Abstract
Background
Femoral rotation on AP radiographs affects several parameters used to assess morphologic features of the proximal femur but its effect on femoroacetabular impingement parameters remains unknown.
Question/purposes
We therefore evaluated and characterized the potential effect of femoral rotation on (1) AP alpha angle, (2) lateral-center edge angle (LCEA), and (3) medial proximal femoral angle (MPFA) on AP hip radiographs.
Methods
We took seven AP hip radiographs at intervals of successive femoral rotation on a single dry, cadaveric specimen: 60°, 40°, and 20° internal rotation; 0° neutral/anatomic rotation; and 20°, 40°, and 50° external rotation. The AP alpha angle, LCEA, and MPFA were measured on all radiographs by two independent evaluators.
Results
Within the range of femoral rotation studied, the AP alpha angle ranged from 39° to 62°, the LCEA from 25° to 35°, and the MPFA from 70° to 115°. MPFA and AP alpha angle showed a linear relationship with femoral rotation. Each additional degree of internal rotation produced a reciprocal reduction of the MPFA by 0.36° and the AP alpha angle by 0.18° and vice versa in external rotation. The LCEA, especially within the internal rotation range, showed minimal variation.
Conclusions
These changes in radiographic parameters emphasize the importance of femoral rotation and patient positioning. We recommend radiographs be evaluated for excessive femoral rotation or nonstandardized positioning before interpretation for diagnostic and treatment implications. It may be prudent to repeat radiographs in these circumstances or, when standardized positioning is not feasible, proceed toward advance imaging.
Introduction
Symptomatic femoroacetabular impingement (FAI) is a known risk factor for hip osteoarthritis (OA) [8, 9]. This has led to increased interest in the early diagnosis of FAI via potential screening, especially in patients who are considered to be at high risk, such as elite athletes [10], athletes who participate in sports that have higher risks for changes in morphologic features of the hip [16, 24], and siblings of patients with impingement [30]. Abnormalities of morphologic features that can lead to FAI include cam abnormality on the femoral side and/or pincer overcoverage on the acetabular side [15, 33]. Normal parameters for both of these have been defined for plain radiography and advanced imaging [2, 5, 7, 14, 19, 29, 35, 37, 41]. The alpha angle, initially described by Notzli et al. [25] and validated on axial oblique images of MRI [25] (and subsequently CT [14]), has recently emerged as a method of quantifying the cam lesion. The lack of universal availability of MRI and potential uncertain risks of radiation from CT have been limitations with these imaging modalities, forcing exploration of the measurement methods with biplanar radiographs [2, 11, 23, 35] to ensure wider applicability for screening [12, 34]. More recently, AP radiographs have been used for assessment of cam morphology [2, 11, 23]. Additionally, other measurement parameters, such as the lateral center-edge angle (LCEA) [41] and medial proximal femoral angle (MPFA) [27], both originally validated on AP radiographs, have been adapted in diagnosing FAI acetabular morphologic features (pincer type) [5, 18, 29] and used to predict the progression of OA [1].
The emerging use of AP radiography (a convenient, low-cost, and widely available modality) for wider FAI evaluation inevitably invites concern of the well-documented variability in pelvic tilt, magnification, and femoral rotation associated with AP radiographs [3, 20, 32, 36, 38]. Femoral rotation reportedly affects the neck-shaft angle [17], femoral offset [40], Southwick slip angle [21], preoperative hip arthroplasty templating [20], and femoral canal measurements [6]. The use of FAI hip measurement parameters requires an accurate radiographic representation of the proximal femur on AP radiographs to be clinically reliable; on AP radiographs, femoral rotation, which may alter the appearance of the proximal femur, may substantially decrease the clinical reliability of these parameters. Currently, the effect of femoral rotation on FAI hip measurement parameters remains unknown.
We therefore evaluated and characterized the potential effect of femoral rotation on (1) AP alpha angle, (2) LCEA, and (3) MPFA on AP hip radiographs.
Materials and Methods
We procured a single, dry-bone cadaveric pelvis and femur from the same donor. On visual inspection and radiographic analysis, the dry cadaver did not show any grossly obvious proximal femoral deformity, acetabular dysplasia, degenerative disease, or secondary osseous changes related to labral abnormalities (Fig. 1). Institutional review board approval was not required, as this study did not use living subjects.
Fig. 1.

The cadaveric pelvis and proximal femur used in this study are shown.
Radiolucent umbilical tape, serving as an artificial ligamentum teres, was fastened to the femoral head with adhesive and attached to the center of the acetabulum to ensure stable containment of the femoral head in the pelvis during various degrees of rotation. The cadaveric pelvis and proximal femur was placed 4 feet (120 cm) from the x-ray machine (40- to 125-kVp range; SEDECAL IDEAL, SHF-520; SEDECAL, Madrid, Spain). The beam was centered at the hip and the position was not altered while the femur was rotated. A board-certified radiographer performed an AP hip radiograph of the cadaveric pelvis and the proximal femur in 0° neutral/anatomic rotation by placing a metal pin on the superior border of the central femoral head-neck-trochanter axis and ensuring this was parallel to the radiographic cassette [4, 13, 39]; additionally, in this position, a central line marking was made along the superior central axis of the proximal femur. This technique essentially negated the normal femoral anteversion, which was 20° in our cadaver. The normal anteversion was measured by placing the femur on a flat surface with femoral condyles flush to the surface and measuring the exact degree of anteversion of the femoral neck using a medical goniometer. With the pelvis secured, the acetabulum in a consistent position, and the femoral head in constant articulation, rotation was performed. We took care to avoid translation or gliding motion and the umbilical tape prevented any lateral subluxation of the femoral head. Using a medical goniometer, the axis marking previously drawn on the superior proximal femur in relation to the cassette was used to measure the exact degree of rotation. We then x-rayed the femur in rotations of 20°, 40°, and 60° internal rotation (IR) from the neutral position and 20°, 40°, and 50° external rotation (ER) from the neutral position for a total of seven radiographs (Fig. 2). The pelvis was secured to the table and remained in the same position while the femur was rotated. Sixty degrees ER was not possible with this cadaver owing to eventual mechanical femoroacetabular abutment.
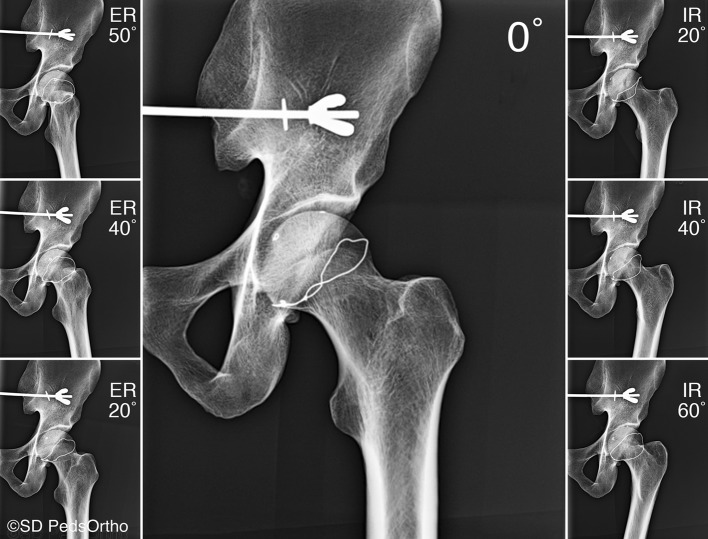
Fig. 2.
AP radiographs of the cadaver proximal femur in 50°, 40°, and 20° external rotation (ER), 0° neutral/anatomic rotation, and 20°, 40°, and 60° internal rotation (IR) are shown. A radiopaque wire had been glued to the cadaveric proximal femur to represent a theoretical growth plate for a previous unpublished study but was not used in this study.
Two of us (SM, MA) used Merge® PACS™ imaging software (Merge Healthcare Inc, Chicago, IL, USA) to measure the alpha angle [25, 35], LCEA [41], and MPFA [1, 27] on each femoral rotation radiograph (Fig. 3). Intraobserver and interobserver reliabilities for each measure were assessed using intraclass correlation (ICC) analysis to verify the reliability of the measurement method used in this study. ICC has a range between 0.0 and 1.0, with values closer to 1.0 representing stronger agreement. The interobserver reliability ICCs were 0.995 (95% CI, 0.972–0.999; p < 0.001) for the alpha angle, 0.739 (95% CI, 0.023–0.951; p = 0.005) for the LCEA, and 0.966 (95% CI, 0.835–0.994; p < 0.001) for the MPFA.
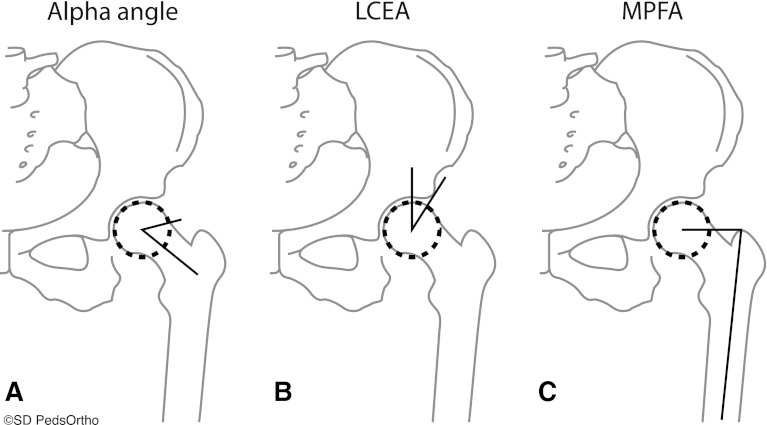
Fig. 3A–C.
The methods for measuring (A) the alpha angle, (B) lateral center-edge angle (LCEA), and (C) medial proximal femoral angle (MPFA) are shown. The alpha angle is formed between the line from the center of the femoral head to the middle of the narrowest part of the femoral neck and a line from the center of the femoral head to the point where the femoral head deviates from the circle contour. The LCEA is formed between a line from the center of the femoral head, vertically, and a line from the center of the femoral head to the lateral point of the acetabulum. The MPFA is formed between a line from the center of the femoral head to the proximal tip of the greater trochanter and a line from the proximal tip of the greater trochanter to the middle of the most distal part of the femur.
We used the two-way mixed model (absolute agreement), as the evaluators in this study were not randomly selected and were measuring identical radiographs. The average of the measurements of the two evaluators was used for analysis. We performed a linear regression analysis to further characterize the relationship among MPFA, alpha angle, and rotation. All statistical analyses were conducted using SPSS® software (SPSS Version 12; SPSS Inc, Chicago, IL, USA).
Results
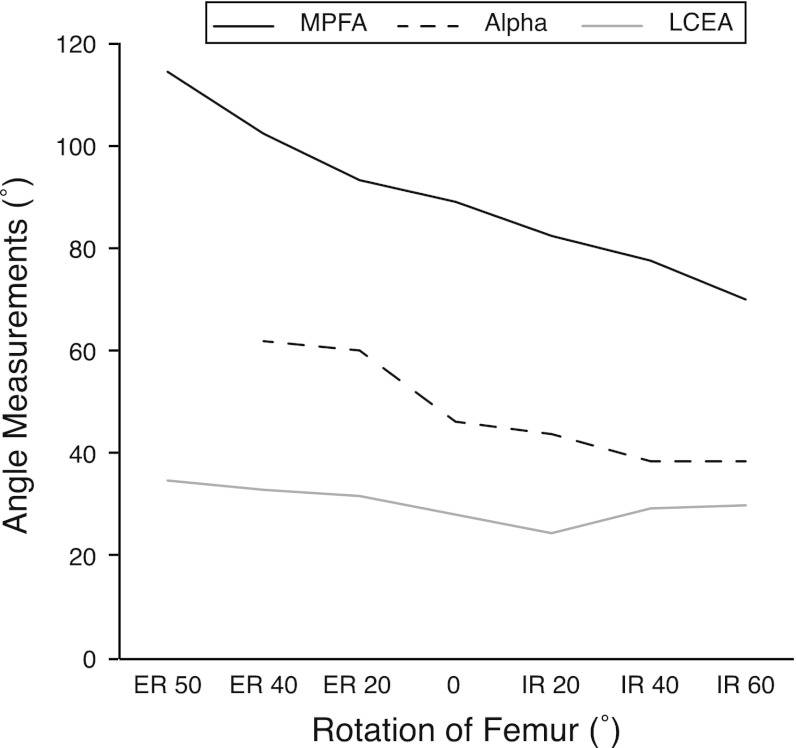
The alpha angle at 0° neutral/anatomic rotation was 46° and ranged overall from 39° to 62° with femoral rotation (Table 1). At 50° external rotation, the head-neck junction was not adequately observed to accurately measure the alpha angle. From 40° ER to 60° IR, there was a steady decrease in the alpha angle (Fig. 4). We found a linear relationship between alpha angle and rotation. Rotation accounted for approximately 58% of variation in the alpha angle. Linear regression analysis identified each additional 1° increase in IR reduced (p = 0.047) the alpha angle by approximately 0.176°.
Table 1.
Femoroacetabular impingement parameter measurements at each degree of femoral rotation
| Femoral rotation | Alpha angle (°) | Lateral center-edge angle (°) | Medial proximal femoral angle (°) |
|---|---|---|---|
| External rotation 50° | NA* | 35 | 115 |
| External rotation 40° | 62 | 33 | 102 |
| External rotation 20° | 60 | 32 | 94 |
| 0° | 46 | 28 | 89 |
| Internal rotation 20° | 44 | 25 | 83 |
| Internal rotation 40° | 39 | 30 | 78 |
| Internal rotation 60° | 39 | 30 | 70 |
Values are the averages of the two evaluators’ measurements; * the head-neck junction was not visible at 50° external rotation; NA = not applicable.
Fig. 4.
A graph shows the average of the two evaluators’ measurements of the alpha angle, lateral center-edge angle (LCEA), and medial proximal femoral angle (MPFA) from 50° external rotation (ER) to 60° internal rotation (IR). The effect of femoral rotation on the alpha angle and MPFA is characterized by a linear decrease in measurement with IR. The LCEA shows minimal variation with femoral rotation and no clear effect can be characterized.
The LCEA at 0° neutral/anatomic rotation was 28° and ranged overall from 25° to 35° with femoral rotation (Table 1). From 40° ER to 60° IR, there was only a maximum 5° variation from the 0° neutral/anatomic rotation, with the highest variation at 50° ER (Fig. 4). In the IR range, there was only a maximum 3° variation. We identified no clear relationship with femoral rotation.
The MPFA at 0° neutral/anatomic rotation was 89° and ranged overall from 70° to 115° with femoral rotation (Table 1). From 50° ER to 60° IR, there was a steady decrease in the MPFA (Fig. 4). We found a linear relationship between the MPFA and rotation. Rotation accounted for approximately 95% of the variation in the MPFA. Linear regression analysis identified each additional 1° increase in IR reduced (p < 0.001) the MPFA by approximately 0.359°.
Discussion
Approach to a patient with symptomatic FAI should include a thorough clinical examination, including the impingement test, followed by appropriate plain radiographs, which then are followed by advanced imaging [28]. Many patients presenting with nonspecific groin and hip pain during activities are being diagnosed as having FAI [26]. In many institutions, especially in the community where resources for advanced imaging are limited, standard imaging work-up for nonspecific groin and hip pain often begins with an AP radiograph of the pelvis. One should be aware of the associated variability in pelvic tilt, magnification, and femoral rotation [3, 20, 32, 36, 38], which may alter the radiographic appearance of the pelvis and/or proximal femur, while assessing and interpreting these biplanar radiographs. We therefore evaluated and characterized the potential effect of femoral rotation on (1) AP alpha angle, (2) LCEA, and (3) MPFA on AP hip radiographs.
This study had some limitations. First, we used only one cadaver, and the morphologic features of this cadaver hip were obviously individual to it. This study therefore should be considered a pilot study and any reported results will need to be confirmed in future studies with a large cohort of patients and/or specimens with varying morphologic features. Second, the MPFA, as described by Paley [27], uses the center of the distal femur in measuring the femoral axis. In a standard AP pelvic or hip radiograph, the distal femur is not seen, so we used the center of the distal portion of the visualized femur, as described by Bardakos and Villar [1], in which the MPFA predicted the likelihood of subsequent OA in FAI. Third, the radiographs performed in this study were AP hip radiographs and not true AP pelvic radiographs. However, the x-ray beam was placed at the same distance as in a true pelvic radiograph and was not altered in any way as the femur was rotated. Therefore, the beam was not a variable in the study and we would not expect differing results had the hip radiographs been true AP pelvic radiographs.
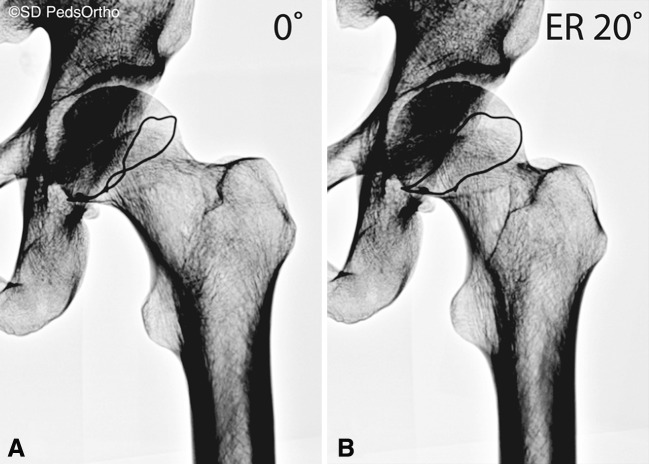
The alpha angle, which quantifies head-neck offset, has been used to describe cam morphology (ie, the loss of head-neck offset). Although described and validated on axial oblique images on MRI, there have been reports in the literature exploring its use on biplanar radiography [2, 23]. In this study, we found the alpha angle decreased with progressive IR of the femur and increased with ER. It was particularly concerning that only an ER of 20° was required to radiographically transform a normal alpha angle of 46° at the 0° neutral/anatomic position to an abnormal measurement of 61° (Fig. 4). The variability of the alpha angle with femoral rotation highlights the importance of standardization of patient positioning during radiography and a possible future need for the creation of a normative data atlas in different ages and sexes, with standardized rotation in asymptomatic hips without FAI. While reviewing literature related to the subject, one may have to be particularly cautious in interpreting retrospective studies that explored the utility of AP radiographs for cam morphology where standardization of patient positioning was not verified.
In contrast to the alpha angle, we found no large variation of the LCEA with femoral rotation. Minimal detectable changes for the LCEA have been reported to range from 3.0° to 6.0° [22]. All measurements, except at 50° ER, varied less than 6° from the 28° that the LCEA measured at 0° neutral/anatomic rotation. Although conceptually the femoral head often has been thought of as a perfect sphere, this is not the case, even in asymptomatic normal hips [31], and may account for the small variation seen in the LCEA with femoral rotation. A femoral head that is less or more spherical than the one used in this study may result in possibly more or less variability of the LCEA, respectively.
Similar to the alpha angle, the MPFA increased with ER and decreased with IR. Bardakos and Villar [1] reported a lower MPFA mean of 81° with a 7° SD in patients who progressed to OA versus a mean of 87° with a 7° SD in patients who did not progress to OA. In this study, we found a 5° minimum variation and a 22° maximum from the 0° neutral/anatomic rotation. In interpreting the increase in MPFA with IR, understanding the physics of conventional AP radiography is crucial. Traditional biplanar radiography uses a diverging conical x-ray beam that results in the magnification of structures that are closer to the x-ray beam, which in the case of AP radiographs, are the more anterior structures (Fig. 5). As the proximal femur internally rotates, the greater trochanter becomes more anterior and therefore will be magnified relative to the femoral head, as seen in the proximal femur with 60° IR (Fig. 1). This results in the greater trochanter proximal tip becoming more vertical on the AP radiograph relative to the center of the femoral head and therefore decreasing the MPFA. A relatively small difference is seen between patients who progress to OA and those who do not [1]. The large variation seen with even a minimal rotation of 20° raises concerns of the reliability of this measurement without strict standardization of patient positioning.
Fig. 5A–B.
AP radiographs show the cadaveric pelvis and proximal femur at (A) 0° neutral/anatomic rotation and (B) 20° external rotation (ER). No evidence of cam morphology is seen at 0° neutral/anatomic rotation, but with 20° ER, a radiograph image of cam morphology is apparent.
Plain radiography has remained the orthopaedist’s preferred diagnostic tool for more than a century. Even in the current era, it continues to be important in understanding and diagnosing more recently understood conditions, such as FAI. Global availability of plain radiographs is a strong positive, but the variable measurements found with femoral rotation highlights the importance of standardizing limb positioning and rotation while obtaining these radiographs. Our data suggest the need to evaluate each radiograph for evidence of excessive femoral rotation or nonstandard positioning before interpreting important radiographic parameters that have diagnostic and treatment implications. It may be prudent to repeat radiographs, or in circumstances where standardized positioning is not feasible, advance imaging may be recommended.
Acknowledgments
We thank Kai Ziebarth MD, Alia Karmali MBBS, and Diana Glaser PhD for help with the cadaver radiography.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91:162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 2.Barton C, Salineros MJ, Rakhra KS, Beaule PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469:464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell AL, Brand RA. Roentgenographic changes in proximal femoral dimensions due to hip rotation. Clin Orthop Relat Res. 1989;240:194–199. [PubMed] [Google Scholar]
- 4.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colvin AC, Koehler SM, Bird J. Can the change in center-edge angle during pincer trimming be reliably predicted? Clin Orthop Relat Res. 2011;469:1071–1074. doi: 10.1007/s11999-010-1581-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eckrich SG, Noble PC, Tullos HS. Effect of rotation on the radiographic appearance of the femoral canal. J Arthroplasty. 1994;9:419–426. doi: 10.1016/0883-5403(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 7.Fowkes LA, Petridou E, Zagorski C, Karuppiah A, Toms AP. Defining a reference range of acetabular inclination and center-edge angle of the hip in asymptomatic individuals. Skeletal Radiol. 2011;40:1427–1434. doi: 10.1007/s00256-011-1109-3. [DOI] [PubMed] [Google Scholar]
- 8.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 10.Gerhardt MB, Romero AA, Silvers HJ, Harris DJ, Watanabe D, Mandelbaum BR. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40:584–588. doi: 10.1177/0363546511432711. [DOI] [PubMed] [Google Scholar]
- 11.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49:436–441. doi: 10.1080/02841850801935567. [DOI] [PubMed] [Google Scholar]
- 12.Hailey D, Marshall D. The place of magnetic resonance imaging in health care. Health Policy. 1995;31:43–52. doi: 10.1016/0168-8510(94)00673-3. [DOI] [PubMed] [Google Scholar]
- 13.Hananouchi T, Sugano N, Nakamura N, Nishii T, Miki H, Yamamura M, Yoshikawa H. Preoperative templating of femoral components on plain X-rays: rotational evaluation with synthetic X-rays on ORTHODOC. Arch Orthop Trauma Surg. 2007;127:381–385. doi: 10.1007/s00402-007-0349-0. [DOI] [PubMed] [Google Scholar]
- 14.Heyworth BE, Dolan MM, Nguyen JT, Chen NC, Kelly BT. Preoperative three-dimensional CT predicts intraoperative findings in hip arthroscopy. Clin Orthop Relat Res. 2012;470:1950–1957. doi: 10.1007/s11999-012-2331-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 16.Kapron AL, Anderson AE, Aoki SK, Phillips LG, Petron DJ, Toth R, Peters CL. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93:e111(1–10). [DOI] [PubMed]
- 17.Kay RM, Jaki KA, Skaggs DL. The effect of femoral rotation on the projected femoral neck-shaft angle. J Pediatr Orthop. 2000;20:736–739. doi: 10.1097/01241398-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Kutty S, Schneider P, Faris P, Kiefer G, Frizzell B, Park R, Powell JN. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36:505–510. doi: 10.1007/s00264-011-1302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laborie LB, Lehmann TG, Engesaeter IO, Eastwood DM, Engesaeter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. doi: 10.1148/radiol.11102354. [DOI] [PubMed] [Google Scholar]
- 20.Linclau L, Dokter G, Peene P. Radiological aspects in preoperative planning and postoperative assessment of cementless total hip arthroplasty. Acta Orthop Belg. 1993;59:163–167. [PubMed] [Google Scholar]
- 21.Loder RT. Effect of femur position on the angular measurement of slipped capital femoral epiphysis. J Pediatr Orthop. 2001;21:488–494. [PubMed] [Google Scholar]
- 22.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. doi: 10.1007/s11999-010-1447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 24.Nepple JJ, Brophy RH, Matava MJ, Wright RW, Clohisy JC. Radiographic findings of femoroacetabular impingement in National Football League combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy. 2012;28:1396–1403. doi: 10.1016/j.arthro.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 26.Ochoa LM, Dawson L, Patzkowski JC, Hsu JR. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res. 2010;468:2710–2714. doi: 10.1007/s11999-010-1233-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paley D. Normal Lower limb alignment and joint orientation. Principles of Deformity Correction. New York, NY: Springer-Verlag; 2003:1–19.
- 28.Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561–570. doi: 10.5435/00124635-200709000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Philippon MJ, Wolff AB, Briggs KK, Zehms CT, Kuppersmith DA. Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center-edge angle. Arthroscopy. 2010;26:757–761. doi: 10.1016/j.arthro.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 30.Pollard TC, Villar RN, Norton MR, Fern ED, Williams MR, Murray DW, Carr AJ. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Joint Surg Br. 2010;92:209–216. doi: 10.2106/JBJS.I.01200. [DOI] [PubMed] [Google Scholar]
- 31.Sankar WN, Neubuerger CO, Moseley CF. Femoral head sphericity in untreated developmental dislocation of the hip. J Pediatr Orthop. 2010;30:558–561. doi: 10.1097/BPO.0b013e3181e4f53e. [DOI] [PubMed] [Google Scholar]
- 32.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 33.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 34.Stockburger WT. CT imaging, then and now: a 30-year review of the economics of computed tomography. Radiol Manage. 2004;26:20–22, 24–27; quiz 28–30. [PubMed]
- 35.Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CW. How useful is the alpha angle for discriminating between symptomatic patients with cam-type femoroacetabular impingement and asymptomatic volunteers? Radiology. 2012;264:514–521. doi: 10.1148/radiol.12112479. [DOI] [PubMed] [Google Scholar]
- 36.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 37.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis: what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 38.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 39.Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res. 2009;467:876–885. doi: 10.1007/s11999-008-0473-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Unnanuntana A, Toogood P, Hart D, Cooperman D, Grant RE. The evaluation of two references for restoring proximal femoral anatomy during total hip arthroplasty. Clin Anat. 2010;23:312–318. doi: 10.1002/ca.20921. [DOI] [PubMed] [Google Scholar]
- 41.Werner CM, Ramseier LE, Ruckstuhl T, Stromberg J, Copeland CE, Turen CH, Rufibach K, Bouaicha S. Normal values of Wiberg’s lateral center-edge angle and Lequesne’s acetabular index—a coxometric update. Skeletal Radiol. 2012;41:1273–1278. doi: 10.1007/s00256-012-1420-7. [DOI] [PubMed] [Google Scholar]