Abstract
Objective
To evaluate the relationship of family and parenting factors to long-term executive dysfunction and attention problems after early childhood traumatic brain injury (TBI). We hypothesized that the magnitude of executive dysfunction and attention problems would be moderated by family and parenting factors.
Design
A multicenter, prospective cohort study that included an orthopedic injury (OI) reference group.
Setting
Three tertiary academic children’s hospital medical centers and one general medical center.
Participants
Children, ages 3–7 years, hospitalized for OI, moderate TBI, or severe TBI.
Methods and Outcome Measurements
Parental ratings of family functioning and parenting styles were obtained 18 months after the injury occurred. The main outcome measurements, which were parental ratings of children’s executive function and attention, were performed at least 24 months after the injury occurred (mean, 39 months; range, 25–63 months).
Analysis
Group comparisons were conducted with use of t-tests, χ2 analysis, analysis of variance, and Pearson and Spearman correlations. Regression analysis was used to examine associations of the outcomes with family functioning and parenting styles and to test moderating effects of these factors on group differences.
Results
Participants with severe TBI demonstrated increased executive dysfunction and attention problems compared with those who sustained moderate TBI or OI. Lower levels of family dysfunction were associated with better executive function and attention across groups but did not moderate group differences. However, attention deficits after severe TBI were exacerbated under conditions of more permissive parenting relative to attention deficits after OIs.
Conclusions
Executive function and attention problems persisted on a long-term basis (>24 months) after early childhood TBI, and positive global family functioning and nonpermissive parenting were associated with better outcomes. Better characterization of the optimal family environment for recovery from early childhood TBI could help target future interventions.
INTRODUCTION
Traumatic brain injury (TBI) is a major public health concern [1,2]. An estimated 1.7 million people sustain a TBI annually in the United States [2]. In children 0–14 years of age, an estimated 473,947 emergency visits, 35,136 hospitalizations, and 2174 deaths are related to TBI each year [2]. Pediatric TBI has a long-term impact among survivors, with neurocognitive and behavioral deficits predominating after the injury occurs [3–8].
In early childhood TBI (ie, in children aged 2–6 years), more severe injuries and younger age at injury are associated with poorer outcomes across multiple behavioral, cognitive, and educational domains [9–11]. In general, executive dysfunction and attention problems are common after pediatric TBI [12–17]. Executive function is associated with various cognitive and behavioral constructs, including attentional control, cognitive flexibility, goal setting, and information processing [18]. Executive functions begin developing in early childhood and continue to mature and develop through adolescence and young adulthood [18,19]. Because the development of executive functions and problem-solving skills is important for children to succeed academically, socially, and behaviorally, an important goal is to characterize the effect TBI has on executive function and attention outcomes in children.
TBI has lasting negative effects on school-aged children. In an investigation of children aged 7–15 years who sustained a moderate or severe TBI, executive dysfunction was present 1 year after the injury occurred, especially in children who sustained an injury at a younger age [20]. In addition, executive dysfunction and attention problems measured 2 years after a childhood TBI (in children aged 8–12 years) were most pronounced in those who sustained a severe injury [21,22]. Executive dysfunction also has been associated with decreased social problem-solving skills and poorer social outcomes in young adults who sustained a TBI in late childhood or early adolescence (ie, from ages 8–12 years), which suggests that the effects of a TBI extend to critical aspects of everyday functioning [23].
Emerging research that is examining long-term executive dysfunction after early childhood TBI is providing evidence of persistent effects, particularly among younger children and those with more severe injuries. Specifically, Ewing-Cobbs et al [16] demonstrated that working memory and inhibitory control measured approximately 1–2 years after injury were adversely affected, especially after moderate and severe TBI that occurred before the age of 6 years. Similarly, Anderson et al [24] reported attention impairments 30 months after early childhood TBI (ie, in children aged 2–7 years), with the most pronounced effects following more severe injuries and those occurring at a younger age.
Family environment, socioeconomic status (SES), and availability of resources play important roles in moderating recovery after pediatric TBI [11,25]. TBI is known to lead to increased family stressors and injury-related family burden [26–32]. Conversely, family functioning, both before and after the injury, also affects the recovery process [33–35]. Previous work has demonstrated main and moderation effects of family environment on recovery after early childhood TBI. Poor family functioning is associated with increased executive dysfunction across different severities of injury (main effects); however, the combination of more severe injuries with poor family functioning is associated with a greater increase in executive dysfunction (moderation effects) [36]. When TBI occurs in later childhood, the family environment also moderates recovery most significantly in persons with severe TBI [25]. Maladaptive parenting styles, family dysfunction, and low SES predict clinical elevations in executive dysfunction and externalizing behaviors longitudinally across the initial 18 months after early childhood TBI [37]. Favorable family environments were associated with better outcomes over an 18-month period across multiple domains, including global cognitive function, memory, spatial reasoning, and executive function, regardless of the nature (TBI versus orthopedic injury [OI]) or severity of the injury [38].
Further elucidation of the joint effect that early childhood TBI and environmental factors have on long-term executive function and attention is necessary to improve the understanding of recovery after early childhood TBI. In this study, we built upon previous work that evaluated outcomes of early childhood TBI up to 18 months after the injury occurred [37,38]. We examined the relationship of family functioning and parenting practices assessed 18 months after the time of the injury to long-term (>24 months after injury) attention and executive function deficits after moderate and severe pediatric TBI in early childhood (ages 3–6 years). We tested 2 alternative models of environmental influence. First, we examined the hypothesis that positive global family functioning and effective parenting are associated with less executive dysfunction and fewer attention problems long term, not only after early childhood TBI for children with both moderate and severe injuries, but also for children with OI. An alternative possibility is that family function and parenting would moderate the association of injury severity with executive dysfunction and attention problems. Specifically, the effects of family functioning and parenting on executive dysfunction and attention problems would be more evident in children with more-severe TBI than in children with moderate TBI or OI. Previous research supports both main and moderating effects of the social environment on recovery of executive function and attention after early childhood TBI [36–39]. This study provides an opportunity to distinguish these alternate models of influence.
METHODS
Participants
Participants were recruited from a broader prospective, longitudinal study that evaluated recovery from early childhood TBI. Participants in this study were recruited from 3 children’s hospitals and one general hospital in Ohio. As part of the original study, the participants underwent assessments at multiple time points, including the immediate postacute period (0–3 months after injury) and 6, 12, and 18 months after the injury occurred. The assessment at 18 months after the time of the injury included measures of parenting style and family functioning completed by the parents. For the current study, the parents completed an additional follow-up assessment by mail an average of 39 months after the injury occurred (range, 25–63 months). As part of that assessment, they completed ratings of children’s executive functioning and attention.
Inclusion criteria included hospitalization overnight for traumatic injury (TBI or OI) sustained between the ages of 36 and 83 months, no evidence of child abuse as the cause of the injury, no history of documented neurologic problems or developmental delays before the injury, and English as the primary language in the home. The participants were divided into 3 groups: severe TBI, moderate TBI, and OI. We used the Glasgow Coma Scale (GCS) to characterize TBI severity [40]. The severe TBI group had a GCS score less than or equal to 8 as the lowest postresuscitation score. The moderate TBI group had a GCS score of 9–12 or a GCS score of 13–15 in association with abnormal brain imaging. Children with mild TBI, defined as a GCS of 13–15 without evidence of abnormal brain imaging, were excluded from the current analysis to focus on the more-severe injuries. The OI group included children who sustained a bone fracture (not including skull fractures), had an overnight stay in the hospital, and did not exhibit alterations in consciousness or other signs or symptoms of head trauma or brain injury.
Procedures for the Extended Mail Follow-up Study
Upon approval by each site’s institutional review board, all the parents or guardians of the participants enrolled in the initial study were contacted by telephone and/or mail by a research coordinator at the initial recruitment site. The participants who had previously withdrawn from the parent study or asked not to be contacted in the future were not recruited for this study. During the initial contact, the study was explained to the primary caregiver (parent or guardian), who then was invited to participate. Once parents and/or guardians verbally agreed to participate, a research coordinator sent out a packet of questionnaires, a cover letter that outlined all the required elements of consent, a telephone number for use if the parent or guardian had any questions concerning participation, and a self-addressed, stamped envelope in which to return the questionnaires. The mailing procedures also were approved by the institutional review boards of all the participating institutions. Upon completion and return of the questionnaires, the parents were paid a modest amount for their time and effort.
Family Functioning and Parenting Assessments
The 12-item General Functioning subscale of the McMaster Family Assessment Device (FAD-GF) was used to assess family functioning. The FAD-GF has shown good reliability and validity [41,42] and has been used previously in the evaluation of pediatric TBI to assess family functioning [43]. Lower scores represent better family functioning. The Parenting Practices Questionnaire (PPQ) was used to assess the extent to which parents characterize themselves as engaging in authoritative, authoritarian, and permissive parenting behaviors [44]. The PPQ is a 62-item instrument that uses a 5-point Likert scale. We used the raw total score for each of these dimensions to characterize parenting styles, which originally were described by Baumrind [45,46]. The permissive parent allows the child to regulate his or her own activities, avoids control, and uses reason and manipulation but not power to parent the child. The authoritarian parent shapes and controls the child in accordance with a set standard and often restricts the child’s autonomy. The authoritative parent directs the child in a rational manner, encourages give and take, and both autonomy and disciplined conformity are valued. Permissive and authoritarian parenting styles are generally considered maladaptive, whereas authoritative parenting is considered an effective parenting style.
Executive Function and Attention Measures
The Behavior Rating Inventory of Executive Function (BRIEF) is a parent-rated measure of executive dysfunction [47–50]. A school-age version is used for children aged 5–18 years [50] and a preschool version is used for children aged 2–5 years [49]. The measure has good internal consistency, interrater reliability, and test-retest reliability and has been validated in children with TBI [47]. The Global Executive Composite score was used to measure global executive functioning in this study. Higher scores indicate increased executive dysfunction, with a score of 65 or higher indicating clinical impairment. In addition, inconsistency scores on the BRIEF were reviewed, and none of the questionnaires met the criteria for inconsistency; therefore, all questionnaires were determined to be valid.
The Child Behavior Checklist (CBCL) is a widely used measure that assesses a child’s competencies and adjustment. It includes school-age [51] and preschool versions [52]. In this study, we used the CBCL Attention Deficit Hyperactivity Disorder (ADHD) rating scale to specifically assess attention problems. Higher scores indicate more attention problems, with a score of 65 or higher defining clinical impairment. During the immediate postacute period (0–3 months) after injury, parents were asked to rate the child based on preinjury behavior on the BRIEF and CBCL ADHD rating scale to assess preinjury executive function and attention. The BRIEF and CBCL were completed at the extended follow-up more than 24 months after the injury occurred to assess longer-term postinjury functioning.
Rationale for Use of Measures and Assessments at Specified Follow-up Time Points
We used FAD-GF and PPQ scores that were obtained 18 months after the time of the injury in the analysis to prospectively examine the relationship of family functioning and parenting styles to later executive dysfunction and attention problems. We chose to use measures of family functioning and parenting styles obtained 18 months after the injury occurred because they best addressed our hypothesis that family functioning and parenting styles would potentially influence executive functioning and attention in the future, 24 months after the time of the injury. Longitudinal analyses suggest substantial stability in FAD-GF and PPQ scores over time, with Pearson correlation coefficients ranging from 0.56–0.77.
Data Analysis
The two-tailed t-test and χ2 were used to examine possible differences between participants and nonparticipants with regard to demographic and injury characteristics, including mean age at the time of the injury, the mean injury severity score, gender, race, SES, type of injury, mean GCS, and percentage of abnormal computed tomography scans. An index of SES was constructed by averaging z scores for caregiver education and census tract income. Analysis of variance was used to compare executive function measures (BRIEF), attention measures (CBCL Attention Deficit Hyper-activity Problems scale), quality of family functioning (FAD-GF), and parenting style (PPQ) among the OI, moderate TBI, and severe TBI groups. The Bonferroni method for multiple comparisons with analysis of variance was used to conduct post hoc comparisons of the individual groups. A χ2 analysis was used to compare the proportion of individuals within the OI, moderate TBI, and severe TBI groups that scored in the impaired range on the BRIEF and CBCL Attention Deficit Hyperactivity Problems scale. Pearson or Spearman correlations were used to evaluate the association of the primary outcome measures (BRIEF and CBCL Attention Deficit Hyperactivity Problems scores), covariates (baseline BRIEF, baseline CBCL Attention Deficit Hyperactivity Problems scores, race, SES, and time since injury), and quality of family functioning (FAD-GF) with parent practices. General linear regression was performed by using the BRIEF and CBCL Attention Deficit Hyperactivity Problems scores as dependent variables. The TBI injury group was divided into a moderate group and a severe group based on the severity of injury, with the OI group serving as a reference category. Dummy coding was used to contrast the moderate and severe TBI groups with the OI reference group. Interaction terms were created to allow us to examine whether the relationship of family functioning and parenting styles to executive function and attention problems varied as a function of the nature (OI versus TBI) and severity (moderate versus severe TBI) of the injury (moderation hypothesis). Initially, all covariates, FAD-GF, parenting style ratings, and interaction terms were included in the model. Factors that did not demonstrate an influence (P > .15) were trimmed from the final model. These factors included race, time since the injury occurred, parenting style, and all interaction terms for both models, except for the permissive parenting interactions term, which was significant in the CBCL Attention Deficit Hyperactivity Problems scale model. Therefore the permissive parenting rating and interactions terms between permissive parenting and injury severity were included in the final model for this variable only. SPSS 15 for Windows was used to perform all analyses (SPSS for Windows, 2006; SPSS Inc, Chicago, IL).
RESULTS
Analysis of Demographics
Of the 221 families initially recruited into the broader study, 154 agreed to participate and completed the questionnaires in the extended follow-up study. Persons who participated in the study included 68 parents of children with moderate-to-severe TBI and 75 parents of children with OI. Demographic variables were compared between participating and nonparticipating families (Table 1). A significant difference was noted in the mean age at the time of the injury, in that participants were significantly younger at the time the injury occurred than were nonparticipants. In addition, a higher percentage of participants sustained a TBI (47.6%) than did the nonparticipants (30.2%).
Table 1.
Comparison of demographic variables between participants and nonparticipants with use of the 2-tailed t-test or χ2 test
| Participants | Nonparticipants | |
|---|---|---|
| All subjects | ||
| Mean (SD) age at injury, mo | 59.20 ± 13.36* | 63.51 ± 12.40* |
| Mean (SD) ISS | 10.27 ± 6.81 | 9.82 ± 6.38 |
| % Male gender | 55.20 | 68.30 |
| % Not white | 28.00 | 28.60 |
| SES (SD) | 0.04 ± 1.01 | −.04 ± 0.98 |
| Census median (SD) family income in thousands of dollars | 60.46 ± 22.82 | 61.68 ± 26.65 |
| Percent below poverty (SD) | 11.83 ± 13.63 | 12.45 ± 13.71 |
| Percent OI* | 52.40* | 69.80* |
| Percent TBI* | 47.6* | 30.20* |
| TBI only | ||
| Mean (SD) GCS | 10.69 ± 4.72 | 11.68 ± 4.58 |
| % Abnormal CT scan | 77.90 | 84.20 |
| Percent severe TBI | 27.90 | 21.10 |
SD = standard deviation; ISS = injury severity scale; SES = socioeconomic status measured by combined caregiver education and census tract income z score; OI = orthopedic injury; TBI = traumatic brain injury; GCS = Glasgow Coma Scale; CT = computed tomography.
Indicates significant differences between the groups; P < .05.
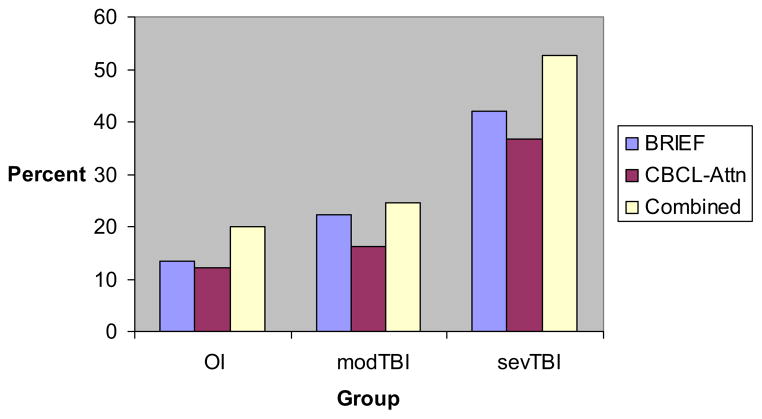
Comparison of Primary Outcome and Environmental Measures Between Groups
As reported in Table 2, children with severe TBI have significantly higher scores on the BRIEF and CBCL Attention Deficit Hyperactivity Problems scale than did those with moderate TBI (BRIEF: P = .02, CBCL: P < .005) or OI (BRIEF: P < .005, CBCL: P < .005), based on Bonferroni post hoc comparisons. No significant differences were found between the OI and moderate TBI groups on the BRIEF and CBCL Attention Deficit Hyperactivity Problems scale. Significant differences were found between groups in the proportion of persons who scored above the clinical cutoffs for the BRIEF and CBCL Attention Deficit Hyperactivity Problems scales (Figure 1). A significantly higher percentage of persons in the severe TBI group were in the impaired range on the BRIEF (P = .02) and CBCL Attention Deficit Hyperactivity Problems scale (P = .04) compared with the OI and moderate TBI groups. The groups did not differ on measures of global family functioning (FAD-GF) or parenting practices.
Table 2.
Analysis of variance, comparing mean (standard deviation) of executive function, attention, and family functioning measures among orthopedic injury, severe traumatic brain injury, and moderate traumatic brain injury groups
| Measure | OI | Moderate TBI | Severe TBI | P Value |
|---|---|---|---|---|
| BRIEF | 49.10 ± 11.80 | 50.80 ± 14.93 | 60.89 ± 13.49 | <.005 |
| CBCL-Attn | 54.46 ± 6.65 | 55.45 ± 7.82 | 62.39 ± 8.07 | <.005 |
| FAD-GF | 1.54 ± 0.52 | 1.63 ± 0.41 | 1.74 ± 0.55 | .26 |
| PPQ ratings | ||||
| Authoritative | 4.28 ± 0.38 | 4.33 ± 0.35 | 4.1 ± 0.42 | .10 |
| Authoritarian | 1.91 ± 0.41 | 1.92 ± 0.42 | 1.93 ± 0.52 | .98 |
| Permissive | 2.03 ± 0.52 | 2.04 ± 0.42 | 2.28 ± 0.48 | .14 |
OI = orthopedic injury; TBI = traumatic brain injury; BRIEF = Behavioral Rating Inventory of Executive Function; CBCL-Attn = Child Behavior Checklist Attention Deficit Hyperactivity Problems score; FAD-GF = Family Assessment Device general functioning scale; PPQ = Parental Practice Questionnaire ratings.
Figure 1.
The percentage of individuals in the impaired range within the orthopedic injury, moderate traumatic brain injury, or severe traumatic brain injury groups on executive function and attention measures. OI = orthopedic injury; modTBI = moderate TBI; sevTBI = severe TBI; BRIEF = Behavioral Rating Inventory of Executive Function; CBCL-Attn = Child Behavior Checklist Attention Deficit Hyperactivity Problems score; Combined = individuals with scores in the impaired range for either the BRIEF or CBCL-Attn.
Correlation of Measures of Executive Function and Attention With Family Measures
As shown in Table 3, higher levels of executive dysfunction on the BRIEF at extended follow-up were associated with higher levels of executive dysfunction before the injury, lower SES, greater family dysfunction on the FAD-GF, and greater endorsement of both authoritarian and permissive parenting styles. However, executive dysfunction was unrelated to race, time since the injury occurred, or authoritative parenting. A similar pattern of associations was found for the attention problems at follow-up. This finding was expected because the BRIEF and CBCL Attention Deficit Hyperactivity Problems scores were positively correlated with each other.
Table 3.
Correlation of outcome measures, covariates, family functioning measures, and parenting styles*
| BRIEF | CBCL-Attn | Race: White | SES | TSS | FAD-GF | Authoritative | Authoritarian | Permissive | Baseline Brief | |
|---|---|---|---|---|---|---|---|---|---|---|
| BRIEF | xxxx | |||||||||
| CBCL-Attn | .81† | xxxx | ||||||||
| Race: white | −.07 | −.13 | xxxx | |||||||
| SES | −.29† | −.37† | .34† | xxxx | ||||||
| TSS | .07 | .10 | .03 | −.05 | xxxx | |||||
| FAD-GF | .32† | .34† | −.01 | −.06 | .00 | xxxx | ||||
| Authoritative | −.16 | −.16 | .01 | .05 | −.16 | −.34† | xxxx | |||
| Authoritarian | .32† | .28† | −.04 | −.06 | −.13 | .40† | −.42† | xxxx | ||
| Permissive | .29† | .32† | −.06 | −.24† | −.09 | .35† | −.23† | .50† | xxxx | |
| Baseline BRIEF | .60† | .52† | −.09 | −.20† | .04 | .17† | −.10 | .30† | .36† | xxxx |
| Baseline CBCL | .51† | .49† | −.15 | −.23† | .07 | .17† | .02 | .20† | .35† | .71† |
BRIEF = Behavioral Rating Inventory of Executive Function; CBCL-Attn = Child Behavioral Checklist Attention Deficit Hyperactivity Problems score; SES = socioeconomic status measured by combined caregiver education and census tract income z score; TSS = time since injury; FAD-GF = Family Assessment Device general functioning scale.
Pearson correlations were used for all comparisons except for race, which was compared with other variables through use of the Spearman correlation.
Indicates correlation is significant at the .05 level (2 tailed).
Regression Models
Executive Function Model (BRIEF Global Executive Composite Score)
Quality of family functioning (FAD-GF) accounted for significant variance in executive functioning (BRIEF); specifically, higher levels of family dysfunction at 18 months after the injury were associated with more executive difficulties at long-term follow-up (Table 4). With family functioning in the model, parenting style did not account for significant variance in executive function, and thus parenting style was trimmed from the model. The interaction terms between TBI severity and quality of family function or parenting styles also were not significant, and thus the interaction terms were trimmed from the model.
Table 4.
Linear regression analysis for executive function and attention measures
| Variable | R2 | R2 Change | Significance, F-change | Standard Coefficients, β | Coefficient β, 95% CI | Significance |
|---|---|---|---|---|---|---|
| BRIEF | ||||||
| Baseline score | .36 | .36 | <.005 | .51 | 0.40–0.68 | <.005 |
| SES | .40 | .03 | .01 | −.14 | −3.90 to −0.08 | .04 |
| Severe TBI vs OI | .42 | .03 | .05 | .16 | 0.567–11.89 | .03 |
| Moderate TBI vs OI | .00 | −3.98-3.81 | .97 | |||
| FAD-GF | .46 | .04 | <.005 | .20 | 1.976–9.26 | <.005 |
| CBCL-Attn | ||||||
| Baseline score | .24 | .24 | <.005 | .36 | 0.30–0.69 | <.005 |
| SES | .31 | .07 | <.005 | −.23 | −2.88 to −0.68 | <.005 |
| Severe TBI vs OI | .38 | .07 | <.005 | −.64 | −29.09-0.28 | .05 |
| Moderate TBI vs OI | .39 | −4.18–16.68 | .24 | |||
| FAD-GF | .43 | .05 | .01 | .20 | 0.97–5.35 | .01 |
| Permissive | .01 | −2.78–3.00 | .94 | |||
| Moderate TBI, permissive | .47 | .05 | .01 | −.40 | −8.15–1.90 | .22 |
| Severe TBI, permissive | .90 | 2.33–15.200 | .01 | |||
BRIEF = Behavioral Rating Inventory of Executive Function; SES = socioeconomic status measured by combined caregiver education and census tract income z score; TBI = traumatic brain injury; OI = orthopedic injury; FAD-GF = Family Assessment Device general functioning scale; CBCL-Attn = Child Behavioral Checklist Attention Deficit Hyperactivity Problems score; Permissive = permissive parenting raw score rating.
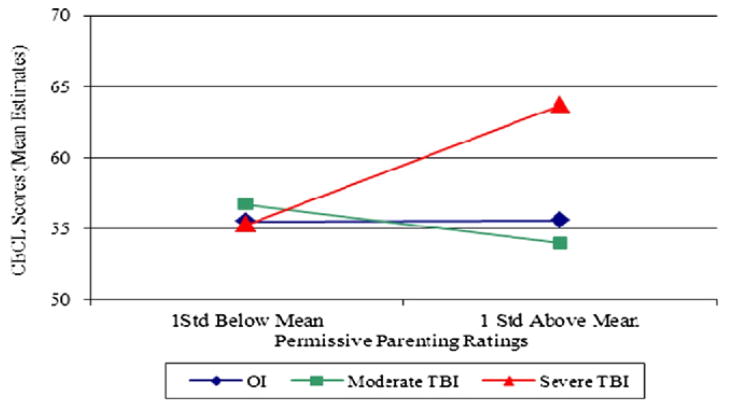
Attention Problems Model (The Child Behavior Checklist Attention Deficit Hyperactivity Disorder Rating Scale)
Quality of family functioning (FAD-GF) also accounted for significant variance in attention (Table 4). Again, higher levels of family dysfunction at 18 months after the injury were associated with more attention problems at long-term follow-up. The interaction between permissive parenting and TBI severity also was significant. Therefore, permissive parenting and interaction terms with permissive parenting were kept in the final attention problems model (Table 4; Figure 2). Higher ratings of permissive parenting were associated with more attention problems after severe TBI but not moderate TBI or OI (Figure 2). Put differently, the difference between the severe TBI and OI groups was larger at higher levels of permissive parenting. Authoritarian and authoritative parenting practices did not account for significant variance in either model.
Figure 2.
Mean estimates of Child Behavior Checklist Attention Deficit Hyperactivity Problems scores (y axis) for permissive parent ratings dichotomized by one standard deviation below or above the mean (x axis) for groups (orthopedic injury, moderate traumatic brain injury, and severe traumatic brain injury). CBCL = Child Behavior Checklist; OI = orthopedic injury; TBI = traumatic brain injury.
Overall, these findings indicate that lower family dysfunction is associated with less executive dysfunction and attention problems regardless of the severity or type of injury (OI versus TBI). The findings also provide evidence that permissive parenting moderates the association of injury severity with long-term attention problems, specifically exacerbating the adverse effects of severe TBI.
DISCUSSION
We found that executive dysfunction and attention problems, as rated by parents or guardians after early childhood TBI, persisted in children with severe TBI an average of 39 months after the time of the injury compared with children who had OI and moderate TBI. Children from more dysfunctional families, regardless of parenting styles or severity of injury, also had greater difficulties with executive function and attention. We failed to find evidence that family functioning moderated the association of injury severity with either long-term executive function or attention. However, permissive parenting moderated the association of severe TBI with long-term attention problems. Higher ratings of permissive parenting were associated with more attention problems after severe TBI. At least 2 explanations for this finding exist. Permissive parenting may exacerbate the negative effects of TBI on attention problems, or it may be that because attention problems in severe TBI are difficult to control effectively, parents become more permissive in their approach to managing the child. In other words, parenting could affect attention problems in the child or the child’s inattentiveness could affect parenting. Previous research provides evidence of a bidirectional relationship between the family’s functioning and the child’s behavioral adjustment after TBI and points to the possibility of complex reciprocal relationships over time [53].
Because the TBI-related family burden may increase over time [54], the nature of the reciprocal relationship of family functioning to child behavior also is likely to change over time. Family functioning and social resources also moderate the relationship of TBI-related burden and caregiver distress [31]; therefore, changes in social resources over time also may influence the bidirectional relationship between parenting and child executive function and behavior. In this project, our measures of family function and parenting styles remained stable over time. However, unmeasured relationships or influences that change on a more incremental basis may exist, and if so, they were not captured in this study. Nadebaum et al [36] examined executive functions 5 years after early TBI and demonstrated that executive dysfunction was greatest after severe TBI and that a positive family environment contributed to better outcomes. Their study included 54 subjects in the TBI group and 17 “healthy controls.” The current study adds to these findings by demonstrating long-term effects on executive function and attention in children with severe TBI relative to an “other injury” comparison group. The current study also extends findings from a previous follow-up of children from the same cohort at 18 months after the time of the injury [37,38] by demonstrating persistent executive dysfunction and attention deficits more than 3 years after the injury occurred on average.
Many correlations were significant among the primary outcome measures of executive function and attention, covariates, and the social environmental measures. Consistent with our hypotheses and prior research, lower SES, maladaptive parenting styles (permissive and authoritarian), and poorer global family functioning were each associated with long-term executive dysfunction and attention problems. These findings may reflect a complex interplay among multiple factors that determines the ideal environment to promote long-term recovery of executive function and attention problems.
In multivariate regression models, global family functioning demonstrated main effects on long-term executive function and attention measures after accounting for the effects of parenting, SES, and injury severity. This finding is in agreement with previous studies that demonstrated that better family functioning was associated with better executive functioning after pediatric TBI [36–38]. The association of preinjury psychosocial difficulties with attention deficits after TBI observed in this study is also consistent with past research [12,55]. We found no evidence that global family functioning moderated the effects of injury severity on executive functioning or attention. Although these findings are contrary to our hypothesis, they are consistent with those of Yeates et al [39], who found evidence that social moderation effects diminished with increasing time since the injury in the same cohort. Thus although the social environment broadly and family functioning specifically continue to be important to executive functioning and attention problems in early childhood TBI, the association holds true regardless of the type or severity of the injury. However, we did find that permissive parenting moderated the association of severe TBI with attention problems more than 3 years after the injury occurred, which is in agreement with findings from Chapman et al [37], who demonstrated that permissive parenting was associated with increased behavioral dysfunction in the same cohort up to 18 months after the time of the injury [39]. Although our primary outcome measures of attention and executive function were correlated with each other, permissive parenting only moderated the effect of group (ie, TBI severity) on our attention measure. It is not surprising that our measures of executive function and attention are correlated, because attention is a component of executive function (ie, poor attention is likely to lead to executive dysfunction). The BRIEF score incorporates various constructs of executive function, including areas of emotional control, initiation, working memory, and organization, whereas the CBCL ADHD scale measures the symptoms of ADHD more specifically. The finding of moderation effects only with the ADHD scale in persons with severe TBI deserves further consideration. It is possible that permissive parenting has a more significant impact on the emergence of ADHD symptomatology after severe TBI, but the impact is of smaller magnitude when considering the more global construct of executive function. In addition, although we evaluated a relatively large cohort of persons with moderate or severe TBI, we still may not have had sufficient power to detect subtle moderation effects.
The persistence of problems more than 3 years after the injury occurred suggests that persons who sustained an early childhood TBI should be followed up into later childhood and adolescence. In this study, more than 50% of children who sustained a severe TBI in early childhood exhibited clinically impaired executive function or attention. Family function was important in determining long-term executive and attention functioning across injury types and severity. In addition, parenting styles could affect the association of severe TBI with long-term attention problems.
LIMITATIONS
One limitation of the study is that children who sustained an injury at a younger age were more likely to participate in the long-term follow-up than were children who sustained an injury at an older age. This differential attrition could potentially limit the generalizability of the results to the slightly younger individuals in the current cohort; however, the difference in average age at time of injury between the participants and nonparticipants was only 4 months. This difference is unlikely to be of clinical significance, especially because the development of executive function occurs on a continuum throughout childhood and adolescence [18]. In addition, attrition was greater within the OI group, which could potentially limit our power to detect subtle differences. Our preinjury measures of executive function and attention were subjected to recall bias because the measures were obtained 0–3 months after the injury occurred. As a consequence, the association of these baseline measures with long-term outcomes after injury may be artificially inflated. Moreover, by statistically controlling for preinjury functioning, we may be statistically reducing the likelihood of finding differences and associations after the injury occurred. In addition, because our primary outcome measures of executive dysfunction and attention problems were based on caregiver ratings, a potential bias related to these ratings exists.
Caregivers of children with TBI are likely emotionally involved in the care of their children, and ratings could potentially yield different results if assessments were performed by individuals not directly involved in caretaking responsibilities. However, the outcome measures used, BRIEF and CBCL, have been well validated with other widely accepted measures of executive dysfunction and attention problems [49–52]. Furthermore, caregivers likely have the most significant interaction with their children and will likely provide the most accurate assessment of executive and attention functioning on an everyday basis. The BRIEF was specifically developed to assess “real-world” manifestation of executive function [47], and it does not necessarily correlate with performance-based measures of executive function [56].
Finally, our family assessment measures and parent practice questionnaires also were based on caregiver self-ratings. Collection of parenting and/or family variables and child outcomes from a single informant, the primary caregiver, may artificially inflate associations. However, the FAD-GF and PPQ are commonly used in the literature and have been well validated as assessment tools [42,46]. Thus, despite these limitations, the primary findings that caregiver ratings of executive dysfunction and attention problems persist long term after early childhood TBI and that improved family function is associated with improved outcomes remain valid.
CONCLUSION
Executive function and attention problems rated by caregivers persist on a long-term basis after early childhood TBI, and positive global family functioning is associated with improved outcomes for all injury types. These findings extend previous research on outcomes of TBI in young children by demonstrating these associations in a relatively large cohort of young children with TBI compared with children who have OI. The findings indicate that executive dysfunction and attention problems persist long after early childhood TBI and that family functioning is important in determining the overall outcome. Future research is needed to determine specific family functions that are associated with better recovery. Numerous potentially important environmental factors that were not examined in the current study (eg, parental health status, number of siblings, community resources, and the presence of an extended family) influence family functioning and, ultimately, recovery and reintegration of the child with TBI into the family. In addition, further elucidation of the bidirectional relationship between family functioning and child behavior after an injury occurs is warranted and should be extended to additional outcomes (eg, cognitive, behavioral, and psychosocial) beyond those evaluated here. A more detailed characterization of the optimal family environment for recovery from early childhood TBI could help target future interventions. Long-term rehabilitation programs that facilitate management of executive function and attention will be critical for these children to be as successful as possible. Family and parental training and education would likely be an important component in these programs.
Acknowledgments
Research support: Funding for this study was provided through grant R01 HD42729 from the National Institute of Child Health and Human Development, Rehabilitation Medicine Scientist Training Program (RMSTP) grant 7K12 HD001097-14, in part by United States Public Health Service National Institutes of Health grant M01 RR 08084, and by Trauma Research grants from the State of Ohio Emergency Medical Services.
We thank Christine Abraham, Andrea Beebe, Lori Bernard, Anne Birnbaum, Beth Bishop, Tammy Matecun, Karen Ober-john, and Elizabeth Roth for their contributions, and Maegan Swarthout for assistance with data collection and coding. We also thank Amy Cassedy, PhD, for her assistance with data management. The Cincinnati Children’s Medical Center Trauma Registry, Rainbow Pediatric Trauma Center, Rainbow Babies and Children’s Hospital, Columbus Children’s Hospital Trauma Program, and MetroHealth Center Department of Pediatrics and Trauma Registry provided assistance with recruitment.
Footnotes
Disclosure: nothing to disclose
Contributor Information
Brad G. Kurowski, Division of Physical Medicine and Rehabilitation, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Ave, MLC 4009, Cincinnati, OH 45229, and Department of Pediatrics, Cincinnati Children’s Hospital Medical Center and University of Cincinnati College of Medicine, Cincinnati, OH.
H. Gerry Taylor, Division of Developmental and Behavioral Pediatrics and Psychology, Department of Pediatrics, Case Western Reserve University and Rainbow Babies and Children’s Hospital, University Hospitals Case Medical Center, Cleveland, OH.
Keith Owen Yeates, Department of Pediatrics, The Ohio State University and Center for Biobehavioral Health, The Research Institute at Nationwide Children’s Hospital, Columbus, OH.
Nicolay C. Walz, Division of Behavioral Medicine and Clinical Psychology, Department of Pediatrics, Cincinnati Children’s Hospital Medical Center and University of Cincinnati College of Medicine, Cincinnati, OH.
Terry Stancin, Division of Pediatric Psychology, Department of Psychiatry, MetroHealth Medical Center and Case Western Reserve University, Cleveland, OH.
Shari L. Wade, Division of Physical Medicine and Rehabilitation, Department of Pediatrics, Cincinnati Children’s Hospital Medical Center and University of Cincinnati College of Medicine, Cincinnati, OH.
References
- 1.Bruns J, Jr, Hauser WA. The epidemiology of traumatic brain injury: A review. Epilepsia. 2003;44(Suppl 10):2–10. doi: 10.1046/j.1528-1157.44.s10.3.x. [DOI] [PubMed] [Google Scholar]
- 2.Faul M, Xu L, Wald MM, Coronado VG. [Accessed March 1, 2010];Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002–2006. Available at www.cdc.gov/TraumaticBrainInjury.
- 3.Jaffe KM, Fay GC, Polissar NL, et al. Severity of pediatric traumatic brain injury and early neurobehavioral outcome: A cohort study. Arch Phys Med Rehabil. 1992;73:540–547. [PubMed] [Google Scholar]
- 4.Jaffe KM, Polissar NL, Fay GC, Liao S. Recovery trends over three years following pediatric traumatic brain injury. Arch Phys Med Rehabil. 1995;76:17–26. doi: 10.1016/s0003-9993(95)80037-9. [DOI] [PubMed] [Google Scholar]
- 5.Taylor HG. Research on outcomes of pediatric traumatic brain injury: Current advances and future directions. Dev Neuropsychol. 2004;25:199–225. doi: 10.1080/87565641.2004.9651928. [DOI] [PubMed] [Google Scholar]
- 6.Massagli TL, Jaffe KM, Fay GC, Polissar NL, Liao S, Rivara JB. Neurobehavioral sequelae of severe pediatric traumatic brain injury: A cohort study. Arch Phys Med Rehabil. 1996;77:223–231. doi: 10.1016/s0003-9993(96)90102-1. [DOI] [PubMed] [Google Scholar]
- 7.Massagli TL, Michaud LJ, Rivara FP. Association between injury indices and outcome after severe traumatic brain injury in children. Arch Phys Med Rehabil. 1996;77:125–132. doi: 10.1016/s0003-9993(96)90156-2. [DOI] [PubMed] [Google Scholar]
- 8.Fay GC, Jaffe KM, Polissar NL, Liao S, Rivara JB, Martin KM. Outcome of pediatric traumatic brain injury at three years: A cohort study. Arch Phys Med Rehabil. 1994;75:733–741. [PubMed] [Google Scholar]
- 9.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116:1374–1382. doi: 10.1542/peds.2004-1728. [DOI] [PubMed] [Google Scholar]
- 10.Anderson VA, Catroppa C, Dudgeon P, Morse SA, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20:42–57. doi: 10.1037/0894-4105.20.1.42. [DOI] [PubMed] [Google Scholar]
- 11.Anderson VA, Morse SA, Catroppa C, Haritou F, Rosenfeld JV. Thirty month outcome from early childhood head injury: A prospective analysis of neurobehavioural recovery. Brain. 2004;127:2608–2620. doi: 10.1093/brain/awh320. [DOI] [PubMed] [Google Scholar]
- 12.Wassenberg R, Max JE, Lindgren SD, Schatz A. Sustained attention in children and adolescents after traumatic brain injury: Relation to severity of injury, adaptive functioning, ADHD and social background. Brain Inj. 2004;18:751–764. doi: 10.1080/02699050410001671775. [DOI] [PubMed] [Google Scholar]
- 13.Schachar R, Levin HS, Max JE, Purvis K, Chen S. Attention deficit hyperactivity disorder symptoms and response inhibition after closed head injury in children: Do preinjury behavior and injury severity predict outcome? Dev Neuropsychol. 2004;25:179–198. doi: 10.1080/87565641.2004.9651927. [DOI] [PubMed] [Google Scholar]
- 14.Max JE, Lansing AE, Koele SL, et al. Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol. 2004;25:159–177. doi: 10.1080/87565641.2004.9651926. [DOI] [PubMed] [Google Scholar]
- 15.Catroppa C, Anderson V. Children’s attentional skills 2 years post-traumatic brain injury. Dev Neuropsychol. 2003;23:359–373. doi: 10.1207/S15326942DN2303_3. [DOI] [PubMed] [Google Scholar]
- 16.Ewing-Cobbs L, Prasad MR, Landry SH, Kramer L, DeLeon R. Executive functions following traumatic brain injury in young children: A preliminary analysis. Dev Neuropsychol. 2004;26:487–512. doi: 10.1207/s15326942dn2601_7. [DOI] [PubMed] [Google Scholar]
- 17.Max JE, Schachar RJ, Levin HS, et al. Predictors of attention-deficit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. J Am Acad Child Adolesc Psychiatry. 2005;44:1032–1040. doi: 10.1097/01.chi.0000173293.05817.b1. [DOI] [PubMed] [Google Scholar]
- 18.Anderson P. Assessment and development of executive function (EF) during childhood. Child Neuropsychol. 2002;8:71–82. doi: 10.1076/chin.8.2.71.8724. [DOI] [PubMed] [Google Scholar]
- 19.Anderson VA, Anderson P, Northam E, Jacobs R, Catroppa C. Development of executive functions through late childhood and adolescence in an Australian sample. Dev Neuropsychol. 2001;20:385–406. doi: 10.1207/S15326942DN2001_5. [DOI] [PubMed] [Google Scholar]
- 20.Slomine BS, Gerring JP, Grados MA, et al. Performance on measures of executive function following pediatric traumatic brain injury. Brain Inj. 2002;16:759–772. doi: 10.1080/02699050210127286. [DOI] [PubMed] [Google Scholar]
- 21.Anderson V, Catroppa C. Recovery of executive skills following paediatric traumatic brain injury (TBI): A 2 year follow-up. Brain Inj. 2005;19:459–470. doi: 10.1080/02699050400004823. [DOI] [PubMed] [Google Scholar]
- 22.Catroppa C, Anderson V. A prospective study of the recovery of attention from acute to 2 years following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2005;11:84–98. doi: 10.1017/S1355617705050101. [DOI] [PubMed] [Google Scholar]
- 23.Muscara F, Catroppa C, Anderson V. Social problem-solving skills as a mediator between executive function and long-term social outcome following paediatric traumatic brain injury. J Neuropsychol. 2008;2:445–61. doi: 10.1348/174866407x250820. [DOI] [PubMed] [Google Scholar]
- 24.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Attentional and processing skills following traumatic brain injury in early childhood. Brain Inj. 2005;19:699–710. doi: 10.1080/02699050400025281. [DOI] [PubMed] [Google Scholar]
- 25.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 26.Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO, Minich NM. A prospective study of long-term caregiver and family adaptation following brain injury in children. J Head Trauma Rehabil. 2002;17:96–111. doi: 10.1097/00001199-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Rivara JB, Fay GC, Jaffe KM, Polissar NL, Shurtleff HA, Martin KM. Predictors of family functioning one year following traumatic brain injury in children. Arch Phys Med Rehabil. 1992;73:899–910. [PubMed] [Google Scholar]
- 28.Anderson VA, Catroppa C, Haritou F, Morse S, Rosenfeld JV. Identifying factors contributing to child and family outcome 30 months after traumatic brain injury in children. J Neurol Neurosurg Psychiatry. 2005;76:401–408. doi: 10.1136/jnnp.2003.019174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rivara JM, Jaffe KM, Polissar NL, Fay GC, Liao S, Martin KM. Predictors of family functioning and change 3 years after traumatic brain injury in children. Arch Phys Med Rehabil. 1996;77:754–764. doi: 10.1016/s0003-9993(96)90253-1. [DOI] [PubMed] [Google Scholar]
- 30.Rivara JB. Family functioning following pediatric traumatic brain injury. Pediatr Ann. 1994;23:38–44. doi: 10.3928/0090-4481-19940101-09. [DOI] [PubMed] [Google Scholar]
- 31.Stancin T, Wade SL, Walz NC, Yeates KO, Taylor HG. Family adaptation 18 months after traumatic brain injury in early childhood. J Dev Behav Pediatr. 2010;31:317–325. doi: 10.1097/DBP.0b013e3181dbaf32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stancin T, Wade SL, Walz NC, Yeates KO, Taylor HG. Traumatic brain injuries in early childhood: Initial impact on the family. J Dev Behav Pediatr. 2008;29:253–261. doi: 10.1097/DBP.0b013e31816b6b0f. [DOI] [PubMed] [Google Scholar]
- 33.Anderson VA, Catroppa C, Haritou F, et al. Predictors of acute child and family outcome following traumatic brain injury in children. Pediatr Neurosurg. 2001;34:138–148. doi: 10.1159/000056009. [DOI] [PubMed] [Google Scholar]
- 34.Rivara JB, Jaffe KM, Polissar NL, et al. Family functioning and children’s academic performance and behavior problems in the year following traumatic brain injury. Arch Phys Med Rehabil. 1994;75:369–379. doi: 10.1016/0003-9993(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 35.Rivara JB, Jaffe KM, Fay GC, et al. Family functioning and injury severity as predictors of child functioning one year following traumatic brain injury. Arch Phys Med Rehabil. 1993;74:1047–1055. doi: 10.1016/0003-9993(93)90060-n. [DOI] [PubMed] [Google Scholar]
- 36.Nadebaum C, Anderson V, Catroppa C. Executive function outcomes following traumatic brain injury in young children: A five year follow-up. Dev Neuropsychol. 2007;32:703–728. doi: 10.1080/87565640701376086. [DOI] [PubMed] [Google Scholar]
- 37.Chapman LA, Wade SL, Walz NC, Taylor HG, Stancin T, Yeates KO. Clinically significant behavior problems during the initial 18 months following early childhood traumatic brain injury. Rehabil Psychol. 2010;55:48–57. doi: 10.1037/a0018418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gerrard-Morris A, Taylor HG, Yeates KO, et al. Cognitive development after traumatic brain injury in young children. J Int Neuropsychol Soc. 2010;16:157–168. doi: 10.1017/S1355617709991135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010;24:345–356. doi: 10.1037/a0018387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;II:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 41.Byles J, Byrne C, Boyle MH, Offord DR. Ontario Child Health Study: Reliability and validity of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. 1988;27:97–104. doi: 10.1111/j.1545-5300.1988.00097.x. [DOI] [PubMed] [Google Scholar]
- 42.Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. J Marital Fam Ther. 1985;11:345–356. [Google Scholar]
- 43.Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO, Minich NM. Parent-adolescent interactions after traumatic brain injury: Their relationship to family adaptation and adolescent adjustment. J Head Trauma Rehabil. 2003;18:164–176. doi: 10.1097/00001199-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Robinson CC, Mandleco B, Olsen SF, Hart CH. Authoritative, authoritarian, and permissive parenting practices: Development of a new measure. Psychol Rep. 1995;77:819–830. [Google Scholar]
- 45.Baumrind D. Effects of authoritative parental control on child behavior. Child Development. 1966;37:887–907. [Google Scholar]
- 46.Baumrind D. Child care practices anteceding three patterns of pre-school behavior. Genet Psychol Monogr. 1967;75:43–88. [PubMed] [Google Scholar]
- 47.Gioia GA, Isquith PK. Ecological assessment of executive function in traumatic brain injury. Dev Neuropsychol. 2004;25:135–158. doi: 10.1080/87565641.2004.9651925. [DOI] [PubMed] [Google Scholar]
- 48.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function. Child Neuropsychol. 2000;6:235–238. doi: 10.1076/chin.6.3.235.3152. [DOI] [PubMed] [Google Scholar]
- 49.Gioia G, Espy KA, Isquith PK. Preschool Version. Lutz, FL: Psychological Assessment Resources Inc; 2003. BRIEF-P: Behavior Rating Inventory of Executive Function. [Google Scholar]
- 50.Gioia G, Isquith PK, Guy SC, Kenworthy L. BRIEF: Behavior Rating Inventory of Executive Function. Lutz, FL: Psychological Assessment Resources Inc; 2000. [Google Scholar]
- 51.Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 52.Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2000. [Google Scholar]
- 53.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. J Int Neuropsychol Soc. 2001;7:755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- 54.Josie KL, Peterson CC, Burant C, et al. Predicting family burden following childhood traumatic brain injury: A cumulative risk approach. J Head Trauma Rehabil. 2008;23:357–368. doi: 10.1097/01.HTR.0000341431.29133.a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Max JE, Schachar RJ, Levin HS, et al. Predictors of secondary attention-deficit/hyperactivity disorder in children and adolescents 6 to 24 months after traumatic brain injury. J Am Acad Child Adolesc Psychiatry. 2005;44:1041–1049. doi: 10.1097/01.chi.0000173292.05817.f8. [DOI] [PubMed] [Google Scholar]
- 56.Vriezen ER, Pigott SE. The relationship between parental report on the BRIEF and performance-based measures of executive function in children with moderate to severe traumatic brain injury. Child Neuropsychol. 2002;8:296–303. doi: 10.1076/chin.8.4.296.13505. [DOI] [PubMed] [Google Scholar]