Abstract
The death of a parent is a profoundly stressful form of childhood adversity, increasing the short- and long-term risk of mental health problems. Emerging research suggests it may also disrupt biological regulatory systems and increase the risk of long-term physical health problems. This article presents a theoretical framework of the process by which the experience of parental death during childhood may influence mental and physical health outcomes over time. Drawing from a broad literature on adaptation following childhood parental loss, we focus on risk and protective factors in the childhood environment that are theoretically and empirically linked to emotional and biological regulatory responses to stress later in life, the effects of which may accumulate to impact long-term health.
Once viewed primarily as a mental health issue, exposure to childhood adversity is now an established risk factor for a wide array of short- and long-term health and health behavior problems. Prospective longitudinal studies consistently link greater exposure to childhood adversity to mental health problems (Grant et al., 2003). Large birth cohort studies suggest that temporary stressful separations from a parent during childhood increase long-term risk of psychiatric disorder and substance use problems (Räikkönen et al., 2011; Veijola et al., 2008). The Adverse Childhood Experiences (ACE) and other studies link childhood stress to a wide variety of physical illnesses across the lifespan (Anda et al., 2006; Brown et al., 2010; Davis, Luecken, & Zautra, 2005).
Exposure to significant adversity is not a rare occurrence. Close to three-quarters of children are estimated to experience at least one major form of adversity, including natural or manmade disasters, accidents, parental psychopathology, poverty, crime victimization, parental death, physical or sexual abuse, or domestic violence (Kessler, Davis, & Kendler, 1997). The widespread exposure to adversity in combination with evidence linking adversity to health has prompted calls for interventions to reduce the impact of childhood stress and the associated public health burden (Shonkoff, Boyce, & McEwen, 2009). However, the ability to effectively intervene is hampered by limited understanding of underlying mechanisms. Identifying modifiable pathways by which childhood adversity affects lifespan health is a critical next step.
Theoretical reviews propose cognitive, emotional, behavioral, and biological pathways linking childhood adversity in a variety of forms to short and long-term health outcomes (Anda et al., 2006; Repetti, Taylor, & Seeman, 2002; Luecken & Lemery, 2004; Matthews, Gallo, & Taylor, 2010; Taylor, Way, & Seeman, 2011). Although some pathways certainly overlap across forms of adversity, others are likely pronounced following specific adversities. Stressors concomitant with or subsequent to adversity vary widely; for example, interparental conflict typically accompanies parental divorce, while parental bereavement can bring yearly anniversaries of the death and changes in caregivers. Notably, for children who experience parental divorce, externalizing disorders, substance abuse, and low educational attainment are prominent (Maier & Lachman, 2000), whereas internalizing disorders and lower self-confidence are prominent for bereaved youth (Mack, 2001). Protective pathways may also differ; greater family cohesion and peer support have been observed among young adults who experienced parental death, as compared to divorce, in childhood (Short, 2008). Although maladaptive biological stress responses may contribute to poor health outcomes in a consistent manner across different adversities, factors influencing the pattern of dysregulation may vary (e.g., Luecken et al., 2005; Luecken & Appelhans, 2006).
The current paper addresses the mental and physical health consequences of the childhood death of a parent, with a focus on potentially modifiable pathways. First, we discuss the rationale for focusing attention on parental death. Evidence concerning short- and long-term mental and physical health consequences of parental death is reviewed. Next, we propose a comprehensive model of pathways linking early parental death to health. Finally, methodological issues and conclusions are discussed.
Why focus on death of a parent?
Almost 4% of children under the age of 18 in the US experience the death of a parent (Social Security Administration, 2000). Although prior research has generally examined the consequences of a broad category of loss that includes divorce, separation, prolonged absence, and death (Tennant, 1988), parental death is a unique trauma best examined with a dedicated focus. Parental death is one of the most stressful events that can occur in the life of a child, prompting a profound emotional crisis that can threaten a child’s sense of security and controllability over the environment (Sandler, 2001), and engender concerns about their own mortality (Christ, 2010). In contrast to other types of adversity, parental death involves the permanent loss of a critical attachment relationship, often with little or no warning or plausible explanation. Bereaved offspring are then tasked to learn how to live without the presence of a guiding developmental figure. Other adults may be inadequately prepared to respond to the emotional needs of a grieving child, which differ from the needs of a child exposed to parental divorce (Marwit & Carusa, 1998). Parental bereavement cuts across socioeconomic classes, often occurring in a family that was well-functioning before the death. Bereaved children also typically face unique stressors in the years following the death, including relocation, increased family responsibilities, disruption of daily routines, and a surviving parent with elevated distress.
Health consequences of childhood parental death
Mental health
In the short-term, the majority of bereaved children experience elevated symptoms of psychological distress, including acute grief reactions, sleep problems, anger and irritability, and behavioral problems (Silverman & Worden, 1992). For most children, these symptoms resolve in time, but an estimated 10–21% of bereaved children develop clinical levels of internalizing and/or externalizing disorder (Gersten, Beals, & Kallgren, 1991; Worden, 1996). Bereaved children remain at higher long-term risk of a variety of mental health problems (Luecken, 2008). This risk is particularly high after the loss of a parent to suicide, accident, or sudden death (Brent, Melham, Donohoe, & Walker, 2009). Some studies find that childhood parental death is an independent predictor of psychiatric disorders in middle-aged and older adults (Agid et al., 1999; Kendler, Gardner, & Prescott, 2002, 2006; Kivela, Luukinen, Koski, Viramo, & Kimmo, 1998), although other studies have not found direct effects on adult psychopathology (Kessler, et al., 1997; Mireault & Bond, 1992; Kendler, Neale, Kessler, Heath, & Eaves, 1992).
Although parental bereavement is associated with higher lifetime risk for psychological problems, most children progress through the “normal” grieving process and return to healthy functioning without significant impairment. Understanding the pathways through which adaptation occurs can help identify optimal areas or time points for intervention, maximizing the opportunity to promote positive adjustment in the aftermath of parental death.
Physical health and biological stress response systems
In contrast to psychological outcomes, the potential physical health consequences of childhood parental death have been less studied. In a large birth cohort study in England, Neeleman, Sytema, and Wadsworth (2002) found that middle-aged participants who reported the death of a parent before their 16th birthday endorsed significantly more physical health complaints than non-bereaved participants. A few epidemiological and correlational studies link childhood parental death to lifespan physical health problems (Agid et al., 1999; Felitti et al., 1998; Krause, 1998; Lowman, Drossman, Cramer, & McKee, 1987), while others do not (Maier and Lachman, 2000; Tennant, 1988).
One mechanism frequently proposed to link childhood adversity to physical health involves biological stress response systems. When a situation is perceived as a threat, processes regulated by the sympathetic-adrenomedullary (SAM) axis result in the immediate release of epinephrine and norepinephrine into the bloodstream, prompting cardiovascular responses such as increased heart rate and respiration. The hypothalamic-pituitary-adrenal (HPA) axis enacts a delayed response, directing a series of endocrine activities that result in the secretion of cortisol. Well-regulated biological stress responses support adaptive cognitive, emotional, and behavioral responses to challenging situations. However, exposure to traumatic or chronic stressors during childhood can cause SAM and HPA stress responses to become dysregulated, as evidenced by alterations in magnitude or duration (McCrory, De Brito, & Viding, 2010).
Although dysregulated biological responses have been linked to harsh family environments (Lehman, Taylor, Kiefe, & Seeman, 2009; Troxel & Matthews, 2004), maltreatment (Van Voorhees et al. 2004), and other forms of adversity (Elzinga et al., 2008), research specific to parental death is limited. Bereaved children (Pfeffer, Altemus, Heo, & Jiang, 2007) and adults who experienced parental death during childhood (Nicolson, 2004) had higher basal cortisol relative to non-bereaved comparison groups. Permanent parental separation in childhood has been associated with elevated (Pesonen et al., 2010) and attenuated (Bloch, Peleg, Koren, Aner, & Klein, 2007) cortisol following stress, as well as lower basal cortisol (Flinn, Quinlan, Decker, Turner, & England, 1996). Higher blood pressure (BP) during stress (Luecken, 1998) and lower daily ambulatory blood pressure (ABP; Luecken, Appelhans, Kraft, & Enders, 2009) have also been found among young adults parentally bereaved during childhood.
Ongoing dysregulation increases vulnerability to physical disorder later in life (McEwen & Wingfield, 2003). For example, chronic elevated cortisol has been associated with insulin resistance, a precursor to Type 2 diabetes, and may increase risk for cardiovascular disease (Lundberg, 2005) and upper respiratory illnesses (Edwards et al., 2003). Abnormally low cortisol has been observed among individuals with chronic fatigue and fibromyalgia (Demitrack & Crofford, 1998). Exaggerated cardiovascular reactivity, prolonged recovery, and elevated resting heart rate are powerful risk factors for high blood pressure, dysrhythmias, coronary heart disease, and cardiovascular disease mortality (Curtis & O’Keefe, 2002; Stewart & France, 2001; Cooney et al., 2010). Blunted cardiovascular activity has been associated with poor health outcomes, including worse self-rated health and obesity (Phillips, 2011).
Theoretical model of pathways linking early parental loss to health over time
A logical conclusion to be reached from studies of health outcomes is that circumstances after parental death may be stronger indicators of the long-term impact than the loss event itself (Harris, Brown, & Bifulco, 1986; Sandler, 2001). A risk and protective factor model proposed by Sandler (2001) suggests that the cumulative impact of multiple risk and protective factors following childhood parental death can help explain differential mental health outcomes. Although Sandler’s model does not address physical health consequences of parental death, many of the theorized risk and protective factors are relevant to biological systems and physical health. These risk and protective factors can be considered moderators and/or mediators of the impact of the death on children’s physical and psychological adjustment. That is, the risk for poor outcomes is elevated in the presence of risk factors, and decreased by the presence of protective factors: in this sense, these factors serve as moderators that help explain individual differences in outcomes among bereaved children. In addition, parental death can initiate a “cascade” of risk factors that mediate the impact of the death over time. For example, Kendler, Gardner, & Prescott (2006) find that the relation between early parental loss and major depression in adult men is partially mediated by low parental warmth and later stressful events.
Transactional models posit dynamic person-environment processes that underlie adaptation across time. Applied to parental death, a transactional framework recognizes that youth must adapt to the disruptions and restructuring of their environments that happen as a result of the death (Sandler et al., 2008). The model shown in Figure 1 proposes that risk and protective qualities of the post-loss environment influence the satisfaction of children’s basic needs in ways that can either enhance or impair the ability to successfully negotiate later-life challenges. Specifically, risk and protective factors can influence the extent to which future interactions with the environment are perceived as stressful, which will influence emotional and biological regulatory responses, which ultimately influence long-term mental and physical health. Bolger and Zuckerman’s (1995) framework provides a useful heuristic for illustrating how risk and protective factors can influence the stress process in the lives of bereaved youth; 1) Differential exposure: parental death and post-loss risk and protective factors influence the frequency of exposure to stress, 2) Differential reactivity: parental death and post-loss risk and protective factors alter the magnitude of reactivity to stress, or 3) Differential exposure-reactivity: parental death and post-loss risk and protective factors influence both exposure and reactivity to stress.
Figure 1.
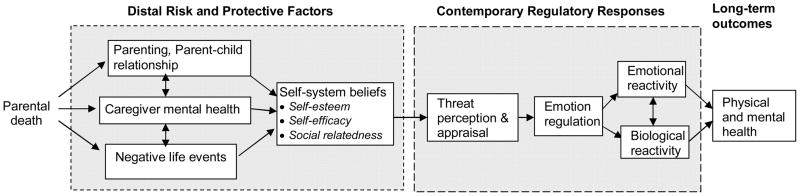
Theoretical model of pathways linking childhood parental death to physical and mental health
Distal Risk and Protective Factors
Parenting and the parent-child relationship
Across a wide range of studies, a warm relationship with the surviving caregiver consistently emerges as a critical protective factor after parental death. Positive parenting, defined as caregiver warmth and consistent discipline, predicts lower mental health problems for bereaved children, even in the face of continuing negative life events (Haine, Wolchik, Sandler, Millsap, & Ayers, 2006). Warmth from the surviving parent also consistently predicts fewer long-term mental health problems (Bifulco, Brown, & Harris, 1987; Kendler, Gardner, and Prescott, 2006). Limited research has examined physical health, however several studies note the influence of parenting and the parent-child relationship on biological regulatory response systems in bereaved youth (discussed below).
Caregiver mental health
Considerable evidence links the mental health of bereaved children to the mental health of their surviving caregiver (Kalter et al., 2002). The concordance between parent and child mental health is not unique to bereaved families. However, the experience of spousal death may precipitate depression in a previously well-functioning caregiver (Stroebe & Stroebe, 1993). Multiple pathways increase risk for children of depressed caregivers. Caregiver depression negatively impacts parenting behaviors and the quality of parent-child interactions (Caughy et al, 2009; Goodman & Gotlib, 2002) and may compromise the development of skills needed to respond adaptively to future stressors. Bereaved children may be at particular risk for maladjustment if they must manage not only their own grief, but that of their depressed caregiver. Although not specific to bereavement, studies have associated parental depression with maladaptive HPA and cardiovascular activity as well as poor physical health in their offspring (Gump et al., 2009).
Negative life events
The early death of a parent increases exposure to other stressors, both in childhood and later in life, and negative life events serve as an important mediator of the relation between the death experience and mental health outcomes (Thompson, Kaslow, Price, Williams, & Kingree, 1998). The occurrence of negative life events following parental death can increase the risk of parenting difficulties and interfere with the parent-child relationship (Wolchik, Tein, Sandler, & Ayers, 2006). Similar “cumulative adversity” theories (e.g., Hertzman, 1999) suggest that childhood parental death can increase the risk of adverse long-term physical health outcomes through exposure to additional life stressors, which over time contribute to dysregulation and breakdown of bodily systems.
Self-system beliefs
In Sandler’s model (2001), parental death serves as a threat to a child’s maintenance of basic needs, including a sense of self-esteem, self-efficacy, and social relatedness. The fulfillment of these basic needs is collectively refered to as the child’s set of self-system beliefs. Parental death disrupts an important esteem-supporting relation, and stressful events after the death can further reduce child self-esteem (Haine, Ayers, Sandler, Wolchik, & Weyer, 2003). The adverse effects of parental loss on self-esteem can be especially pronounced among younger children whose simplistic reasoning may lead them to erroneously blame themselves for the death (Christ, 2010). Low self-esteem has been found to mediate the relation between parental death and depressive disorders in children (Lutzke, Ayers, Sandler, & Barr, 1997) and adult men (Kendler et al., 2006). Self-efficacy beliefs, defined as the belief that one can effectively deal with the stressor and the emotions aroused by it, may be threatened by the unpredictable and/or uncontrollable nature of the death, leading to to poor adjustment in bereaved children (Worden & Silverman, 1996). Children’s sense of security in their relationship with their surviving caregiver may also be compromised by parental death. Poorly developed attachment bonds can negatively impact children’s social competence and their expectations of others (Sroufe, 2005). Parental bereavement can increase the likelihood that securely attached offspring develop an insecure attachment style later in life (Waters, Merrick, Treboux, Crowell, & Albersheim, 2000). Accordingly, childhood parental death has been associated with unstable personal relationships and fewer social resources in adulthood (Ragan & McGlashan, 1986; Johnson & Barer, 2002).
Qualities of the family environment can impact children’s satisfaction of these basic needs (self-esteem, self-efficacy, and social relatedness) following parental loss. Lin and colleagues (2004) found that bereaved children with caregivers who provided high levels of warmth and consistent discipline had higher self-esteem and self-efficacy than vulnerable children. Luecken (2000a) found that a highly caring surviving parent predicted higher social support in young adults who experienced childhood parental death.
Childhood parental bereavement and contemporary regulatory responses to stress
Threat perception and appraisal
As reviewed above, parental death increases exposure to additional life stressors. It may also increase the perception of threat in ambiguous or benign events (Luecken, Appelhans, Kraft, & Brown, 2006). Parentally bereaved children rendered vulnerable by low self-esteem, self-efficacy, or inadequate social support may lack the resources to accurately perceive or appraise potential threats in the environment. Uncontrollable traumas such as parental death can disrupt an existing model of the world in which experiences are predictable and controllable (Brewin, Dalgleish, & Joseph, 1996). Chaotic or unpredictable rearing conditions can similarly lead children to develop a heightened sense of danger (Wandersman & Nation, 1998), leading to greater distress, poor self-regulation (Evans, Gonnella, Marcynszyn, Gentile, & Sapelkar, 2005), and increased daily cortisol output (Chen, Cohen, & Miller, 2009).
Children who view their world as highly threatening may selectively attend to negative aspects of their environment or perceive ambiguous situations as threatening. At an unconscious level, Luecken and Appelhans (2005) reported that childhood parental death influenced regulatory responses during a “dot probe” paradigm used to measure automatic, non-conscious vigilance towards threat cues. Young adults from bereaved families failed to show an adaptive pattern of attentional avoidance of threat words (i.e., a “protective bias”), as was evident among non-bereaved youth. Notably, the pattern evident among bereaved participants was also distinct from that of young adults from divorced families, who showed vigilance towards threat cues. Bereaved youth who fail to achieve meaningful and supportive interpersonal relations may be suspicious of others’ intentions in a manner that predisposes them to perceive threat in social situations (Wolchik et al., 2006). In contrast, higher quality caregiver-child relationships and greater self-efficacy have been associated with lower perceived threat in response to negative life events (Lin et al., 2004), and attentional avoidance of threat cues (Luecken & Appelhans, 2005) among bereaved youth.
Emotion Regulation
Once perceived, emotional and biological regulatory responses are initiated in the service of either responding to the threat or minimizing harm. The ability to regulate emotions in socially and contextually appropriate ways is a critical factor promoting positive mental and physical health in adulthood (Beauchaine, Gatze-Kopp, & Mead, 2007; Campbell-Sills & Barlow, 2007; Joormann & Gotlib, 2010). Emotion regulation refers to conscious and automatic efforts to modulate one’s emotional experience and expression through influence exerted on the type, timing, and intensity of emotions (Mauss, Bunge, & Gross, 2007). The unique trauma and strong emotions associated with early parental death create a potent test of children’s developing regulatory capacities. Stressors subsequent to parental death may continue to strain children’s emotion regulation skills. Thus, adaptive emotion regulation skills may be especially critical for bereaved youth.
The family environment is the primary context in which children learn to regulate emotions. The extent to which children meet the emotional challenges of bereavement may be strongly influenced by the aforementioned risk and protective factors. Children faced with the intense emotions and stressors associated with the death of their parent may be particularly dependent on a strong parent-child relationship to build skills critical for managing future stressors. In general, positive parenting is associated with the development of adaptive emotion regulation (Eisenberg et al., 2005), while negative parenting is linked to maladaptive emotion regulation (Sheffield Morris, Silk, Steinberg, Myers, & Robinson, 2007). Considerable research finds that caregiver depression compromises children’s development of emotion regulation (Goodman & Gotlib, 2002; Sohr-Preston & Scaramella, 2006). For bereaved children, caregiver depression can decrease positive parenting, which in turn can further impair the development of emotion regulation (Kwok, Haine, Sandler, Ayers, & Wolchik, 2005).
Emotional reactivity
The effectiveness of emotion regulation is theorized to predict emotional and biological reactivity to stressors. We define emotional reactivity as the nature and intensity of emotion experienced as a result of stress exposure and associated regulatory attempts. Luecken et al. (2009) collected diary reports of hassles, negative affect, and ABP every 30 minutes for one day from young adults who experienced early parental death. Hassles were associated with higher negative affect and ABP, but higher caring from the surviving parent predicted fewer hassles, and lower negative emotional reactivity to hassles. Notably, the protective influence of parental caring was not evident in a non-bereaved comparison group. Slavich, Monroe, & Gotlib (in press) suggest that bereaved children may be differentially emotionally reactive to stress over the lifespan, such that the death emotionally sensitizes individuals to later life interpersonal losses, resulting in higher depressive responses to lower levels of stress relative to nonbereaved adults.
Biological reactivity to stress
Parental death and subsequent stressors can potentially lead to maladaptive patterns of stress responsivity. Among a sample of parentally bereaved adolescents, exposure to a greater number of negative life events following parental death was associated with lower cortisol across a stressful task six years later (Hagan, Luecken, Sandler, & Tien, 2010). In the long-term, parental death has been associated with elevated cortisol levels among bereaved youth exposed to family conflict, abuse, or low care from the surviving parent, effects that were not evident in non-bereaved comparison groups (Luecken, 2000b; Luecken & Appelhans, 2006). Among bereaved youth who experienced low positive parenting in childhood, Hagan et al. (2011) observed a positive relation between recent negative life events and cortisol levels during a stressful task, while cortisol levels were not related to recent negative life events among bereaved youth who experienced higher positive parenting. The effects of bereavement may differ from those associated with other childhood adversities. For example, higher quality family relationships have been associated with greater cardiovascular reactivity and stronger recovery among bereaved youth relative to youth from divorced families (Luecken, Rodriguez, & Appelhans, 2005).
Other Relevant Pathways
The proposed model focuses on psychosocial pathways, but does not fully capture the complexity of relations between childhood parental death and long-term health. Reciprocal paths are not modeled, but may characterize associations between factors. For example, children’s social relationships may influence and be influenced by biased threat appraisals. Certainly there are other biological and psychosocial/behavioral processes that influence long-term adaptation that are beyond the scope of this article. Below, we describe a few promising factors, with the caveat that there is a lack of strong empirical support specific to parental death.
Health behaviors
The influence of risky behaviors on health in the general population is clear. Risk and protective aspects of the childhood family environment after parental death can influence the development of health behaviors, representing a potential path to long-term health outcomes. Childhood adverse experiences are associated with smoking and early initiation of alcohol use in adolescence, smoking, risky sexual behavior, and alcohol and drug abuse in adulthood (Dube, Anda, Felitti, Edwards, & Croft, 2002). However, effects specific to parental death have not been found (Kendler, Sheth, Gardner, & Prescott, 2002; Estaugh & Power, 1991).
Genetics
At a most basic level, genotypes that contributed to premature parental death may directly influence offspring health (e.g., children may inherit risk for specific medical illnesses). Genetic influences on risk-taking, impulsivity, psychopathology and substance abuse (Kreek, Nielsen, Butelman, & LaForge, 2005; van Beek, 2011; Mortensen, Pedersen, Melbye, Mors, & Ewald, 2003) may play a role in accidental or violent parental death as well as children’s subsequent behavioral or mental health problems. However, evidence directly linking specific genes to specific mental or physical health outcomes is rare, and is unlikely to explain most associations between parental death and offspring health. More likely, gene-environment interactions may help understand offspring vulnerability. For example, the short allele of the serotonin transporter gene has been linked to depression after childhood maltreatment (Karg, Burmeister, Shedden, & Sen, 2011). Epigenetic modifications may also help understand how childhood stressors can alter DNA methylation in a manner that increases risk of adverse physical and psychological outcomes (Essex et al., in press).
Genetic research specific to parental death is limited. However, several studies have evaluated individual components of the model in Figure 1. The short allele of the serotonin transporter gene has been linked to aspects of emotion regulation (Fox, Ridgewell, & Ashwin, 2009; Kwang, Wells, McGeary, Swann, & Beevers, 2010). Kinnally et al., (2009) reported that high quality parental care moderated the impact of the low activity MAOA gene on aggressive behavior in women who experienced childhood parental loss, separation, divorce, or abuse. Genes that regulate the HPA axis also appear relevant to understanding vulnerability following childhood adversity (Tyrka et al., 2008).
Pre-existing vulnerability
Vulnerability factors prior to parental death may compound bereavement effects on health. Brent et al. (2009) observed a greater risk of depression among youth reporting one or more depressive episodes prior to parental death, as well as an indirect effect of prior history through exposure to a greater number of negative life events. Similarly, caregivers with a history of depression may be particularly vulnerable to mental health problems following spousal loss, impacting child well-being (Weller, Weller, Fristad, & Bowes, 1991).
Socioeconomic Status
Low socioeconomic status (SES) can negatively affect adult health (Cohen, Janicki-Deverts, Chen, & Matthews, 2010). The financial hardship that often results from parental death may compound the health impact. Sandler (2001) notes that parental death can impair achievement of developmental competencies such as academic or occupational success, potentially prolonging socioeconomic hardship. In non-bereaved samples, low SES has been linked to parenting difficulties (McLloyd, 1998), negative life events (Evans & English, 2002), exaggerated threat appraisals (Chen, Langer, Raphaelson, & Matthews, 2004), and dysregulated physiological stress responses (Evans & Kim, 2007). Socioeconomic adversity during childhood may also program a “defensive phenotype” characterized by dysregulated neuroendocrine and inflammatory stress responses that may ultimately impact physical health (Miller et al., 2009).
Methodological Considerations
Across studies, small sample sizes often force the use of broad definitions of parental loss that combine parental death with divorce and separations from a parent for any reason. As reviewed above, unique qualities of each experience, as well as the family stressors that precede and follow, may direct children onto different pathways that impact adult health (Sandler, 2001; Mack, 2001). Future research specific to parental death and comparisons of bereavement to other forms of adversity may elucidate these differences. Use of other overly inclusive terms has been problematic. “Early” parental death has been studied with respect to loss experienced childhood, adolescence or early adulthood. The scarcity of prospective, longitudinal studies make it difficult to form conclusions about age effects or “critical periods”. Although some research suggests younger children are at greater risk following parental death (Agid et al., 1999), others have observed no age-related differences (Luecken et al., 2009; Tyrka et al., 2008). However, developmental differences in children’s cognitive and emotional growth, as well as their understanding of death, may alter the relative importance of particular pathways to adjustment (Dowdney, 2000). For example, the effects of caregiver depression may be pronounced for young children, for whom the development of emotion regulation is more highly dependent on caregiver behavior.
Evaluating long-term health outcomes associated with parental death requires a complex model of individual, familial, and environmental factors that operate across cognitive, emotional, and biological systems. The nature of parental death poses a significant challenge to testing elaborate models, as bereaved youth are difficult to identify and recruit into research (Dowdney, 2000). Sample size and study design limitations often only support piecemeal analyses of proposed pathways. Small samples sizes may also impede critical research into genetic mechanisms and gene-enviroment interactions affecting health outcomes in bereaved youth. Although considerable time and resources are required, integrative approaches represent a pivotal step in advancing research on parental bereavement. Informed by comprehensive models, early interventions with bereaved youth can target putative mediators, providing a powerful test of theorized pathways linking parental death to physical and mental health (see Sandler et al., 2010; Luecken et al., 2010).
Concluding Comments
The evidence is clear that adverse childhood experiences can have a lasting impact on mental and physical health. The early death of a parent represents a particularly profound form of adversity. We propose a theoretical model that emphasizes post-death risk and protective factors and their impact on the development of responses to future stressors as pathways to long-term health. Risky environments are predicted to impair bereaved children’s capacity to adaptively regulate emotional and behavioral responses to those stressors, resulting in poor health outcomes over time. Conversely, protective environments are theorized to promote adaptive emotion regulation, leading to lower emotional and physiological stress burden and better health outcomes over time.
Evidence to support each specific link in the proposed theoretical model is limited, and much remains to be empirically evaluated. Continued investigation into pathways and mechanisms is needed. Nonetheless, it is our hope that this model will be useful in the design of interventions to reduce the negative health impact of childhood bereavement. Important progress has been made in the development of preventive interventions for parentally-bereaved families (Sandler et al., 2003; 2010). By focusing on modifiable mediators along the proposed pathways (e.g., improving the relationship with the surviving caregiver or decreasing child exposure to negative life events), it may be possible for targeted interventions to prevent or minimize long-term mental and physical health problems following childhood parental death.
References
- Agid O, Shapira B, Zislin J, Ritsner M, Hanin B, Murad H, Troudart T, Bloch M, Heresco-Levy U, Lerer B. Environment and vulnerability to major psychiatric illness: a case control study of early parental loss in major depression, bipolar disorder, and schizophrenia. Molecular Psychiatry. 1999;4:163–172. doi: 10.1038/sj.mp.4000473. [DOI] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Gatze-Kopp L, Mead HK. Polyvagal theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology. 2007;74:174–184. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bifulco A, Brown G, Harris T. Childhood loss of parent, lack of adequate parental care and adult depression: A replication. Journal of Affective Disorders. 1987;12:115–128. doi: 10.1016/0165-0327(87)90003-6. [DOI] [PubMed] [Google Scholar]
- Bloch M, Peleg I, Koren D, Aner H, Klein E. Long-term effects of early parental loss due to divorce on the HPA axis. Hormones and Behavior. 2007;51:516–523. doi: 10.1016/j.yhbeh.2007.01.009. [DOI] [PubMed] [Google Scholar]
- Bolger N, Zuckerman A. A framework for studying personality in the stress process. Journal of Personality and Social Psychology. 1995;69:890–902. doi: 10.1037//0022-3514.69.5.890. [DOI] [PubMed] [Google Scholar]
- Brent D, Melham N, Donohoe MB, Walker M. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. American Journal of Psychiatry. 2009;166:786–794. doi: 10.1176/appi.ajp.2009.08081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Dalgleish T, Joseph SA. A dual representation theory of posttraumatic stress disorder. Psychological Review. 1996;103:670–686. doi: 10.1037/0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- Brown DW, Anda RF, Felitti VJ, Edwards VJ, Malarcher AM, Croft JB, Giles WH. Adverse childhood experiences are associated with the risk of lung cancer: a prospective cohort study. BMC Public Health. 2010;10:20. doi: 10.1186/1471-2458-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross JJ, editor. Handbook of emotion regulation. New York: Guilford Press; 2007. [Google Scholar]
- Caughy MO, Huang K, Lima J. Patterns of conflict interaction in mother-toddler dyads: Differences between depressed and non-depressed mothers. Journal of Child and Family Studies. 2009;18:10–20. doi: 10.1007/s10826-008-9201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Cohen S, Miller GE. How low socioeconomic status affects 2-year hormonal trajectories in children. Psychological Science. 2009;21:31–37. doi: 10.1177/0956797609355566. [DOI] [PubMed] [Google Scholar]
- Chen E, Langer DA, Raphaelson YE, Matthews KA. Socioeconomic status and health in adolescents: the role of stress interpretations. Child Development. 2004;75(4):1039–1052. doi: 10.1111/j.1467-8624.2004.00724.x. [DOI] [PubMed] [Google Scholar]
- Christ GH. Children bereaved by the death of a parent. In: Balk D, Corr C, editors. Children’s Encounters with Death, Bereavement, and Coping. Springer Publishing Company, LLC; New York, NY: 2010. pp. 169–193. [Google Scholar]
- Cohen S, Janicki-Deverts D, Chen E, Matthews KA. Childhood socioeconomic status and adult health. Annals of the New York Academy of Sciences. 2010;1186:37–55. doi: 10.1111/j.1749-6632.2009.05334.x. [DOI] [PubMed] [Google Scholar]
- Cooney MT, Vartiainen E, Laakitainen T, Juolevi A, Dudina A, Graham IM. Elevated resting heart rate is an independent risk factor for cardiovascular disease in healthy men and women. American Heart Journal. 2010;159:612–619. doi: 10.1016/j.ahj.2009.12.029. [DOI] [PubMed] [Google Scholar]
- Curtis BM, O’Keefe JH. Autonomic tone as a cardiovascular risk factor: The dangers of chronic fight or flight. Mayo Clinic Proceedings. 2002;77:45–54. doi: 10.4065/77.1.45. [DOI] [PubMed] [Google Scholar]
- Davies KA, Macfarlane GJ, McBeth J, Morriss R, Dickens C. Insecure attachment style is associated with chronic widespread pain. Pain. 2009;143:200–205. doi: 10.1016/j.pain.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis D, Luecken LJ, Zautra A. Are reports of childhood maltreatment related to the development of chronic pain in adulthood? A meta-analytic review of the literature. Clinical Journal of Pain. 2005;21:398–405. doi: 10.1097/01.ajp.0000149795.08746.31. [DOI] [PubMed] [Google Scholar]
- Demitrack MA, Crofford LJ. Evidence for and pathophysiologic implications of hypothalamic-pituitary-adrenal axis dysregulatino in fibromyalgia and chronic fatigue syndrome. Annals of the New York Academy of Sciences. 1998;840:684–697. doi: 10.1111/j.1749-6632.1998.tb09607.x. [DOI] [PubMed] [Google Scholar]
- Dowdney L. Annotation: Childhood bereavement following parental death. Journal of Child Psychology and Psychiatry. 2000;41:819–830. [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors. 2002;27:713–725. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- Edwards S, Hucklebridge F, Clow A, Evans P. Components of the diurnal cortisol cycle in relation to upper respiratory symptoms and perceived stress. Psychosomatic Medicine. 2003;65:320–327. doi: 10.1097/01.psy.0000033123.70631.8e. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Zhou Q, Spinrad TL, Valiente C, Fabes RA, Liew J. Relations among positive parenting, children’s effortful control, and externalizing problems: A three-wave longitudinal study. Child Development. 2005;76(5):1055–1071. doi: 10.1111/j.1467-8624.2005.00897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elzinga BM, Roelofs K, Tollenaar MS, Bakvis P, van Pelt J, Spinhoven P. Diminished cortisol response to psychosocial stress associated with lifetime adverse effects: A study among healthy young subjects. Psychoneuroendocrinology. 2008;33:227–237. doi: 10.1016/j.psyneuen.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Boyce WT, Hertzman C, Lam LL, Armstrong JM, Neumann SMA, Kobor MS. Epigenetic vestiges of early developmental adversity: Childhood stress exposure and DNA methylation in adolescence. Child Development. doi: 10.1111/j.1467-8624.2011.01641.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estaugh V, Power C. Family disruption in early life and drinking in young adulthood. Alcohol and Alcoholism. 1991;26:639–644. doi: 10.1093/oxfordjournals.alcalc.a045168. [DOI] [PubMed] [Google Scholar]
- Evans GW, English K. The environment of poverty: multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Development. 2002;73:1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- Evans GW, Gonnella C, Marcynszyn LA, Gentile L, Salpekar N. The role of chaos in poverty and children’s socioemotional adjustment. Psychological Science. 2005;16:460–565. doi: 10.1111/j.0956-7976.2005.01575.x. [DOI] [PubMed] [Google Scholar]
- Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychological Science. 2007;18:953–7. doi: 10.1111/j.1467-9280.2007.02008.x. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Flinn MV, Quinlan RJ, Decker SA, Turner MT, England BG. Male-female differences in effects of parental absence on glucocorticoid stress response. Human Nature. 1996;7:125–162. doi: 10.1007/BF02692108. [DOI] [PubMed] [Google Scholar]
- Fox E, Ridgewell A, Ashwin C. Looking on the bright side: biased attention and the human serotonin transporter gene. Proceedings of the Royal Society B. 2009;276:1747–1751. doi: 10.1098/rspb.2008.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gersten J, Beals J, Kallgren C. Epidemiology and preventive interventions: Parental death in childhood as a case example. American Journal of Community Psychology. 1991;19:481–499. doi: 10.1007/BF00937988. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Children of depressed parents: Mechanisms of risk and Implications for treatment. Washington DC: American Psychology Association; 2002. [Google Scholar]
- Grant KE, Compas BE, Stuhlmacher AG, Thurm AE, McMahon SD, Halpert JA. Stressors and child and adolescent psychopathology: Moving from markers to mechanisms of risk. Psychological Bulletin. 2003;129:447–466. doi: 10.1037/0033-2909.129.3.447. [DOI] [PubMed] [Google Scholar]
- Gump BB, Reihman J, Stewart P, Lonky E, Darvill T, Granger DA, Matthews K. Trajectories of maternal depressive symptoms over her child’s life span: Relation to adrenocortical, cardiovascular, and emotional functioning in children. Development and Psychopathology. 2009;21(1):207–225. doi: 10.1017/S0954579409000133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan M, Luecken LJ, Sandler IN, Tien JY. Prospective effects of post-bereavement negative events on cortisol activity in parentally bereaved youth. Developmental Psychobiology. 2010;52:394–400. doi: 10.1002/dev.20433. [DOI] [PubMed] [Google Scholar]
- Hagan M, Roubinov D, Gress J, Luecken LJ, Sandler I, Wolchik S. Positive parenting during childhood moderates the impact of recent negative events on cortisol activity in parentally bereaved youth. Psychopharmacology. 2011;214:231–238. doi: 10.1007/s00213-010-1889-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haine RA, Ayers TS, Sandler IN, Wolchik SA, Weyer JL. Locus of control and self-esteem as stress-moderators or stress-mediators in parentally bereaved children. Death Studies. 2003;27:619–640. doi: 10.1080/07481180302894. [DOI] [PubMed] [Google Scholar]
- Haine RA, Wolchik SA, Sandler IN, Millsap RE, Ayers TS. Positive parenting as a protective resource for parentally bereaved children. Death Studies. 2006;30:1–28. doi: 10.1080/07481180500348639. [DOI] [PubMed] [Google Scholar]
- Harris TO, Brown GW, Bifulco AT. Loss of parent and adult psychiatric disorder: The role of lack of adequate parental care. Psychological Medicine. 1986;16:641–659. doi: 10.1017/s0033291700010394. [DOI] [PubMed] [Google Scholar]
- Hertzman C. The biological embedding of early experience and its effects on health in adulthood. Annals of the N Y Academy of Sciences. 1999;896:85–95. doi: 10.1111/j.1749-6632.1999.tb08107.x. [DOI] [PubMed] [Google Scholar]
- Johnson CL, Barer BM. Life course effects of early parental loss among very old African Americans. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2002;57:108–116. doi: 10.1093/geronb/57.2.s108. [DOI] [PubMed] [Google Scholar]
- Joormann J, Gotlib IH. Emotion-regulation in depression: Relation to cognitive inhibition. Cognition and Emotion. 2010;24:281–298. doi: 10.1080/02699930903407948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalter N, Lohnes KL, Chasin J, Cain AC, Dunning S, Rowan J. The adjustment of parentally bereaved children: Factors associated with short-term adjustment. Omega: Journal of Death and Dying. 2002;46:15–34. [Google Scholar]
- Karg K, Burmeister M, Shedden K, Sen S. The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: evidence of genetic moderation. Archives of General Psychiatry. 2011;68:444–454. doi: 10.1001/archgenpsychiatry.2010.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Childhood parental loss and adult psychopathology in women. Archives of General Psychiatry. 1992;49:109–116. doi: 10.1001/archpsyc.1992.01820020029004. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. American Journal of Psychiatry. 2002;159:1133–1145. doi: 10.1176/appi.ajp.159.7.1133. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. American Journal of Psychiatry. 2006;163:115–124. doi: 10.1176/appi.ajp.163.1.115. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Sheth K, Gardner CO, Prescott CA. Childhood parental loss and risk for first-onset of major depression and alcohol dependence: the time-decay of risk and sex differences. Psychological Medicine. 2002;32(7):1187–1194. doi: 10.1017/s0033291702006219. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the U.S. National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kinnally EL, Huang Y, Haverly R, Burke AK, Galfalvy H, Brent DP, Oquendo MA, Mann JJ. Parental care moderates the influence of MAOA-uVNTR genotype and childhood stressors on trait impulsivity and aggression in adult women. Psychiatric Genetics. 2009;19:126–133. doi: 10.1097/YPG.0b013e32832a50a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivela S, Luukinen H, Koski K, Viramo P, Kimmo P. Early loss of mother or father predicts depression in old age. International Journal of Geriatric Psychiatry. 1998;13:527–530. doi: 10.1002/(sici)1099-1166(199808)13:8<527::aid-gps814>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Krause N. Early parental loss, recent life events, and changes in health among older adults. Journal of Aging and Health. 1998;10:395–421. doi: 10.1177/089826439801000401. [DOI] [PubMed] [Google Scholar]
- Kreek MJ, Nielsen DA, Butelman ER, LaForge KS. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nature Neuroscience. 2005;8:1450–1457. doi: 10.1038/nn1583. [DOI] [PubMed] [Google Scholar]
- Kwang T, Wells TT, McGeary JE, Swann WB, Jr, Beevers CG. Association of the serotonin transporter promoter region polymorphism with biased attention for negative word stimuli. Depression and Anxiety. 2010;27:746–51. doi: 10.1002/da.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok OM, Haine R, Sandler IN, Ayers TS, Wolchik SA. Positive parenting as a mediator of the relations between parental psychological distress and mental health problems of parentally-bereaved children. Journal of Clinical Child and Adolescent Psychology. 2005;34:261–272. doi: 10.1207/s15374424jccp3402_5. [DOI] [PubMed] [Google Scholar]
- Lehman BJ, Taylor SE, Kiefe CI, Seeman TE. Relationship of early life stress and physiological functioning to blood pressure in the CARDIA study. Health Psychology. 2009;28:338–346. doi: 10.1037/a0013785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin KK, Sandler IN, Ayers TS, Wolchik SA, Luecken LJ. Resilience in parentally-bereaved children and adolescents: Family, child, and stress variables. Journal of Clinical Child and Adolescent Psychology. 2004;33:673–683. doi: 10.1207/s15374424jccp3304_3. [DOI] [PubMed] [Google Scholar]
- Lowman BC, Drossman DA, Cramer EM, McKee DC. Recollection of childhood events in adults with irritable bowel syndrome. Journal of Clinical Gastroenterology. 1987;9(3):324–30. doi: 10.1097/00004836-198706000-00017. [DOI] [PubMed] [Google Scholar]
- Luecken LJ. Childhood attachment and loss experiences affect adult cardiovascular and cortisol function. Psychosomatic Medicine. 1998;60:765–772. doi: 10.1097/00006842-199811000-00021. [DOI] [PubMed] [Google Scholar]
- Luecken LJ. Attachment and loss experiences during childhood are associated with adult hostility, depression, and social support. Journal of Psychosomatic Research. 2000a;49(1):85–91. doi: 10.1016/s0022-3999(00)00151-3. [DOI] [PubMed] [Google Scholar]
- Luecken LJ. Parental caring and loss during childhood and adult cortisol responses to stress. Psychology and Health. 2000b;15:841–851. [Google Scholar]
- Luecken LJ. Long-term consequences of parental death in childhood: Physiological and psychological manifestations. In: Stroebe M, Hansson RO, Schut H, Stroebe W, editors. Handbook of Bereavement Research and Practice: 21st Century Perspectives. American Psychological Association Press; 2008. [Google Scholar]
- Luecken LJ, Appelhans B. Information-processing biases in young adults from bereaved and divorced families. Journal of Abnormal Psychology. 2005;114:309–313. doi: 10.1037/0021-843X.114.2.309. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Appelhans BM. Early parental loss and cortisol stress responses in young adulthood: The moderating role of family environment. Development and Psychopathology. 2006;18:295–308. doi: 10.1017/S0954579406060160. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Appelhans BM, Kraft A, Brown A. Never far from home: A cognitive-affective model of the impact of early-life family relationships on physiological stress responses in adulthood. Journal of Social and Personal Relationships. 2006;23(2):189–203. [Google Scholar]
- Luecken LJ, Appelhans BA, Kraft AJ, Enders C. Emotional and cardiovascular sensitization to daily stress following childhood parental loss. Developmental Psychology. 2009;45(1):296–302. doi: 10.1037/a0013888. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Hagan MJ, Sandler IN, Tien J, Ayers TS, Wolchik SA. Cortisol levels six-years after participation in the Family Bereavement Program. Psychoneuroendocrinology. 2010;35:785–789. doi: 10.1016/j.psyneuen.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecken LJ, Lemery K. Early caregiving and adult physiological stress responses. Clinical Psychology Review. 2004;24:171–191. doi: 10.1016/j.cpr.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Rodriguez AP, Appelhans BM. Cardiovascular stress responses in young adulthood associated with family-of-origin relationship experiences. Psychosomatic Medicine. 2005;67:514–521. doi: 10.1097/01.psy.0000160466.10397.18. [DOI] [PubMed] [Google Scholar]
- Lundberg U. Stress hormones in health and illness: The role of work and gender. Psychoneuroendocrinology. 2005;30:1017–1021. doi: 10.1016/j.psyneuen.2005.03.014. [DOI] [PubMed] [Google Scholar]
- Lutzke JR, Ayers TS, Sandler IN, Barr A. Risks and interventions for the parentally bereaved child. In: Wolchik S, Sandler I, editors. Handbook of children’s coping: Linking theory and intervention. New York: Plenum Press; 1997. pp. 215–244. [Google Scholar]
- Mack KY. Childhood family disruption and adult well-being: The differential effects of divorce and parental death. Death Studies. 2001;25:419–443. doi: 10.1080/074811801750257527. [DOI] [PubMed] [Google Scholar]
- Maier EH, Lachman ME. Consequences of early parental loss and separation for health and well-being in midlife. International Journal of Behavioral Development. 2000;24:183–189. [Google Scholar]
- Marwit SJ, Carusa SS. Communicated support following loss: Examining the experiences of parental death and parental divorce in adolescence. Death Studies. 1998;22:237–255. doi: 10.1080/074811898201579. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections. Annals of the New York Academy of Sciences. 2010;1186:146–173. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- Mauss IB, Bunge SA, Gross JJ. Automatic emotion regulation. Social and Personality Compass. 2007;1:146–167. [Google Scholar]
- McCrory, De Brito, Viding Research review: The neurobiology and genetics of maltreatment and adversity. Journal of Child Psychology and Psychiatry. 2010;51:1079–1095. doi: 10.1111/j.1469-7610.2010.02271.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Hormones and Behavior. 2003;43:2–15. doi: 10.1016/s0018-506x(02)00024-7. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53:185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Fok AK, Walker H, Lim A, Nicholls EF, Cole S, Kober Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proceedings of the National Academy of Sciences. 2009;106:14716–14721. doi: 10.1073/pnas.0902971106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mireault GC, Bond LA. Parental death in childhood: Perceived vulnerability and adult depression and anxiety. American Journal of Orthopsychiatry. 1992;62:517–524. doi: 10.1037/h0079371. [DOI] [PubMed] [Google Scholar]
- Mortensen PB, Pedersen CB, Melbye M, Mors O, Ewald H. Individual and familial risk factors for bipolar affective disorders in Denmark. Archives of General Psychiatry. 2003;60:1209–1215. doi: 10.1001/archpsyc.60.12.1209. [DOI] [PubMed] [Google Scholar]
- Neeleman J, Sytema S, Wadsworth M. Propensity to psychiatric and somatic ill-health: evidence from a birth cohort. Psychological Medicine. 2002;32:793–803. doi: 10.1017/s0033291702005901. [DOI] [PubMed] [Google Scholar]
- Nicolson NA. Childhood parental loss and cortisol levels in adult men. Psychoneuroendocrinology. 2004;29(8):1012–1018. doi: 10.1016/j.psyneuen.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Pfeffer CR, Altemus M, Heo M, Jiang H. Salivary cortisol and psychopathology in children bereaved by the September 11, 2001 terror attacks. Biological Psychiatry. 2007;61:957–965. doi: 10.1016/j.biopsych.2006.07.037. [DOI] [PubMed] [Google Scholar]
- Pesonen A, Räikkönen K, Feldt K, Heinonen K, Osmond C, Phillips DIW, Barker DJP, Eriksson JG, Kajantie E. Childhood separation experience predicts HPA axis hormonal responses in late adulthood: A natural experiment of World War II. Psychoneuroendocrinology. 2010;35:758–767. doi: 10.1016/j.psyneuen.2009.10.017. [DOI] [PubMed] [Google Scholar]
- Phillips AC. Blunted cardiovascular reactivity relates to depression, obesity, and self-reported health. Biological Psychology. 2011;86:106–113. doi: 10.1016/j.biopsycho.2010.03.016. [DOI] [PubMed] [Google Scholar]
- Ragan PV, McGlashan TH. Childhood parental death and adult psychopathology. The American Journal of Psychiatry. 1986;143:153–157. doi: 10.1176/ajp.143.2.153. [DOI] [PubMed] [Google Scholar]
- Räikkönen K, Lahti M, Heinonen K, Pesonen A, Wahlbeck K, Kajantie E, Osmond C, Barker DJP, Eriksson JG. Risk of severe mental disorders in adults separated temporarily from their parents in childhood: The Helsinki birth cohort study. Journal of Psychiatric Research. 2011;45 doi: 10.1016/j.jpsychires.2010.07.003. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. [PubMed] [Google Scholar]
- Sandler IN. Quality and ecology of adversity as common mechanisms of risk and resilience. American Journal of Community Psychology. 2001;29:19–61. doi: 10.1023/A:1005237110505. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Ayers TS, Wolchik SA, Tein JY, Kwok OM, Haine RA, Twohey-Jacobs J, Suter J, Lin K, Padgett-Jones S, Weyer JL, Cole E, Kriege G, Griffin WA. The family bereavement program: efficacy evaluation of a theory-based prevention program for parentally bereaved children and adolescents. Journal of Consulting and Clinical Psychology. 2003;71(3):587–600. doi: 10.1037/0022-006x.71.3.587. [DOI] [PubMed] [Google Scholar]
- Sandler I, Ayers TS, Tein JY, Wolchik A, Millsap R, Khoo ST, Kaplan D, Ma Y, Luecken L, Schoenfelder E, Coxe S. Six-year follow-up of a preventive intervention for parentally-bereaved youth: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2010;164:907–914. doi: 10.1001/archpediatrics.2010.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Wolchik SA, Ayers TS, Tein J-Y, Coxe S, Chow W. Linking theory and intervention to promote resilience in parentally-bereaved children. In: Stroebe M, Hansson RO, Schut H, Stroebe W, editors. Handbook of Bereavement Research and Practice: 21st Century Perspectives. American Psychological Association Press; 2008. [Google Scholar]
- Sheffield Morris A, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Short JL. The effects of parental divorce during childhood on college students. Journal Divorce and Remarriage. 2008;38:143–155. [Google Scholar]
- Silverman P, Worden J. Children’s reactions in the early months after the death of a parent. American Journal of Orthopsychiatry. 1992;62:93–104. doi: 10.1037/h0079304. [DOI] [PubMed] [Google Scholar]
- Slavich GM, Monroe SM, Gotlib IH. Early parental loss and depression history: Associations with recent life stress in major depressive disorder. Journal of Psychiatric Research. doi: 10.1016/j.jpsychires.2011.03.004. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohr-Preston SL, Scaramella LV. Implications of timing of maternal depressive symptoms and early cognitive and language development. Clinical Child and Family Psychology Review. 2006;9(1):65–83. doi: 10.1007/s10567-006-0004-2. [DOI] [PubMed] [Google Scholar]
- Social Security Administration. Intermediate Assumptions of the 2000 Trustees Report. Washington, DC: Office of the Chief Actuary of the Social Security Administration; 2000. [Google Scholar]
- Stewart JC, France CR. Cardiovascular recovery from stress predicts longitudinal changes in blood pressure. Biological Psychology. 2001;58:105–120. doi: 10.1016/s0301-0511(01)00105-3. [DOI] [PubMed] [Google Scholar]
- Stroebe W, Stroebe M. Determinants of adjustment to bereavement in younger widows and widowers. In: Stroebe M, Stroebe W, Hansson R, editors. Handbook of bereavement: Theory, research, and intervention. New York: Cambridge University Press; 1993. pp. 208–226. [Google Scholar]
- Sroufe LA. Attachment and development: A prospective, longitudinal study from birth to adulthood. Attachment and Human Development. 2005;7:349–367. doi: 10.1080/14616730500365928. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Way BM, Seeman TE. Early adversity and adult health outcomes. Development and Psychopathology. 2011;23:939–954. doi: 10.1017/S0954579411000411. [DOI] [PubMed] [Google Scholar]
- Tennant C. Parent loss in childhood: Its effects in adult life. Archives of General Psychiatry and Clinical Neuroscience. 1988;45:1045–1050. doi: 10.1001/archpsyc.1988.01800350079012. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kaslow NJ, Price AW, Williams K, Kingree JB. Role of secondary stressors in the parental death-child distress relation. Journal of Abnormal Child Psychology. 1998;26:357–366. doi: 10.1023/a:1021951806281. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA. What are the costs of marital conflict and dissolution t to children’s physical health? Clinical Child and Family Psychology Review. 2004;7:29–57. doi: 10.1023/b:ccfp.0000020191.73542.b0. [DOI] [PubMed] [Google Scholar]
- Tyrka AR, Price LH, Gelernter J, Schepker C, Anderson GM, Carpenter LL. Interaction of childhood maltreatment with the corticotropin-releasing hormone receptor gene: Effects on HPA axis reactivity. Biological Psychiatry. 2008;66:681–685. doi: 10.1016/j.biopsych.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Beek JHDA, Kendler KS, de Moor MHM, Geels LM, Bartels M, Vink JM, et al. Stable genetic effects on symptoms of alcohol abuse and dependence from adolescence into early adulthood. Behavior Genetics. 2011 doi: 10.1007/s10519-011-9488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhes E, Scarpa A. The effects of childhood maltreatment on the hypothalamic-pituitary-adrenal axis. Trauma, Violence & Abuse. 2004;5:333–352. doi: 10.1177/1524838004269486. [DOI] [PubMed] [Google Scholar]
- Veijola J, Läärä E, Joukamaa M, Isohanni M, Hakko H, Haapea M, Pirkola S, Mäki P. Temporary parental separation at birth and substance use disorder in adulthood. A long-term follow-up of the Finnish Christmas Seal Home Children. Social Psychiatry and Psychiatric Epidemiology. 2008;43:11–7. doi: 10.1007/s00127-007-0268-y. [DOI] [PubMed] [Google Scholar]
- Wandersman A, Nation M. Urban neighborhoods and mental health: Psychological contributions to understanding toxicity, resilience, and interventions. American Psychologist. 1998;53:647–656. [PubMed] [Google Scholar]
- Waters E, Merrick S, Treboux D, Crowell J, Albersheim L. Attachment security in infancy and early adulthood: A twenty-year longitudinal study. Child Development. 2000;71:684–689. doi: 10.1111/1467-8624.00176. [DOI] [PubMed] [Google Scholar]
- Weller RA, Weller EB, Fristad MA, Bowes JM. Depression in recently bereaved prepubertal children. Journal of Psychiatry. 1991;148:1536–1540. doi: 10.1176/ajp.148.11.1536. [DOI] [PubMed] [Google Scholar]
- Wolchik SA, Tein JY, Sandler IN, Ayers TS. Stressors, quality of the child-caregiver relationship, and children’s mental health problems after parental death: The mediating role of self-system beliefs. Journal of Abnormal Child Psychology. 2006;34:221–238. doi: 10.1007/s10802-005-9016-5. [DOI] [PubMed] [Google Scholar]
- Worden JW. Children and grief: when a parent dies. New York: Guilford Press; 1996. [Google Scholar]
- Worden JW, Silverman PR. Parental death and the adjustment of school-aged children. Omega Journal of Death and Dying. 1996;33:91–102. [Google Scholar]


