Abstract
Background:
Mechanical thrombectomy devices are gaining popularity in large vessel occlusions where chemical thrombolysis is usually futile. MERCI, Multi-MERCI, Penumbra and SWIFT trails have elevated the status of mechanical thrombectomy from being a complementary treatment modality to mainstream stroke intervention. The aim of this study was to compare our immediate recanalization rates with available mechanical devices.
Materials and Methods:
A retrospective review from March 2009 to August 2012 was performed on patients who underwent mechanical thrombectomy for large vessel occlusion. Cases where IATPA and/or balloon angioplasty was performed without mechanical thrombectomy were excluded from the study. Recanalization rates were assessed immediately post-procedure by follow-up angiography. TICI scores were used to quantify the extent of recanalization and the residual clot burden.
Results:
Twenty two procedures were performed on 20 patients using Merci (MER):5; Penumbra (PEN):11; Solitaire-FR (SOL):6. Two patients underwent intervention using both Merci and Penumbra devices. The M:F ratio was 1.2:1. The most common vascular territory involved was the right MCA (9/20) followed by left MCA (5/20), left ICA (2/20), basilar (3/20) and vertebral arteries (1/20). The average door to needle time was 210 minutes [MER: 184.4; PEN: 249.2; SOL: 162]. Additional procedures were performed in 63.4% (14/22) of the patients [MER: 80% (4/5); PEN: 72.7% (8/11) and SOL: 33.3% (2/6)]. Vasospasm was observed in MER: 20% (1/5); PEN: 9.1% (1/11); SOL: 0% (0/6)]. Complete recanalization was achieved in 59.1% (13/22) [MER: 40% (2/5); PEN: 45.5% (5/11); SOL: 100% (6/6)]. The rate of complete recanalization was statistically significant for the Solitaire group vs. the MERCI group (P=0.0062) as well as the Penumbra group (0.0025). The average pre-procedure TICI was 0.4 [MER: 0.6; PEN: 0.3; SOL: 0.3], while the average post-procedure TICI was 2.5 [MER: 2.4; PEN: 2.3; SOL: 3.0].
Conclusions:
The study reveals a higher rate of angiographic recanalization using the Solitaire-FR device, requiring a lesser number of passes and other associated procedures as compared to MERCI and Penumbra. Thus, Stentrievers (Solitaire-FR) are advantageous in faster device delivery and quick flow restoration. However, future prospective randomized large trials are required to confirm these early results.
Keywords: Acute ischemic stroke, large vessel occlusion, mechanical thrombectomy, merci, penumbra, solitaire-FR, stroke intervention
Introduction
There has been a gradual shift in the paradigm of stroke management over the last decade. Mechanical thrombectomy has slowly evolved from being a complementary treatment to mainstream intervention in the management of acute onset ischemic stroke (AIS), especially where intra-arterial or intravenous thrombolysis is ineffective or marginally effective in large vessel occlusions, or associated with high re-occlusion rates.[1–5] The MERCI, multi-MERCI, Penumbra Pivotal trial and SWIFT studies have further strengthened the use of mechanical devices for large vessel occlusions.[6–12] Merci and Penumbra can be classified as the first generation mechanical thrombectomy devices, whereas the stentrievers like Solitaire and Trevo can be included as a second generation thrombectomy devices.
Materials and Methods
A retrospective chart review was conducted in patients who had undergone mechanical thrombectomy for AIS at a single institution. The study was conducted after approval from the IRB. The study period was from March 2009 to August 2012. Cases where IATPA and/or balloon angioplasty was performed without mechanical thrombectomy were excluded from the study. Duke stroke center guidelines for endovascular management in patients with acute ischemic stroke were followed for intervention. Non-contrast CT scan of the head and CT-Angiogram were obtained prior to every intervention to confirm the diagnosis of large vessel occlusion and to rule out intra-cranial hemorrhage. Interventional treatment was initiated within 8 hours from onset of stroke symptoms, and all procedures were performed under general anesthesia. The ‘time of symptom onset’ was defined as the acute onset of symptoms as observed by the family members or when the patient was last seen at baseline, as in wake-up or post-procedure strokes. The ‘door time’ was defined as the time when the patient showed up in the emergency room and the ‘needle time’ was the actual groin puncture time. The extent of recanalization was assessed immediately post-procedure by follow-up angiography. Post-procedure, all patients were managed in the neuro critical care unit by an experienced team of neuro-intensivists. Thrombolysis in Cerebral Infarction (TICI) scores were used to evaluate the extent of pre-procedure clot burden, the post-intervention residual clot burden and the success rate of the procedure.
Results
Between March 2009 and August 2012, 20 patients presented to Duke University hospital with stroke symptoms and had CTA evidence of large vessel occlusion, subsequently undergoing mechanical thrombectomy. A total of twenty-two thrombectomy procedures were performed on these 20 patients. Two patients underwent intervention using both MERCI and Penumbra devices. Thus, the MERCI device was used in five cases, the Penumbra device was used in 11 cases and the Solitaire-FR device was used in 6 cases.
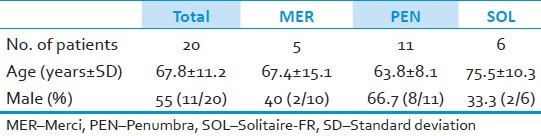
Patient demographics are presented in Table 1. Overall, the average age of the patient population was 67.8 ± 11.2 years with a male to female ratio (M:F) of 1.2:1. Several of the patients were already hospitalized with significant co-morbidities at the time of stroke symptom onset (6/20). The majority of these patients had significant cardiac history as a risk factor for embolic event (16/20), including recent cardiac surgery [valve replacement, coronary artery bypass grafting, pacer/defibrillator placement (7/20)], atrial fibrillation (6/20) and cardiomyopathy (3/20). One patient was undergoing treatment for known thrombus of a left ventricular assist device. Two patients (2/20) had history of heavy cocaine use immediately prior to presentation, one of which had a significant history of cocaine-induced MI and CVA. The other presented with ICH. Additional co-morbidities included hypertension, diabetes mellitus, end-stage renal disease and liver cirrhosis. One patient suffered from vertebral artery injury during C-spine surgery with subsequent thrombo-embolic occlusion of the basilar artery.
Table 1.
Baseline patient profile
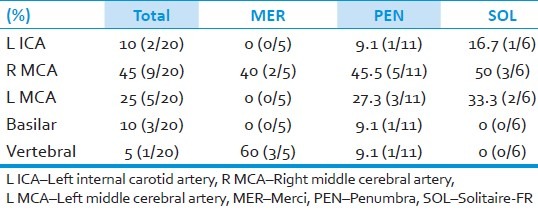
Distribution of vascular occlusion is presented in Table 2. In the case of multiple sequential occlusions (i.e., basilar and posterior cerebellar artery), the proximal vessel was used as a data point. The most common vascular territory involved was the right MCA (9/20) followed by left MCA (5/20), left ICA (2/20), basilar (3/20) and vertebral arteries (1/20).
Table 2.
Site of vascular occlusion
The average time for intervention from symptom onset was 274.6 min [MER: 379; PEN: 257.1; SOL: 218.6] [Table 3]. All the ‘groin puncture time’ was recorded within 8 hours of symptom onset with the exception of one patient who had basilar artery occlusion and a symptom onset to needle time of 12 hours. The average door to needle time was 210 min [MER: 184.4; PEN: 249.2; SOL: 162]. In cases involving inpatients, the time of symptom onset was used as the arrival time. For the patient who underwent C-spine surgery, the anesthesia induction time was used as symptom onset time as this was when he was last seen at baseline.
Table 3.
Time to treatment
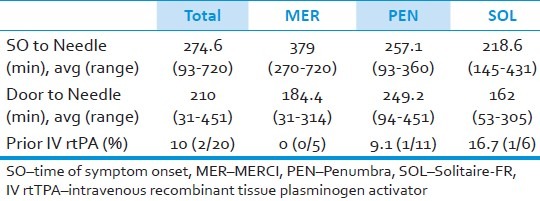
Two out of 20 patients received IV tPA prior to intervention, while the others met exclusion criteria and were directly referred for intervention. One patient received IV tPA at an outside institution prior to transfer to Duke for intervention, while the other patient had received IV tPA due to left ventricular assist device thrombus prior to onset of stroke symptoms. During intervention, additional procedures (IATPA, Balloon angioplasty, or alternate thrombectomy device) were performed in 63.4% (14/22) of the procedures [MER: 80% (4/5); PEN: 72.7% (8/11) and SOL: 33.3% (2/6)]. Pre-thrombectomy [Table 4] TICI was 0 or 1 in 18/22 cases, and 2/22 had a TICI of 2a. Post-procedure TICI [Table 4 and Figure 1] was 2b or better in 80% of patients overall, with complete recanalization achieved in 63% (14/22) [MER: 40% (2/5); PEN: 54.5% (6/11); SOL: 100% (6/6)]. The rate of complete recanalization was statistically significant for the Solitaire group vs the MERCI group (P=0.0062) as well as the Penumbra group (0.0025). The average pre-procedure TICI was 0.4 [MER: 0.6; PEN: 0.3; SOL: 0.3], while the average post-procedure TICI was 2.5 [MER: 2.4; PEN: 2.3; SOL: 3.0].
Table 4.
Recanalization results
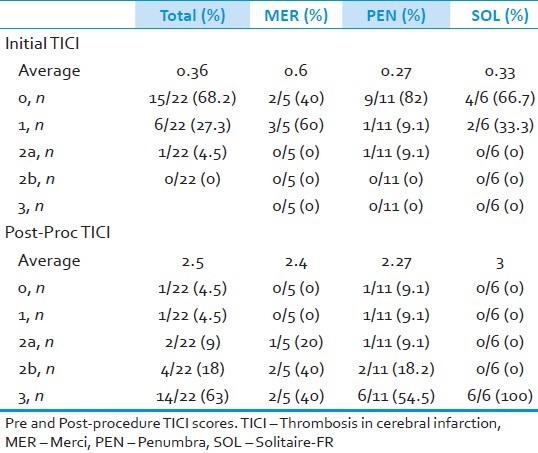
Figure 1.
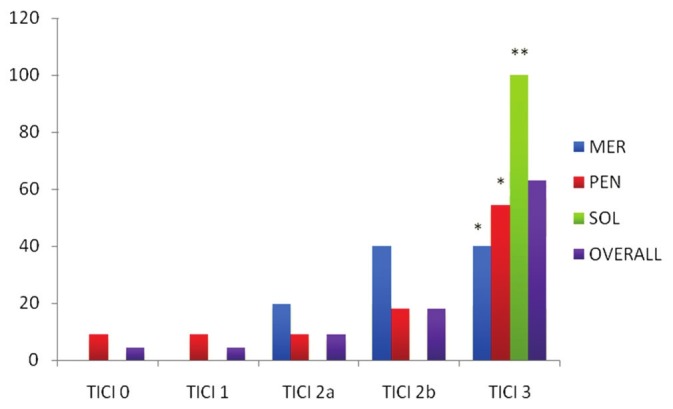
Comparison of TICI scores using various mechanical clot retrieval devices on immediate post-procedure follow-up angiography. *Statistically significant vs Solitaire-FR (P< 0.05). **Statistically significant vs Merci and Penumbra (P< 0.05)
Intra-procedural vasospasm was observed in 2 patients [MER: 20% (1/5); PEN: 9.1% (1/11); SOL: 0% (0/6)]. Post-procedure ICH was seen in 18.2% (4/22) overall [MER: 20% (1/5); PEN: 18.2% (2/11); SOL: 16.7% (1/6)]. ICH resulted in death in one of the cases involving a Penumbra device. A fractured Penumbra wire was encountered during one procedure. This was not retrievable and was subsequently left in the intracranial ICA.
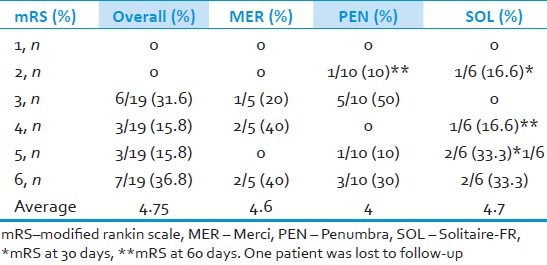
Clinical outcomes are presented in Table 5. The mRS scores were assessed at 90 days when possible, with some assessed at 30 and 60 days as noted. One patient was lost to follow-up. Overall, 31.6% (6/19) of patients had good outcomes with mRS of 3 or better [MER: 20% (1/5); PEN: 60% (6/10); SOL 16.6% (1/6). A mRS score of 4 or 5 was seen in 31.6% (6/19) of patients overall [MER: 40% (2/5); PEN: 10% (1/10); SOL: 50% (3/6).] In total, 36.8% (7/19) of the patients expired within 14 days after recanalization [MER: 40% (2/5); PEN: 30% (3/10); SOL: 2/6 (33.3%)].
Table 5.
Modified rankin scale (90d)
Discussion
The treatment of acute ischemic stroke focuses on vessel recanalization with subsequent blood flow restoration. The various methods used to achieve this goal comprise thrombolysis by intravenous plasminogen activation (IVTPA), thrombolysis by intra-arterial plasminogen activation (IATPA), mechanical clot destruction or thrombectomy (MT), and a combination of any of the aforementioned methods applying the ‘bridging’ concept. The main limitation of IVTPA is the inadequate recanalization of large vessel occlusions with some studies showing the overall recanalization rate of IVTPA to be less than 50%.[1–3,13–15] The Prolyse in acute cerebral thromboembolism (PROACT) trial[16] was an attempt to improve successful reperfusion above that achieved with IVTPA using intra-arterial thrombolysis. The success rates of localized arterial thrombolysis prompted further attempts at other mechanical ways to achieve clot removal. Multiple studies and trials are available on clot destructing and retrieving devices.
The MERCI and Multi-MERCI trials[6,7,9] focus on the Merci retriever, a corkscrew shaped device made with a flexible nitinol wire in five helical loops. This is designed for distal placement to the thrombus for en bloc removal. Multi-MERCI Part I trial established a higher rate of revascularization (69%) when treatment with the Merci retriever system was combined with IATPA than when the Merci retriever system was employed alone (54%). The Multi-MERCI Part II trial was conducted to provide proof that the system was equally safe and efficacious in patients who did or did not receive IATPA.
The Penumbra Pivotal Stroke Trial,[8] a prospective multicentric study was done to establish the safety of Penumbra Thrombus Perturbation and Aspiration system, which in contrast to the Merci retriever works proximal to the thrombus by first disrupting and then aspirating the thrombus. Since the device also employs a separator, the fear of perforation limits its use to straight arterial segments despite high vessel revascularization rates (>80%), quoted in the literature.[5,17–22]
Self-expanding stents (SES) are the next logical step in establishing revascularization once recanalization has been achieved. They have obvious advantages, the principle being immediacy of response and a high reported rate of recanalization. The SARIS[23,24] (Stent Assisted Recanalization in acute Ischemic Stroke) pilot study evaluated the performance of the Wingspan stent in patients who had no improvement or had a contradiction to IV thrombolysis. The study showed achievement of recanalization in 100% of patients. However the major disadvantages with this stent system were a high (11%) percentage of in-stent stenosis and the need for an aggressive anti-platelet therapy with resultant higher rates of hemorrhages.
The SWIFT trial (Solitaire FR with the Intention for Thrombectomy) is a randomized, blinded, multi-center trial evaluating the effectiveness of the Solitaire-FR Revascularization Device, an intracranial stent delivered by a standard microcatheter technique with the unique property of being fully retrievable. In addition, the deployment of the stent causes the clot to be pushed against the wall of the artery leading to immediate intraluminal flow restoration.[12,25,26] Major advantages of Stentrievers are navigability and quick flow restoration without the need and associate disadvantage of a permanent intracranial stent.
Some of the important factors that contribute to successful recanalization are the appropriate patient selection, age of the patient and onset of symptoms. Other factors that favor favorable outcomes are the extent and sit of large vessel occlusion and duration of neurological insult. Our results are comparable to other studies published in the literature. Figure 2 is a case illustration using Solitaire mechanical thrombectomy device. The most common vascular territory to be involved in the anterior circulation was the MCA [Right (9/20); Left (5/20)] followed by ICA, while it was the basilar artery followed by the vertebral artery in the posterior circulation.
Figure 2.
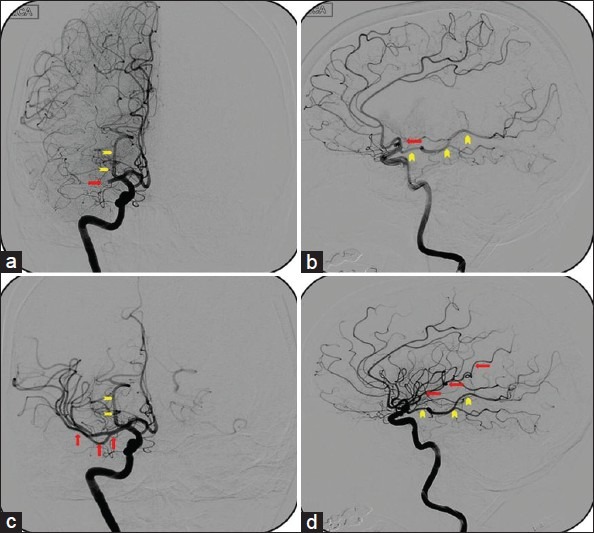
Antero-posterior (a) and lateral (b) cerebral angiogram of a 60-year-old female who presented to the emergency department with symptoms of large vessel occlusion. CT scan of the head was negative for hemorrhage. CT angiogram demonstrated acute cut off of distal right M1 segment - ‘TICI grade 0’ (bold arrow). The vascular territory of fetal PCA (arrow heads) should not be confused with the MCA territory. Solitaire mechanical thrombectomy device was used to retrieve the clot form of the distal M1 segment. Post-procedure antero-posterior (c) and lateral (d) cerebral angiogram illustrating complete opacification of the distal MCA vasculature (arrows). A total of 2 passes were required to clear the clot burden and facilitate flow distally-‘TICI grade 3’
During intervention, additional procedures were performed in 63.4% (14/22) of the procedures. Of these, 4 out of 5 cases of Merci device required additional procedures in the form of IATPA, Balloon angioplasty, or alternate thrombectomy device. Similarly Penumbra required additional procedures in 8 of the 11 cases. However, Solitaire device required additional procedures in 2 of the 6 cases. Although there was no statistical difference between the pre-procedures TICI among the devices, there was a definitive difference among the post-procedure TICI between Solitaire and Penumbra/Merci devices. This can be attributed to the fact that the Stentrievers combine the ability to retrieve the clot and also temporarily bypass the occluded vessel to restore blood flow.
Limitations
Some of the limitations in the current study are the retrospective nature of this study along with small number of cohorts in each group. Our results are limited to immediate post-procedure angiography; and do not compare the angiographic outcome with long-term clinical outcomes. Nonetheless, the literate is scarce with studies comparing various first and second generations’ mechanical thrombectomy devices. We hope that our data offers a skeletal framework for future randomization of studies comparing the first and second generation mechanical thrombectomy devices.
Conclusions
Our limited single center experience proved technical safety and feasibility of mechanical clot retrieval device, namely solitaire along with superior angiographic outcomes when compared to conventional thrombectomy devices like Merci and Penumbra. Further large single or multicenter prospective and randomized studies are required to validate the advantage of one device over the other.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Alexandrov AV, Grotta JC. Arterial reocclusion in stroke patients treated with intravenous tissue plasminogen activator. Neurology. 2002;59:862–7. doi: 10.1212/wnl.59.6.862. [DOI] [PubMed] [Google Scholar]
- 2.Grotta JC, Welch KM, Fagan SC, Lu M, Frankel MR, Brott T, et al. Clinical deterioration following improvement in the NINDS rt-PA Stroke Trial. Stroke. 2001;32:661–8. doi: 10.1161/01.str.32.3.661. [DOI] [PubMed] [Google Scholar]
- 3.Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA Stroke Study Group. Stroke. 1997;28:2109–18. doi: 10.1161/01.str.28.11.2109. [DOI] [PubMed] [Google Scholar]
- 4.Rai AT, Raghuram K, Carpenter JS, Domico J, Hobbs G. Pre-intervention cerebral blood volume predicts outcomes in patients undergoing endovascular therapy for acute ischemic stroke. J Neurointerv Surg. 2012 doi: 10.1136/neurintsurg-2012-010293. [DOI] [PubMed] [Google Scholar]
- 5.Roth C, Papanagiotou P, Behnke S, Walter S, Haass A, Becker C, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010;41:2559–67. doi: 10.1161/STROKEAHA.110.592071. [DOI] [PubMed] [Google Scholar]
- 6.Smith WS. Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part I. AJNR Am J Neuroradiol. 2006;27:1177–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke: Final results of the Multi MERCI trial. Stroke. 2008;39:1205–12. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- 8.The penumbra pivotal stroke trial: Safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–8. doi: 10.1161/STROKEAHA.108.544957. [DOI] [PubMed] [Google Scholar]
- 9.Smith WS, Sung G, Starkman S, Saver JL, Kidwell CS, Gobin YP, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: Results of the MERCI trial. Stroke. 2005;36:1432–8. doi: 10.1161/01.STR.0000171066.25248.1d. [DOI] [PubMed] [Google Scholar]
- 10.Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): A randomised, parallel-group, non-inferiority trial. Lancet. 2012;380:1241–9. doi: 10.1016/S0140-6736(12)61384-1. [DOI] [PubMed] [Google Scholar]
- 11.Dorn F, Stehle S, Lockau H, Zimmer C, Liebig T. Endovascular treatment of acute intracerebral artery occlusions with the solitaire stent: Single-centre experience with 108 recanalization procedures. Cerebrovasc Dis. 2012;34:70–7. doi: 10.1159/000338903. [DOI] [PubMed] [Google Scholar]
- 12.Stampfl S, Hartmann M, Ringleb PA, Haehnel S, Bendszus M, Rohde S. Stent placement for flow restoration in acute ischemic stroke: A single-center experience with the Solitaire stent system. AJNR Am J Neuroradiol. 2011;32:1245–8. doi: 10.3174/ajnr.A2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 14.Schellinger PD, Ringleb P, Hacke W. European Stroke Organisation 2008 guidelines for managing acute cerebral infarction or transient ischemic attack: Part 2. (1186-8, 1190-201).Nervenarzt. 2008;79:1180–4. doi: 10.1007/s00115-008-2532-0. [DOI] [PubMed] [Google Scholar]
- 15.Wahlgren N, Ahmed N, Davalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): An observational study. Lancet. 2007;369:275–82. doi: 10.1016/S0140-6736(07)60149-4. [DOI] [PubMed] [Google Scholar]
- 16.del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: A phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT Investigators. Prolyse in Acute Cerebral Thromboembolism. Stroke. 1998;29:4–21. doi: 10.1161/01.str.29.1.4. [DOI] [PubMed] [Google Scholar]
- 17.Kulcsar Z, Bonvin C, Pereira VM, Altrichter S, Yilmaz H, Lövblad KO, et al. Penumbra system: A novel mechanical thrombectomy device for large-vessel occlusions in acute stroke. AJNR Am J Neuroradiol. 2010;31:628–33. doi: 10.3174/ajnr.A1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tenser MS, Amar AP, Mack WJ. Mechanical thrombectomy for acute ischemic stroke using the MERCI retriever and penumbra aspiration systems. World Neurosurg. 2011;76:S16–23. doi: 10.1016/j.wneu.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Jeromel M, Milosevic ZV, Kocijancic IJ, Lovric D, Svigelj V, Zvan B. Mechanical Revascularization for Acute Ischemic Stroke: A Single-Center, Retrospective Analysis. Cardiovasc Intervent Radiol. 2012 doi: 10.1007/s00270-012-0441-x. [DOI] [PubMed] [Google Scholar]
- 20.Bosel J, Hacke W, Bendszus M, Rohde S. Treatment of acute ischemic stroke with clot retrieval devices. Curr Treat Options Cardiovasc Med. 2012;14:260–72. doi: 10.1007/s11936-012-0172-y. [DOI] [PubMed] [Google Scholar]
- 21.Cohen JE, Gomori JM, Leker RR, Moscovici S, Ramirez-Denoriega F, Itshayek E. Recanalization with stent-based mechanical thrombectomy in anterior circulation major ischemic stroke. J Clin Neurosci. 2012;19:39–43. doi: 10.1016/j.jocn.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Day JS, Hurley MC, Chmayssani M, Rahme RJ, Alberts MJ, Bernstein RA, et al. Endovascular stroke therapy: A single-center retrospective review. Neurosurg Focus. 2011;30:E10. doi: 10.3171/2011.3.FOCUS10267. [DOI] [PubMed] [Google Scholar]
- 23.Levy EI, Rahman M, Khalessi AA, Beyer PT, Natarajan SK, Hartney ML, et al. Midterm clinical and angiographic follow-up for the first Food and Drug Administration-approved prospective, Single-Arm Trial of Primary Stenting for Stroke: SARIS (Stent-Assisted Recanalization for Acute Ischemic Stroke) Neurosurgery. 2011;69:915–20. doi: 10.1227/NEU.0b013e318222afd1. [DOI] [PubMed] [Google Scholar]
- 24.Levy EI, Siddiqui AH, Crumlish A, Snyder KV, Hauck EF, Fiorella DJ, et al. First Food and Drug Administration-approved prospective trial of primary intracranial stenting for acute stroke: SARIS (stent-assisted recanalization in acute ischemic stroke) Stroke. 2009;40:3552–6. doi: 10.1161/STROKEAHA.109.561274. [DOI] [PubMed] [Google Scholar]
- 25.Mordasini P, Brekenfeld C, Byrne JV, Fischer U, Arnold M, Jung S, et al. Experimental Evaluation of Immediate Recanalization Effect and Recanalization Efficacy of a New Thrombus Retriever for Acute Stroke Treatment In Vivo. AJNR Am J Neuroradiol. 2012 doi: 10.3174/ajnr.A3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wehrschuetz M, Wehrschuetz E, Augustin M, Niederkorn K, Deutschmann H, Ebner F. Early single center experience with the solitaire thrombectomy device for the treatment of acute ischemic stroke. Interv Neuroradiol. 2011;17:235–40. doi: 10.1177/159101991101700216. [DOI] [PMC free article] [PubMed] [Google Scholar]


