Abstract
Background
The lower limb osteometry of Chinese differs from that of whites. The joint line of the knee in the coronal plane in Chinese is more medially inclined and the posterior condylar angle of the distal femur in the axial plane is larger. However, it is unclear whether there is any direct association between the coronal plane and axial plane osteometry.
Questions/purposes
We asked whether the joint line obliquity of the knee is related to the posterior condylar angle of the distal femur in young Chinese subjects.
Methods
Ninety-nine young Chinese patients with anterior cruciate ligament injuries were recruited. The lower limb alignment and joint line obliquity were measured using standing long radiographs of the whole lower limb. The rotational alignment of the distal femur was assessed in the axial cuts of the MRI.
Results
The distal femur rotational alignment was associated with the obliquity of the knee in Chinese. The posterior condylar angle was 5° ± 2°. The knee was 5° ± 3° medially inclined.
Conclusions
The joint line of the knee in a group of young Chinese patients was more medially inclined than that of whites. The posterior condylar angle of the distal femur was larger. The presence of an association between distal femur rotational alignment and joint line obliquity in this group of young Chinese patients suggests a possible developmental cause explaining the difference in osteometry between races.
Introduction
TKA is one of the most commonly performed orthopaedic operations. The success of TKA depends on correct implantation of the prosthesis and proper ligament balance of the deformed knee [8, 18]. Restoration of the neutral mechanical alignment of the lower limb in the coronal plane and the correct rotational alignment in the axial plane are considered as two of the most important issues during prosthesis implantation [1, 2, 6, 8].
However, it is well known that the osteometry of Asians differs from that of Western populations in both size and morphology [4, 11, 19, 20, 22, 23]. In a group of young healthy asymptomatic Chinese volunteers, we demonstrated that the mechanical axis of the lower limb in the coronal plane was more varus in the Chinese patients (2.2° varus) and the joint line was more medially inclined (5.2°) [16]. In a separate study of 82 embalmed cadaveric femurs of known Chinese ethnicity [23], we observed that the posterior condylar angle (ie, the angle between the surgical epicondylar axis and posterior condylar line of the distal femur) was larger. The average posterior condylar angle was 5.2°. The reported lower limb alignment and joint line obliquity in whites were varus 1° and medially inclined 3°, respectively [7, 14]. These values differ from those reported for Chinese [20] (Table 1). Despite the observation of the apparent incidental findings of comparable average angle of joint line obliquity (5.2° medial inclination) and posterior condylar angle (5.2°), it is unclear whether the joint line obliquity of the knee is associated with the rotational alignment of the distal femur.
Table 1.
Results of measurements compared with published data
| Publication | Number of knees | Ethnicity | Posterior condylar angle | Joint line obliquity of the knee | Mechanical axis of the lower limb |
|---|---|---|---|---|---|
| Berger et al. [3]* | 75 | White | Male 3.5° (SD 1.2°) Female 0.3° (SD 1.2°) |
– | – |
| Griffin et al. [5]* | 104 | White | 3.1° (SD 1.75°) |
– | – |
| Yip et al. [23]† | 82 | Chinese | 5.2° (SD 1.9°) |
– | – |
| Moreland et al. [14]* | 50 | White | – | Right 3° (SD 1.6°) Left 2.6° (SD 1.4°) |
Right Varus 1.5° (SD 2.0°) Left Varus 1.1° (SD 2.1°) |
| Hsu et al. [7]* | 120 | White | – | Male 1° (SD 1.4°) Female 0.1° (SD 1.9°) |
Male Varus 2.3° (SD 2.3°) Female Varus 1.3° (SD 1.8°) |
| Tang et al. [20]† | 100 | Chinese | – | 5.2° (SD 2.4°) |
Varus 2.2° (SD 2.6°) |
| Current study† | 99 | Chinese | 5° (SD 2°) |
5° (SD 3°) |
Varus 1° (SD 3°) |
* White data; †Chinese data.
We therefore asked whether (1) a correlation existed between the rotational alignment of the distal femur in the axial plane (posterior condylar angle) and the obliquity of the joint line of the knee in the coronal plane; and (2) there was a difference in the posterior condylar angle of the distal femur between varus alignment and valgus alignment of the mechanical axis of the lower limb in the coronal plane.
Materials and Methods
We assessed 120 young Chinese patients with anterior cruciate ligament (ACL) deficiency attending an ACL reconstruction preoperative assessment clinic from March 2008 to September 2011. For patients with bilateral ACL deficiency (five patients), only the right knee was evaluated. The inclusion criteria were as followed: (1) Chinese ethnicity; (2) age from 16 to 40 years old; (3) isolated ACL deficiency without substantial collateral ligament deficiency; and (4) presence of preoperative MRI of the involved knee. Fifteen knees did not satisfy the inclusion criteria: substantial collateral ligament laxity requiring collateral ligament reconstruction in two knees, MRIs absent in seven knees, and six knees in patients older than 40 years. The exclusion criteria were as follows: (1) evidence of osteoarthritis of the involved knee with a Kellgren and Lawrence grading of 2 or above [10]; (2) substantial malrotation of the standing long film of the lower limb as indicated by a noncentral location of the patella; and (3) MRI scanning protocol not complying with the research protocol. Six knees were excluded (two knees with evidence of osteoarthritis on conventional knee radiographs, two knees with malrotated long films, and two knees with a suboptimal MRI scanning protocol). These exclusions left 99 patients with 99 knees for analysis. There were 87 male patients and 12 female patients. The average age of the patients was 25 ± 6 years (range, 16–37 years). There were 53 right knees and 46 left knees. Seventy-three patients had meniscal tears of at least one side. Eighteen patients had isolated medial meniscal tears. Forty-two patients had isolated lateral meniscal tears. Thirteen patients had tears of both medial and lateral menisci. Eight patients underwent surgery on the involved knee before recruitment. One patient underwent a partial lateral meniscectomy. Four had repair of menisci performed (two on the medial meniscus and two on the lateral meniscus). Three patients underwent diagnostic arthroscopy.
Sample size estimation was performed to determine a possible correlation between joint line obliquity of the knee and posterior condylar angle of the distal femur. The reported SD of joint line obliquity of the knee and posterior condylar angle of the distal femur in Chinese were 2.4° [20] and 1.9° [23], respectively. To detect a weak to moderate association of 0.3, assuming a Type I error of 0.05 and setting the power of study at 0.8, a minimal sample of 57 patients was required.
Standing radiographs of the whole lower limb were taken using a standard protocol described in a previous study [20]. All subjects were asked to stand, wearing their usual footwear, with both knees fully extended and both patellae facing forward [9]. A weightbearing AP radiograph of the entire lower limb then was made with the x-ray beam centered at the knees at a distance of 2.5 m. A cassette holding long radiographs (300 × 900 mm) was placed immediately behind the subject. A setting of 60 mA seconds and a kilovoltage of 65 to 80 were required to provide the necessary exposure. Substantial malrotation of the long films was assumed to be present if the patella was not centrally located [9].
Preoperative MRIs of the knee were obtained in all patients. Among the 99 patients, 64 patients underwent MRI at the author’s institution and 35 underwent MRI at other institutions. The MRI scans at the author’s institute were performed with a 1.5-Tesla MRI system (SignaHD; General Electric, Milwaukee, WI, USA) using a knee coil (General Electric). Six sequences, including T1 and T2, in coronal, sagittal, and axial planes were performed. The other parameters for all six sequences included matrix, 256 × 256; field of view, 16 cm; thickness, 4 mm; and space, 0.5 mm. The scanning of the axial scan of the distal femur was performed along the anatomical axis of the distal femur. MRIs at the other institutions were considered satisfactory if the following criteria were met: (1) the MRI system was at least 1.5 Tesla; (2) axial T2-weighed fat-saturated spin echo sequence was done; (3) the scanning of the axial scan of the distal femur should be performed within 10° from the anatomical axis of the distal femur; and (4) the slice thickness should be at least 4 mm or less.
The radiographs were digitized using a VXR-12 plus film digitizer (VIDAR, Herndon, VA, USA) and measurements were made using commercially available software (OsiriX 32-bit 4.1.2; Pixmeo, Geneva, Switzerland). The reported inter- and intraobserver agreement in these measurements was strong to perfect [21]. Two of the authors (WPY, CHY) assessed the axial alignment of the lower limb and joint line obliquity in the digitalized standing radiographs of the whole lower limb. One of the authors (WPY) was the treating surgeon. Two angles were measured: the mechanical axis of the lower limb in the coronal plane and the obliquity of the joint line of the knee with reference to the mechanical axis of the tibia. The mechanical axes of the femur and the tibia were the lines joining the center of the knee to the center of the femoral head and the center of the knee to the center of the ankle, respectively. The centers of the joints were defined according to the protocol previously described [14, 20]. The mechanical axis of the lower limb in the coronal plane was defined as the acute angle between the mechanical axis of the femur and the mechanical axis of the tibia (Fig. 1). It was expressed in varus aligned, neutral, or valgus aligned. The joint line of the knee was defined as a line tangential to the subchondral plate of the proximal tibia (Fig. 2). The obliquity of the joint line with reference to the mechanical axis of the tibia was defined as the acute angle between the joint line of the knee and perpendicular to the mechanical axis of the tibia. It was expressed in medially inclined, neutral, or laterally inclined (Fig. 2).
Fig. 1.
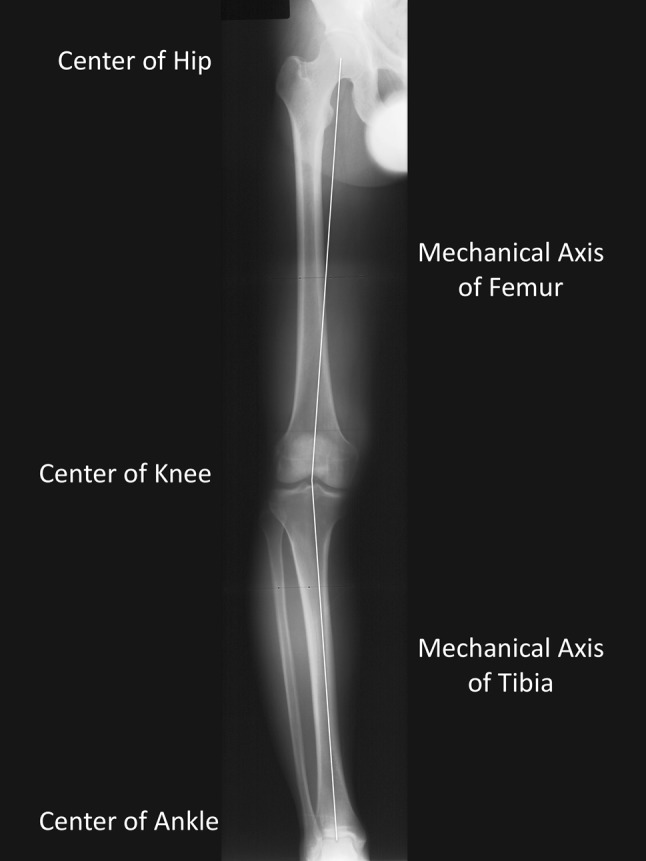
Mechanical axis of the lower limb. Mechanical axis of the lower limb was defined as the acute angle between the mechanical axis of femur and mechanical axis of the tibia. It was expressed as varus aligned, neutral, or valgus aligned. Mechanical axis of the femur was the line joining the center of the femoral head and the center of the knee. Mechanical axis of the tibia was the line joining the center of the knee and the center of the ankle.
Fig. 2.

Obliquity of the joint line with reference to mechanical axis of the tibia. The joint line of the knee was defined as a line tangential to the subchondral plate of the proximal tibia. The obliquity of the joint line with reference to mechanical axis of the tibia was defined as the acute angle between the joint line of the knee and perpendicular to the mechanical axis of the tibia. It was expressed as medially inclined, neutral, or laterally inclined.
The same observers (WPY, CHY) measured the rotational alignment of the distal femur using a T2 axial cut MRI of the knee. The posterior condylar angle was measured according to the protocol previously described [12]. The posterior condylar angle was originally described by Berger et al. [3]. It was the angle between the surgical epicondylar axis and the posterior condylar line of the distal femur. The surgical epicondylar axis was a line joining the medial and lateral femoral epicondyle. The medial femoral epicondyle was identified on the MRI as the deepest point of the medial sulcus, which represented the origin of the deep part of the medial collateral ligament. The lateral femoral epicondyle was defined as the most prominent point at the origin of the lateral collateral ligament. The posterior condylar line was defined as a line tangential to the most posterior point of the cartilage of the medial and lateral femoral condyles (Fig. 3). The inter- and intraobserver variability of mechanical axis of the lower limb, obliquity of the joint line, and posterior condylar angle was determined with an intraclass correlation. For the repeatability in the measurement of mechanical axis of long film and joint line obliquity of the knee, we found an intraobserver ICC of 0.87 and interobserver agreement of 0.85 (Table 2). For the repeatability in the measurement of the posterior condylar angle, the intraobserver agreement was 0.74 and the interobserver agreement was 0.43.
Fig. 3.
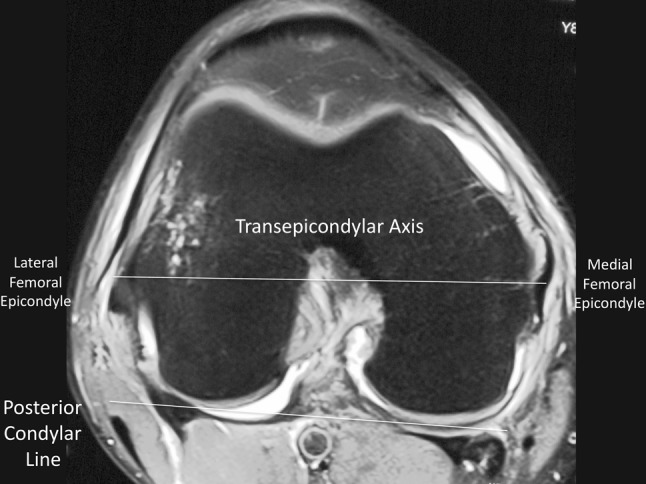
Posterior condyle angle. Posterior condylar angle was the angle between the surgical transepicondylar axis and the posterior condylar line of the distal femur. Surgical transepicondylar axis was a line joining the medial femoral epicondyle (deepest point of the medial sulcus, where the deep part of medial collateral ligament attaches) and lateral femoral epicondyle (most prominent point at the origin of lateral collateral ligament). Posterior condyle line was a line joining the most posterior point of the medial and lateral femoral condyle cartilage.
Table 2.
Interobserver and intraobserver agreement
| Measurement | Interobserver agreement (intraclass correlation) |
Intraobserver agreement (intraclass correlation) |
|---|---|---|
| Posterior condylar angle | 0.43 | 0.74 |
| Joint line obliquity of the knee | 0.85 | 0.87 |
| Mechanical axis of the lower limb in the coronal plane | 0.82 | 0.98 |
We assessed the association between the rotational alignment of the distal femur (ie, the posterior condylar angle) and the obliquity of the joint line using a Pearson correlation. We determined whether there was a difference in the posterior condylar angle of the distal femur between varus alignment and valgus alignment of the lower limb with Student’s t-test. We used SPSS 20.0 (IBM, New York, NY, USA) for all analyses.
Results
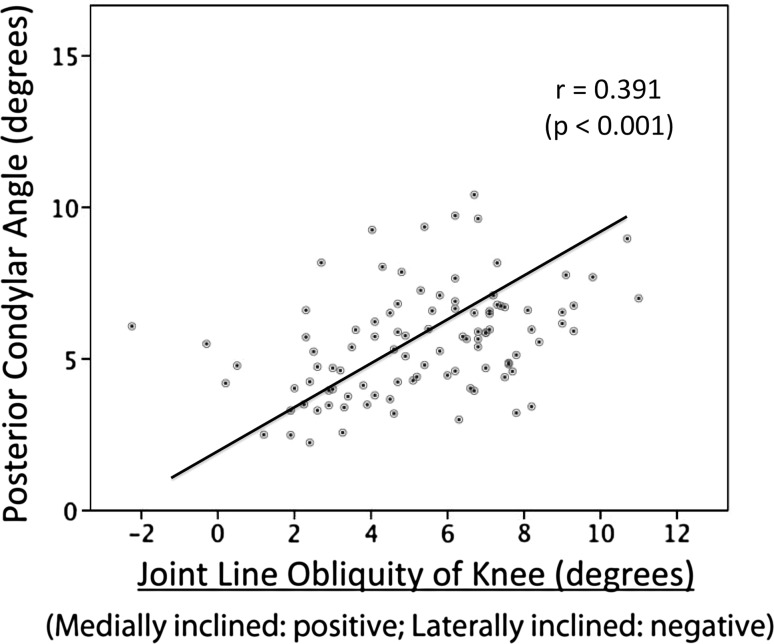
We found an association (r = 0.391, p < 0.001) between the obliquity of the joint line of the knee in the coronal plane and the posterior condylar angle of the distal femur in the axial plane. The average obliquity of joint line was 5° medial inclination. The average posterior condylar angle was 5° (Table 3).
Table 3.
Axial alignment of the lower limb, obliquity of the joint line, and rotational alignment of the distal femur
| Measurement | Result |
|---|---|
| Posterior condylar angle | 5° ± 2° (1°–10°) |
| Male: 6° ± 2° | |
| Female: 5° ± 2° | |
| Joint line obliquity with reference to mechanical axis of tibia | Medial inclined 5° ± 3° (medial inclined 11° to lateral inclined 2°) |
| Male: medial inclined 6° ± 3° | |
| Female: medial inclined 4° ± 2° | |
| Axial alignment of the lower limb in the coronal plane | Varus 1° ± 3° (valgus 7° to varus 8°) |
| Male: varus 1° ± 3° | |
| Female: valgus 1° ± 3° |
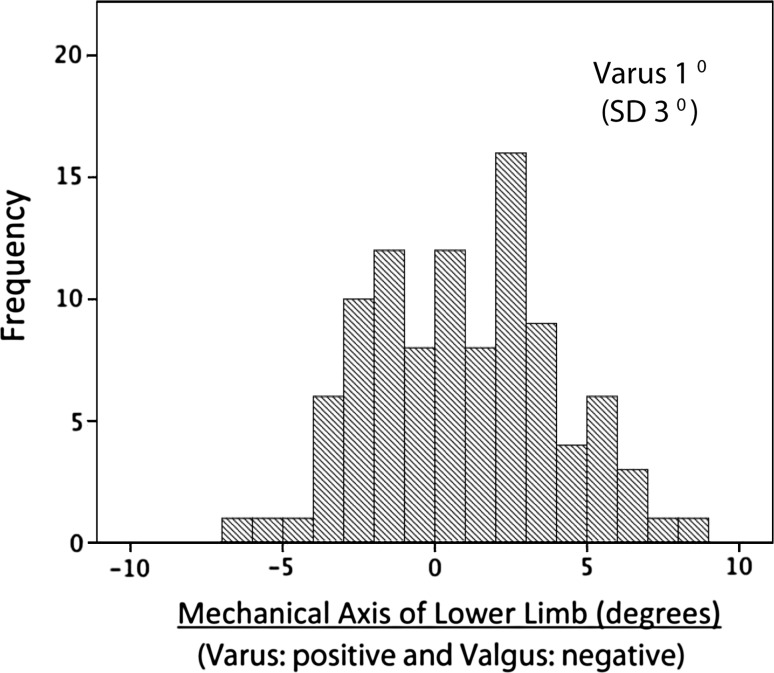
The posterior condylar angle in patients with varus alignment of the lower limb was larger than that in patients with valgus alignment (p = 0.015). The average mechanical axis of the lower limb was varus 1° (Table 3). Sixty lower limbs were in varus alignment. The average posterior condylar angle in varus of the knee was 6°. Thirty-nine lower limbs were in valgus alignment. The average posterior condylar angle in valgus of the knee was 5°.
Discussion
It is well known that the osteometry of Asians differs from that of Western populations [4, 11, 19, 20, 22, 23] (Fig. 4). The lower limb alignment was more varus and the obliquity of the joint line of the knee was more medially inclined in a group of young Chinese volunteers with an average age of 24 years [20]. The posterior condylar angle of Chinese was noted to be larger in studying 82 embalmed Chinese cadaveric femurs of an average age of 78 years [23] (Table 1). However, it is unclear whether there is a direct correlation between the coronal plane osteometry and the axial plane osteometry of the distal femur. We therefore asked whether (1) a correlation existed between the rotational alignment of the distal femur in the axial plane (posterior condylar angle) and the obliquity of the joint line of the knee in the coronal plane; and (2) whether there was a difference in the posterior condylar angle of the distal femur between varus alignment and valgus alignment of the mechanical axis of the lower limb in the coronal plane.
Fig. 4.
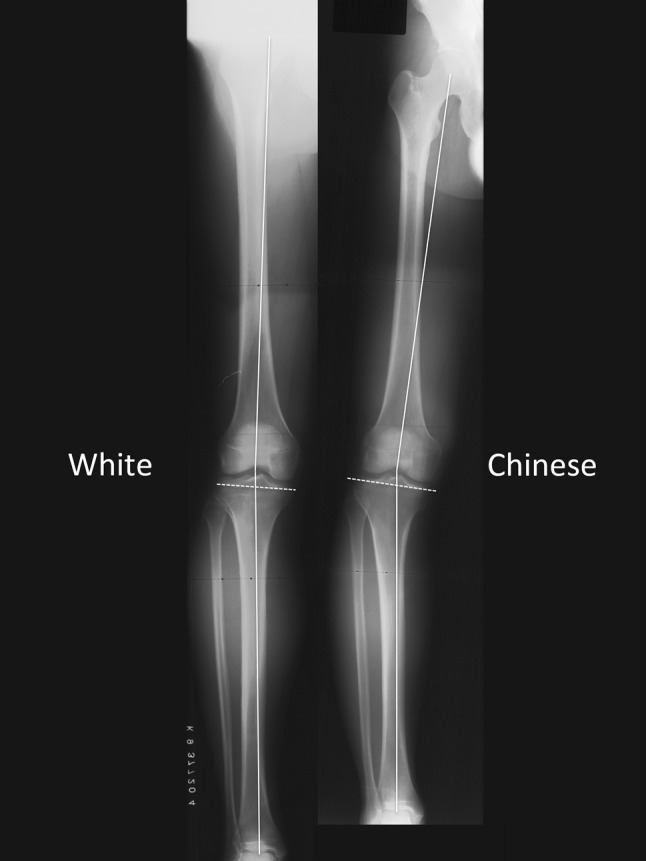
Comparison between white and Chinese lower limb osteometry. The lower limb alignment was more varus and the knee was more medially inclined in Chinese when compared with white patients.
There were a number of limitations in the current study. First, the subjects recruited were biased to a group of young active patients with ACL deficiency. The characteristics of the patients were different from those of older patients requiring TKA. However, early degeneration is more likely in this group of ACL-deficient patients [13, 15–17] because of the abnormal biomechanics in the knee and high chance of concomitant meniscal and cartilage injury. Second, females were underrepresented (14% of the studied knees). This was related to the primary diagnosis in the inclusion criteria (ACL-deficient knee), which was more common in men than in women in our population. Third, despite the attempts at minimizing biases arising from malrotation of the standing radiographs of the lower limb, errors in this area were still unavoidable. In a cadaveric experiment testing the influence of rotation on the errors in measurement of the mechanical axes of the femur, the average reported variation was 2.5° between the positions of 20° of internal rotation and 20° of external rotation [9]. By excluding patients with excessive rotation in the standing long radiographs, the impact should be negligible. Fourth, the use of MRI in assessing the rotational axes of the distal femur might not be optimal. CT would be a better option for identifying these bony landmarks. However, preoperative CT carried substantial radiation hazard and was not appropriate for a group of young active individuals for clinical purposes. Furthermore, because the two collateral ligaments could be identified on the MRI, these provided an additional clue in locating the two femoral epicondyles. Fifth, the interobserver repeatability of measurement of the posterior condylar angle was not high, although the intraobserver agreement was (Table 2). This might be related to the anatomy of the medial femoral epicondyle, which was a sulcus located in the center of a horseshoe-shaped ridge. The depth of the sulcus was small and could be difficult to locate [5]. Sixth, 73 of 99 patients had meniscal tears. One patient had a history of partial lateral meniscectomy. The presence of meniscal tears, especially medial, might influence the varus deformity of the knee.
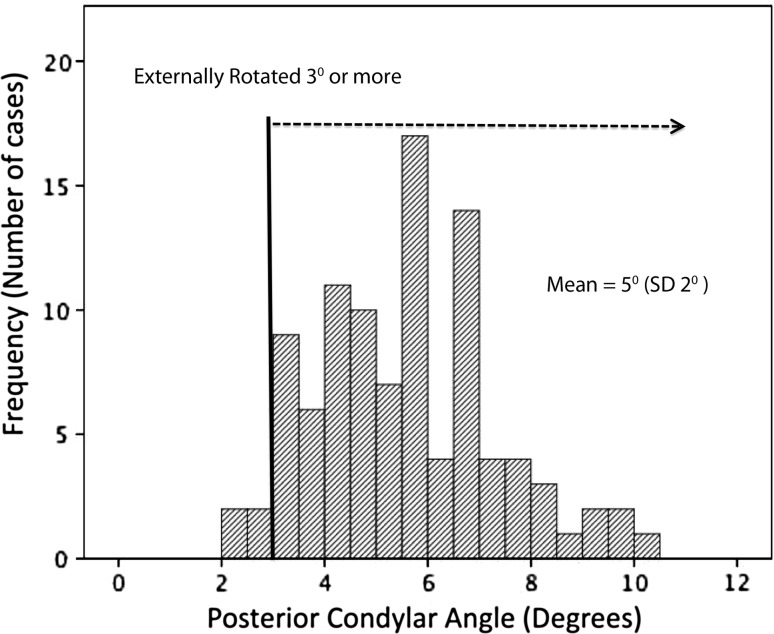
We found an association between the rotational alignment of the distal femur and the joint line obliquity with reference to the anatomical axis of the proximal tibia (Fig. 5). The average joint line obliquity in a group of young Chinese patients with ACL deficiency in the current study was 5°. This was larger than the reported data in the white study (0.5° [7] and 2.8° [14]) (Table 1). The posterior condylar angle was 5° in the current study, which was also bigger than that reported in the white population (3.5° for males and 0.3° for females in one study [3] and 3.1° in another study [5]) (Table 1). A large variation of posterior condylar angle (1°–10°) (Fig. 6) was found in the current study. This finding cautions the practice of routine use of a fixed angle of external rotation from the posterior condylar line (eg, 3°) in determining the rotation of femoral components during TKA in Chinese. Reference to multiple anatomical axes (eg, transepicondylar axis and Whiteside line) and adoption of a balanced flexion gap method and distracter should be considered in individualizing the rotation of the femoral component. The finding of an association between the joint line obliquity and posterior condylar angle may further help preoperative planning of the rotational alignment of the femoral component, especially if an excessive medially inclined joint line is observed in the proximal tibia on the preoperative radiograph.
Fig. 5.
Relationship between joint line obliquity and posterior condylar angle. The coronal plane knee line obliquity was associated with the axial plane posterior condylar angle of the distal femur. The average joint line obliquity was 5° medially inclined and the average posterior condylar angle was 5°.
Fig. 6.
Distribution of posterior condylar angle. The average posterior condylar angle was 5°. However, the dispersion was large (2°–10°). More than 90% of the knee had a posterior condylar angle of more than 3°.
Varus alignment of the lower limb was associated with larger posterior condylar angle of the distal femur. Despite the fact that the average alignment in our study was in the range of that in white reports [7, 14], the dispersion of the data was higher in our series (Fig. 7). The maximal varus alignment was varus 8°. Thirteen knees (13%) had a lower limb alignment of varus 5° or more. This varus malalignment of the lower limb in a group of young ACL-deficient Chinese is likely to be developmental in nature. The medial collateral ligament may be relatively shorter. The association of varus knee alignment with larger posterior condylar angle might create additional difficulty in performing ligament balance during TKA in Chinese. This is because more aggressive medial release may be required in restoring the limbs back to neutral mechanical axis. In the presence of a larger posterior condylar angle, if the femoral component is to be placed parallel to the transepicondylar axis, paradoxical medial laxity may occur in the flexion gap. This may result in midflexion instability of the replaced knee.
Fig. 7.
Distribution of mechanical axis of the lower limb. The mean mechanical axis was varus 1°. The alignment ranged from valgus 7° to valgus 8°. Thirteen knees had a lower limb mechanical axis alignment of varus 5° or more.
To conclude, we found an association between the joint line obliquity of the knee in the coronal plane and posterior condylar angle in the axial plane in young Chinese patients with ACL deficiency. Varus alignment of the lower limb in young patients without osteoarthritis was associated with larger posterior condylar angle of the distal femur.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the reporting of this case and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res. 1999;366:155–163. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed] [Google Scholar]
- 4.Chiu KY, Zhang SD, Zhang GH. Posterior slope of tibial plateau in Chinese. J Arthroplasty. 2000;15:224–227. doi: 10.1016/S0883-5403(00)90330-9. [DOI] [PubMed] [Google Scholar]
- 5.Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL. Anatomy of the epicondyles of the distal femur. MRI analysis of normal knees. J Arthroplasty. 2000;15:354–359. doi: 10.1016/S0883-5403(00)90739-3. [DOI] [PubMed] [Google Scholar]
- 6.Hood RW, Vanni M, Insall JN. The correction of knee alignment in 225 consecutive total condylar knee replacements. Clin Orthop Relat Res. 1981;160:94–105. [PubMed] [Google Scholar]
- 7.Hsu RWW, Himeno S, Coventry MB, Chao EYS. Normal axial alignment of the lower limb and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 8.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:13–22. [PubMed] [Google Scholar]
- 9.Jiang CC, Insall JN. Effect of rotation on the axial alignment of the femur. Pitfalls in the use of femoral intramedullary guides in total knee arthroplasty. Clin Orthop Relat Res. 1989;248:50–56. [PubMed] [Google Scholar]
- 10.Kellegren JH, Lawrence JS. Radiological assessment of osteoarthritis. Ann Rheum Dis. 1957;16:494–501. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ko PS, Tio MK, Ban CM, Mak YK, Ip FK, Lam JJ. Radiologic analysis of the tibial intramedullary canal in Chinese varus knees: implications in total knee arthroplasty. J Arthroplasty. 2001;16:212–215. doi: 10.1054/arth.2001.20908. [DOI] [PubMed] [Google Scholar]
- 12.Lie CWH, Yau WP, Chiu KY, Leung HB, Wong LLS, Wong SHM. Interobserver and intraobserver error in distal femur transepicondylar axis measurement with computed tomography. J Arthroplasty. 2009;24:96–100. doi: 10.1016/j.arth.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 14.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 15.Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE. Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: a prospective cohort study. Am J Sports Med. 2008;36:1717–1725. doi: 10.1177/0363546508316770. [DOI] [PubMed] [Google Scholar]
- 16.Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M. Patellofemoral osteoarthritis 15 years after anterior cruciate ligament injury—a prospective cohort study. Osteoarthritis Cartilage. 2009;17:284–290. doi: 10.1016/j.joca.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 17.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 18.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 19.Tang WM, Chiu KY, Kwan MF, Ng TP, Yau WP. Sagittal bowing of the distal femur in Chinese patients who require total knee arthroplasty. J Orthop Res. 2005;23:41–45. doi: 10.1016/j.orthres.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese patients. J Bone Joint Surg Am. 2000;82:1603–1608. doi: 10.2106/00004623-200011000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Yau WP, Chiu KY, Tang WM. Computer Navigation did not improve alignment in a lower-volume total knee practice. Clin Orthop Relat Res. 2008;466:935–945. doi: 10.1007/s11999-008-0144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong). 2007;15:32–36. doi: 10.1177/230949900701500108. [DOI] [PubMed] [Google Scholar]
- 23.Yip DK, Zhu YH, Chiu KY, Ng TP. Distal rotational alignment of the Chinese femur and its relevance in total knee arthroplasty. J Arthroplasty. 2004;19:613–619. doi: 10.1016/j.arth.2003.11.008. [DOI] [PubMed] [Google Scholar]