Abstract
Background
Studies concerning the relationship between distal radius fracture malunion and a persistent arm-related disability have produced conflicting results.
Questions/purposes
We investigated (1) how arm-related disability changes during the first 2 years after a fracture and (2) whether fracture malunion causes persistent disability.
Methods
One hundred twenty-three patients with distal radius fractures, treated with closed reduction and casts or external or percutaneous pin fixations, completed the DASH questionnaire at baseline, 3 months, 6 months, 1 year, and 2 years after fracture. Radiographic measurements were made at 1 year. Using a definition of malunion as ulnar variance of 1 mm or more and dorsal tilt greater than 10°, the patients were classified into three groups: no malunion (n = 35), malunion involving either ulnar variance or dorsal tilt (n = 65), and malunion involving ulnar variance and dorsal tilt (n = 23). The changes in the DASH scores with time (baseline to 2 years), in relation to malunion, were analyzed using generalized estimating equations adjusted for age, sex, fracture type (extraarticular or intraarticular), and treatment method.
Results
The mean change in DASH scores from baseline to 2 years was worse for patients with malunions involving ulnar variance and dorsal tilt than for patients with no malunions (mean difference, 13; 95% CI, 1.4–25) and for patients with malunions involving either ulnar variance or dorsal tilt (mean difference, 13; 95% CI, 2.2–24).
Conclusion
After distal radius fracture, arm-related disabilities are more likely to persist at least 2 years in patients with fractures that healed with shortening and dorsal angulation than in patients with only shortening or dorsal angulation or without malunion.
Level of evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Fractures of the distal radius commonly cause functional declines in postmenopausal women [8]. Studies [2, 11] concerning the relationship between distal radius fracture malunions and persistent long-term, arm-related disabilities have produced conflicting results. Retrospective studies of patients with distal radius fracture have shown severe malunion to be a common cause of long-term pain and disability. Few prospective studies have used patient-reported outcome measures to investigate the change in disability and pain with time after a distal radius fracture. In a study that used the Patient-Rated Wrist Evaluation (PRWE) questionnaire, most patients had minimal pain and disabilities 6 months after distal radius fractures, but at 1 year, almost one of 10 patients had persistent moderate-to-severe pain and activity limitations [21]. That study provided useful information about the course of recovery during the first year but did not address the determinants of persistent disability.
We previously showed, in patients with distal radius fractures initially treated with closed reductions and casts or with external or percutaneous pin fixations, the degree of disability at 1 year is related to the severity of the fracture malunions [6]. It is not known, however, whether this relationship persists beyond 1 year after time of fracture.
We asked (1) how arm-related disability changes over 2 years after a distal radius fracture treated with closed reduction and cast or with external or percutaneous pin fixation and (2) whether fracture malunion influences patient-reported disability up to 2 years after the fracture.
Patients and Methods
The study population was described previously [6]. During a 15-month period starting January 2001, we performed a prospective cohort study of the patients who attended the two emergency departments in the region of Northeastern Scania in Sweden (Kristianstad and Hässleholm Hospitals) with acute extraarticular or intraarticular fractures of the distal radius. All patients were invited to participate in a longitudinal study consisting of repeated measurement of patient-reported disability up to 2 years using the DASH questionnaire and clinical and radiographic examinations at the hospital at 1 year. The current study was designed to include all patients treated with closed reductions and casts or with closed reductions and external fixation or percutaneous pin fixations. The treatment method was decided by the orthopaedic surgeon in the emergency department (general orthopaedic surgeon or resident in orthopaedic surgery after consultation with an orthopaedic surgeon), based on the clinical evaluation of the patient and the radiographic appearance of the fracture. The study was approved by the Regional Ethical Review Board (LU 516-01) and informed consent was obtained from the patients.
Of 175 consecutive patients, seven patients died within 2 years from fracture, nine declined to participate, 10 were excluded because of severe medical illnesses or cognitive disorders, 10 were excluded because of treatment with open reduction and internal fixation, two did not respond to the outcome measure, and 14 did not attend their followup radiographic examinations. Thus, 123 patients (94 women, 29 men) with a mean age of 63 years (SD, 15 years; range, 19–88 years) were included in this study. The treatment methods were closed reductions and casts in 46 patients (38 women) and closed reductions and fixations in 77 patients (56 women). In the closed reduction and fixation group, 63 patients were treated with external fixations (11 were treated because of fracture redisplacement after initial nonsurgical treatments), five with external fixations and percutaneous pinnings (three were treated after initial nonsurgical treatments), and nine with percutaneous pinning only. The trauma was moderate (falls from the same level) in 79 patients, severe (such as falls from great heights, traffic accidents, and sport injuries) in 43 patients, and of an unknown type in one patient.
At the time of the study, the standard management for a displaced distal radius fracture consisted of an initial reduction and a cast at the emergency department, followed by a postreduction radiograph. If the reduction was judged to be satisfactory, the patient returned to the orthopaedic outpatient department after 7 to 10 days for clinical and radiographic examinations. If the examining surgeon decided to continue cast treatment, the patient was referred to a physiotherapist for cast removal 4 to 5 weeks after the fracture followed by therapy. No further routine followup visits were planned. In case of fracture redisplacement, the patients were offered closed reduction and external fixation. If the initial reduction was unsatisfactory, the patient was treated with closed reduction and external fixation or percutaneous pinning, referred to a physiotherapist for initiation of exercises, and returned to the orthopaedic outpatient department at 5 to 6 weeks postoperatively for removal of the fixation device. The frequency and duration of the therapy were decided by the therapist.
The patients completed the DASH questionnaire at baseline (questionnaires were mailed to patients from the trauma center within 1 week of their fractures and inquired about the patients’ abilities to perform activities the week before their fractures), 3 months, 6 months, 1 year, and 2 years. On all occasions, the DASH questionnaire was sent to the patients by mail. The DASH questionnaire is scored from 0 to 100, with a higher score indicating higher disability [4, 14]. The questionnaire has been used as an outcome measure after distal radius fractures [20] and the minimum, clinically important difference in a DASH score has been estimated to be 10 points in patients with various upper-extremity disorders [13]. When responding to the DASH questionnaire at the 1-year and 2-year followups, the patients had no knowledge of the results of the 1-year radiographic examination (information was planned to be given at study conclusion). DASH scores were missing in 32 (26%) patients at baseline, 26 (21%) patients at 3 months, 38 (31%) patients at 6 months, 26 (21%) patients at 1 year, and 23 (19%) patients at 2 years.
Before treatment began, posteroanterior and lateral radiographs were obtained. At 1 year after the fracture, a radiographic examination of both wrists was performed. Standard radiographic projections were used and forearm rotation carefully controlled. At the conclusion of the study, an experienced radiologist (MP) with no knowledge of the patient’s DASH responses classified the fractures on the initial radiographs as extraarticular or intraarticular. The radiologist measured ulnar variance, dorsal tilt measured from neutral angulation, radial inclination, and intraarticular step-off of the injured wrist on the baseline and 1-year radiographs and of the noninjured wrist on the 1-year radiographs. The reliability of the radiographic measurements in the study population was assessed previously and was found to be high (intraclass correlation coefficient of agreement between two examiners ranged from 0.88 to 0.94) [6]. Radiographs of the noninjured wrist were missing in seven patients. Clinical or radiographic status of the distal radioulnar joint other than ulnar variance, dorsal tilt, and articular step-off was not assessed.
The change in the DASH score with time (baseline to 2 years) was the primary outcome. We investigated the influence of fracture alignment after healing on the DASH score by analyzing individual radiographic variables and a combination of radiographic variables. The mean difference in the change in the DASH score, according to the radiographic outcome, was estimated using generalized estimating equations (GEE), adjusting for baseline factors. This method is an extension of ordinary regression analysis and was used to account for the within-subject correlation that often occurs in longitudinal data. Another advantage of the GEE is that it uses all available data from all patients in the analysis [19], with the DASH score from all times (including baseline) considered as the outcome. In the GEE analyses, the change from baseline at each time was estimated using indicator variables for each of the times. The difference in change for the radiographic outcomes was estimated using interaction terms involving the time indicators and the radiographic variables. In all analyses, an exchangeable correlation structure was assumed. The results from the GEE analyses are interpreted similarly to the results from an ordinary regression analysis. Our first GEE analysis involved the relationships between the individual radiographic variables (ulnar variance, dorsal tilt, radial inclination) and the change in the DASH score from baseline to 2 years. The mean differences in change in the DASH score, according to ulnar variance, dorsal tilt, or radial inclination, were estimated, adjusting for age, sex, fracture type (extraarticular or intraarticular), treatment method, and the corresponding measurement on the contralateral wrist (to adjust for possible anatomic variations). This analysis included data from all except the seven patients without contralateral wrist radiographs.
Our second GEE analysis involved comparing disabilities in patients with or without malunions. Based on the radiographic measurements of the injured wrist at 1 year and using the values of ulnar variance of 1 mm or more and dorsal tilt greater than 10° as malunion, we classified the patients into three groups: patients with no malunion, patients with a malunion type involving either ulnar variance or dorsal tilt, and patients with a malunion type involving both these magnitudes of ulnar variance and dorsal tilt. The cutoff value for dorsal tilt was chosen following consensus recommendations based on several biomechanical and clinical studies [12, 22] that have suggested a dorsal tilt exceeding 10° should not be accepted. Recommendations regarding the amount of positive ulnar variance that may be considered acceptable vary, ranging from 1 to 6 mm [16, 18, 22]. We chose to consider an ulnar variance of 1 mm or greater as malunion because of the lack of convincing evidence suggesting only greater incongruity of the distal radioulnar joint is important regarding disability. In a previous study [6], we found a significant independent relationship between the DASH score and dorsal tilt and ulnar variance but not with radial inclination, which therefore was not included in the definition of malunion. Using GEE, we estimated the mean differences in the change in DASH score from baseline to 2 years according to the malunion type, adjusting for age, sex, fracture type (extraarticular or intraarticular), and treatment method. This analysis included data from all 123 patients.
Additionally, a sensitivity analysis was performed for all GEE models on the subgroup of patients who had baseline DASH scores [19]. The analysis consisted of using the baseline score as a covariate (instead of as part of the primary outcome) and comparing the results with and without adjusting for the baseline DASH score; this showed similar results (ie, the missing baseline scores did not affect the results). To investigate the relationship between fracture type (extraarticular or intraarticular) and the DASH score at 2 years, we also performed an analysis of covariance, adjusting for age, sex, and treatment method. All tests were two-sided. Statistically significant p values were considered to be less than 0.05.
Results
Complications included superficial pin site infection treated with antibiotics in 26 patients. Four other complications were recorded each in one patient: (1) a rupture of the extensor pollicis longus tendon; (2) chronic regional pain syndrome; (3) osteomyelitis of the second metacarpal that resolved with antibiotics; and (4) thumb adduction contracture that improved with physiotherapy. The first three belonged to the external fixation or percutaneous pinning group and the fourth to the closed reduction and cast group; all four patients belonged to the group with malunions involving either ulnar variance or dorsal tilt. No patients underwent corrective osteotomy during the study period.
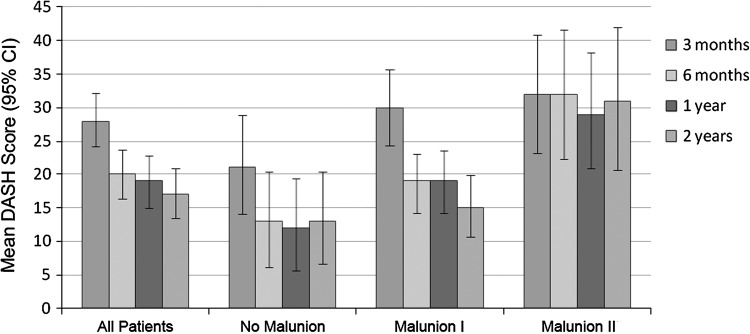
Arm-related disability was highest at 3 months after the fracture and then decreased with time (Table 1). The largest improvement occurred at 6 months, with further smaller improvement up to 2 years (Fig. 1). The mean DASH score did not reach preinjury level (mean, 4.9; SD, 9.2) during the 2-year followup.
Table 1.
Differences in the change in DASH score according to malunion type and time since fracture
| Malunion type* and time since fracture | Mean change in DASH score from baseline† | 95% CI | p value |
|---|---|---|---|
| No malunion (n = 35) | |||
| 3 months | 20 | 13–26 | < 0.001 |
| 6 months | 13 | 5.9–19 | < 0.001 |
| 1 year | 11 | 4.8–17 | 0.001 |
| 2 years | 9.9 | 3.7–16 | 0.002 |
| Malunion Type I (n = 65) | |||
| 3 months | 25 | 19–30 | < 0.001 |
| 6 months | 16 | 12–19 | < 0.001 |
| 1 year | 15 | 10–19 | < 0.001 |
| 2 years | 10 | 5.9–14 | < 0.001 |
| Malunion Type II (n = 23) | |||
| 3 months | 24 | 14–33 | < 0.001 |
| 6 months | 23 | 15–30 | < 0.001 |
| 1 year | 20 | 12–29 | < 0.001 |
| 2 years | 23 | 13–33 | < 0.001 |
* No malunion = ulnar variance 0 mm or less and dorsal tilt 10° or less; Malunion Type I = ulnar variance 1 mm or more or dorsal tilt less than 10°; Malunion Type II = ulnar variance 1 mm or more and dorsal tilt less than 10°; †generalized estimating equations, adjusting for age, sex, fracture type (extraarticular or intraarticular), and treatment method; the analysis included all 123 patients.
Fig. 1.
A graph shows the mean DASH scores at 3 months, 6 months, 1 year, and 2 years after distal radius fracture. No malunion = ulnar variance of 0 mm or less and dorsal tilt of 10° or less; Malunion Type I = ulnar variance of 1 mm or more or dorsal tilt greater than 10°; Malunion Type II = ulnar variance of 1 mm or more and dorsal tilt greater than 10°.
Fracture malunion was associated with higher arm-related disability over 2 years. The mean change in DASH score increased with positive ulnar variance and with dorsal tilt, whereas radial inclination had no effect (Table 2). The mean ulnar variance of the injured wrist was 2.6 mm (SD, 3.5 mm) at baseline and 2.5 mm (SD, 3.4 mm) at 1 year and that of the uninjured wrist was 0 mm (SD, 1.7 mm). The mean dorsal tilt was 20° (SD, 17°) at baseline and 3° (SD, 11°) at 1 year and that of the uninjured wrist was −8° (SD, 8°). The mean radial inclination was 15° (SD, 7°) at baseline and 18° (SD, 6°) at 1 year and that of the uninjured wrist was 22° (SD, 4°).
Table 2.
Differences in the change in the DASH score according to radiographic variable
| Radiographic variable | Mean difference in change in DASH score from baseline* | 95% CI | p value |
|---|---|---|---|
| Ulnar variance (mm) | 1.35 | 0.26–2.45 | 0.016 |
| Dorsal tilt (°) | 0.40 | 0.06–0.73 | 0.021 |
| Radial inclination (°) | −0.24 | −0.92 to 0.45 | 0.497 |
* Generalized estimating equations, adjusting for age, sex, fracture type (extraarticular or intraarticular), treatment method, and the corresponding radiographic value of the contralateral side; the analysis included 116 patients.
The mean change in DASH score over 2 years was less in the 23 patients with malunion involving ulnar variance and dorsal tilt than in the 35 patients with no malunion (adjusted mean difference, 13; 95% CI, 1.4–25) and in the 65 patients with malunion involving either ulnar variance or dorsal tilt (adjusted mean difference, 13; 95% CI, 2.2–24) (Table 3).
Table 3.
Differences in the change in the DASH score according to malunion type
| Comparison of malunion types* | Mean difference in change in DASH score from baseline† | 95% CI | p value |
|---|---|---|---|
| Malunion Type II versus no malunion | 13 | 1.4–25 | 0.028 |
| Malunion Type II versus Malunion Type I | 13 | 2.2–24 | 0.018 |
| Malunion Type I versus no malunion | 0.2 | −7.3 to 7.7 | 0.961 |
* No malunion = ulnar variance 0 mm or less and dorsal tilt 10° or less; Malunion Type I = ulnar variance 1 mm or more or dorsal tilt less than 10°; Malunion Type II = ulnar variance 1 mm or more and dorsal tilt less that 10°; †generalized estimating equations adjusting for age, sex, fracture type (extraarticular or intraarticular), and treatment method; analysis including all 123 patients.
Intraarticular step-off of 1 mm or more at 1 year was found in seven patients. Fracture type had no influence on arm-related disability. For extraarticular fractures (n = 88), the mean DASH score was 4.7 (SD, 9.3) at baseline and 17 (SD, 19) at 2 years. For intraarticular fractures (n = 35), it was 5.2 (SD, 9.2) and 17 (SD, 19), respectively, with a mean difference in the 2-year DASH score of 0.1 (95% CI, −7.7 to 7.9) (p = 0.97).
Discussion
Studies concerning the relationship between distal radius fracture malunion and a persistent arm-related disability have produced conflicting results. We investigated (1) how arm-related disability changes during the first 2 years in distal radius fractures treated with closed reduction and cast or with external or percutaneous pin fixation and (2) whether fracture malunion causes persistent disability. We found patient-reported disability was, on average, highest at 3 months. After 6 months, improvement in disability was considerably slower, and even though the mean DASH score was low after 6 months, it did not reach preinjury level. We also found patients with malunions involving a positive ulnar variance and substantial dorsal tilt had worse disability over 2 years. In addition, we found fracture type (extraarticular or intraarticular) did not influence arm-related disability at 2 years after the fracture, which is in agreement with previous studies [7, 10].
This study has limitations. Complete followup data were not available for all the patients. To handle the missing data, we used GEE models assessed with sensitivity analyses; this method uses data from all patients, including those with incomplete followup, to improve the precision of the estimates [19]. The treatment methods used in this study generally have been replaced by open reduction and fixation with volar plates. However, because the definition of malunion was based on 1-year radiographs of healed fractures regardless of treatment method, it is reasonable to speculate the effect of malunion would be similar for the same type of fractures treated with internal fixation. Further, treatment method was adjusted for in all analyses and it is unlikely factors related to the type of treatment (closed reduction followed by cast, pinning, or external fixation) influenced disability 2 years after fracture, beyond their possible effect on the occurrence of malunion. Another limitation is the large age range (19–88 years), although age was adjusted for in all analyses. The baseline DASH scores (mean, 4.9; SD, 9.2) obtained within 1 week after the trauma (inquiring about the function before the fracture) were lower than the normative values for the US general population (mean, 10; SD, 15) [15] but similar to those for a random Swedish general population sample of 71 persons of similar age and sex characteristics (median, 2.5) [1]. We did not assess the potential effect of associated distal radioulnar joint instability, but a recent study showed a lack of association between instability of the distal radioulnar joint and DASH score after fracture [24]. We also did not investigate with the DASH questionnaire whether symptomatic degenerative arthritis developed between the 1-year radiographic examination and the 2-year followup. However, it is unlikely this would have occurred in a substantial number of patients to be a major issue.
Our study also has several strengths. It was prospectively conducted at the only facility that manages this type of fracture in the target population. During 15 months, the majority of patients in the population who were treated for acute distal radius fracture with closed reduction and cast or external or percutaneous fixation participated in the study. To our knowledge, no other prospective study has presented 2-year followup results based on radiographic examination of the injured and uninjured wrists after the fracture had healed and used an established patient-reported disability measure.
Our findings are partly in agreement with those reported by MacDermid et al. [21] in their study of 129 patients evaluated with the PRWE score at 2, 3, 6, and 12 months after distal radius fractures. They suggested the high level of disability at 2 to 3 months after the fracture coincided with the reparative phase of bone and soft tissue healing, and during a rehabilitative phase, a slower improvement in pain and disability occurs; the majority of their patients had recovered at 6 months after the fractures. In our study, patients whose fractures healed with positive ulnar variances and substantial dorsal tilts showed slower improvement in disability, and at 2 years, their mean DASH scores had not decreased to the same levels as the patients with no fracture malunions. MacDermid et al. [21] reported a minority of their patients experienced prolonged disability at 1 year, although they did not report any specific determinants of worse outcome.
Several studies [12, 17, 22] have suggested a strong relationship between anatomic restoration and function after fracture, whereas others [7, 25] have reported the precision of fracture reduction and the degree to which it is maintained have no predictive value. Some authors [3, 9, 28] have reported satisfactory function regardless of radiographic deformity, especially among the elderly. We recently reported a relationship between a more pronounced fracture malunion and greater age-adjusted patient-reported disability 1 year after a distal radius fracture [6]. In that analysis, we found this relationship persisted up to 2 years after the fracture. Ulnar variance and dorsal tilt affected the patient-reported disability up to 2 years after the fracture, whereas radial inclination did not. A positive ulnar variance is thought to alter loading of the wrist [23] and has been shown to affect subjective outcome, grip strength, and ROM after distal radius fractures [5, 27]. Dorsal tilt may alter the force distribution in the radiocarpal joint, increasing the load through the ulna, and may result in midcarpal instability [26]. Fractures that heal with dorsal tilt have been related to weaker grip strength, persistent pain, and increased difficulties with everyday activities and work [12, 17, 22]. Patients with malunion, however, involving only positive ulnar variance with no or minor dorsal tilt or only substantial dorsal tilt with neutral or negative ulnar variances, did not have worse DASH scores than patients with no malunions. This finding suggests the combination of a substantial dorsal tilt and positive ulnar variance appears to cause the persistent disability, although the exact reason is unknown. A possible explanation may be that substantial dorsal tilt accentuates the incongruity of the distal radioulnar joint caused by the radial shortening.
The finding of a relationship between a distal radius fracture malunion and persistent patient-reported disability up to 2 years after the fracture supports the use of treatment methods that minimize the risk of a malunion. Patients with persistent disability at 1 year after fracture showing a malunion with positive ulnar variances and substantial dorsal tilts may be considered for corrective osteotomies.
Acknowledgments
We thank Mats Billsten for help with data acquisition and Gunilla Persson for administrative assistance.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Department of Orthopedics Hässleholm-Krisitianstad, Hässleholm Hospital, Hässleholm, Sweden.
References
- 1.Abramo A, Kopylov P, Tagil M. Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthop. 2008;79:376–385. doi: 10.1080/17453670710015283. [DOI] [PubMed] [Google Scholar]
- 2.Altissimi M, Antenucci R, Fiacca C, Mancini GB. Long-term results of conservative treatment of fractures of the distal radius. Clin Orthop Relat Res. 1986;206:202–210. [PubMed] [Google Scholar]
- 3.Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93:2146–2153. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 4.Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand. 2000;71:613–618. doi: 10.1080/000164700317362262. [DOI] [PubMed] [Google Scholar]
- 5.Batra S, Gupta A. The effect of fracture-related factors on the functional outcome at 1 year in distal radius fractures. Injury. 2002;33:499–502. doi: 10.1016/S0020-1383(01)00174-7. [DOI] [PubMed] [Google Scholar]
- 6.Brogren E, Hofer M, Petranek M, Wagner P, Dahlin LB, Atroshi I. Relationship between distal radius fracture malunion and arm-related disability: a prospective population-based cohort study with 1-year follow-up. BMC Musculoskelet Disord. 2011;12:9. doi: 10.1186/1471-2474-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung KC, Kotsis SV, Kim HM. Predictors of functional outcomes after surgical treatment of distal radius fractures. J Hand Surg Am. 2007;32:76–83. doi: 10.1016/j.jhsa.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA. Functional decline after incident wrist fractures—Study of Osteoporotic Fractures: prospective cohort study. BMJ. 2010;341:c3324. doi: 10.1136/bmj.c3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92:1851–1857. doi: 10.2106/JBJS.I.00968. [DOI] [PubMed] [Google Scholar]
- 10.Flinkkila T, Raatikainen T, Hamalainen M. AO and Frykman’s classifications of Colles’ fracture: no prognostic value in 652 patients evaluated after 5 years. Acta Orthop Scand. 1998;69:77–81. doi: 10.3109/17453679809002362. [DOI] [PubMed] [Google Scholar]
- 11.Foldhazy Z, Tornkvist H, Elmstedt E, Andersson G, Hagsten B, Ahrengart L. Long-term outcome of nonsurgically treated distal radius fractures. J Hand Surg Am. 2007;32:1374–1384. doi: 10.1016/j.jhsa.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Gliatis JD, Plessas SJ, Davis TR. Outcome of distal radial fractures in young adults. J Hand Surg Br. 2000;25:535–543. doi: 10.1054/jhsb.2000.0373. [DOI] [PubMed] [Google Scholar]
- 13.Gummesson C, Atroshi I, Ekdahl C. The Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. doi: 10.1186/1471-2474-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 15.Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84:208–215. doi: 10.2106/00004623-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Jupiter JB, Masem M. Reconstruction of post-traumatic deformity of the distal radius and ulna. Hand Clin. 1988;4:377–390. [PubMed] [Google Scholar]
- 17.Karnezis IA, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005;36:1435–1439. doi: 10.1016/j.injury.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 18.Kopylov P, Johnell O, Redlund-Johnell I, Bengner U. Fractures of the distal end of the radius in young adults: a 30-year follow-up. J Hand Surg Br. 1993;18:45–49. doi: 10.1016/0266-7681(93)90195-L. [DOI] [PubMed] [Google Scholar]
- 19.Little RJ, D’Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, Frangakis C, Hogan JW, Molenberghs G, Murphy SA, Neaton JD, Rotnitzky A, Scharfstein D, Shih WJ, Siegel JP, Stern H. The prevention and treatment of missing data in clinical trials. N Engl J Med. 2012;367:1355–1360. doi: 10.1056/NEJMsr1203730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacDermid JC, Richards RS, Donner A, Bellamy N, Roth JH. Responsiveness of the Short Form-36, Disability of the Arm, Shoulder, and Hand questionnaire, Patient-Rated Wrist Evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg Am. 2000;25:330–340. doi: 10.1053/jhsu.2000.jhsu25a0330. [DOI] [PubMed] [Google Scholar]
- 21.MacDermid JC, Roth JH, Richards RS. Pain and disability reported in the year following a distal radius fracture: a cohort study. BMC Musculoskelet Disord. 2003;4:24. doi: 10.1186/1471-2474-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988;70:649–651. doi: 10.1302/0301-620X.70B4.3403617. [DOI] [PubMed] [Google Scholar]
- 23.Nygaard M, Nielsen NS, Bojsen-Moller F. A biomechanical evaluation of the relative load change in the joints of the wrist with ulnar shortening: a “handbag” model. J Hand Surg Eur Vol. 2009;34:724–729. doi: 10.1177/1753193409337965. [DOI] [PubMed] [Google Scholar]
- 24.Scheer JH, Adolfsson LE. Radioulnar laxity and clinical outcome do not correlate after a distal radius fracture. J Hand Surg Eur Vol. 2011;36:503–508. doi: 10.1177/1753193411403690. [DOI] [PubMed] [Google Scholar]
- 25.Souer JS, Lozano-Calderon SA, Ring D. Predictors of wrist function and health status after operative treatment of fractures of the distal radius. J Hand Surg Am. 2008;33:157–163. doi: 10.1016/j.jhsa.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Taleisnik J, Watson HK. Midcarpal instability caused by malunited fractures of the distal radius. J Hand Surg Am. 1984;9:350–357. doi: 10.1016/s0363-5023(84)80222-1. [DOI] [PubMed] [Google Scholar]
- 27.Villar RN, Marsh D, Rushton N, Greatorex RA. Three years after Colles’ fracture: a prospective review. J Bone Joint Surg Br. 1987;69:635–638. doi: 10.1302/0301-620X.69B4.3611172. [DOI] [PubMed] [Google Scholar]
- 28.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25:19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]