Abstract
Background
The first year of graduate medical education is an important period in the professional development of physicians. Disruptive behavior interferes with safe and effective clinical practice.
Objective
To determine the frequency and nature of disruptive behavior perceived by interns and attending physicians in a teaching hospital environment.
Method
All 516 interns at Partners HealthCare (Boston, MA) during the 2010 and 2011 academic years were eligible to complete an anonymous questionnaire. A convenience nonrandom sample of 40 attending physicians also participated.
Results
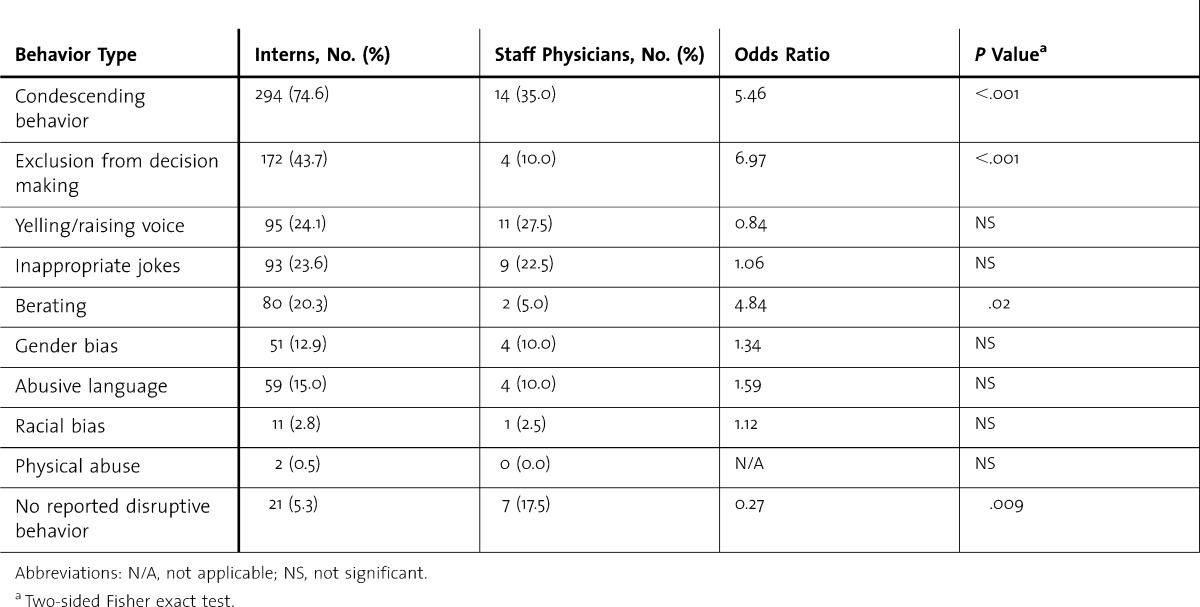
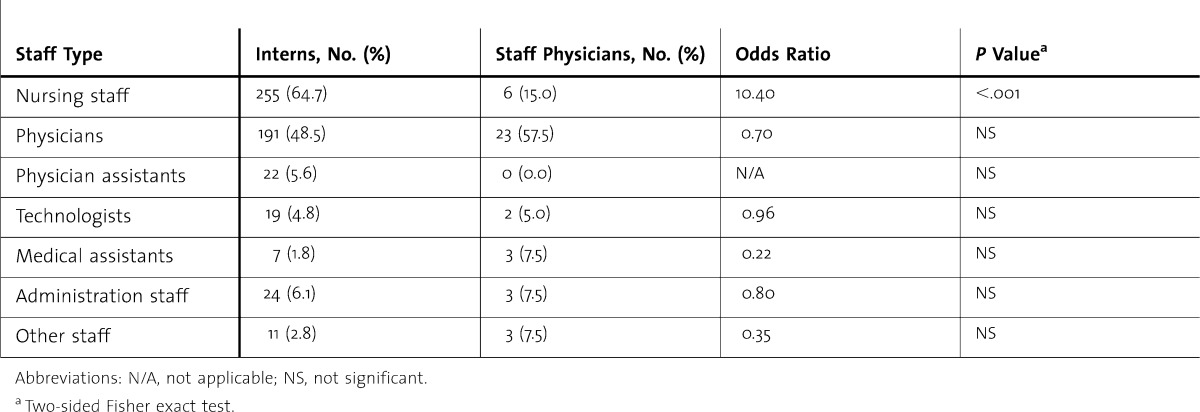
A total of 394 of 516 eligible interns (76.4%) participated. Attendings and interns each reported that their team members generally behaved professionally (87.5% versus 80.4%, respectively). A significantly greater proportion of attendings than interns felt respected at work (90.0% versus 71.5% respectively; P = .01). Disruptive behavior was experienced by 93% of interns; 54% reported that they experienced it once a month or more. Interns reported disruptive behavior significantly more frequently than attending physicians, including increased reports of condescending behavior (odds ratio [OR], 5.46 for interns compared with attendings; P < .001), exclusion from decision making (OR, 6.97; P < .001), and berating (OR, 4.84; P = .02). Inappropriate jokes, abusive language, and gender bias were also reported, and they were not significantly more frequent among interns than attending physicians. Interns most frequently identified nurses as the source of disruption, and were significantly more likely than faculty to identify nurses as the source of disruptive behavior (OR, 10.40; P < .001). Attendings reported other physicians as the most frequent source of disruption.
Conclusions
Although interns generally feel respected at work, they frequently experience disruptive behavior. Interns described more disruptive behaviors than a convenience sample of attending physicians at our institution.
Editor's Note: The online version of the article contains the survey instrument (24.8KB, docx) used in this study.
What was known
Disruptive behavior by members of the health care team interferes with safe and effective clinical practice.
What is new
A survey finds interns generally feel respected at work, but they experience disruptive behavior at a greater frequency than a convenience sample of attending physicians.
Limitations
Single health care system study limits generalizability; data were self-reported, and the anonymous nature of data collection limits the ability to explore the contexts in which disruptive behavior occurred.
Bottom line
Interns report disruptive behavior at a greater rate than attending physicians, cite nurses as a frequent source, and describe condescending behavior, exclusion from decision making, and berating as commonly experienced behaviors. Addressing these findings will require a change in institutional culture.
Introduction
The first year of graduate medical education is an important period in physicians' professional development. The extent to which interns experience or witness perceived disruptive behavior in the workplace may affect their own behavior and the development of future professional relationships. Abusive behavior has been identified as a source of stress among residents, leading to burnout and decreased satisfaction with training.1 Communicating in an effective and respectful manner with patients and staff is one of the general competencies that the Accreditation Council for Graduate Medical Education (ACGME) expects residents to attain.2 Disruptive behavior leads not only to poor interprofessional relationships, but can be a source of adverse patient outcomes by interfering with effective communication among health care staff.3–5
The Joint Commission and the ACGME standards indicate the importance of addressing disruptive behavior among physicians and trainees.6,7 These organizations acknowledge that disruptive behavior is a national problem needing regulatory oversight, and they advocate for the implementation of systems to identify unprofessional conduct by health care team members and provide the opportunity for remediation.8 The aim of this study was to determine the frequency and nature of disruptive behavior perceived by interns and a representative sample of clinically active attending physicians in an academic medical center environment. We also sought to determine whether there were any differences between the groups regarding the type and source of disruption.
Methods
Setting and Participants
A total of 394 interns from diverse residency programs from one large health care organization (Partners HealthCare) who attended a required session on professionalism in academic years 2010 and 2011 were invited to complete a questionnaire. The participants were not incentivized to participate in the study. Forty attending physicians from the same organization who were active on the inpatient teaching service were invited to complete the same questionnaire while attending a similar program on professionalism.
Survey Instrument and Administration
A questionnaire was developed by reviewing the literature to determine frequent sources and types of disruptive behavior reported in health care organizations and by drawing on the authors' experience working on professionalism issues with residents.3,9–11 The resulting instrument was reviewed by a panel of expert colleagues to establish face validity. It was then edited by the authors and piloted in a series of focus groups with 18 trainees and attendings. In the focus groups, the participants completed the survey and then shared their interpretation of the meaning of each question. The prompts were then rewritten for interpretative clarity. The final questionnaire comprised 11 items requiring single or multiple closed responses (the instrument is provided as online supplemental material). In addition to basic demographic data, the items explored the frequency, nature, and source of disruptive behavior experienced during clinical assignments. Participants were asked to reflect on their work environment (hospital, clinics, and other sites within the institution) when completing the questionnaire. Types of disruptive behavior included abusive language, inappropriate jokes, yelling, racial and gender bias, berating, exclusion from decision making, condescending behavior, and physical abuse. Respondents were asked to consider the staff group or groups who were the source of disruptive behavior (physicians, nursing staff, medical assistants, administration staff, physician assistants, technologists, or other staff groups). The questionnaire was administered to interns using an audience response system (TurningPoint, Turning Technologies, Youngstown, OH) to facilitate confidential and efficient data acquisition.
Data collection was performed immediately prior to commencement of the professionalism training session. A concise description of the study and its aims was provided, indicating that data collection would be anonymous. It was made clear to attendees that they were free to opt out of the survey, and participation or nonparticipation would have no effect on the subsequent training session or their standing. Keypads for the audience response system were then distributed. At the time of the study, all interns had completed approximately 8 months of postgraduate medical training. The interns did not confer while completing the questionnaire using the audience response system, and were not able to view responses from other attendees. The data collected were anonymized. Attending physicians were able to self-select a date to attend the professionalism program, and these sessions were conducted in smaller groups at flexible times to accommodate their schedules. Attending physicians were also informed that they were under no obligation to complete the survey and that responses were collected and evaluated anonymously. All 40 attending physicians participating in the professionalism program completed the paper questionnaire. This level of confidentiality limited our ability to examine the effect of specialty or unit on responses. All surveys were filled out just prior to the start of the professionalism training session.
Ethical approval for this study was obtained from the Institutional Review Board of Partners HealthCare.
Analysis
Statistical analysis was performed, including the use of 2-sided Fisher exact test for comparison of variables between interns and attendings. Significance was determined using as P < .05.
Results
All 394 interns invited to participate in the study completed the questionnaire. Participating interns represented 76.4% of the 516 first-year trainees at our hospitals. Although all participants answered at least one question, several interns did not provide responses to all items, as noted below. Of the respondents, 180 interns (48.1%) were women, 194 were men, and 20 participants did not indicate sex when completing the questionnaire. Most of the interns (246; 64.9%) were younger than 30 years, 132 (34.8%) were ages 30–39 years, and 15 did not indicate age. Forty attendings completed the questionnaire, including 11 women (27.5%) and 29 men (72.5%). Among attending physicians, 17 (42.5%) were ages 30–39 years, 8 (20.0%) were ages 40–49 years, and 15 (37.5%) were older than 50 years.
Most interns (80.4%) and attending physicians (87.5%) indicated that professional behavior among work colleagues was the norm (P = .30). Although most interns (71.5%) felt respected at work, this was significantly lower than the 90.0% of attendings who reported feeling respected (P = .01).
Interns reported a higher frequency of disruptive behavior than attending physicians. Most interns (93%) reported disruptive behaviors, compared with 45% of faculty (P < .001). Furthermore, 54.4% of interns encountered disruptive behavior at least once per month, compared with 15.0% of faculty (odds ratio [OR], 6.76; P < .001); 70.3% of interns had experienced disruptive behavior from 2 or more work colleagues in the prior 6 months, compared with 17.5% of attending physicians (OR, 11.16; P < .001). The age of the intern respondents was not associated with their likelihood of reporting disruptive behavior.
table 1 shows the types of disruptive behavior experienced by participants (participants were able to choose all behavior types that applied). Condescending behavior, exclusion from decision making, and berating were significantly more frequently reported by interns than faculty. Yelling/raising of voice, inappropriate jokes, abusive language, and gender bias were reported frequently by interns (table 1), but there was no significant difference compared with attendings for these types of behavior.
table 1.
Types of Disruptive Behavior Experienced by Participants
When asked to indicate the most typical source of disruptive behavior, 48.6% of interns identified nonphysician health care team members, compared with 37.5% of faculty physicians. table 2 shows that most interns indicated that nurses were the source of most of the perceived disrespectful behavior in the work environment, compared with 15.0% of attending physicians (P < .001). Disrespectful actions by other health care team members most frequently occurred in person for both interns (62.8%) and attendings (74.3%). However, a minority of interns (29.9%) most frequently experienced disrespect during telephone interactions, which was significantly greater than the 8.6% of faculty staff who reported this finding (P = .009).
table 2.
Professional Groups Identified as a Cause of Disruptive Behavior by Participants
Discussion
Our findings indicate that interns generally feel respected at work, but most experience and witness perceived disruptive behavior from colleagues of various disciplines. Participants' age and sex did not have a significant effect on responses. Nurses are identified by most interns as the source of disruptive behavior, whereas attending physicians are most likely to experience such behavior from other physicians.
Data obtained by the American College of Physician Executives indicate that 95% of senior physicians regularly encounter disruptive behavior from hospital staff.12 This type of disruptive behavior by health care staff leads to poor communication and suboptimal patient care.3 Poor communication is commonly identified as a contributory cause of sentinel events13 and patient dissatisfaction.14,15 Approximately 1 in 6 health care staff members in a multicenter survey could recall specific adverse events caused by disruptive behavior.16 Prior negative behavior at medical school is a predictor of later poor professional performance,17 emphasizing the importance of professional conduct throughout training. Effective communication skills are essential for competent clinical practice and patient safety. Interns need their communication skills reinforced and strengthened during postgraduate training because this is a time when interactions with nurses, physicians, and other health professionals are not only frequent but also critical for effective patient care. Modeling highly professional interactions would be expected to foster professionalism among residents and students.18
In addition to diminishing professional development, stress caused by problematic work relationships may contribute to burnout among interns. Research has shown that residents experience high levels of burnout19 and report greater rates of self-perceived error due to fatigue and distress.20 Burnout is also recognized as a frequent problem among academic faculty,21 contributing to absenteeism and high rates of staff turnover.22,23 Decreased job satisfaction may also have an adverse effect on development of professionalism,1 and can lead to cynicism and low morale.23 By exacerbating training stress, disruptive behavior may therefore inhibit effective group dynamics between physicians and other hospital staff. Because effective patient care depends on physicians working in teams,24 it is important to raise awareness of barriers to collaborative practice.
The finding that interns reported nurses as the most frequent source of disruptive behavior likely reflects the context in which interns practice. Interns spend a greater proportion of time in the patient care environment, and therefore they work alongside nursing staff on a more frequent basis. Communication barriers between physicians and nurses have been explored in various studies, highlighting discrepant attitudes relating to teamwork and perceived scope of practice.25,26 Conflicting ideas on collaboration between nurses and the respective work for the two types of health care professionals may be more pronounced for interns, who have less authority for decision making and team leadership compared with faculty physicians. An evolving awareness of the expectations of nurses and other colleagues is a key element of the transition from resident to attending.27 Greater awareness of roles and responsibilities, as well as increased competence that develops with increasing seniority, may play a role in limiting both disruptive behavior and the perception of disruptive behavior.
“Exclusion from decision making” was frequently experienced by interns in this study. The findings are consistent with other studies, which have described lack of autonomy and lack of influence on work planning as causes of reduced job satisfaction among residents.19 Exclusion not only feels terrible and negatively affects self-esteem, but it can also lead to distorted perception and decision making.28
Changing an institution's culture to address prevalent behavior change is not easy. In addition to providing resources to advise on, manage, remediate, and track disruptive behaviors and individuals, a more system-wide effort to clarify expectations and train individuals on how to manage the behavior is needed. Efforts to promote more effective interprofessional collaboration and teamwork, as well as reflective exercises to help professionals identify their own behaviors and recognize disruption, are needed.29,30 Shared awareness of disruptive and disrespectful behavior is a key component of systems that effectively manage unprofessional conduct in hospitals.31,32 Because disruptive behavior can be a manifestation of burnout, measures that promote meaning in work have been advocated as a method of reducing burnout among physicians,33 since job satisfaction has a protective effect against burnout.34 Our institution has a dedicated program aimed at fostering the principles of professional practice; there is also an institution-wide process to investigate and resolve unprofessional behavior.
Our study has several limitations. First, the data collated in this study were self-reported by interns and attending physicians, and were therefore not objectively confirmed. Because individual study participants may have different perspectives on the nature of disruptive behavior, the lack of objective data is a limitation of the study. Second, the anonymous nature of data collection limits the ability to determine the specific context where any disruptive behavior occurred. However, the inclusion of many different types of interns and the consistency of the reports indicate that the issue is not localized to a specific clinical unit or center. Third, the interns participating in the study were working in the environment of several hospitals associated with one health care organization, and it may not be possible to generalize the findings to other institutions.
By asking the interns to complete the questionnaire 8 months after the commencement of graduate training, the authors considered that participants would have had adequate time to experience several of our treatment units and reflect more accurately on the interprofessional dynamics of the hospitals' environments than they would have at an earlier stage of internship. Residents have previously been shown to respond reliably to other surveys.35 Therefore, a survey tool on disruptive behavior with participation by most interns in a large training program may provide valid data. We surmise that the anonymity of the reports is more likely to be reflective of the true perceptions of the respondents than could be achieved through other approaches. Although it is important to acknowledge the subjective nature of these perceptions, even perceived problem behavior might affect professional development, whether or not the behavior can be objectively demonstrated. Although we report data from several hospitals associated with one large integrated health care system, the work environment is likely to be similar to several other large academic institutions throughout the United States, which are bound by uniform training requirements. There are no directly comparable published data from other institutions, yet our findings are consistent with other studies that have indicated that stress in work relationships contributes to emotional distress and burnout among residents.19,36
Conclusions
In this single-institution study of interns from diverse specialties, interns reported high levels of professionalism in their clinical interactions during the first 8 months of training. However, most interns experienced some form of disruptive behavior at least once per month. The frequency of perceived disruptive behavior was greater for interns than a convenience sample of attending physicians at the same institution. Interns perceived that nurses were the most frequent source of these disruptions, whereas attendings reported that their peers were the most frequent source.
Footnotes
Charles P. Mullan, MB, MMSc, is Staff Radiologist in the Department of Radiology, Altnagelvin Hospital, Derry, Northern Ireland; Jo Shapiro, MD, is Chief of the Division of Otolaryngology and and Director of the Center for Professionalism and Peer Support, Brigham and Women’s Hospital, and is Associate Professor of Otology and Laryngology, Harvard Medical School; and Graham T. McMahon, MD, MMSc, is Associate Professor of Medicine in the Department of Medicine, Brigham and Women’s Hospital, and Harvard Medical School.
Funding: The authors report no external funding source for this study.
The authors wish to thank Jessica Perlo and Sara Nadelman for assistance in data acquisition.
References
- 1.Mareiniss DP. Decreasing GME training stress to foster residents' professionalism. Acad Med. 2004;79(9):825–831. doi: 10.1097/00001888-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements. https://www.acgme.org/acgmeweb/Portals/0/PDFs/commonguide/IVA5d_EducationalProgram_ACGMECompetencies_IPCS_Documentation.pdf. Accessed January 7, 2013. [Google Scholar]
- 3.Leape LL, Fromson JA. Problem doctors: is there a system-level solution. Ann Intern Med. 2006;144(2):107–115. doi: 10.7326/0003-4819-144-2-200601170-00008. [DOI] [PubMed] [Google Scholar]
- 4.Leape LL, Shore MF, Dienstag JL, Mayer RJ, Edgman-Levitan S, Meyer GS, et al. Perspective: a culture of respect, part 1: the nature and causes of disrespectful behavior by physicians. Acad Med. 2012;87(7):845–852. doi: 10.1097/ACM.0b013e318258338d. [DOI] [PubMed] [Google Scholar]
- 5.Leape LL, Shore MF, Dienstag JL, Mayer RJ, Edgman-Levitan S, Meyer GS, et al. Perspective: a culture of respect, part 2: creating a culture of respect. Acad Med. 2012;87(7):853–858. doi: 10.1097/ACM.0b013e3182583536. [DOI] [PubMed] [Google Scholar]
- 6.Youssi MD. JCAHO standards help address disruptive physician behavior. Physician Exec. 2002;28(6):12–13. [PubMed] [Google Scholar]
- 7.The Joint Commission. Sentinel event alert: behaviors that undermine a culture of safety. http://www.jointcommission.org/sentinel_event_alert_issue_40_behaviors_that_undermine_a_culture_of_safety/. Accessed November 27, 2012. [PubMed] [Google Scholar]
- 8.Harmon L, Pomm RM. Evaluation, treatment and monitoring of disruptive physician behavior. Psychiatr Ann. 2004;34(10):770–774. [Google Scholar]
- 9.Rosenstein AH, O'Daniel M. Managing disruptive physician behavior: impact on staff relationships and patient care. Neurology. 2008;70:1564–1570. doi: 10.1212/01.wnl.0000310641.26223.82. [DOI] [PubMed] [Google Scholar]
- 10.Veltman LL. Disruptive behavior in obstetrics: a hidden threat to patient safety. Am J Obstet Gynecol. 2007;196(6):587.e1–e4. doi: 10.1016/j.ajog.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 11.Rosenstein AH. Nurse-physician relationships: impact on nurse satisfaction and retention. Am J Nurs. 2002;102(6):26–34. doi: 10.1097/00000446-200206000-00040. [DOI] [PubMed] [Google Scholar]
- 12.Weber DO. Poll results: doctors' disruptive behavior disturbs physician leaders. Physician Exec. 2004;30(5):6–14. [PubMed] [Google Scholar]
- 13.The Joint Commission. Sentinel event alert: leadership committed to safety. http://www.jointcommission.org/sentinel_event_alert_issue_43_leadership_committed_to_safety/. Accessed November 27, 2012. [PubMed] [Google Scholar]
- 14.Hickson GB, Federspiel CF, Pichert JW, Miller CS, Gauld-Jaeger J, Bost P. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951–2957. doi: 10.1001/jama.287.22.2951. [DOI] [PubMed] [Google Scholar]
- 15.Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118:1126–1133. doi: 10.1016/j.amjmed.2005.01.060. [DOI] [PubMed] [Google Scholar]
- 16.Rosenstein AH, O'Daniel M. Disruptive behavior and clinical outcomes: perceptions of nurses and physicians. Am J Nurs. 2005;105:54–64. doi: 10.1097/00000446-200501000-00025. [DOI] [PubMed] [Google Scholar]
- 17.Papadakis MA, Teherani A, Banach MA, Knettler TR, Rattner SL, Stern DT, et al. Disciplinary action by medical boards and prior behavior in medical school. N Engl J Med. 2005;353(25):2673–2682. doi: 10.1056/NEJMsa052596. [DOI] [PubMed] [Google Scholar]
- 18.Viggiano TR, Pawlina W, Lindor KD, Olsen KD, Cortese DA. Putting the needs of the patient first: Mayo Clinic's core value, institutional value and professional covenant. Acad Med. 2007;82(11):1089–1093. doi: 10.1097/ACM.0b013e3181575dcd. [DOI] [PubMed] [Google Scholar]
- 19.Thomas NK. Resident burnout. JAMA. 2004;292(23):2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 20.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 21.Dyrbye LN, West CP, Satele D, Sloan JA, Shanafelt TD. Work/Home conflict and burnout among academic internal medicine physicians. Arch Intern Med. 2011;171:1207–1209. doi: 10.1001/archinternmed.2011.289. [DOI] [PubMed] [Google Scholar]
- 22.Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC, et al. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med. 2001;111:170–175. doi: 10.1016/s0002-9343(01)00814-2. [DOI] [PubMed] [Google Scholar]
- 23.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513–519. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 24.Lee TH. Turning doctors into leaders. Harv Bus Rev. 2010;88(4):50–58. [PubMed] [Google Scholar]
- 25.Cadogan MP, Franzi C, Osterweil D, Hill T. Barriers to effective communication in skilled nursing facilities: differences in perception between nurses and physicians. J Am Geriatr Soc. 1999;47(1):71–75. doi: 10.1111/j.1532-5415.1999.tb01903.x. [DOI] [PubMed] [Google Scholar]
- 26.Thomas EJ, Sexton JB, Helmreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med. 2003;31(3):956–959. doi: 10.1097/01.CCM.0000056183.89175.76. [DOI] [PubMed] [Google Scholar]
- 27.Westerman M, Teunissen PW, van der Vleuten CPM, Scherpbier AJ, Siegert CE, van der Lee N, et al. Understanding the transition from resident to attending physician: a transdisciplinary qualitative study. Acad Med. 2010;85:1914–1919. doi: 10.1097/ACM.0b013e3181fa2913. [DOI] [PubMed] [Google Scholar]
- 28.Campbell WK, Krusemark EA, Dyckman KA, Brunell AB, McDowell JE, Twenge JM, et al. A magnetoencephalography investigation of neural correlates for social exclusion and self-control. Soc Neurosci. 2006;1(2):124–134. doi: 10.1080/17470910601035160. [DOI] [PubMed] [Google Scholar]
- 29.Klein EJ, Jackson JC, Kratz L, Marcuse EK, McPhillips HA, Shugerman RP, et al. Teaching professionalism to residents. Acad Med. 2003;78(1):26–33. doi: 10.1097/00001888-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Weller JM, Barrow M, Gasquoine S. Interprofessional collaboration among junior doctors and nurses in the hospital setting. Med Educ. 2011;45(5):478–488. doi: 10.1111/j.1365-2923.2010.03919.x. [DOI] [PubMed] [Google Scholar]
- 31.Hickson GB, Pichert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Acad Med. 2007;82(11):1040–1048. doi: 10.1097/ACM.0b013e31815761ee. [DOI] [PubMed] [Google Scholar]
- 32.Wasserstein AG, Brennan PJ, Rubenstein AH. Institutional leadership and faculty response: fostering professionalism at the University Of Pennsylvania School Of Medicine. Acad Med. 2007;82(11):1049–1056. doi: 10.1097/ACM.0b013e31815763d2. [DOI] [PubMed] [Google Scholar]
- 33.Shanafelt TD. Enhancing meaning in work: a prescription for preventing physician burnout and promoting patient-centered care. JAMA. 2009;302(12):1338–1340. doi: 10.1001/jama.2009.1385. [DOI] [PubMed] [Google Scholar]
- 34.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347:724–728. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 35.Holt KD, Miller RS, Philibert I, Heard JK, Nasca TJ. Residents' perspectives on the learning environment: data from the Accreditation Council for Graduate Medical Education Resident Survey. Acad Med. 2010;85:512–518. doi: 10.1097/ACM.0b013e3181ccc1db. [DOI] [PubMed] [Google Scholar]
- 36.Sargent MC, Sotile W, Sotile MO, Rubash H, Barrack RL. Stress and coping among orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2004;86-A(7):1579–1586. doi: 10.2106/00004623-200407000-00032. [DOI] [PubMed] [Google Scholar]


