Abstract
A 6-month-old infant with LIS1 17p13.3 deletion-positive Miller-Dieker syndrome (MDS) presented with increased seizures in the setting of a Pseudomonal and Enterococcal urinary tract infection and a buttock abscess associated with a lumbosacral dermal sinus tract. MRI of the neuraxis revealed lissencephaly (figure 1), a tethered cord without lipoma or other mass (figure 2A), and an infected lumbosacral dermal sinus tract. Communication with the spinal canal could not be appreciated (figure 2B). The dermal sinus was explored and found not to extend into the spinal canal. This tract was excised and the lateral abscess drained. Tethered cord release is planned upon resolution of infection.
A 6-month-old infant with LIS1 17p13.3 deletion-positive Miller-Dieker syndrome (MDS) presented with increased seizures in the setting of a Pseudomonal and Enterococcal urinary tract infection and a buttock abscess associated with a lumbosacral dermal sinus tract. MRI of the neuraxis revealed lissencephaly (figure 1), a tethered cord without lipoma or other mass (figure 2A), and an infected lumbosacral dermal sinus tract. Communication with the spinal canal could not be appreciated (figure 2B). The dermal sinus was explored and found not to extend into the spinal canal. This tract was excised and the lateral abscess drained. Tethered cord release is planned upon resolution of infection.
Figure 1. Axial T2-weighted MRI of the brain demonstrating agyria and ventriculomegaly, the imaging features of lissencephaly.
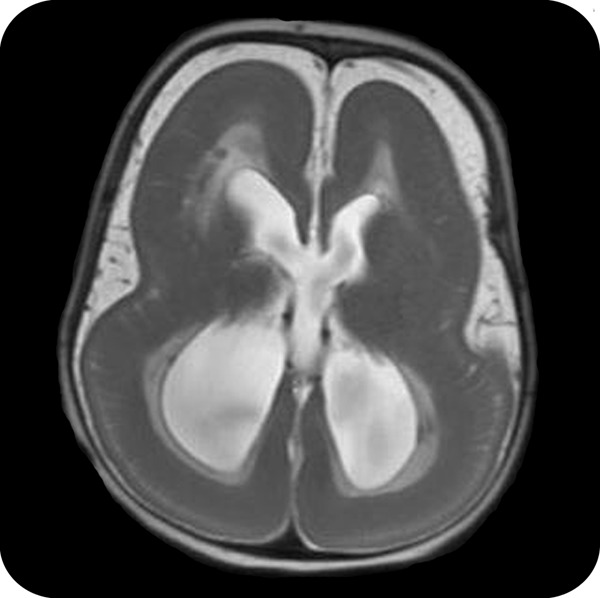
Figure 2. Spine MRI.
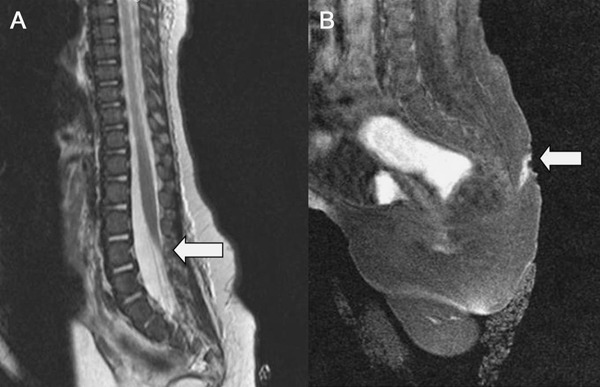
(A) Sagittal T2-weighted MRI of the spine shows the termination of the conus medullaris at the upper level of L4, defining a tethered cord, without an identified lipoma. (B) An inflamed lumbosacral sinus dermal tract was demonstrated with diffuse gadolinium enhancement along its course.
The neurologic manifestations of MDS can include cognitive delays, cerebral palsy, and epilepsy that is often difficult to treat. Typical facial dysmorphisms can include forehead prominence and a short upturned nose. Sacral dimples are common in patients with MDS,1 and may harbor an underlying dermal sinus tract. When in communication with the neuraxis or when complicated by infection, surgical resection of the dermal sinus tract is indicated. Dermal sinus tracts may also be associated with abnormalities in the spinal cord, including caudal intraspinal lipomas or cord tethering. Tethered cords have been reported previously in MDS1,2 and can result in neurogenic bladder dysfunction resulting in frequent urinary tract infections. Additionally, as progressive motor or sensory deterioration can also occur, tethered cord release is advisable. In addition to lissencephaly, spinal dysraphisms should be considered in the spectrum of possible CNS dysgenetic manifestations of 17p13.3 deletions.
DISCLOSURES
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/cp for full disclosures.
REFERENCES
- 1.Dobyns WB, Curry CJ, Hoyme HE, et al. Clinical and molecular diagnosis of Miller-Dieker syndrome. Am J Hum Genet 1991;48:584–594 [PMC free article] [PubMed] [Google Scholar]
- 2.Chen SJ, Peng SF, Kuo MF, et al. Miller-Dieker syndrome associated with tight filum terminale. Pediatr Neurol 2006;34:228–230 [DOI] [PubMed] [Google Scholar]


