Abstract
Background
Heart failure patients have inadequate nutritional intake and alterations in metabolism contributing to an overall energy depleted state. Left ventricular assist device (LVAD) support is a common and successful intervention in patients with end-stage heart failure. LVAD support leads to alterations in cardiac output, functional status, neurohormonal activity and transcriptional profiles but the effects of LVADs on myocardial metabolism are unknown. This study set out to measure cardiac metabolites in non-failing hearts, failing hearts, and hearts post-LVAD support.
Methods
The study population consisted of 8 non-ischemic failing (at LVAD implant) and 8 post-LVAD hearts, plus 8 non-failing hearts obtained from the tissue bank at the University of Colorado. NMR spectroscopy was utilized to evaluate differences in myocardial energy substrates. Paired and non-paired t-tests were used to determine differences between the appropriate groups.
Results
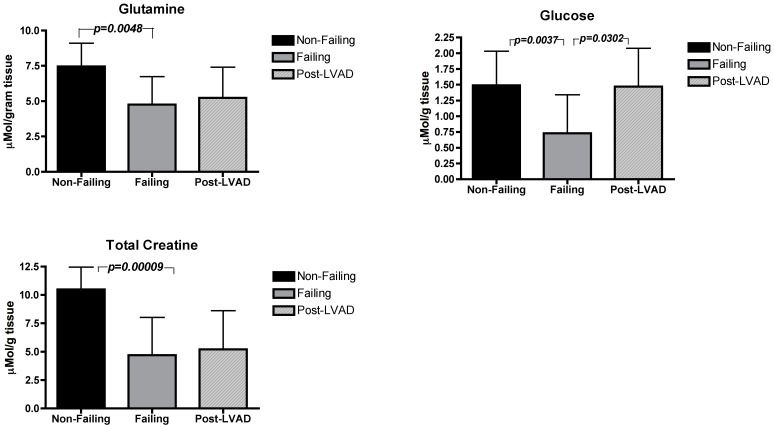
Glucose and lactate values both decreased from non-failing to failing hearts and increased again significantly in the (paired) post-LVAD hearts. Glutamine, alanine, and aromatic amino acids decreased from non-failing to failing hearts and did not change significantly post-LVAD. Total creatine and succinate decreased from non-failing to failing hearts and did not change significantly post-LVAD.
Discussion
Measured metabolites related to glucose metabolism are diminished in failing hearts, but recovered their values post-LVAD. This differed from the amino acid levels, which decreased in heart failure but did not recover following LVAD. Creatine and the citric acid cycle intermediate succinate followed a similar pattern as the amino acid levels.
Introduction
Patients with chronic heart failure often have inadequate intake of calories and protein and diminished energy availability [1]. Likewise, it has been hypothesized that the failing heart is in a chronic energy starved state [2], [3] [4] and that abnormalities in metabolism contribute to myocardial dysfunction. [5] There are also considerable data to support an obesity paradox in heart failure with BMI's between 30–35 associated with lower mortality than BMI's closer to 25 [6]. Together, these ideas would seem to argue that patients with heart failure are energy depleted and it is plausible they could benefit from targeted nutrition therapy. Historically, nutritional interventions in this population focus on limiting sodium intake and maximizing intake of minerals such as calcium and magnesium [7], while little is known about metabolic substrates and metabolism in the failing heart.
Left ventricular assist device (LVAD) placement is becoming increasingly common as a bridge to transplant and as destination therapy. These patients often suffer from significant malnutrition both pre- and post- device placement. These devices have been shown to improve quality of life and survival in patients with end-stage heart disease when compared to medical therapy. [8] Many cardiac parameters improve following LVAD implantation; however, little is known about how this device affects the nutritional and metabolic parameters of the unloaded left ventricle (LV).
For some patients, unloading of the LV by LVAD placement leads to improved function of the native LV, known as reverse remodeling. Noted effects of reverse remodeling on the LV include reductions in mass, end-diastolic diameter, and ejection fraction compared to pre-LVAD implantation [9]. The hypoperfusion characteristic of HF leads to systemic neurohormonal and cytokine alterations, many of which are also normalized by LVAD use [10]. Despite normalization of numerous cardiac and systemic parameters post-LVAD implantation, incidence of successful LVAD removal without transplant is low [10]. A number of parameters do not recover post- LVAD, including those involving the extracellular matrix (increased collagen content, cross-linking, and myocardial stiffness) [11]–[13] and those involving genes related to metabolism [14].
The aim of this study was to measure key metabolites related to nutrition and energy in the myocardium of patients suffering from heart failure, and compare these measures to the myocardial metabolism in healthy patients and in patients following LVAD therapy. Our hypothesis is that the failing heart will have lower levels of most key metabolites than the non-failing hearts; and some of these metabolites will return to healthy levels after LVAD placement. This study focuses on levels of metabolites that might be altered via nutritional intervention.
Methods
Patients and Cardiac Tissue
Ethics Statement: The protocol for the collection, storage, and analysis of tissue for this study was approved by the Colorado Multiple Institutional Review Board and is outlined in a previous publication [15]. Written consent was given by patients for their information to be stored and used for research purposes. Eight patients with end-stage non-ischemic cardiomyopathy prior to LVAD placement were recruited and LV tissue samples were collected and flash frozen at the time of LVAD implantation (pre-LVAD) and at the time of cardiac transplant (post-LVAD) from each individual. Eight donor hearts harvested for transplant, but unused for reasons unrelated to the heart were utilized as the non-failing control samples. The pre-LVAD tissue sample was a core sample from the LV apex, at the in-flow cannulation site of the LVAD. The post-LVAD tissue sample was similar in size and was taken from the explanted heart. All tissue samples were directly flash frozen in liquid nitrogen in the operating room and transported to a −80°C freezer. No cardioplegia solutions were utilized. Pre-LVAD samples experienced <10 seconds of ischemia time from removal of tissue from the patient to when it was placed in liquid nitrogen. For post-LVAD samples this time was <10 minutes.
Retrospective review of medical records for demographic and clinical data was conducted by a trained physician. Time points for echocardiographic and hemodynamic data collection were chart entries closest to LVAD implantation and cardiac transplantation. Post-LVAD data reflect device settings clinically indicated and represent the combined effects of native LV function as well as LVAD-related unloading.
Quantitative Proton Nuclear Magnetic Resonance Spectroscopy
0.1 to 0.4 g of snap-frozen cardiac tissue was weighed out from each patient sample and homogenized in a mortar grinder in the presence of liquid nitrogen. Ice cold perchloric acid (PCA, 4 mL, 12%) extraction was carried out as described previously allowing for protein precipitation and separation of hydrophilic and lipophilic metabolites [16]–[18] The samples were centrifuged, and after the aqueous phase was neutralized with KOH, they were centrifuged again. The extract was lyophilized overnight. Next, the dry pellets were redissolved in 0.55 mL of deuterium oxide (D2O) for hydrophilic extracts and with 1.5 ml of deuterated methanol/chloroform for lipids.
H-NMR was carried out as published previously in order to evaluate cardiac metabolism [19]. In short, one-dimensional magnetic resonance spectra of hydrophilic and lipid extracts were recorded on a Bruker DRX500 MHz NMR spectrometer and processed with TopSpin software (Bruker, Billerica, MA). A 5-mm TXI inverse probe was used for all experiments. The operating frequency for proton NMR was 500 MHz, and a standard presaturation pulse program was used for water suppression. Other parameters included: 40 accumulations, 90-degree pulse angle, 0-dB power level, 7.35-µs pulse width, 10-ppm spectral width, and 12.85-s repetition time. Absolute quantification of metabolites (µmol/g tissue) was performed using trimethylsilyl propionic-2,2,3,3,-d4 acid (0.6 mM/L)as an external standard. 1H chemical shifts of spectra were referenced to trimethylsilyl propionic-2,2,3,3,-d4 acid at 0 ppm.
Metabolites in cardiac tissue were compared via t-test (for comparisons of non-failing and failing hearts) and paired t-test (for comparisons of pre-LVAD vs. post-LVAD samples) using SAS/STAT® software version 9.2, The SAS Institute, USA.
Results
Patient characteristics are found in Table 1. There were no statistically significant demographic differences between the failing/post-LVAD group and the non-failing group. Patients in the failing and post-LVAD group had a mean age of 40, and those in the non-failing group were on average 48 years old.
Table 1. Demographic Characteristics of Patients.
| Failing and Post-VAD (n = 8) | Non-Failing (n = 8) | |
| Patient Characteristics | ||
| Mean age (years) | 40.5±11.5 | 48±8.2 |
| Male gender | 7 (88%) | 3 (38%) |
| Caucasian | 4 (50%) | 7 (88%) |
| African American | 4 (50%) | 0 (0%) |
| Hispanic | 0 (0%) | 1 (13%) |
| Mean duration of HF prior to LVAD (months) | 56±22 | |
| Days on LVAD | 143±41 | |
| Baseline Cardiac Index (l/min/m2) | 1.8±.4 | |
| Baseline Pulmonary Capillary Wedge Pressure | 27±7 | |
| HeartMate XVE LVAD* | 5 (62%) | |
| HeartMate II LVAD* | 3 (39%) | |
| Medical Therapy/Interventions Pre-LVAD | ||
| Intravenous inotropic agent | 8 (100%) | |
| Intravenous vasodilator | 5 (62%) | |
| β-blocker | 0 (0%) | |
| ACE inhibitor/ARB | 2 (25%) | |
| Aldosterone antagonist | 7 (88%) | |
| Diuretic | 8 (100%) | |
| Medical Therapy During LVAD Support | ||
| Intravenous inotropic agent | 0 (0%) | |
| β-blocker | 6 (75%) | |
| ACE inhibitor/ARB | 7 (88%) | |
| Aldosterone antagonist | 7 (88%) | |
| Diuretic | 6 (75%) |
HF = Heart Failure, LVAD = Left Ventricular Assist Device, NYHA = New York Heart Association, ACE = Angiotensin-Converting Enzyme, ARB = Angiotensin II Receptor Blocker.
Thoratec, Pleasanton, CA.
Pre-LVAD, all patients in the failing/post-LVAD group were on intravenous inotropic agents and diuretics, 88% were on an aldosterone antagonist, 62% and intravenous vasodilator, and 25% an ACE inhibitor. During LVAD support 88% of patients in this group were on an aldosterone antagonist and/or an ACE inhibitor. 75% took a β-blocker and/or a diuretic prior to LVAD implantation (Table 1). Seven of the eight donor patients received IV vasopressors (unknown doses) after brain death, but none of these donor patients received inotropic agents. Table 1 lists clinical and hemodynamic information for hearts in the failing/LVAD group only. All parameters improved significantly after LVAD implantation.
Table 2 describes the baseline characteristics of the failing heart group. 5 (62.5%) had the HeartMate XVE® device implanted, while 3 (37.5%) of the patients had the HeartMate II® implanted. Patients in this study were on LVAD support an average of 143±41 days. Ejection fraction improved significantly after LVAD implantation from 10.0 percent (sd 1.07) to 25.6 percent (sd 11.4), (p = 0.003). Cardiac index also improved significantly after LVAD implantation from 1.5 l/min/m2 (sd 0.4) to 2.47 l/min/m2 (sd 0.7), (p = 0.016).
Table 2. Clinical and Hemodynamic Variables for Failing Hearts.
| Failing | Post-VAD (matched n = 8) | p-value | |
| Ejection Fraction (%) | 10 (1.0) | 26 (11.0) | 0.0065 |
| LVEDs (cm) | 6.8 (1.2) | 4.1 (1.3) | <0.0001 |
| LVEDd (cm) | 7.6 (1.2) | 4.9 (1.4) | <0.0001 |
| Mean PAP (mmHg) | 40.1 (8.4) | 19.0 (6.2) | 0.0062 |
| MAP (mmHg) | 72.4 (6.0) | 90.1 (11.7) | 0.0155 |
| NYHA Heart Class | 4 (0) | 2.1 (1) | <0.0001 |
LVEDs: Left Ventricular End Systolic Diameter, LVEDd: Left Ventricular End Diastolic Diameter, PAP: Pulmonary Artery Pressure, MAP: Mean Arterial Pressure, NYHA: New York Heart Association.
Key differences in myocardial metabolism are described in Table 3. In general, amino acids were significantly lower in failing than in non-failing hearts and did not significantly increase post-LVAD (Table 3). Alanine levels were higher in non-failing hearts (4.88±1.44 µmol/g of tissue vs. 2.13±1.57; p = 0.0004) than in failing hearts; and did not significantly increase post-LVAD support (2.83±1.6; p = 0.116). Levels of aromatic amino acids were higher in non-failing hearts (10.8 ±1.64 µmol/g of tissue) vs. failing hearts (8.29±2.8; p = 0.018); and did not increase post-LVAD (7.19±3.23; p = 0.330). Glutamine was higher in non-failing hearts (7.46±1.64 µmol/g of tissue) than in failing hearts (4.74±1.99; p = 0.0048) and did not increase post-LVAD (5.22±0.53; p = 0.442).
Table 3. Metabolite Differences Between Patient Groups (µmol/g of tissue).
| Metabolite Category | Non-Failing | Failing | Post-VAD |
| Glucose/Sugars | |||
| Glucose | 1.49±0.54 | 0.72±0.61* | 1.46±0.61** |
| Lactate | 11.2±3.69 | 5.72±5.76* | 15.6±5.54** |
| Amino Acids | |||
| Glutamine | 7.46±1.64 | 4.74±1.99* | 5.22±0.53 |
| Alanine | 4.88±1.44 | 2.13±1.57* | 2.83±1.6 |
| Aromatic Amino Acids | 10.8±1.64 | 8.29±2.80* | 7.19±3.23 |
| Other | |||
| Total Creatine | 10.4±1.97 | 4.70±3.32* | 5.20±3.4 |
| Succinate | 3.55±0.91 | 2.19±1.23* | 3.48±1.25 |
Metabolite differences between non-failing and failing hearts (* = p<0.05) and failing and post-VAD hearts (** = p<0.05).
Glucose was higher in non-failing hearts (1.49±0.54 µmol/g of tissue) than in failing hearts (0.72±0.61 µmol/g of tissue; p = 0.0037), and the level increased again significantly after LVAD support (1.46±0.61 µmol/g of tissue; p = 0.0302). Lactate also was higher in non-failing hearts (11.2±3.69 µmol/g of tissue) than in failing hearts (5.72±5.76 µmol/g of tissue; p = 0.0045); and also increased again significantly after LVAD support (15.6±5.54 µmol/g of tissue; p = 0.0082).
Total creatine was higher in non-failing (10.4±1.97 µmol/g of tissue) than failing hearts (4.70±3.32 µmol/g of tissue; p = 0.00009); and creatine did not increase significantly after LVAD support (5.20±3.4 µmol/g of tissue; p = 0.3554). Succinate was significantly higher in non-failing (3.55±0.91 µmol/g of tissue) than failing hearts (2.19±1.23 µmol/g of tissue; p = 0.0113), and did not change significantly post-LVAD (3.48±1.25 µmol/g of tissue; p = 0.0917).
Discussion
Our data indicates that significant changes in myocardial metabolism occur in the failing heart and some, but not all of these changes, are improved by LVAD placement. The amino acid levels in this study indicate that these substrates decrease significantly in cardiac tissue from non-failing to failing hearts and they do not recover during LVAD support. These data seem to support the hypothesis that the heart is depleting its amino acid stores and that unloading the heart through LVAD support does not allow replenishment of these losses.
Select metabolites from each category are represented graphically in Figure 1. We chose to measure glutamine levels as a result of previous data showing the cardioprotective effects of this amino acid. Glutamine has been shown to return contractile function in vitro in chick cardiomyocytes post ischemia/reperfusion (I/R) injury [20]. Glutamine has also been shown to enhance myocardial tissue metabolism, glutathione content, and improve myocardial function (cardiac output) after I/R injury in a working heart model [21]. This particular amino acid has also been shown in double-blind, placebo-controlled, randomized trials carried out by our group and others to be protective of the myocardium in human clinical trials when administered during cardiopulmonary bypass (CPB) [22], [23]. In these studies, glutamine treatment prior to CPB decreased troponin I [22], creatine kinase-MB [23], and clinical complications [23]. It has been shown that the most dominant pathway through which glutamine exerts its effects on the cardiomyocyte and other cells in the body is through the induction of heat shock proteins [21]. Additional important pathways exist including glutamine conversion to alpha ketoglutarate to be utilized in the TCA cycle.
Figure 1. Differences in select metabolites between non-failing, failing, and post-LVAD hearts.
P-values indicated only where differences are statistically significant (p<0.05).
Substrates related to glucose metabolism showed a different pattern pre-/post-LVAD placement than the measured amino acid levels. Both glucose and lactate decreased in heart failure but increased again after LVAD support. It is known that during heart failure there is a switch in substrate preference from fatty acids (β-oxidation) to carbohydrates (glycolysis) as the primary fuel preference. This is part of the reversion to the fetal energy substrate pattern known to occur during heart failure [24]. Unlike amino acid metabolism, levels of substrates related to carbohydrate metabolism seem to revert back to normal after LVAD support. It is plausible that the glucogenic amino acids are being utilized to synthesize glucose and to maintain glycolysis thus causing amino acid stores to “burn out” while carbohydrate levels are replenished in the post-LVAD samples. However, more focused studies need to be carried out to prove this hypothesis.
Total creatine levels (creatine plus phosphocreatine) were measured in an attempt to determine relative energy availability in the cardiac tissues. The pattern of total creatine data looked much like the amino acid data as it decreased significantly from non-failing to failing hearts and remained low post-LVAD. This was interesting in light of our overall hypothesis, as there is a link in the literature between glutamine and creatine. In rat models of ischemia/reperfusion, glutamine supplementation leads to an increase in the creatine and phosphocreatine content of the myocardium [21], [25]. While patients in this study were not supplemented with glutamine, it is not surprising that creatine followed a similar overall pattern to glutamine levels as these previous data showed.
Succinate levels were also measured in order to determine the function of the citric acid cycle (CAC) under the disease states studied. Levels of CAC intermediates are crucial for the oxidation of acetyl-CoA to CO2 and the generation of NADH and FADH2 for the electron transport chain. Increasingly cardiovascular researchers are studying the role of ‘anapleurosis’ in the heart, meaning the process of replenishing depleted metabolic cycle intermediates (in this case CAC intermediates) [26]. The fact that succinate levels were significantly decreased in heart failure and did not improve significantly post-LVAD indicates that CAC intermediates are affected in the failing heart, and that they follow the same pattern as the amino acids, and creatine.
Increasing anapleurotic flux in the setting of cardiac disease is considered beneficial [26]. One challenge in accomplishing this increase is that activity of the enzymes aconitase and citrate synthase are decreased in heart failure [27]. For this reason, carbohydrates and fatty acids are utilized less efficiently than substrates that bypass these enzymes and enter further along the TCA cycle. Thirteen of the 22 amino acids enter the CAC past this point, one is glutamine.
In conclusion, these data show that cardiac tissue amino acid stores are depleted in heart failure and they do not recover after LVAD support. This is of particular interest for the amino acid glutamine since it is known to have cardioprotective effects. Total creatine and succinate (a CAC intermediate) follow the same pattern as amino acids, while metabolites related to glycolytic metabolism recover their levels after LVAD implantation. It is known that individuals who have lower BMI's (and thus less lean body mass) have higher mortality from heart failure. In light of the obesity paradox and the cardiac data presented here, a clinical trial of targeted amino acid supplementation in patients with heart failure should be considered.
There are several limitations to this study. A disadvantage of measuring metabolites only in cardiac tissue is the inability to obtain samples from the vast majority of patients with heart failure. Our study is confined to patients with advanced disease who received mechanical cardiac support. We did not prospectively collect peripheral blood on these patients so it is unknown if these changes in tissue metabolic substrates correlate with peripheral abnormalities. It is also unknown if these changes effect patients with less severe disease. It is interesting to note that data from the Framingham study has recently shown that higher peripheral glutamine is strongly associated with reduced cardiovascular risk. [28] Our results suggest only that these abnormalities involve the myocardium in end-stage heart failure. Further prospective studies are necessary to evaluate the correlation of peripheral and tissue metabolites as well as their prognostic significance. These experiments are also limited in that they only measure cardiac metabolites and as such provide limited insight into the molecular mechanisms of these processes. Future combined studies in metabolomics, transcriptomics and proteomics will be necessary to elucidate the full mechanisms of these abnormalities as well as overall system biology of heart failure. Finally, there is lack of data from the donor patients and donor hearts including BMI, diabetes status, and catecholamine levels. Procurement of donor heart tissue is the only manner in which to reasonably obtain non-failing control tissue. These limitations are universal when utilizing human myocardial samples. End-stage heart failure is a complex phenotype. Given the small sample size these findings should be considered hypothesis generating until the underlying mechanisms are elucidated and the findings confirmed in larger cohorts.
SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. in the USA and other countries.
Funding Statement
This work is supported by NIH P20 HL101435 (Lowes, Brian: PI) (National Institutes of Health). Amrut Ambardekar is supported by NIH/NCRR Colorado CTSI Grant Number UL1 RR025780. Contents are the authors' sole responsibility and do not necessarily represent official NIH views. Paul Wischmeyer, MD and Lindsay Weitzel PhD received support from the NIH (R01 GM078312) for this work. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Aquilani R, Opasich C, Verri M, Boschi F, Febo O, et al. (2003) Is nutritional intake adequate in chronic heart failure patients? J Am Coll Cardiol 42: 1218–1223. [DOI] [PubMed] [Google Scholar]
- 2. Sheeran FL, Pepe S (2006) Energy deficiency in the failing heart: linking increased reactive oxygen species and disruption of oxidative phosphorylation rate. Biochim Biophys Acta 1757: 543–552. [DOI] [PubMed] [Google Scholar]
- 3. Ingwall JS, Weiss RG (2004) Is the failing heart energy starved? On using chemical energy to support cardiac function. Circ Res 95: 135–145. [DOI] [PubMed] [Google Scholar]
- 4. Katz AM (1998) Is the Failing Heart Energy Depleted? Cardilogy Clinics 16. [DOI] [PubMed] [Google Scholar]
- 5. Neubauer S (2007) The failing heart–an engine out of fuel. N Engl J Med 356: 1140–1151. [DOI] [PubMed] [Google Scholar]
- 6. Anker SD, von Haehling S (2011) The obesity paradox in heart failure: accepting reality and making rational decisions. Clin Pharmacol Ther 90: 188–190. [DOI] [PubMed] [Google Scholar]
- 7. Arcand J, Floras V, Ahmed M, Al-Hesayen A, Ivanov J, et al. (2009) Nutritional inadequacies in patients with stable heart failure. J Am Diet Assoc 109: 1909–1913. [DOI] [PubMed] [Google Scholar]
- 8. Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, et al. (2001) Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med 345: 1435–1443. [DOI] [PubMed] [Google Scholar]
- 9. Maybaum S, Mancini D, Xydas S, Starling RC, Aaronson K, et al. (2007) Cardiac improvement during mechanical circulatory support: a prospective multicenter study of the LVAD Working Group. Circulation 115: 2497–2505. [DOI] [PubMed] [Google Scholar]
- 10. Burkhoff D, Klotz S, Mancini DM (2006) LVAD-induced reverse remodeling: basic and clinical implications for myocardial recovery. J Card Fail 12: 227–239. [DOI] [PubMed] [Google Scholar]
- 11. Klotz S, Foronjy RF, Dickstein ML, Gu A, Garrelds IM, et al. (2005) Mechanical unloading during left ventricular assist device support increases left ventricular collagen cross-linking and myocardial stiffness. Circulation 112: 364–374. [DOI] [PubMed] [Google Scholar]
- 12. McCarthy PM, Nakatani S, Vargo R, Kottke-Marchant K, Harasaki H, et al. (1995) Structural and left ventricular histologic changes after implantable LVAD insertion. Ann Thorac Surg 59: 609–613. [DOI] [PubMed] [Google Scholar]
- 13. Nakatani S, McCarthy PM, Kottke-Marchant K, Harasaki H, James KB, et al. (1996) Left ventricular echocardiographic and histologic changes: impact of chronic unloading by an implantable ventricular assist device. J Am Coll Cardiol 27: 894–901. [DOI] [PubMed] [Google Scholar]
- 14. Razeghi P, Young ME, Ying J, Depre C, Uray IP, et al. (2002) Downregulation of metabolic gene expression in failing human heart before and after mechanical unloading. Cardiology 97: 203–209. [DOI] [PubMed] [Google Scholar]
- 15. Ambardekar AV, Walker JS, Walker LA, Cleveland JC Jr, Lowes BD, et al. (2011) Incomplete recovery of myocyte contractile function despite improvement of myocardial architecture with left ventricular assist device support. Circ Heart Fail 4: 425–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Serkova NJ, Glunde K (2009) Metabolomics of cancer. Methods Mol Biol 520: 273–295. [DOI] [PubMed] [Google Scholar]
- 17. Serkova N, Fuller TF, Klawitter J, Freise CE, Niemann CU (2005) H-NMR-based metabolic signatures of mild and severe ischemia/reperfusion injury in rat kidney transplants. Kidney Int 67: 1142–1151. [DOI] [PubMed] [Google Scholar]
- 18. Cohen MJ, Serkova NJ, Wiener-Kronish J, Pittet JF, Niemann CU (2010) 1H-NMR-based metabolic signatures of clinical outcomes in trauma patients–beyond lactate and base deficit. J Trauma 69: 31–40. [DOI] [PubMed] [Google Scholar]
- 19. Stringer KA, Serkova NJ, Karnovsky A, Guire K, Paine R 3rd, et al. (2011) Metabolic consequences of sepsis-induced acute lung injury revealed by plasma (1)H-nuclear magnetic resonance quantitative metabolomics and computational analysis. Am J Physiol Lung Cell Mol Physiol 300: L4–L11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wischmeyer PE, Vanden Hoek TL, Li C, Shao Z, Ren H, et al. (2003) Glutamine preserves cardiomyocyte viability and enhances recovery of contractile function after ischemia-reperfusion injury. JPEN J Parenter Enteral Nutr 27: 116–122. [DOI] [PubMed] [Google Scholar]
- 21. Wischmeyer PE, Jayakar D, Williams U, Singleton KD, Riehm J, et al. (2003) Single dose of glutamine enhances myocardial tissue metabolism, glutathione content, and improves myocardial function after ischemia-reperfusion injury. JPEN J Parenter Enteral Nutr 27: 396–403. [DOI] [PubMed] [Google Scholar]
- 22. Lomivorotov VV, Efremov SM, Shmirev VA, Ponomarev DN, Lomivorotov VN, et al. (2011) Glutamine Is Cardioprotective in Patients with Ischemic Heart Disease following Cardiopulmonary Bypass. Heart Surg Forum 14: E384–388. [DOI] [PubMed] [Google Scholar]
- 23. Sufit A, Weitzel L, Hamiel C, Queensland K, Dauber I, et al. (2012) Oral Glutamine Reduces Myocardial Injury and Peri-Operative Complications in Patients Undergoind Cardiac Surgery: A Randomized Pilot Trial. Journal of Parenteral and Enteral Nutrition In Press [DOI] [PubMed] [Google Scholar]
- 24. Rajabi M, Kassiotis C, Razeghi P, Taegtmeyer H (2007) Return to the fetal gene program protects the stressed heart: a strong hypothesis. Heart Fail Rev 12: 331–343. [DOI] [PubMed] [Google Scholar]
- 25. Khogali SE, Harper AA, Lyall JA, Rennie MJ (1998) Effects of L-glutamine on post-ischaemic cardiac function: protection and rescue. J Mol Cell Cardiol 30: 819–827. [DOI] [PubMed] [Google Scholar]
- 26. Des Rosiers C, Labarthe F, Lloyd SG, Chatham JC (2011) Cardiac anaplerosis in health and disease: food for thought. Cardiovasc Res 90: 210–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Qanud K, Mamdani M, Pepe M, Khairallah RJ, Gravel J, et al. (2008) Reverse changes in cardiac substrate oxidation in dogs recovering from heart failure. Am J Physiol Heart Circ Physiol 295: H2098–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cheng S, Rhee EP, Larson MG, Lewis GD, McCabe EL, et al. (2012) Metabolite profiling identifies pathways associated with metabolic risk in humans. Circulation 125: 2222–2231. [DOI] [PMC free article] [PubMed] [Google Scholar]