndrome). Although these iatrogenic disorders are common, affecting 1 in 7 patients with PD on dopamine agonists, they often elude detection by the treating physician. ICD lead to serious consequences, causing significant financial loss and psychosocial morbidity for many patients and families. ICD can appear at any time during treatment with dopamine agonists, sometimes within the first few months, but most often after years of treatment, particularly when patients receive dopamine agonists and levodopa together. In most cases ICD resolve if the dopamine agonist is withdrawn, and PD motor symptoms are managed with levodopa monotherapy. Familiarity with the clinical aspects, risk factors, pathophysiology, and management of ICD is essential for physicians using dopaminergic therapies to treat PD and other disorders.
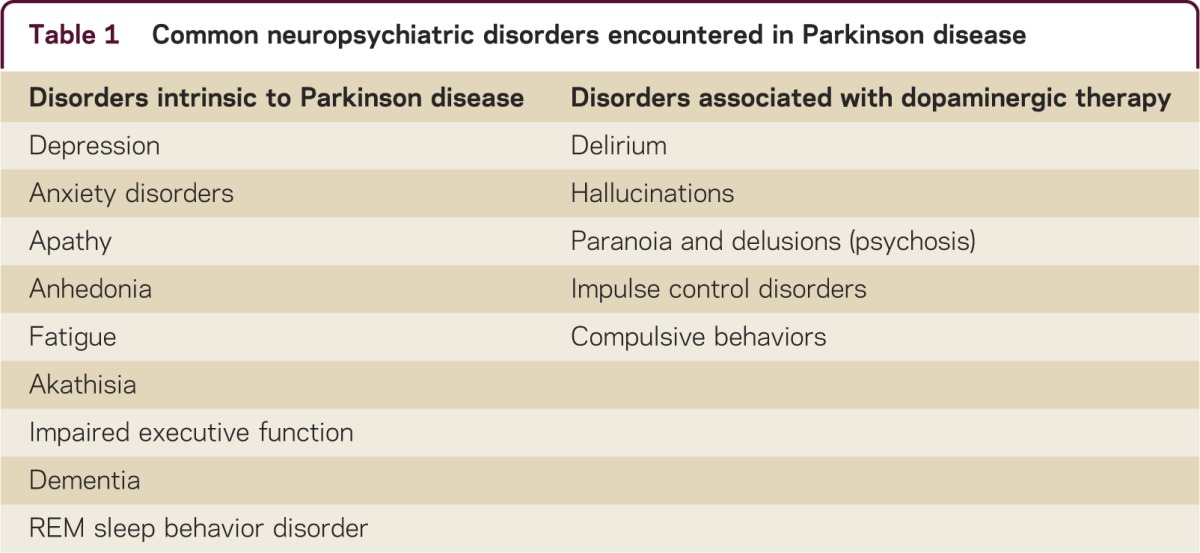
Although historically Parkinson disease (PD) has been conceptualized as a movement disorder, this narrow view understates the complexity of the condition. Significant psychiatric and behavioral problems, including depression, anxiety disorders, akathisia, apathy, anhedonia, impaired executive function, cognitive decline, sleep disorders, and fatigue, are intrinsic features of PD for many patients. In addition, the dopaminergic medications used to treat motor dysfunction of PD have the potential to produce or exacerbate a variety of neuropsychiatric problems, including delirium, hallucinations, delusions, paranoia, psychosis, compulsive behaviors, and impulse control disorders (ICD) (table 1). The development of compulsive behaviors and ICD triggered by dopamine replacement therapy is an important but often under-recognized problem for clinicians and patients.1,2
Table 1.
Common neuropsychiatric disorders encountered in Parkinson disease
Several nonmotor problems (including REM sleep behavior disorder, constipation, cardiac sympathetic denervation, and decreased sense of smell) are known to occur many years before the onset of motor symptoms in PD. Some studies also suggest there might be a pre-Parkinson personality profile: individuals who subsequently develop PD may be more likely to have a cautious personality characterized by industriousness, punctuality, orderliness, reliability, lack of novelty seeking, and risk aversion. Epidemiologic studies revealed that people who develop PD are statistically less likely to smoke, use alcohol, drink coffee, or indulge in other addictive behaviors earlier in life. These cautious personality characteristics have been considered a possible clinical expression of the diminished brain dopamine levels that develop years prior to detectable motor dysfunction in PD.
What might happen to the behavior of some members of this intrinsically cautious cohort after PD is diagnosed, and the treating physician attempts to improve motor function by restoring brain dopamine levels? An early clue was provided shortly after the introduction of levodopa to clinical practice in the early 1970s, when sporadic case reports of hypersexuality appeared in the medical literature. At the time, this aberrant behavior seemed to be an uncommon phenomenon, and considered a curiosity. However, over the past decade, astute clinicians caring for patients with PD recognized the important role of dopaminergic treatment in provoking ICD and other repetitive goal-directed behaviors.
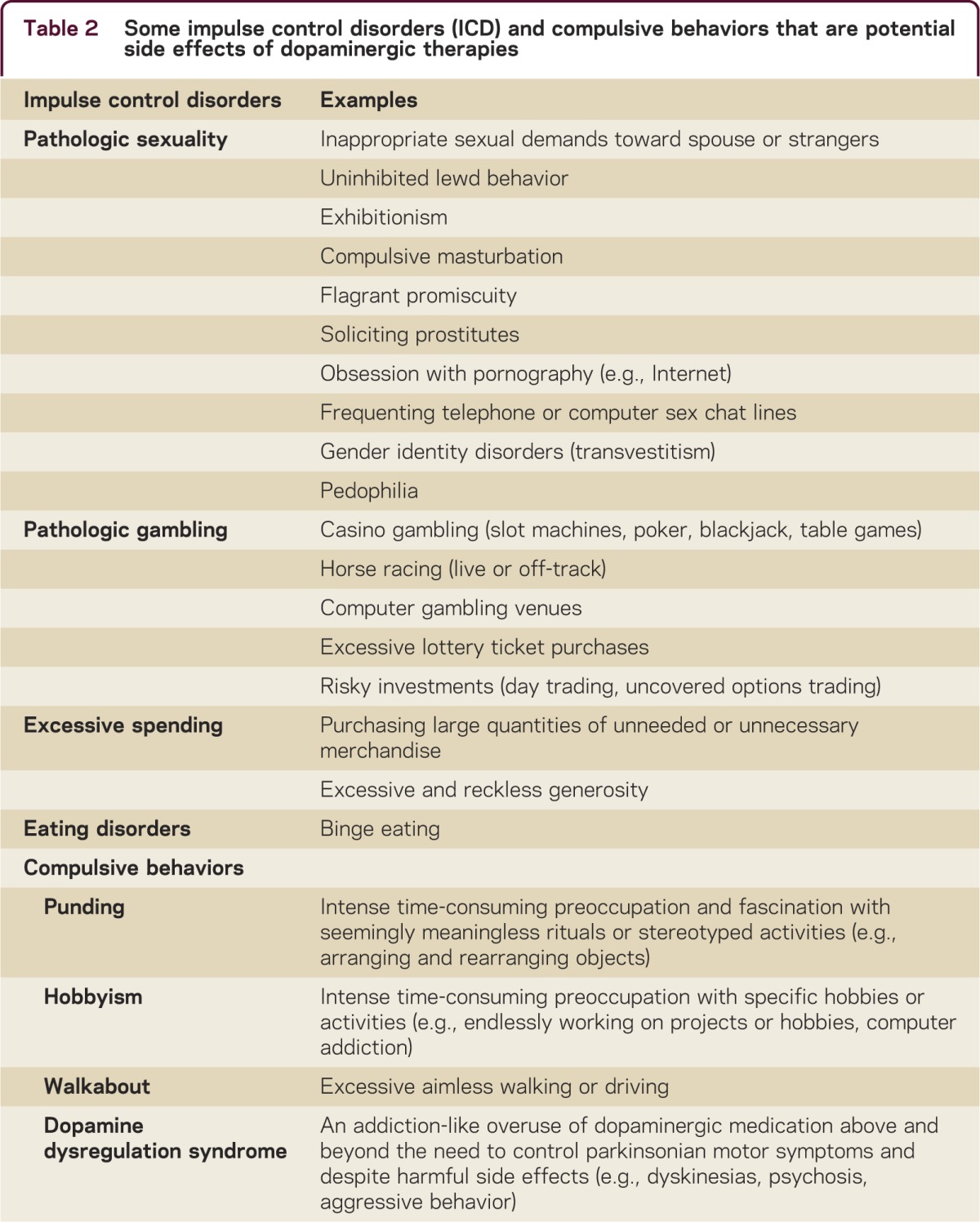
ICD are a family of psychiatric conditions whose essential clinical feature is the irresistible and uncontrollable drive or temptation to perform an action, although the activity may be potentially detrimental to oneself or others. ICD have been conceptualized as behavioral addictions, and are often performed without the patient experiencing subjective distress.3 Compulsive behaviors (repetitive semi-purposeful goal-directed behaviors) such as punding, hobbyism, computer addiction, and dopamine dysregulation syndrome have also been well documented as complications of dopaminergic therapies (table 2).
Table 2.
Some impulse control disorders (ICD) and compulsive behaviors that are potential side effects of dopaminergic therapies
Prevalence
ICD are not a rare phenomenon in patients receiving treatment for PD. A large cross-sectional study of 3,090 patients with PD being treated at 46 centers across the United States and Canada identified an ICD in 13.6% of patients. Problem gambling was diagnosed in 5%, aberrant sexual behavior in 3.5%, excessive spending in 5.7%, and binge eating in 4.3%. Nearly 4% of the patients had 2 or more ICD, and many patients also had concurrent compulsive behaviors (e.g., hobbyism).4 Other series have observed similar or even higher rates of ICD in patients receiving dopaminergic therapies for PD. By comparison, the incidence of pathologic gambling in the general public is less than 1%.
ICD occur predominantly in patients receiving a dopamine agonist (e.g., pramipexole, ropinirole, rotigotine, or pergolide) as part of their PD treatment. The problem is a class effect unrelated to a specific dopamine agonist or a specific dose. The risk of developing an ICD is increased in patients receiving dopamine agonist monotherapy, but is even higher when patients receive a combination of a dopamine agonist plus levodopa. In contrast, the prevalence of ICD in patients with PD receiving levodopa monotherapy is only slightly higher than in the general population, except for those receiving unusually high levodopa doses. Levodopa monotherapy is more likely to provoke compulsive behaviors, such as punding or the dopamine dysregulation syndrome, than ICD.
Challenges in the recognition and detection of ICD
Although ICD are not rare, affecting approximately 1 in 7 patients with PD receiving dopamine agonist therapy, these problem behaviors often go undetected. Dopamine agonists were in widespread clinical use for many years before these serious side effects were reported. This partly reflects that although ICD sometimes ensue shortly after starting the medication, symptoms often develop only after years of treatment when dopamine agonist doses are increased, or when levodopa and dopamine agonists are used together. However, it also underscores the important realization that ICD and other abnormal behaviors will not be detected unless the clinician is knowledgeable about the potential effects of dopaminergic medication on behavior, and assiduously inquires about these disorders. However, even in situations where the treating physician was aware of the relationship between dopaminergic therapies and ICD, they remained undetected in over 50% of the patients who were experiencing an active ICD.5 Diagnosis is important because the consequences of ICD are potentially devastating, including major financial loss, bankruptcy, disrupted social relationships, divorce, institutionalization, and legal problems. One study reported a mean loss of over $100,000 in patients with PD who developed pathologic gambling as a complication of dopamine agonist therapy.2
There are many stumbling blocks to the detection of ICD. Patients are unlikely to spontaneously disclose uncontrollable urges to engage in sexual activity, gambling, or excessive spending. Furthermore, unusual behaviors are sometimes highly individualized and idiosyncratic. For example, reckless generosity, impulsive cigarette smoking, transvestitism, kleptomania, hoarding, and obsessive painting have also been reported as complications of dopaminergic therapies. Patients, families, and physicians may fail to recognize that medication side effects can masquerade as altered behavior or primary psychiatric disease.6
As a first step in facilitating the diagnosis of ICD, physicians need to specifically inquire about unusual behaviors or uncontrollable gambling, sexual, or spending activity. This can be particularly difficult when screening for aberrant sexuality, as many physicians feel uncomfortable probing these very personal topics, particularly with patients of the opposite sex. To avoid seeming voyeuristic or inappropriate, questions about the patient’s sexual interests and personal behavior should be preceded by a brief explanation that medications used to improve brain dopaminergic motor function can also have very unusual effects on behavior that need to be candidly discussed. Since ICD can begin as early as a few months or sometimes only after many years of starting dopamine agonist, discussing and screening for abnormal behaviors should be done before initiating treatment, and regularly throughout the course of treatment.
However, even when asked, patients with ICD frequently minimize or deny the extent of their behaviors, or do not regard their behaviors as abnormal. To recount a recent conversation with one patient:
“Do you gamble?”
“Never, doctor, gambling is the work of the devil!”
“Do you purchase lottery tickets?”
“All the time.”
“How many do you buy?”
“Several hundred dollars a week—it’s like a magnet and I can’t resist it.”
Some patients consciously conceal or deny abnormal behaviors. In our series, the diagnosis of ICD would have remained undetected in more than half of the cases if we relied solely on the information provided by the patient without also interviewing family members or caregivers.5 Interviewing family members and caregivers must also be done on a regular basis to detect abnormal behaviors in patients on dopaminergic medication. Screening instruments for ICD in PD have been developed,7 but are not readily available for general clinical practice.
About one-third of patients who develop an ICD on dopaminergic therapy have multiple ICD and other coexisting behavioral disorders. ICD are often accompanied by depressed mood, disinhibition, irritability, and appetite disturbance.8 Patients with ICD are also at higher risk of concurrently experiencing compulsive behaviors (such as punding, computer addiction, hobbyism, or dopamine dysregulation syndrome), and vice versa. When interviewing the patient, physicians should inquire about nocturnal activity, as people with punding, hobbyism, or computer addiction commonly stay up all night performing their repetitive behaviors.
Unfortunately, despite concerted efforts to interview the patient and obtain collateral information from family or caregivers, ICD can still elude detection. Patients with ICD may be intentionally deceptive to conceal their uncontrollable urges and behaviors. Pathologic gambling is associated with lying, stealing, and other dishonest behaviors, sometimes being discovered only after major financial setbacks can no longer be hidden. Families sometimes discover serious gambling problems only after life savings have been squandered, or when the Internal Revenue Service begins legal proceedings for nonpayment of taxes. Aberrant sexual behavior may remain clandestine until the patient develops legal problems related to soliciting prostitutes or pedophilia.
The development of ICD in patients receiving dopamine agonists is not a phenomenon unique to PD. ICD have also been reported in patients receiving dopamine agonists for other disorders, including restless legs syndrome (pramipexole, ropinirole, rotigotine), prolactin secreting pituitary tumors (cabergoline), fibromyalgia, and chronic fatigue syndrome. Lower doses of dopamine agonist are generally used in these conditions compared to PD. Studies in patients with PD have not revealed a robust correlation between agonist dose and the risk of developing an ICD. Therefore using low doses of agonist for treating these other conditions should not make physicians sanguine that ICD will not occur.
Proposed mechanisms for the development of ICD
Why do dopamine agonists have an increased propensity to provoke ICD compared to levodopa? The pharmacology of brain dopamine receptors may provide the clue. D1 and D2 receptors are both highly expressed in striatal motor regions. The major motor effects of dopamine are attributed to D2 receptor stimulation. D1 stimulation is synergistic to D2 activity in promoting motor responses, and may contribute to development of dyskinesias. D3 receptors mediate motor responses, but are also located in limbic nuclei, and are the target for psychiatric drugs. D3 receptor stimulation has been implicated in the addiction process.
The dopamine agonists have specific affinity for D3 receptors (approximately 20 to 100 times more affinity for D3 than D2), and little or no affinity for D1 receptors. Thus dopamine agonists stimulate pathways that govern reward behavior, pleasure, and addiction more avidly than the dopamine derived from levodopa therapy. The differences in receptor affinity might explain the higher proclivity of dopamine agonists to provoke behavioral alterations (hallucinations, psychosis, and ICD) compared to levodopa.2 The decreased D2 and D1 receptor affinity of the dopamine agonists compared to levodopa also explains their diminished efficacy in palliating motor symptoms in PD, and lower risk of triggering dyskinesias. Ongoing PET, SPECT, and functional MRI studies provide additional insights into altered brain activity in patients with ICD on dopaminergic therapies.
Management
The best remedies are preemption and prevention. Prior to initiating dopaminergic therapies, patients and their families require counseling about the risks of developing ICD, and should be instructed to monitor behaviors after medication is started. Although relatively few patients with PD have a history of ICD prior to initiation of dopamine agonist therapy, these medications should be avoided whenever possible in those who do. Patients with a personal or family history of obsessive-compulsive disorder, impulsive personality, alcoholism, drug abuse, smoking, or other addictive behaviors are likely at higher risk for ICD. In these groups dopamine agonists should either be avoided or used only with extra caution and vigilance.1
Tapering and discontinuing dopamine agonist therapy will eliminate or dramatically reduce ICD behaviors in the vast majority of patients. Improvement occurs despite the fact that levodopa doses might need to be slightly increased to control PD motor symptoms after dopamine agonist withdrawal.9 Patients with PD, even those with significant motor fluctuations, can usually be successfully managed with carefully titrated doses of levodopa (plus supplemental catechol-O-methyl transferase inhibitors or monoamine oxidase type-b inhibitors if needed) without taking dopamine agonists.
Addiction-like withdrawal symptoms (anxiety, panic feelings, irritability, diaphoresis, dysphoria, pain, fatigue, drug craving) occur in some patients with ICD as the dopamine agonist is eliminated (dopamine agonist withdrawal syndrome).10 For patients who require continued dopamine agonist treatment (to prevent withdrawal symptoms or control motor symptoms), improvement in ICD sometimes occurs when lower agonist doses are used, or after switching to a different agonist.
Participation in Gamblers Anonymous, support groups, and behavioral interventions are indicated for many patients with ICD. It may be important for the family to limit the patient’s access to money or the Internet to reduce the ability to gamble, shop, or pursue illicit sexual activity.
The evidence supporting the benefit of psychiatric medications for treating ICD in patients with ICD and PD is weak. Most reports are limited to small open-label studies with no uniform results. Patients with persistent ICD symptoms after reducing or eliminating dopamine agonist therapy might benefit from the atypical neuroleptics quetiapine or clozapine. Other neuroleptics should be avoided in PD, as they potentially worsen motor function because of D2 receptor blockade. The value of selective serotonin uptake inhibitors, although effective in palliating many obsessive-compulsive disorders, is uncertain in treating ICD or compulsions triggered by dopaminergic therapies.
Deep brain stimulation (DBS) might be helpful in some situations by improving control of dyskinesias and motor fluctuations, thereby making it easier to reduce the doses of dopaminergic therapies. However, there have been case reports of ICD behaviors and compulsions beginning after patients underwent DBS for PD.
Clinical and ethical quandaries
Is treatment of ICD always necessary? We live in an era where unusual behavior is deemed acceptable if it is not harmful to others. One can argue that buying hundreds of dollars of lottery tickets each week or huge casino gambling losses are not a problem for a wealthy person. However, it certainly is a problem for an elderly person living on a small fixed income. Intense or unusual sexual demands are not always a problem for the patient’s spouse, but can wreak havoc if this behavior is subsequently directed toward strangers. It is reasonable to worry that seemingly tolerable ICD can spin out of control, eventually causing serious financial, social, or legal consequences. In addition, patients with an ICD often have other ICD or compulsive behaviors that have eluded detection. Consequently, recognizing, monitoring, and treating ICD is generally appropriate, even when the behaviors do not seem to pose an immediate problem.
Important ethical considerations arise when patients develop ICD that presumably would not have occurred in the absence of dopaminergic therapy. Does dopaminergic therapy produce completely new forms of behavior or merely intensify latent preexisting behaviors? Should patients with iatrogenic ICD be held responsible personally, morally, financially, and legally for their abnormal behaviors? These questions are being debated in the courts and by neuroethicists.11
Additional ethical and medicolegal concerns are raised for the physician who administers medications that might impair decision-making processes and lead to irresistible abnormal behaviors. All patients with PD ultimately require dopaminergic medication to ameliorate their motor symptoms, and these therapies greatly improve the quality of life for patients with PD. Clinical management decisions need to weigh the relative risks and benefits of using dopamine agonists or levodopa. For most patients, levodopa is more effective in controlling motor symptoms. The dopamine agonists are more expensive, have a higher risk of inducing psychiatric side effects, and have no sustained long-term benefit compared to levodopa monotherapy. This would argue for preferring levodopa as initial treatment in most cases, an exception possibly being younger patients with PD (under age 45) who are at higher risk for developing severe dyskinesias and motor fluctuations on levodopa than older patients with PD.
Patients and their families need to be prospectively educated about possible behavioral side effects of dopaminergic therapies, especially if the physician recommends treatment with a dopamine agonist. This applies not only in PD, but when dopamine agonists are used for other indications such as restless legs syndrome. Large malpractice verdicts have been awarded against the pharmaceutical companies who manufacture the dopamine agonists for failure to adequately warn about the risk of ICD, and against physicians who failed to warn about or attempt to diagnose ICD.
DISCLOSURES
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/cp for full disclosures.
REFERENCES
- 1.Stamy W, Jankovic J. Impulse control disorders and pathological gambling in patients with Parkinson disease. Neurologist 2008;14:89–99. [DOI] [PubMed] [Google Scholar]
- 2.Voon V, Fox SH. Medication-related impulse control disorders and repetitive behaviors in Parkinson disease. Arch Neurol 2007;64:1089–1096. [DOI] [PubMed] [Google Scholar]
- 3.Evans AE, Strafella A, Weintraub D, Stacy M. Impulsive and compulsive behaviors in Parkinson’s disease. Mov Disord 2009;24:1561–1570. [DOI] [PubMed] [Google Scholar]
- 4.Weintraub D, Koester J, Potenza MN, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol 2010;67:589–595. [DOI] [PubMed] [Google Scholar]
- 5.Weiss HD, Hirsch ES, Swearingen L, Williams JR, Marsh L. Detection of impulse control disorders in Parkinson disease patients. Neurologist 2010;16:406–407. [DOI] [PubMed] [Google Scholar]
- 6.Bostwick JM, Hecksel KA, Stevens SR, Bower JH, Ahlskog JE. Frequency of new-onset pathologic compulsive gambling or hypersexuality after drug treatment of idiopathic Parkinson disease. Mayo Clin Proc 2009;84:310–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weintraub D, Hoops S, Shea JA, et al. Validation of the questionnaire for impulsive-compulsive disorders in Parkinson’s disease. Mov Disord 2009;24:1461–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pontone G, Williams JR, Bassett SS, Marsh L. Clinical features associated with impulse control disorders in Parkinson disease. Neurology 2006;67:1258–1261. [DOI] [PubMed] [Google Scholar]
- 9.Mamikonyan E, Siderowf AD, Duda JE, et al. Long-term follow-up of impulse control disorders in Parkinson’s disease. Mov Disord 2008;23:75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rabinak CA, Nirenberg MJ. Dopamine agonist withdrawal syndrome in Parkinson disease. Arch Neurol 2010;67:58–63. [DOI] [PubMed] [Google Scholar]
- 11.Carter A, Ambermoon P, Hall WD. Drug-induced impulse control disorders: a prospectus for neuroethical analysis. Neuroethics 2011;4:91–102. [Google Scholar]


