Abstract
Background
The factors that influence interest among medical students toward different medical specialties with time are important. The potential impact of changes in work-hour rules on orthopaedic applications in comparison to that of primary care medicine has not been reported. The change in number of applicants to general surgery during this period also is unknown.
Questions/purposes
The goals of our study were to assess the changes in orthopaedic applications relative to the 80-hour workweek and to compare these changes with those in the primary care field. We also documented the change in applications to general surgery after the work-hour changes.
Methods
A retrospective analysis of data from the National Resident Matching Program, San Francisco Matching Programs, and the American Urological Association from 1997 to 2010 was performed. Two cohorts of medical school applicants to primary care and surgery were established: those who applied from 1997 to 2002, predating work-hour changes, and those who applied from 2005 to 2010, after implementation of the 80-hour regulation. From the surgical data, applications to orthopaedic and general surgery were subselected and analyzed. Data were analyzed from a total applicant pool of 111,973 representing primary care and surgery applications. There were 59,996 and 51,977 applicants before and after the work-hour changes, respectively.
Results
Applications to orthopaedics increased by 21% (3310 to 4011 applicants) after implementation of work-hour changes, whereas primary care applications decreased by 18% (42,587 to 34,884 applicants) after the work-hour rules. General surgery applications decreased by 24% during this period.
Conclusions
Residency applications to orthopaedic surgery have increased since inception of the 80-hour workweek. By contrast, applications to primary care programs and general surgery have decreased after implementation of work-hour restrictions.
Introduction
Concerns about patient safety, working conditions for residents, and resident education led to implementation of work-hour restrictions, which are codified in Section 405 of the New York State Public Health Code, and in similar policies of the Accreditation Council for Graduate Medical Education. One such restriction, the 80-hour workweek, went into effect in 2003 [16]. Whether these regulations have been successful in fulfilling their objectives is unclear as there continues to be controversy nearly a decade after introduction of the regulations [4]. The relationship between physician fatigue and patient mortality is hard to describe because of numerous confounding factors [4]. Concerns regarding continuity of care, housestaff signouts, excessive cross-coverage, and handoffs have been raised as issues that may prove detrimental as work hours are lessened [6, 9, 12]. However, proponents of work-hour regulations argue that these rules protect patients from dangerously fatigued care providers [4, 16].
The 80-hour workweek also has had an impact on resident workload and attitude. Multiple studies have noted an improved quality of life for residents owing to the regulations, with the possible tradeoff being concerns about operative experience [10, 14, 19]. Although the impact of work-hour changes on the interest of medical students in general surgery has been studied [3, 18], we are unclear if the rate of applications to this field has changed. Similarly, the number of applicants to orthopaedic surgery and primary care (internal medicine, pediatrics, and family medicine) since the duty hour changes is unknown. Although there are likely multiple factors that determine ones commitment to a certain specialty, the comparative differences between orthopaedic surgery (a surgical field with historically longer residency work hours before the work-hour changes than the primary care field) and primary medicine since the work-hour changes were implemented may allow us to understand if the work-hour change may be a potential contributor to applicant interest.
The goals of this study were to (1) document the trend in the orthopaedic applicant pool before and after the 80-hour workweek implementation, (2) compare the changes noted with those seen in the primary care fields, and (3) evaluate the changes in relation to those seen in general surgery.
Materials and Methods
Data for this study were collected from online resources that are publicly available and put together by the National Resident Matching Program [13], San Francisco Matching Programs (SF Match) [15], and the American Urological Association [1]. These organizations historically have been responsible for conducting the match for those applying for a residency position in the United States. The information was fully blinded and provided on a yearly level. No specific data for individual applicants were reviewed or available. As such, our study is observational and we examined only the trends in the medical student applicant pool before and after the 80-hour work rule.
From 1997 to 2010, a 14-year period, we identified the number of US medical school students applying for a residency position in primary care (pediatrics, family care, and internal medicine) and the major surgical fields (orthopaedic surgery, general surgery, neurosurgery, ophthalmology, otolaryngology, and urology). We divided our applicant pool into two groups: Group 1 consisting of applicants from 1997 to 2002 and Group 2 consisting of those from 2005 to 2010, each group spanning a 6-year period before and after the work-hour changes, respectively. We determined 2005, 2 years after the work-hour changes, to be a sufficient time to begin our post-80 hour workweek regulation analysis because it allowed for implementation and adequate regulation of the new rule. We compared the number of applicants in each specialty of interest (primary care, orthopaedics, and general surgery) before and after the work-hour changes.
We examined a total of 111,973 applicants to surgery and primary care medicine from 1997 to 2010. There were a total of 59,996 and 51,977 applicants in primary care and surgery groups before and after the work-hour changes respectively (Table 1).
Table 1.
Applicant data
| Specialty | Before work-hour changes | After work-hour changes | Percentage change |
|---|---|---|---|
| Orthopaedics | 3310 | 4011 | 21.2 |
| Primary care | 42,587 | 34,884 | −18.1 |
| General surgery | 7182 | 5425 | −24.4 |
| Neurosurgery | 899 | 1080 | 20 |
| Urology | 1742 | 2159 | 24 |
| Ear, nose & throat | 1756 | 1717 | −2.2 |
| Ophthalmology | 2520 | 2701 | 7.2 |
| Total | 59,996 | 51,977 | 111,973 |
The primary outcome variable included within-group changes in number of applications to each field of interest. Applicants in the first and second groups were stratified as the unexposed and exposed populations, respectively. We compared these groups using a Pearson’s chi-square test. Odds ratios were calculated for those exposed to the 80-hour workweek versus those who were unexposed to it. Comparison groups are specified as either versus all applicants, all primary care and surgical or specific subspecialties (orthopaedic surgery) for the purposes of generating odds ratios. All statistics were calculated with SPSS Version 16.0 (SPSS Inc, Chicago, IL, USA).
Results
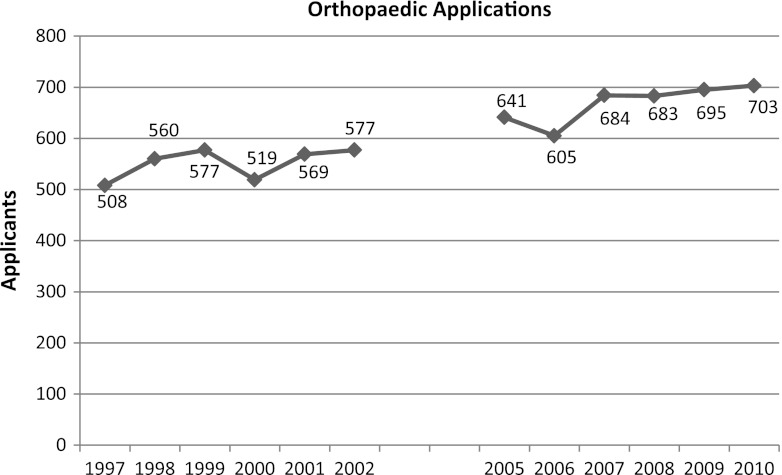
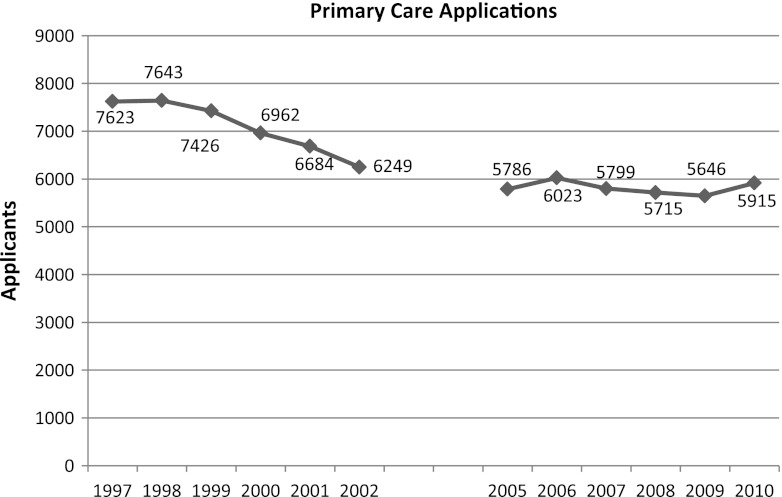
In the years following the new regulations, within-group analysis revealed that applications increased in orthopaedic surgery and decreased in primary care. Specifically, we noted a 21.2% (3310 to 4011; p < 0.001) increase in orthopaedic applications (Fig. 1) compared with a decline of 18.3% (42,587 to 34,884; p < 0.001) in primary care applications after the work-hour regulations (Fig. 2).
Fig. 1.
The changes in applications to orthopaedic surgery before and after the implementation of the 80-hour workweek are shown.
Fig. 2.
The changes in applications to primary care (PC) before and after implementation of the 80-hour workweek are shown.
Despite the increase in orthopaedic surgery applications, when the applications were aggregated, a decrease was seen in the overall number of applications to surgery (17,409 to 17,093). This was mostly the result of a significant decrease in general surgery applications (7182 to 5425; 24%; p < 0.001). The odds ratio of applying to a surgical field compared with primary care was 1.20 (range, 1.16–1.23) after the 80-hour workweek compared with the prework-hour changes. The odds ratio of going into orthopaedics compared with primary care was 1.48 (range, 1.41–1.55) after the 80-hour workweek compared with the prework hour changes.
Discussion
Our study revealed an increase in the number of applicants to orthopaedics after the work-hour changes. This is in contrast to the primary care field which has seen a major decline in applications during the past decade. These respective changes are likely multifactorial with the work-hour changes being only one possible factor. Other potential factors include the decreasing reimbursement for primary care physicians in comparison to more specialized fields and the increasing debt load of graduating US medical students [17]. In addition, we noted a decrease in applications to general surgery indicating an increased predilection for students to choose surgical subspecialty training despite a reduction of work hours in general surgery training. This also alludes to the complexities involved in trends and changes in interest toward certain fields with time.
Our study has several important limitations. First, it is an observational study, and observational studies in general cannot make causative connections between exposure and outcome. Therefore, we cannot surmise that the increased number of applications in orthopaedic surgery observed after the new work-hours restrictions are the result of those new regulations. Other study designs, perhaps including surveys, would be required to make inferences regarding causation. Our study is retrospective and therefore lacks the merits of a prospective and controlled study further complicating the ability to establish definitive conclusions. Owing to limitations in the dataset, subgroup and multivariate analyses could not be performed to exclude potential confounders. For example, the extent of medical student debt and age among applicants may influence how medical students choose their field of interest. Other confounders may include changes in physician reimbursement, job availability, and duration of training. Determining the effect of these variables is beyond the scope of our study but they may substantially affect what a medical student decides to pursue. In addition, we are unable to determine how the changes noted in our study periods compare with trends seen in the past, for example, we do not know the magnitude of change in the number of applicants to primary care before the start of our study period. Despite these weaknesses, this study may serve as a pilot for further investigation into this topic and provides insight into the trends in this field with respect to the work hours.
We noted a substantial increase in medical student applications to orthopaedics since the change in work hours. Although it is not our intent to imply that this is specifically attributable to the hour changes, this information allows for further evaluation and speculation of its impact on the field. While this has not been studied previously, other potential consequences of the work-hour changes in orthopaedic training have been reported. The theory that reduced work hours are associated with decreased stress and better-rested trainees has been clearly documented [10, 11, 14]. This is countered by concerns regarding lack of operative experience and education with this rule [19] that, to date, has not been objectively proven [7]. Baskies et al. reviewed operative logs and noted that residents actually participated in more cases after the work-hour implementation [5].
Our data indicate that since the work-hour restrictions were instituted, the number of applicants to primary care medicine has decreased overall and also in comparison to orthopaedics. This finding likely is multifactorial, but it may be driven partly by medical students who may elect not to pursue primary care training if they perceive that the work hours do not differ substantially compared with specialty training. This is important in an uncertain healthcare environment that has included recent congressional emphasis on stimulating interest in primary care to help reduce excessive healthcare costs [8]. Whether the work-hour changes influence the direction of primary care medicine remains to be fully elucidated and should be an area of future research.
In a survey study of medical students before and after their general surgery rotations [2], the change in work hours was associated with a more favorable impression of a general surgeon’s lifestyle. However, they did not note an increase in interest as far as likelihood to go into general surgery. It was important for us to decipher whether applicants may be averse to primary care training alone or if there is a general aversion to nonspecialty training even in the surgical realm. We noted a substantial decline in students applying to general surgery despite a reduction in work hours. Therefore, even in the presence of relatively easier residency training, medical students still choose to pursue surgical specialties like orthopaedic surgery, indicating that the motivation to pursue a specific field is related to multiple factors at any given time. It also alludes to a general proclivity for graduating medical students to seek specialty training whether in a medical or surgical field.
To the best of our knowledge this is the first study to address the number of applications to orthopaedic surgery residencies since the inception of the 80-hour workweek, and compare this number with that in primary care medicine. Applications to orthopaedic surgery programs have increased since the inception of the 80-hour workweek. This is in contrast to primary care and general surgery, which have seen precipitous decreases in applicants since the inception of the 80-hour workweek.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at University of Pennsylvania Medical Center, Philadelphia, PA.
Contributor Information
Oke A. Anakwenze, Email: oanakwenze@gmail.com.
Samir Mehta, Email: Samir.Mehta@uphs.upenn.edu.
References
- 1.American Urological Association. Residency Match 2013. Available at: http://www.auanet.org/content/residency/residency-match.cfm#statistics. Accessed August 9, 2012.
- 2.Arnold MW, Patterson AF, Tang AS. Has implementation of the 80-hour work week made a career in surgery more appealing to medical students? Am J Surg. 2005;189:129–133. doi: 10.1016/j.amjsurg.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Bakaeen FG. The 80-hour work week and interest in surgery. J Surg Res. 2011;165:49–51. doi: 10.1016/j.jss.2010.08.044. [DOI] [PubMed] [Google Scholar]
- 4.Baldwin K, Namdari S, Donegan D, Kamath AF, Mehta S. Early effects of resident work-hour restrictions on patient safety: a systematic review and plea for improved studies. J Bone Joint Surg Am. 2011;93:e5. doi: 10.2106/JBJS.J.00367. [DOI] [PubMed] [Google Scholar]
- 5.Baskies MA, Ruchelsman DE, Capeci CM, Zuckerman JD, Egol KA. Operative experience in an orthopaedic surgery residency program: the effect of work-hour restrictions. J Bone Joint Surg Am. 2008;90:924–927. doi: 10.2106/JBJS.G.00918. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein J, MacCourt DC, Jacob DM, Mehta S. Utilizing information technology to mitigate the handoff risks caused by resident work hour restrictions. Clin Orthop Relat Res. 2010;468:2627–2632. doi: 10.1007/s11999-010-1376-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Froelich J, Milbrandt JC, Allan DG. Impact of the 80-hour workweek on surgical exposure and national in-training examination scores in an orthopedic residency program. J Surg Educ. 2009;66:85–88. doi: 10.1016/j.jsurg.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Iglehart JK. Health reform, primary care, and graduate medical education. N Engl J Med. 2010;363:584–590. doi: 10.1056/NEJMhpr1006115. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan LJ, Maerz LL, Schuster K, Lui F, Johnson D, Roesler D, Luckianow G, Davis KA. Uncovering system errors using a rapid response team: cross-coverage caught in the crossfire. J Trauma. 2009;67:173–178; discussion 178–179. [DOI] [PubMed]
- 10.Kusuma SK, Mehta S, Sirkin M, Yates AJ, Miclau T, Templeton KJ, Friedlaender GE. Measuring the attitudes and impact of the eighty-hour workweek rules on orthopaedic surgery residents. J Bone Joint Surg Am. 2007;89:679–685. doi: 10.2106/JBJS.F.00526. [DOI] [PubMed] [Google Scholar]
- 11.Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, Rothschild JM, Katz JT, Lilly CM, Stone PH, Aeschbach D, Harvard Work Hours, Health and Safety Group Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 12.Morrissey S, Dumire R, Bost J, Gregory JS. Feasibility of and barriers to continuity of care in US general surgery residencies with an 80-hour duty week. Am J Surg. 2011;201:310–313; discussion 313–314. [DOI] [PubMed]
- 13.National Resident Match Program. NRMP Historical Reports. Available at: http://www.nrmp.org/data/historicalreports.html#mainmatch. Accessed August 7, 2012.
- 14.Peabody T. The effect of work hour restrictions on the education of orthopaedic surgery residents. Clin Orthop Relat Res. 2006;449:128–133. doi: 10.1097/01.blo.0000224037.54345.77. [DOI] [PubMed] [Google Scholar]
- 15.San Francisco Matching Programs. SF Match Residency and Fellowship Matching Services. Available at: http://www.sfmatch.org/. Accessed August 7, 2012.
- 16.Steinbrook R. The debate over residents’ work hours. N Engl J Med. 2002;347:1296–1302. doi: 10.1056/NEJMhpr022383. [DOI] [PubMed] [Google Scholar]
- 17.Woo B. Primary care: the best job in medicine? N Engl J Med. 2006;355:864–866. doi: 10.1056/NEJMp068154. [DOI] [PubMed] [Google Scholar]
- 18.Zarebczan B, Rajamanickam V, Lewis B, Leverson G, Sippel RS. The impact of the 80-hour work week on student interest in a surgical career. J Surg Res. 2011;171:422–426. doi: 10.1016/j.jss.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zuckerman JD, Kubiak EN, Immerman I, Dicesare P. The early effects of code 405 work rules on attitudes of orthopaedic residents and attending surgeons. J Bone Joint Surg Am. 2005;87:903–908. doi: 10.2106/JBJS.D.02801. [DOI] [PubMed] [Google Scholar]