Abstract
Background
Coronal alignment is considered key to the function and longevity of a TKA. However, most studies do not consider femoral and tibial anatomical features such as lateral femoral bowing and the effects of these features and subsequent alignment on function after TKA are unclear.
Questions/purposes
We therefore determined (1) the prevalence of lateral femoral bowing, varus femoral condylar orientation, and severe tibia plateau inclination in female Koreans undergoing TKA; (2) whether postoperative alignments are affected by these anatomical features and improved by the use of navigation; and (3) whether postoperative coronal alignments are associated with function.
Methods
We measured alignment in 367 knees that underwent TKA and 60 sex- and age-matched normal knees (control group). We determined patterns and degrees of femoral bowing angle, femoral condylar orientation, and tibial plateau inclination on preoperative full-limb radiographs. Postoperatively, coronal alignment of limbs and of femoral and tibial components was measured. We compared American Knee Society scores, WOMAC scores, and SF-36 scores in aligned knees and outliers (beyond ± 3° or ± 2°) at 1 year.
Results
The prevalence of lateral femoral bowing was 88% in the TKA group and 77% in the control group. Mean femoral condylar orientation angle was varus 2.6° in the TKA group and valgus 1.1° in the control group, and mean tibial plateau inclination was varus 8.3° in the TKA group and varus 5.4° in the control group. Femoral lateral bowing and varus femoral condylar orientation were associated with postoperative alignments. Several clinical outcome scales were inferior in the outliers in mechanical tibiofemoral angle, anatomical tibiofemoral angle, and tibial coronal alignment but not in femoral coronal alignment outliers.
Conclusions
Lateral femoral bowing, varus condylar orientation, and severe varus inclination of the tibia plateau should be considered when performing TKA in Korean patients or patients with otherwise similar anatomical features.
Introduction
When performing TKA, restoring proper coronal alignment is arguably regarded as a key surgical tenet in terms of restoring function and achieving a durable implant [2, 20, 21, 33, 37]. Consequently, the goal of postoperative coronal alignment in TKA is to restore mechanical limb alignment to neutral by aligning both the femoral and tibial components perpendicular to the mechanical axes of the femur and tibia, respectively [20]. In a normal femur, the femoral shaft has no bowing and a 3° valgus orientation of the femoral condylar surface with respect to the femoral mechanical axis, whereas the proximal tibial articular surface is at a corresponding 3° of varus with reference to the tibial mechanical axis [11, 20, 26]. This 3° of varus inclination of the tibial plateau and approximately the same degree of valgus orientation of the distal femoral condyle have been viewed as basic in past anatomical studies [11, 26] and as the norm to achieve proper coronal alignment using most TKA instrumentation systems. However, several authors have reported considerable variations in normal alignment between ethnicities [16, 29, 30, 36, 40]. Furthermore, several Asian studies have found femoral lateral bowing and obliquity of the proximal tibial joint surface in knees with advanced osteoarthritis can present with more severe varus inclination (> 3°) [16, 29, 30, 36, 40]. In addition, we have observed the femora in these patients frequently have lateral bowing of the shaft and varus orientation at the condyles and the tibiae exhibit a much larger varus inclination at the plateaus in Koreans. In theory, the presence of lateral bowing of the femoral shaft may result in varus orientation of the femoral component unless special attention is paid during the implantation of an intramedullary guiding system [20, 31, 40]. A knee with severe varus inclination of the tibia plateau requires modification of surgical techniques such as more aggressive medial release or greater external rotation of the femoral component to create rectangular gaps [20]. Furthermore, it is conceivable the presence of these anatomical features is associated with the occurrence of outliers in the coronal alignment and that knees with such outliers have inferior function and durability to properly aligned knees [9, 10, 20, 21, 33].
We therefore determined (1) the prevalence of lateral femoral bowing, varus femoral condylar orientation, and severe tibia plateau inclination in female Koreans undergoing TKA; (2) whether postoperative alignments were affected by these anatomical features and improved by the use of navigation; and (3) whether postoperative coronal alignments are associated with functional outcomes.
Patients and Methods
We retrospectively reviewed all 367 female patients who had undergone unilateral TKA for advanced osteoarthritis using a standard instrumentation system (Genesis II; Smith & Nephew, Memphis, TN, USA) or an image-free navigation system (Orthopilot; B. Braun-Aesculap, Tuttlingen, Germany) from March 2004 to April 2010. We excluded 36 patients (8.9% of 403 eligible patients treated during the study period) for: (1) a history of femoral or tibial fracture or osteotomy around the knee; (2) the presence of a congenital anomaly in the femur or tibia; (3) a history of prior knee or hip arthroplasty; (4) a diagnosis other than primary osteoarthritis; and (5) a position in radiographs preventing complete evaluation of radiographic variables or the absence of radiographs after TKA resulting from followup loss. Sixty sex- and aged-matched patients who visited our knee clinic as a result of knee symptoms but with no radiographic findings for osteoarthritis (Kellgren-Lawrence Grade 0 or 1 [15]) were assigned to the control group. Mean age in the TKA group was 69.0 years (range, 50–88 years) and in the control group was 65.9 years (range, 50–85 years). The mean height, weight, and body mass index in the TKA group were 151.7 cm (range, 131–167 cm), 61.0 kg (range, 38–97 kg), and 26.4 kg/m2 (range, 18.9–39.1 kg/m2), respectively. No patients were lost to followup. All patients were followed and followup data reported at 1 year. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. This study was approved by our institutional review board.
To determine whether our sample size was sufficient, we performed a priori power analysis using the two-sided hypothesis test at an alpha level of 0.05. Sixty-four knees were required to detect a 5° difference in motion arc and a 5% difference in outcome scales. We considered these cutoff values to be clinically important because motion arc was measured to the nearest 5° and a 6% difference of maximum score has been suggested as the minimal clinically important difference for WOMAC and SF-36 [1]. Thus, the sample sizes used were regarded as adequate.
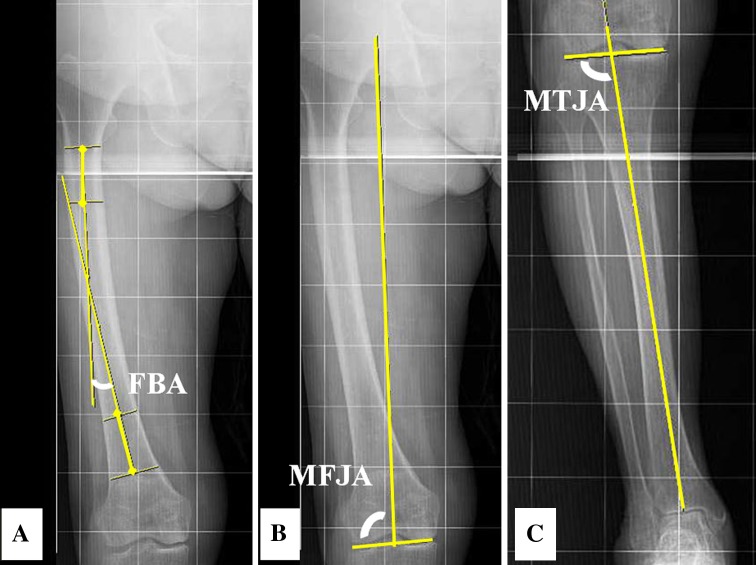
Preoperatively a standing whole-limb AP radiograph was used to measure three parameters, namely, femoral bowing angle, femoral condylar orientation, and tibial plateau inclination (Fig. 1). Femoral bowing angle was defined as the angle between the line connecting the points bisecting the femur at 0 and 5 cm below the lowest portion of the lesser trochanter and the line connecting the points bisecting the femur at 5 cm and 10 cm above the lowest portion of the lateral femoral condyle (Fig. 1A). Negative and positive femoral bowing angle values indicate lateral and medial bowing, respectively. To calculate femoral condylar orientation, we measured the mechanical femoral joint angle (defined as the lateral angle between the femoral mechanical axis, a line connecting the hip center and the top point of the intercondylar notch of the femur, and the bisecting midline of the tibiofemoral joint; Fig. 1B). Femoral condylar orientation values were calculated by subtracting mechanical femoral joint angle from 90°, and thus, a negative femoral condylar orientation value indicates varus orientation of the femoral condyles. To calculate tibial plateau inclination, we measured mechanical tibial joint angle (defined as the lateral angle between the tibial mechanical axis, the line connecting the midpoint of the medial and lateral tibial eminences and the midpoint of the talus dome, and the bisecting midline of the tibiofemoral joint; Fig. 1C). Tibial plateau inclination values were calculated by subtracting mechanical tibial joint angle values from 90°, and thus, negative values indicate varus inclination of the tibia plateau.
Fig. 1A–C.
Radiographs showing the three radiographic measurements: femoral bowing angle (A), femoral condylar orientation (B), and tibial plateau inclination (C). FBA = femoral bowing angle; MFJA = mechanical femur joint angle; MTJA = mechanical tibial joint angle.
All surgeries were performed by a single surgeon (TKK) using a standard medial parapatellar approach; all patients underwent a similar rehabilitation protocol after surgery. Decisions regarding surgical modality (the standard instrument system or the navigation system) were made by the operating surgeon based on considerations for multiple factors including surgery schedule, but generally, knees were randomly assigned. A fixed-bearing posterior-stabilized prosthesis (Genesis II; Smith & Nephew) was implanted when the standard instrumentation system was used and a mobile-bearing posterior-stabilized system (e.motion-RP/PS; B. Braun-Aesculap) when the navigation system was used. In addition, when the standard instrumentation system was used, an intramedullary guide was used for the femur and an extramedullary guide for the tibia. To achieve a distal femoral bone cut perpendicular to the mechanical axis of the femur, the angle of the distal femoral cutting block was set at the measured angle between the femoral mechanical axis and the femoral anatomical axis. Navigated procedures were performed as recommended by the manufacturer [18]. Briefly, after tracking devices were placed, kinematic and anatomical registrations were performed, and the accuracy of registration was confirmed using preoperative radiographic measurements [7]. Bone resections started with the tibia; neutral coronal alignment and a posterior slope of 0° to 1° were targeted, and the level of bone resection was aimed for 9 to 10 mm at the intact plateau, typically the lateral tibial plateau. The accuracy of bone resection of the proximal tibia was checked using the navigation system. Extension and flexion gaps were assessed, and gap balancing was carried out in accordance with initial gap assessments. Gap assessments were repeated after gap balancing, and femoral resections were planned with consideration of gaps and alignments. Typically, neutral overall limb alignment defined as mechanical tibiofemoral angle of 0° was targeted. If the medial side of an extension gap was too tight but with a well-balanced flexion gap, distal femoral resection was targeting 1° or 2° of varus to help create a balanced extension gap. The patella was resurfaced in all knees, and all prostheses were fixed with cement. Patients were encouraged to start knee motion with quadriceps-strengthening exercises on the day after surgery. Ambulation with a walking aid was initiated on the second postoperative day. Typically, patients were discharged to home or to a rehabilitation center 7 days after surgery.
All clinical information was prospectively collected using predesigned data sheets and maintained in a database by an independent investigator (YGK). The clinical information included demographic data, preoperative clinical statuses, and postoperative outcomes evaluated at 6 and 12 months postoperatively and annually thereafter. Preoperative clinical statuses and postoperative outcomes were evaluated using knee ROM, American Knee Society knee and function scores [13], WOMAC scales [3], and SF-36 scores [39]. ROM was calculated by subtracting flexion contracture from maximum flexion. An independent investigator (YGK) measured flexion contracture and maximum flexion to the nearest 5° using a standard (38 cm) clinical goniometer with patients positioned supine.
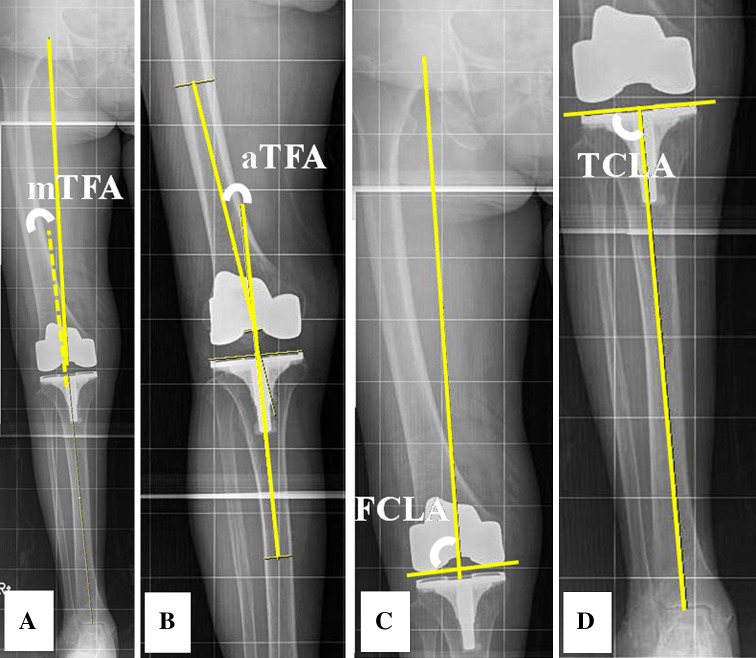
Postoperatively, a standing whole-limb AP radiograph taken at 6 or 12 months after surgery was used to measure four parameters, namely, mechanical tibiofemoral angle, anatomical tibiofemoral angle, coronal femoral prosthesis alignment, and coronal tibial prosthesis alignment (Fig. 2). Two of us (KJL, YGK) made all radiographic measurements using full-length weightbearing AP leg radiographs, which included the hip, knee, and ankle. To achieve the same foot rotation angle, a reference template was positioned on the platform of our plane radiographic system. All radiographic images were digitally acquired using a picture archiving and communication system (PACS) (Infinitt, Seoul, Korea). Assessments were performed on a 20-inch LCD monitor (PCBANK) in portrait mode using PACS software. The software package allowed the investigator to detect the bisecting point of any region on the femur or tibia and to measure angles between any two lines drawn on the digital image. The minimum detectable angular change was 1°. As a surrogate of overall limb alignment, we measured mechanical tibiofemoral angle of the knee, which was defined as the angle formed by the intersection between the mechanical axes of the femur (the line from the femoral head center to the femoral intercondylar notch center) and the tibia (the line from the ankle talus center to the center of tibial spine tips) (Fig. 2A). A negative value was given to knees in varus alignment. Another surrogate of overall limb alignment, anatomical tibiofemoral angle, was defined as the angle between the anatomical axes of the femur (the line from a point on the bisector of the femur, 15 cm proximal to the lowest point of lateral femoral condyle, to the center of the femoral intercondylar notch) and the tibia (the line from the midpoint between the medial and lateral tibial eminences to a point on the bisector of the tibia, 15 cm distal to the highest point of lateral tibial plateau) (Fig. 2B). A knee with an anatomical tibiofemoral angle ranging from 5° to 9° was considered aligned. To assess coronal alignment of the femoral component, we measured the femoral component lateral angle defined as the lateral angle between the femoral mechanical axis and a line connecting the most distal points of the medial and lateral condyles of the femoral component. Coronal femoral prosthesis alignment was calculated by subtracting the femoral component lateral angle from 90°, and thus, a negative value was given to varus orientation of the femoral component (Fig. 2C). To assess coronal alignment of the tibial component, we measured the tibial component lateral angle, defined as the lateral angle between the tibial mechanical axis and the line parallel to the top surface of the tibial component (Fig. 2D). We calculated coronal tibial prosthesis alignment by subtracting the tibial component lateral angle from 90°, and thus, a negative value was given to varus orientation of the tibial component.
Fig. 2A–D.
Radiographs showing postoperative radiographic measurements: (A) mechanical tibiofemoral angle, (B) anatomical femoral angle, (C) coronal femoral prosthesis alignment, and (D) coronal tibial prosthesis alignment. mTFA = mechanical tibiofemoral angle; aTFA = anatomical TFA; FCLA = femoral condylar lateral angle; TCLA = tibial component lateral angle.
To determine the intra- and interobserver reliabilities of radiographic assessments, the two investigators performed all radiographic assessments in 20 randomly selected radiographs twice with an interval of 1 week. The intra- and interobserver reliabilities of assessments of all radiographic measurements were evaluated using intraclass correlation coefficients (ICCs). The ICCs of the intra- and interobserver reliabilities of all measurements were > 0.88 (range, 0.88–0.96). Because the measurements were judged reliable, measurements taken by a single investigator (KJL) were used in the analyses.
To document the coronal radiographic features of femurs and tibiae, data were summarized as means and SDs and as ranges for femoral bowing angle, femoral condylar orientation, and tibial plateau inclination. In addition, the proportions of knees of different severities as defined using several relevant cutoff values such as mild, moderate, severe, or very severe for tibial plateau inclination were calculated. The differences between the TKA and control groups were determined using the Student’s t-test for means and using the chi square test or the Fisher’s exact test for proportions. To determine whether postoperative alignments were affected by these anatomical features and improved by the use of navigation, partial correlation analyses between anatomical features and postoperative alignment parameters and comparisons of means and of the frequencies of outliers in subgroups of different anatomical severities were performed. These analyses were performed separately in 185 knees for which the standard instruments were used in TKA (the standard instrumentation group) and 182 knees for which the navigation system was used (the navigated group). Outliers were defined as knees with a mechanical tibiofemoral angle > ± 3°, knees with a coronal femoral prosthesis alignment > ± 3°, or knees with a coronal tibial prosthesis alignment > ± 3°. In partial correlation analyses of the three anatomical features, namely, femoral bowing angle, femoral condylar orientation, or tibial plateau inclination, the other two factors were entered as confounders to control for their effects on postoperative alignment. To determine whether postoperative alignments of limbs and prostheses affected functional outcomes, the functional outcomes at 1 year postoperatively were compared between aligned knees and outliers using the analysis of covariance. The cutoff values for outliers were > ± 3° for mechanical tibiofemoral angle, beyond the 5° to 9° range for anatomical tibiofemoral angle, and > ± 2° for coronal femoral prosthesis alignment and coronal tibial prosthesis alignment. This cutoff value was chosen for coronal femoral prosthesis alignment and coronal tibial prosthesis alignment because the cutoff value of > ± 3° did not provide sufficient numbers for comparison. Because postoperative functional outcomes could be influenced by other multiple factors, when determining the differences between the two groups using analysis of covariance, age, body mass index, and the corresponding preoperative scores of outcome scales were entered as covariates to control their confounding effects. All statistical analyses were carried out using SPSS for Windows (Version 15.0; SPSS, Inc, Chicago, IL, USA).
Results
We found differences between the TKA and control groups for femoral bowing angle, femoral condylar orientation, and tibial plateau inclination (Table 1). Mean femoral bowing angle in the TKA group was greater (p < 0.001) than in the control group (−5.4° versus −3.0°). The proportion of knees with severe or very severe lateral bowing was higher (p = 0.010) in the TKA group (42% versus 22%). Varus femoral condylar orientation was common (80%) in the TKA group, whereas the majority (78%) in the control group had valgus femoral condylar orientation. Mean femoral condylar orientation differed (p < 0.001) in the two groups: varus of 2.6° in the TKA group and valgus of 1.1° in the control group. Mean tibial plateau inclination was greater (p < 0.001) in the TKA group (−8.3° versus −5.4°), and the proportion of knees with severe varus inclination was higher (p < 0.001) in the TKA group (77% versus 50%).
Table 1.
Comparisons of femoral bowing angles, femoral condylar orientations, and tibial plateau inclinations in the TKA and control groups
| Variables | TKA (n = 367) |
Control (n = 60) |
p values |
|---|---|---|---|
| Femoral bowing angle | |||
| Mean (SD) | −5.4° (4.8°) | −3.0° (4.0°) | < 0.001 |
| Range | −23°–6° | −16°–4° | |
| Grade* | 0.010 | ||
| Medial or no bowing (FBA ≥ 0°) | 44 (12.0) | 14 (23.3) | |
| Mild lateral (−5° ≤ FBA < 0°) | 168 (45.8) | 33 (55.0) | |
| Severe lateral (−10° ≤ FBA < −5°) | 101 (27.5) | 9 (15.0) | |
| Very severe lateral (FBA < −10°) | 54 (14.7) | 4 (6.7) | |
| Femoral condylar orientation | |||
| Mean (SD) | −2.6° (2.8°) | 1.1° (2.2°) | < 0.001 |
| Range | −14°–7° | −4°–7° | |
| Grade* | < 0.001 | ||
| Valgus or neutral (FCO ≥ 0°) | 72 (19.6) | 47 (78.3) | |
| Mild varus (−3° ≤ FCO < 0°) | 180 (49.0) | 11 (18.3) | |
| Severe varus (FCO < −3°) | 115 (31.3) | 2 (3.3) | |
| Tibia plateau inclination | < 0.001 | ||
| Mean (SD) | −8.3° (3.6°) | −5.4° (3.1°) | |
| Range | −19°–3° | −13°–1° | |
| Grade* | < 0.001 | ||
| Valgus or neutral (TPI ≥ 0°) | 3 (0.8) | 5 (8.3) | |
| Mild varus (−3° ≤ TPI < 0°) | 30 (8.2) | 9 (15.0) | |
| Severe varus (−5° ≤ TPI < −3°) | 51 (13.9) | 16 (26.7) | |
| Very severe varus (TPI < −5°) | 283 (77.1) | 30 (50.0) |
* Data are presented as numbers of knees with percentages in parentheses; FBA = femoral bowing angle; FCO = femoral condylar orientation; TPI = tibial plateau inclination.
Femoral lateral bowing and varus orientation of femoral condyles were associated with postoperative limb and femoral component alignments, whereas navigation reduced outliers. In the standard instrumentation group, femoral bowing angle and femoral condylar orientation correlated with mechanical tibiofemoral angle (correlation coefficient [CC] = 0.20 and 0.26, respectively) and coronal femoral prosthesis alignment (CC = 0.19 and 0.35, respectively), suggesting lateral femoral bowing angle or varus femoral condylar orientation was associated with varus alignment of limb and femoral component (Table 2). However, in the navigation group, we found weak correlations (CC, 0.15–0.20) between femoral condylar orientation and tibial plateau inclination or between mechanical tibiofemoral angle and coronal femoral prosthesis alignment, indicating the effects of anatomical features on postoperative limb and component alignment were smaller in the navigated group. Comparisons between subgroups of anatomical feature severities showed that in the standard instrumentation group, more severe femoral lateral bowing and varus femoral condylar orientation were associated with greater varus orientation in the limb and femoral component than knees with less severe lateral bowing or varus condylar orientation (Table 3). The mean mechanical tibiofemoral angle and coronal femoral prosthesis alignment were lowest (ie, most severe varus alignment) (p < 0.001) in the knees with very severe lateral bowing and in the knees with severe varus condylar orientation. However, in the navigation group, these patterns were not observed, and mean mechanical tibiofemoral angle and coronal femoral prosthesis alignment were closer to a neutral orientation than in the standard group (Table 4). In addition, comparisons of outliers showed the rate of outliers was greater in the standard group than in the navigation group (mechanical tibiofemoral angle = 25% versus 15%; p = 0.037; coronal femoral prosthesis alignment = 5.4% versus 0%; p = 0.002; and coronal tibial prosthesis alignment = 2.2% versus 0%; p = 0.123) (Table 5).
Table 2.
Partial correlation analyses between the three radiographic features and postoperative alignments of limbs and components in the standard instrumentation group of 185 knees*
| Variable | mTFA | cFPA | cTPA |
|---|---|---|---|
| Standard group | |||
| Femoral bowing angle | 0.20 (0.026) | 0.19 (0.019) | 0.10 (0.226) |
| Femoral condylar orientation | 0.26 (0.002) | 0.35 (< 0.001) | −0.03 (0.700) |
| Tibia plateau inclination | −0.02 (0.820) | −0.08 (0.358) | 0.08 (0.345) |
| Navigation group | |||
| Femoral bowing angle | 0.12 (0.117) | 0.04 (0.649) | −0.01 (0.890) |
| Femoral condylar orientation | 0.15 (0.047) | 0.16 (0.036) | −0.02 (0.774) |
| Tibia plateau inclination | 0.20 (0.008) | 0.15 (0.044) | 0.13 (0.087) |
* Data are presented as correlation coefficients with p values in parentheses; mTFA = mechanical tibiofemoral angle; cFPA = coronal femoral prosthesis alignment; cTPA = coronal tibial prosthesis alignment.
Table 3.
Comparisons of postoperative alignments in the standard instrumentation group of 185 knees stratified by anatomical feature severity*
| Grade | mTFA | cFPA | cTPA |
|---|---|---|---|
| Femoral bowing angle | < 0.001† | < 0.001† | 0.020† |
| Medial bowing (≥ 0°) (n = 24) | 1.0 (2.3) | 0.0 (2.1) | 0.2 (1.1) |
| Mild lateral bowing (−5° ≤ < 0°) (n = 85) | 0.4 (2.9) | −0.6 (1.3) | 0.4 (1.8) |
| Severe lateral bowing (−10 ° ≤ < −5°) (n = 47) | −0.5 (2.9) | −1.0 (1.6) | 0.4 (1.6) |
| Very severe lateral bowing (< −10°) (n = 29) | −2.3 (2.7) | −1.7 (1.6) | −0.6 (1.6) |
| Femoral condylar orientation | < 0.001† | < 0.001† | NS† |
| Valgus (≥ 0°) (n = 31) | 1.3 (2.8) | 0.0 (1.8) | 0.3 (1.2) |
| Mild varus (−3° ≤ < 0°) (n = 85) | 0.1 (2.9) | −0.7 (1.5) | 0.4 (1.6) |
| Severe varus (< −3°) (n = 69) | −1.2 (2.7) | −1.4 (1.5) | 0.1 (1.9) |
| Tibia plateau inclination | NS† | NS† | NS† |
| Valgus (≥ 0°) (n = 2) | 0.5 (3.5) | 1.0 (2.8) | 0.0 (0.0) |
| Mild varus (−3° ≤ < 0°) (n = 12) | 0.8 (1.2) | −0.6 (0.8) | 0.7 (1.1) |
| Severe varus (−5° ≤ < −3°) (n = 23) | −0.1 (3.4) | −1.1 (2.3) | 0.1 (1.2) |
| Very severe varus (< −5°) (n = 148) | −0.3 (3.0) | −0.8 (1.5) | 0.2 (1.8) |
* Data are given as mean angles with SDs in parentheses; †the significances of differences between subgroups were determined by analysis of variance with Bonferroni’s post hoc test. Values significantly different from the others after post hoc testing are presented in bold font; mTFA = mechanical tibiofemoral angle; cFPA = coronal femoral prosthesis alignment; cTPA = coronal tibial prosthesis alignment; NS = not significant.
Table 4.
Comparisons of postoperative alignments in the navigated group of 182 knees stratified by anatomical feature severity*
| Grade | mTFA | cFPA | cTPA |
|---|---|---|---|
| Femoral bowing angle | 0.003† | NS† | NS† |
| Medial bowing (≥ 0°) (n = 20) | −0.2 (1.9) | −0.3 (1.0) | 0.1 (1.1) |
| Mild lateral bowing (−5 ° ≤ < 0°) (n = 83) | −0.0 (2.2) | −0.3 ((1.2) | 0.3 (1.2) |
| Severe lateral bowing (−10° ≤ < −5°) (n = 54) | −0.9 (2.7) | −0.3 (1.3) | −0.3 (1.2) |
| Very severe lateral bowing (< −10°) (n = 25) | −2.0 (2.9) | −1.0 (1.2) | 0.2 (1.5) |
| Femoral condylar orientation | 0.004† | 0.004† | NS† |
| Valgus (≥ 0°) (n = 41) | −0.0 (2.4) | −0.1 (1.3) | 0.0 (1.3) |
| Mild varus (−3° ≤ < 0°) (n = 95) | −0.3 (2.3) | −0.3 (1.3) | 0.1 (1.3 |
| Severe varus (< −3°) (n = 46) | −1.7 (1.9) | −0.9 (0.9) | 0.1 (1.2) |
| Tibia plateau inclination | 0.001† | NS† | NS† |
| Valgus (≥ 0°) (n = 1) | 3.0 (NA) | 0.0 (NA) | 2.0 (NA) |
| Mild varus (−3° ≤ < 0°) (n = 18) | 1.7 (1.4) | −0.1 (1.0) | 0.1 (1.0) |
| Severe varus (−5° ≤ < −3°) (n = 28) | 0.8 (2.2) | −0.1 (1.3) | 0.3 (1.3) |
| Very severe varus (< −5°) (n = 135) | −1.0 (2.6) | −0.5 (1.2) | 0.0 (1.3) |
* Data are mean angles with SDs in parentheses; †the significances of differences between subgroups were determined by analysis of variance with Bonferroni’s post hoc test. Values significantly different from others after post hoc testing are displayed in bold font; mTFA = mechanical tibiofemoral angle; cFPA = coronal femoral prosthesis alignment; cTPA = coronal tibial prosthesis alignment; NS = not significant; NA = not applicable.
Table 5.
Comparisons of the incidences of outliers among subgroups stratified by anatomical feature severity*
| Grade | Standard (n = 185) |
Navigated (n = 182) |
||||||
|---|---|---|---|---|---|---|---|---|
| Number | mTFA | cFPA | cTPA | Number | mTFA | cFPA | cTPA | |
| Femoral bowing angle | 0.006† | 0.022† | NS† | 0.007† | NA | NA | ||
| Medial bowing (≥ 0°) | 24 | 4 (16.7) | 2 (8.3) | 0 | 20 | 1 (5.0) | 0 | 0 |
| Mild lateral bowing (−5 ° ≤ < 0°) | 85 | 22 (25.9) | 0 | 4 (4.2) | 83 | 6 (7.2) | 0 | 0 |
| Severe lateral bowing (−10° ≤ < −5°) | 47 | 11 (23.4) | 5 (10.6) | 0/0 | 54 | 12 (22.2) | 0 | 0 |
| Very severe lateral bowing (< −10°) | 29 | 9 (31.0) | 3 (10.3) | 0 | 25 | 9 (36.0) | 0 | 0 |
| Femoral condylar orientation | 0.022† | NS† | NS† | < 0.001† | NA | NA | ||
| Valgus (≥ 0°) | 31 | 7 (22.6) | 1 (3.2) | 0 | 41 | 3 (7.3) | 0 | 0 |
| Mild varus (−3° ≤ < 0°) | 85 | 21 (24.7) | 3 (3.5) | 3 (3.5) | 95 | 13 (13.7) | 0 | 0 |
| Severe varus (< −3°) | 69 | 18 (26.5) | 6 (8.7) | 1 (1.4) | 46 | 12 (26.1) | 0 | 0 |
| Tibia plateau inclination | NS† | NS† | NS† | 0.009† | NA | NA | ||
| Valgus (≥ 0°) | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Mild varus (−3° ≤ < 0°) | 12 | 0 | 0 | 0 | 18 | 0 | 0 | 0 |
| Severe varus (−5° ≤ < −3°) | 23 | 5 (21.7) | 4 (17.4) | 1 (4.3) | 28 | 2 (7.1) | 0 | 0 |
| Very severe varus (< −5°) | 148 | 41 (27.7) | 6 (4.1) | 3 (2.0) | 135 | 26 (19.3) | 0 | 0 |
* Data are presented as numbers of knees with percentages in parentheses; †statistical significance (p value) was calculated using the chi square test or the Yates test; mTFA = mechanical tibiofemoral angle; cFPA = coronal femoral prosthesis alignment; cTPA = coronal tibial prosthesis alignment; NA = not applicable; NS = not significant.
The outliers had worse scores in a few outcome scales (Table 6). Compared with aligned knees, knees with a mechanical tibiofemoral angle of > ± 3° had a poorer American Knee Society knee score (87.2 versus 81.1, p = 0.049) and SF-36 physical component summary score (41.9 versus 39.1, p = 0.035). Knees beyond the range of 5° to 9° valgus had a poorer WOMAC pain score (4.1 versus 3.2, p = 0.040), WOMAC function score (20.1 versus 16.8, p = 0.018), and SF-36 physical component summary score (38.9 versus 43.2, p = 0.001) than the knees within this range. We observed no difference (p > 0.05) between aligned knees and outliers in coronal femoral prosthesis alignment in terms of any functional outcome scale. Outliers in coronal tibial prosthesis alignment had lower (p = 0.007) mean SF-36 physical component summary score than aligned knees (36.6 versus 41.8).
Table 6.
Comparisons of functional outcomes after stratification by postoperative limb and prosthesis alignments
| Variable | Aligned | Outlier* | p value |
|---|---|---|---|
| Mechanical TFA | N = 292 (79.5%) | N = 75 (20.5%) | |
| ROM | 129.0 (13.0) | 128.6 (13.8) | 0.824 |
| AKS knee | 87.2 (17.3) | 81.1 (20.0) | 0.049 |
| Function | 86.2 (20.1) | 79.9 (25.3) | 0.088 |
| WOMAC pain | 3.5 (3.1) | 3.6 (3.4) | 0.814 |
| Stiffness | 2.1 (1.5) | 2.4 (1.7) | 0.224 |
| Function | 18.4 (9.8) | 18.1 (11.0) | 0.824 |
| SF-36 PCS | 41.9 (7.9) | 39.1 (9.7) | 0.035 |
| MCS | 45.5 (12.0) | 47.0 (10.2) | 0.416 |
| Anatomical TFA | N = 241 (65.6%) | N = 126 (34.4%) | |
| ROM | 128.2 (13.7) | 129.9 (12.6) | 0.354 |
| AKS knee | 85.1 (19.3) | 83.3 (18.4) | 0.496 |
| Function | 83.9 (22.5) | 83.0 (22.1) | 0.780 |
| WOMAC pain | 3.2 (2.7) | 4.1 (3.8) | 0.040 |
| Stiffness | 2.1 (1.4) | 2.4 (1.7) | 0.094 |
| Function | 16.8 (9.2) | 20.1 (11.1) | 0.018 |
| SF-36 PCS | 43.2 (7.6) | 38.9 (9.4) | 0.001 |
| MCS | 46.2 (12.4) | 44.9 (10.2) | 0.405 |
| Coronal femoral alignment | N = 319 (86.9%) | N = 48 (13.1%) | |
| ROM | 129.2 (13.1) | 126.2 (14.0) | 0.256 |
| AKS knee | 85.4 (18.4) | 90.9 (13.6) | 0.072 |
| Function | 84.4 (21.5) | 89.4 (20.1) | 0.248 |
| WOMAC pain | 3.5 (3.2) | 3.7 (2.8) | 0.78 |
| Stiffness | 2.2 (1.5) | 2.2 (1.6) | 0.918 |
| Function | 18.1 (9.8) | 19.8 (12.3) | 0.422 |
| SF-36 PCS | 41.7 (8.3) | 39.0 (7.4) | 0.173 |
| MCS | 45.7 (11.7) | 48.2 (12.1) | 0.378 |
| Coronal tibial alignment | N = 338 (92.1%) | N = 29 (7.9%) | |
| ROM | 128.6 (13.2) | 132.2 (12.1) | 0.210 |
| AKS knee | 85.7 (18.3) | 91.1 (11.6) | 0.057 |
| Function | 84.7 (21.7) | 89.3 (16.6) | 0.345 |
| WOMAC pain | 3.5 (3.1) | 4.1 (3.4) | 0.335 |
| Stiffness | 2.2 (1.5) | 1.8 (1.8) | 0.266 |
| Function | 18.1 (9.7) | 21.2 (13.4) | 0.166 |
| SF-36 PCS | 41.8 (8.0) | 36.6 (9.4) | 0.007 |
| MCS | 45.4 (11.8) | 49.7 (9.8) | 0.126 |
* Outliers were defined as the knees with an mTFA of > 3° or < −3° for mechanical TFA, aTFA > 9° or < 5° for anatomical TFA, cFPA > 2° or < −2° for coronal femoral alignment, and cTPA > 2° or < −2° for coronal tibial alignment; TFA = tibiofemoral angle; AKS = American Knee Society; PCS = physical component summary; MCS = mental component summary; mTFA = mechanical tibiofemoral angle; aTFA = anatomical tibiofemoral angle; cFPA = coronal femoral prosthetic alignment; cTPA = coronal tibial prosthetic alignment.
Discussion
The achievement of proper limb and prosthetic alignment and well-balanced gaps are the surgical principles that underlie the success of TKA [20]. Coronal radiographic features of the femur may have considerable implications to the application of these surgical principles in individual patients. We have observed many patients present with severe lateral bowing of the femur, varus condylar orientation, and large varus inclination of the tibial plateau, which often require modification of surgical techniques. We therefore determined the prevalence of lateral femoral bowing, varus femoral condylar orientation, and severe tibia plateau inclination in female Koreans undergoing TKA and the effects of these anatomical features on alignment and the effects of postoperative alignments on function.
Several limitations should be noted before interpreting our findings. First, as a result of the extreme female sex predominance in Koreans undergoing TKA [6, 17], the number of male patients treated during the study period was insufficient to provide the statistical power required to detect sex effects on outcomes. Therefore, we decided to exclude male subjects. However, considering the universally observed female dominance in TKA series [8, 19], we believe our findings have surgical implications for patients in many other regions. Second, we used only one conventional instrumentation system (Genesis II) and only one navigation system (Orthopilot), and different systems of standard instrument or navigation may produce different findings. Third, we used standing whole-limb AP radiographs for radiographic measurements, and although this radiographic view is known to have satisfactory accuracy and reliability [5, 35] and have been frequently used in previous studies with similar purposes [11, 26, 29, 30, 36, 40], it may be affected by several factors such as degree of rotation. To maintain the quality of radiographic images, we used a specially designed template to control rotation. Furthermore, patients with less than good images were excluded. Finally, the clinical value of navigation technology for TKA and whether outliers in the coronal plane are in fact associated with compromised longevity are topics of debate [4, 9, 14, 21, 27, 32, 33], but we convey no information regarding the longevity of prostheses.
We found femoral lateral bowing, varus femoral condylar orientation, and large varus tibia plateau inclination are common in female Koreans undergoing TKA. However, it is not feasible to compare our findings directly with those of previous studies because of differences in age and sex compositions of populations studied, the types of parameters measured, and the types of variables reported [11, 16, 26, 29, 30, 36, 38, 40]. Nonetheless, it appears that like the Korean female patients in this study, Asian (Chinese, Indian, and Japanese) patients undergoing TKA for medial osteoarthritis commonly exhibit lateral femoral bowing and varus condylar orientation and a larger tibial plateau inclination than healthy Western subjects (Table 7) [11, 26, 29, 30, 36, 40]. A high prevalence of lateral femoral bowing has been reported in China [40], India [29], and Japan [30], and a varus femoral condylar orientation tendency has been reported in India [29]. Furthermore, a large tibia plateau inclination of > 3° was reported in a study of Japanese patients with knee medial osteoarthritis [30] and in a study of young healthy Chinese subjects [36]. A lack of relevant information regarding coronal alignments in Western or other Asian countries prevents us from concluding that these anatomical features are unique in Asia. Future studies in other countries and in other ethnic groups are warranted to clarify this issue, which potentially has important surgical implications.
Table 7.
Summary of studies that have reported coronal radiographic features
| Study (year) | Country | Study subjects | Femoral bowing angle | Femoral condylar orientation | Tibia plateau inclination |
|---|---|---|---|---|---|
| Moreland et al.* (1987) [26] | USA | Normal male volunteers | Not measured | Not measured | Right: −3.0°; left: −2.6° |
| Hsu et al.* (1990) [11] | USA | Normal volunteers 120 | Not measured | Not measured | Female: −0.1°; male: −1.0° |
| Tang et al.* (2000) [36] | China (Hong Kong) | Normal young volunteers: male 25 limbs (age, 24 years; age range, 22–31 years) versus female 25 limbs (age, 23 years; age range, 21–29 years) | Not measured | Not measured | Female: −5.4° (2.5); male: −4.9° (2.3) |
| Khattak et al.* (2010) [16] | Pakistan | Normal young volunteers (age, 20–45 years): male 40 versus female 19 | Not measured | Not measured | Female: −1.4° (3.2); male: −3.4° (2.2) |
| Nagamine et al.† (2000) [30] | Japan | Patients undergoing HTO or TKA 133 (age, 69.9 years; age range, 50–89 years) | −2.2° (2.9) | Not measured | −7.2° (3.8) |
| Yau et al.‡ (2007) [40] | China (Hong Kong) | 93 limbs from 10 males and 43 females undergoing TKA for primary OA (age, 67 years; age range, 45–81 years) | −1.6° (4.4); lateral bowing: 82% | Not measured | Not measured |
| Mullaji et al.§ (2009) [29] | India | Patients undergoing UKA or TKA for medial OA 250 limbs (female = 167, male = 83; age, 67 years; age range, 49–85 years) versus young control limbs, 50 limbs in 25 males (age, 32 years; age range, 21–39 years) | −3.6° in patients with OA versus −0.4° in control subjects | −0.1° in patients with OA versus 3.1° in control subjects | Not measured |
| Current study | Korea | Female Koreans undergoing TKA for advanced osteoarthritis 367 (age, 69 years; age range 50–89 years) versus female control subjects with no osteoarthritis (age, 66 years; age range, 50–85 years) | −5.4° in patients undergoing TKA versus −3.0° in control subjects; lateral bowing: 88.0% in patients undergoing TKA versus 76.7% in control subjects | −2.6° in patients undergoing TKA versus 1.1° in control subjects; varus orientation: 80.4% in patients undergoing TKA versus 21.7% in control subjects | −8.3° in patients undergoing TKA versus −5.4° in control subjects; severe varus (> 3°): 91.0% in patients undergoing TKA versus 76.7% in control subjects |
* Tibial plateau inclination was defined as the angle between the mechanical axis of the tibia and the joint line of the knee; †femoral bowing angle was defined as the angle between the proximal and distal diaphyseal lines, and tibial plateau inclination was defined as the angle between the midmedullary line of the proximal tibia and the tangent to the medial and lateral tibial plateaus; ‡femoral bowing angle was defined as the angle between the diaphyseal lines of the most proximal and distal segments of the four segments spanning the femoral shaft; §femoral bowing angle was defined as the angle between a line connecting a point on the line bisecting the lower margin of lesser trochanter and a point on the line bisecting the middle of the femur, and a line connecting a point bisecting the femur 10 cm proximally to the knee and a point bisecting the middle of the femur, and the femoral condylar angle was defined as the angle between the mechanical axis of the femur and the subchondral bone of femoral condyles; HTO = heterotopic ossification; OA = osteoarthritis; UKA = unicompartmental knee arthroplasty.
The findings in partial correlation analyses and subgroup comparisons partly support our hypothesis that femoral lateral bowing, femoral condylar orientation, and tibia plateau inclination are associated with postoperative limb and prosthesis alignment and that the use of navigation reduces postoperative alignment outliers. Nevertheless, our findings are intuitively understandable. It is well known that the accuracy of femoral bone resection using an intramedullary guiding system can be compromised by femoral anatomical variations and that this could result in incomplete intramedullary rod insertion and subsequently erroneous distal femur resection [25, 31, 40]. Previous Western [11] and Asian [13, 27] authors have also reported that knees with a varus deformity are subject to postoperative varus malalignment. One technical tip that the senior author (TKK) has used is to assure that the cutting block for distal femur resection makes contact with bone as anticipated based on an assessment of femoral condylar orientation. For example, if the femur has a varus femoral condylar orientation, the distal cutting block has to make contact only with the lateral femoral condyle to achieve neutral bone resection. On the other hand, few knees had tibia alignment outliers even when standard instruments were used. This finding is also intuitive because surgeons would be able to place the cutting block independently of the anatomy whether a standard extramedullary guiding system or a navigation system is used.
Numerous studies have documented the use of navigation improves alignment [12, 22, 24, 28, 34, 37], but relatively few previous studies have addressed the issue of navigation in the context of the alignment of knees with severe deformity [12, 22, 24, 28, 34, 37]. Our findings are generally in accord with two previous studies, which found that the use of navigation reduces outliers in knees with severe deformity [12, 22, 24, 28, 34, 37]. Furthermore, in the present study, the navigation group also had no outliers in femoral or tibial component alignment. However, interestingly, although the overall incidence of mechanical tibiofemoral angle outliers was lower in the navigation group (15.4% versus 24.9%), it was not lower in knees with severe deformity (Table 5). It is unclear why or how the incidences of outliers remained high even in the absence of component alignment outliers, although the limited nature of radiographic alignment assessments provides one possible explanation.
Our subgroup comparisons of the functional outcomes of aligned knees and outliers may provide some clues to resolving recent debate as to whether the restoration of neutral limb alignment is associated with better functional outcome [4, 23, 32]. Several authors have recently challenged the importance of the restoration of neutral limb alignment [4, 23, 32]. A previous study that compared aligned and varus-malaligned knees found no differences between the two in terms of American Knee Society, WOMAC, or SF-36 scores [23]. In contrast, in our study, the mechanical tibiofemoral angle outlier had a lower American Knee Society knee score and SF-36 physical component summary score, and coronal tibial prosthesis alignment outlier had a low SF-36 physical component summary score. However, we found no differences in other functional scales. These findings suggest postoperative coronal alignment influences patient function but only to a limited extent, particularly given some of the many comparisons might have been significant by chance. However, coronal femoral prosthesis alignment outliers were not different in any functional scale. This suggests surgeons can be flexible to some extent when determining coronal component orientation to achieve a rectangular extension gap without adversely affecting functional outcomes.
In summary, our data document femoral lateral bowing, varus condylar orientation of the femur, and severe varus inclination of the tibial plateau are prevalent in female Koreans undergoing TKA and that the presence of these anatomic features can adversely affect postoperative limb and prosthesis alignments. Thus, these features should be considered during TKA to reduce the risks of adversely affecting postoperative limb and prosthesis alignments.
Acknowledgments
We thank Moon Jong Chang, MD (Department of Orthopaedic Surgery, Seoul National University Bundang Hospital), for his scientific debate and manuscript review and Sung Ju Kim, MS, PhD candidate (Department of Orthopaedic Surgery, Korea University), for his help with statistical analyses.
Footnotes
One or more of the authors (TKK) have received funding from the Korean Human Technology Research Foundation and a clinical research fund of Seoul National University Bundang Hospital, Bundang, Korea.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has approved the human protocol for this investigation in that all investigations were conducted in conformity with ethical principles of research and that informed consent was obtained.
This work was performed at the Joint Reconstruction Center, Seoul National University Bundang Hospital, Bundang, Korea.
References
- 1.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45:384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 2.Bathis H, Perlick L, Tingart M, Luring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682–687. doi: 10.1302/0301-620X.86B5.14927. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 4.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53. doi: 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang CB, Choi JY, Koh IJ, Seo ES, Seong SC, Kim TK. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis Cartilage. 2010;18:530–538. doi: 10.1016/j.joca.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Cho HJ, Chang CB, Kim KW, Park JH, Yoo JH, Koh IJ, Kim TK. Gender and prevalence of knee osteoarthritis types in elderly Koreans. J Arthroplasty. 2011;26:994–999. doi: 10.1016/j.arth.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Chung BJ, Dileep I, Chang CB, Kang YG, Park YB, Kim TK. Novel approach to reducing discrepancies in radiographic and navigational limb alignments in computer-assisted TKA. Orthopedics. 2010;33:62–67. doi: 10.3928/01477447-20100510-56. [DOI] [PubMed] [Google Scholar]
- 8.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006;443:266–272. doi: 10.1097/01.blo.0000188066.01833.4f. [DOI] [PubMed] [Google Scholar]
- 9.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24:39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 10.Heyse TJ, Decking R, Davis J, Boettner F, Laskin RS. Varus gonarthrosis predisposes to varus malalignment in TKA. HSS J. 2009;5:143–148. doi: 10.1007/s11420-009-9118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 12.Huang TW, Hsu WH, Peng KT, Hsu RW. Total knee replacement in patients with significant femoral bowing in the coronal plane: a comparison of conventional and computer-assisted surgery in an Asian population. J Bone Joint Surg Br. 2011;93:345–350. doi: 10.2106/JBJS.J.00325. [DOI] [PubMed] [Google Scholar]
- 13.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 14.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 15.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khattak MJ, Umer M, Davis ET, Habib M, Ahmed M. Lower-limb alignment and posterior tibial slope in Pakistanis: a radiographic study. J Orthop Surg (Hong Kong). 2010;18:22–25. doi: 10.1177/230949901001800105. [DOI] [PubMed] [Google Scholar]
- 17.Kim HA, Kim S, Seo YI, Choi HJ, Seong SC, Song YW, Hunter D, Zhang Y. The epidemiology of total knee replacement in South Korea: national registry data. Rheumatology (Oxford). 2008;47:88–91. doi: 10.1093/rheumatology/kem308. [DOI] [PubMed] [Google Scholar]
- 18.Kim TK, Chang CB, Kang YG, Chung BJ, Cho HJ, Seong SC. Execution accuracy of bone resection and implant fixation in computer assisted minimally invasive total knee arthroplasty. Knee. 2010;17:23–28. doi: 10.1016/j.knee.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 20.Lombardi AV, Jr, Nett MP, Scott WN, Clarke HD, Berend KR, O’Connor MI. Primary total knee arthroplasty. J Bone Joint Surg Am. 2009;91(Suppl 5):52–55. doi: 10.2106/JBJS.I.00403. [DOI] [PubMed] [Google Scholar]
- 21.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77–79. [PubMed] [Google Scholar]
- 22.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22:1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Matziolis G, Adam J, Perka C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg. 2010;130:1487–1491. doi: 10.1007/s00402-010-1064-9. [DOI] [PubMed] [Google Scholar]
- 24.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236–243. doi: 10.2106/JBJS.F.00386. [DOI] [PubMed] [Google Scholar]
- 25.Mihalko WM, Boyle J, Clark LD, Krackow KA. The variability of intramedullary alignment of the femoral component during total knee arthroplasty. J Arthroplasty. 2005;20:25–28. doi: 10.1016/j.arth.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 26.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 27.Morgan SS, Bonshahi A, Pradhan N, Gregory A, Gambhir A, Porter ML. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop. 2008;32:639–642. doi: 10.1007/s00264-007-0391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mullaji A, Kanna R, Marawar S, Kohli A, Sharma A. Comparison of limb and component alignment using computer-assisted navigation versus image intensifier-guided conventional total knee arthroplasty: a prospective, randomized, single-surgeon study of 467 knees. J Arthroplasty. 2007;22:953–959. doi: 10.1016/j.arth.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 29.Mullaji AB, Marawar SV, Mittal V. A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J Arthroplasty. 2009;24:861–867. doi: 10.1016/j.arth.2008.05.025. [DOI] [PubMed] [Google Scholar]
- 30.Nagamine R, Miura H, Bravo CV, Urabe K, Matsuda S, Miyanishi K, Hirata G, Iwamoto Y. Anatomic variations should be considered in total knee arthroplasty. J Orthop Sci. 2000;5:232–237. doi: 10.1007/s007760050157. [DOI] [PubMed] [Google Scholar]
- 31.Nuno-Siebrecht N, Tanzer M, Bobyn JD. Potential errors in axial alignment using intramedullary instrumentation for total knee arthroplasty. J Arthroplasty. 2000;15:228–230. doi: 10.1016/S0883-5403(00)90352-8. [DOI] [PubMed] [Google Scholar]
- 32.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 33.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 34.Rosenberger RE, Hoser C, Quirbach S, Attal R, Hennerbichler A, Fink C. Improved accuracy of component alignment with the implementation of image-free navigation in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2008;16:249–257. doi: 10.1007/s00167-007-0420-y. [DOI] [PubMed] [Google Scholar]
- 35.Skytta ET, Haapamaki V, Koivikko M, Huhtala H, Remes V. Reliability of the hip-to-ankle radiograph in determining the knee and implant alignment after total knee arthroplasty. Acta Orthop Belg. 2011;77:329–335. [PubMed] [Google Scholar]
- 36.Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am. 2000;82:1603–1608. doi: 10.2106/00004623-200011000-00014. [DOI] [PubMed] [Google Scholar]
- 37.Victor J, Hoste D. Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop Relat Res. 2004;428:131–139. doi: 10.1097/01.blo.0000147710.69612.76. [DOI] [PubMed] [Google Scholar]
- 38.Wang Y, Zeng Y, Dai K, Zhu Z, Xie L. Normal lower-extremity alignment parameters in healthy Southern Chinese adults as a guide in total knee arthroplasty. J Arthroplasty. 2010;25:563–570. doi: 10.1016/j.arth.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 39.Ware JE., Jr Sherbourne CD. The MOS 36-item Short-Form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong). 2007;15:32–36. doi: 10.1177/230949900701500108. [DOI] [PubMed] [Google Scholar]