Abstract
Desmoglein-1 (DSG1), a desmosomal protein, maintains the structure of epidermis through its adhesive function. However, heterozygous mutations in DSG1 in humans result in abnormal differentiation, as does downregulation of DSG1 in human skin organ culture, suggesting that it may have important signaling functions. In this issue of the JCI, Harmon et al. elucidate how the binding of the DSG1 cytoplasmic tail to the scaffolding protein Erbin decreases signaling through the Ras-Raf pathway to promote stratification and differentiation of keratinocytes in the epidermis.
Introduction
In an era of research budget cuts and tightened paylines, the significance and translational potential of grant proposals are sometimes equated with the prevalence of the disease being studied and/or the obvious clinical application of the proposal. However, it is important to remember that we have learned a tremendous amount about the normal physiology and pathophysiology of organs through the study of rare diseases and through studies of the basic cell biology of seemingly boring (that is, uncommunicative) structural molecules. In this Commentary, we will illustrate this observation by tracing recent studies centered on desmoglein-1 (DSG1) and its associated diseases.
The discovery of DSG1
The family of desmogleins was characterized in the early 1990s through biochemical isolation, monoclonal antibody production, and then expression cloning, which showed they were in the supergene family of cadherins. Because desmogleins were present in the electron lucent center of the desmosome, a cell adhesion structure, and were in the cadherin family of adhesion molecules, they were presumed to function in cell-cell adhesion (1). In fact, “desmoglein” is composed of the Greek words “desmos” for “tie” and “glein” for “glue-like.” Whereas DSG2 was found in all desmosome-possessing tissues, including nonepithelial myocardium, expression of the family members DSG1 and DSG3 was mainly limited to the epidermis and mucosa (2).
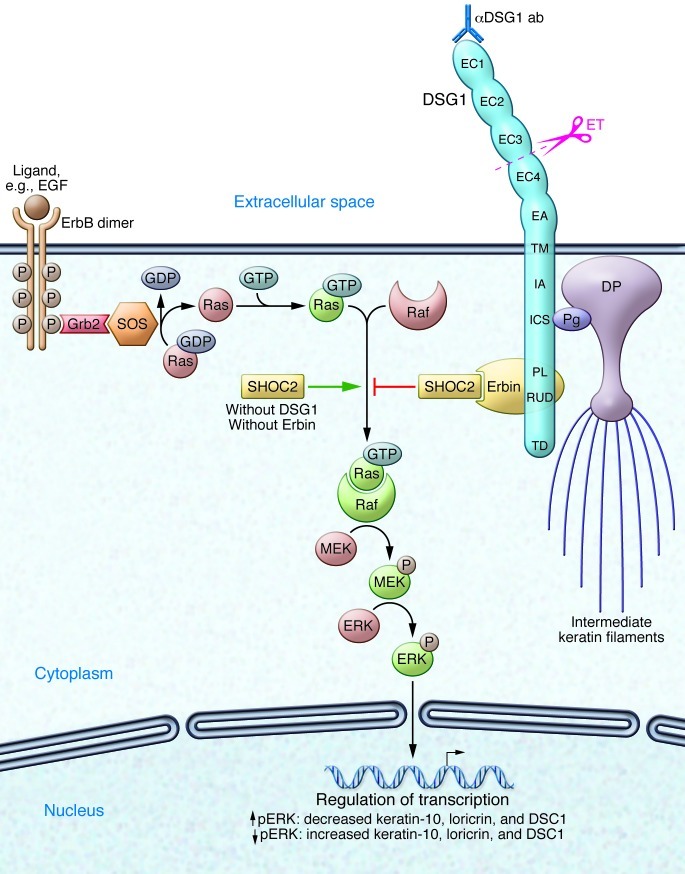
Molecular cloning also indicated that the desmoglein cytoplasmic tail had one segment with homology to that of classical cadherins. This segment binds the armadillo protein plakoglobin, an interaction thought to be important in desmosome assembly through cobinding of plakoglobin (and perhaps other armadillo proteins) to desmoplakin, the major desmosome plaque protein (refs. 3–5 and Figure 1). Desmogleins also have unique intracellular segments (6), the functions of which have now been partially elucidated by Harmon et al. (7) in this issue of the JCI.
Figure 1. Keratinocyte structure, adhesion, and signaling modulated by Erbin and/or DSG1.
The ErbB family includes four receptors with tyrosine kinase activity (ErbB1 [also known as EGFR], ErbB2, ErbB3, ErbB4), which form homodimers and/or heterodimers upon ligand binding. Autophosphorylation leads to direct activation of the PI3K or phospholipase C-γ pathway (not shown). Via adaptor proteins (e.g., Grb2), the guanyl nucleotide exchange factor son of sevenless (SOS) allows exchange of GDP for GTP on Ras and thus activation of this small GTPase. The scaffolding protein SHOC2 accelerates formation of Ras/Raf complexes and leads, in absence of DSG1 and/or Erbin, to activation of the Raf/MEK/ERK pathway, which inhibits differentiation of keratinocytes. In the presence of DSG1, the scaffolding protein Erbin skews the fate of keratinocytes toward differentiation by binding SHOC2 and inhibiting formation of Ras/Raf complexes. Erbin binds to the cytoplasmic tail of DSG1 but not to the intracellular cadherin-like sequence (ICS) that binds plakoglobin (Pg), a protein important for desmosome integrity and function. ET from Staphylococcus aureus cleaves DSG1 between extracellular domain 3 (EC3) and EC4. Anti-DSG1 autoantibodies (αDSG1 ab) mediating PF predominantly target N-terminal extracellular domains, causing loss of cell-cell adhesion. DP, desmoplakin; EC1–EC4, extracellular domains of DSG1; EA, extracellular anchor (also known as EC5); TM, transmembrane domain; IA, intracellular anchor; PL, proline-rich linker; RUD, repeat unit domains; TD, terminal domain; DSC1, desmocollin-1.
The rare autoimmune blistering skin disease pemphigus foliaceus elucidates the adhesive function of DSG1
At about the same time that desmogleins were being characterized, the antigen of a rare autoimmune blistering skin disease, pemphigus foliaceus (PF), was described as a glycoprotein of about the same molecular weight as that of DSG1. Immunochemical studies indicated that the autoantigen was indeed DSG1 (8), and further studies have shown that the autoantibodies, even as monovalent cloned single chain variable fragments from patients (9), can cause loss of cell adhesion in the superficial epidermis where DSG1 is highly expressed. Thus, the study of a rare dermatologic disease demonstrated the critical function of DSG1 in cell adhesion and maintenance of the structure of the normal epidermis.
The work on PF and DSG1 provided insight into the pathophysiology of a much more common disease, bullous impetigo, as well as the related disease staphylococcal scalded skin syndrome, both of which are significant causes of morbidity in children (8). These infectious diseases, known to be associated with the production of a staphylococcal toxin called exfoliative toxin (ET), are characterized by blisters in the superficial epidermis due to loss of cell-cell adhesion with identical histology to that of PF. The crystal structure of ET suggested that it was a serine protease with a specific receptor; however, that receptor remained unknown for many years. The data that indicated that anti-DSG1 antibodies cause loss of cell adhesion in PF suggested that the specific receptor for ET was likely DSG1 as well, because loss of function of DSG1 either by antibody binding or enzymatic cleavage resulted in the same phenotypic blister. Indeed, that conclusion was confirmed when it was shown that ET cleaved DSG1 (but not DSG3 or E-cadherin) at one specific peptide bond (8).
However, throughout this work, which has been so important for understanding the structure of the epidermis and diseases that perturb it, DSG1 has been considered basically as a structural adhesion molecule.
DSG1 is more than a structural molecule — hints from cell biologic studies of desmogleins and a rare disease
Perturbations of desmoglein expression in the epidermis have been shown to do more than affect cell adhesion. For example, misexpression of DSG3 in the superficial epidermis not only allows increased adhesion in those layers (10) but also affects differentiation, resulting in an abnormal stratum corneum, resembling that of mucous membranes, that allows increased transepidermal water loss (11). Similarly, misexpression of DSG2 in epidermis results in increased proliferation in the suprabasilar layers (12).
DSG1 is uniquely positioned, just above the basal layer, to be a candidate to direct stratification and/or differentiation of epidermis. A recent elegant study in which DSG1 was downregulated in skin organ culture confirmed the importance of DSG1 for directing those functions (13). In this study, DSG1 knockdown activated EGF receptor/ErbB2 (EGFR/ErbB2) signaling. Specific blockade of activation of ERK1/2, downstream of one of the arms of this activated receptor, restored epidermal differentiation in DSG1-knockdown cells. DSG1-mediated adhesion was not needed for this effect and neither was plakoglobin binding, but localization at the cell membrane was necessary.
Consideration of the rare genetic disease striate palmoplantar keratoderma (SPPK; OMIM 148700), which is caused by a heterozygous mutation in the DSG1 gene (14), lends further support to the notion that DSG1 affects not only adhesion but also differentiation. Patients with SPPK show a striate (or more diffuse) keratoderma of the palms and soles. Histological and ultrastructural analyses reveal not only widening of cell-cell spaces and small desmosomes (consistent with decreased adhesion) but also marked thickening of the palmoplantar epidermis with abnormal differentiation (15).
Molecular mechanisms of DSG1-mediated modulation of keratinocyte differentiation
In order to address the molecular mechanisms of how DSG1 might modulate differentiation, Harmon et al. (7) hypothesized that heretofore uncharacterized binding partners of the desmoglein-unique domains were involved. Using yeast two-hybrid screening, they found that the cytoplasmic domains of DSG1 carboxy-terminal to the plakoglobin-binding domain bound Erbin, a molecular scaffolding protein known to redistribute to the cell surface of keratinocytes during differentiation (16). Harmon et al. confirmed this redistribution and showed that Erbin colocalized with DSG1 in the differentiating epidermis. Genetic downregulation of Erbin decreased expression of various keratinocyte differentiation markers in organ culture and at the same time increased pERK; conversely, pharmacologic blockade of ERK phosphorylation restored differentiation. The authors then hypothesized that peripheral localization of Erbin may bring it into contact with SHOC2, inhibiting the ability of SHOC2 to form Ras-Raf complexes upstream of ERK (17). Indeed, Harmon et al. found that only when DSG1 brings Erbin to the cell membrane does it interfere with the binding of Ras to the SHOC2 protein (7). To explain these findings, Harmon et al. proposed an elegant model in which, in the presence of DSG1, SHOC2-Erbin complexes form at the expense of SHOC2-Ras complexes, thus decreasing ERK activation and driving differentiation of keratinocytes (Figure 1). With a very creative approach, the authors then confirmed that their model was relevant to the pathophysiology of SPPK. Proximity ligation analysis demonstrated that patients with SPPK (with genetically decreased DSG1 expression), in contrast to healthy controls, have increased SHOC2-Ras complexes, compared with SHOC2-Erbin complexes. As hypothesized, this leads to increased pERK levels and decreased expression of differentiation markers (7).
If SPPK is due to elevated Ras activity, one would predict that other genetic diseases in which Ras pathways are activated should show similar clinical findings on the palms and soles. In fact, they do: in the group of rare genetic diseases of the Ras/MEK/ERK pathway (sometimes called RASopathies), palmar and plantar keratoderma is found in about 76% of patients with Costello syndrome and in about 36% of patients with cardio-facio-cutaneous syndrome (which overlaps genetically and phenotypically with Noonan’s syndrome) (18, 19).
Loose ends
Although Harmon et al. present a beautiful story that explains some aspects of epidermal homeostasis and the molecular pathophysiology of SPPK, there are many questions that remain. In addition to DSG1, there are several desmogleins (as well as other cadherin superfamily members) expressed in epidermis and mucous membranes at various levels. How do the tails of these molecules regulate epidermal homeostasis? What are their binding partners? How do other binding partners of DSG1, for example, plakoglobin and other catenins and armadillo proteins, affect signaling and differentiation? In addition, it is unclear how mutations in keratins or in other desmosomal components, such as desmoplakin, cause SPPK (20).
Finally, desmosomes may be important in tumor suppression, and modulation of signaling through desmosomal cadherin binding proteins, including Erbin, may be critical to that function (16, 21). For example, the most common malignant neoplasm of skin, basal cell carcinoma, shows diminished cell surface DSG1 and cytoplasmic localization of Erbin (16, 22), suggesting that the mechanism proposed by Harmon et al. might be active in maintaining its lack of differentiation.
These and other interesting issues await further study. However, it is very clear that desmosomes and desmogleins are not only structural regulators of adhesion in the epidermis but also are key regulators of signal transduction that in turn affect differentiation and epidermal homeostasis as well as being involved in carcinogenesis. These insights were originally gained from studies of rare diseases and from creative cell biological studies that looked beyond the structural role of desmosomal proteins. Applying these new insights will suggest promising new targets for therapy of rare and more common skin diseases.
Acknowledgments
This work was supported by a grant from the NIAMS, NIH (R01-AR052672) to J.R. Stanley and by a research scholarship from the DFG (HA6736/1-1) to C.M. Hammers.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2013;123(4):1419–1422. doi:10.1172/JCI69071.
See the related article beginning on page 1556.
References
- 1.Steinberg MS, Shida H, Giudice GJ, Shida M, Patel NH, Blaschuk OW. On the molecular organization, diversity and functions of desmosomal proteins. Ciba Found Symp. 1987;125:3–25. doi: 10.1002/9780470513408.ch2. [DOI] [PubMed] [Google Scholar]
- 2.Schafer S, Koch PJ, Franke WW. Identification of the ubiquitous human desmoglein, Dsg2, and the expression catalogue of a subfamily of desmosomal cadherins. Exp Cell Res. 1994;211(2):391–399. doi: 10.1006/excr.1994.1103. [DOI] [PubMed] [Google Scholar]
- 3.Bornslaeger EA, et al. Plakophilin 1 interferes with plakoglobin binding to desmoplakin, yet together with plakoglobin promotes clustering of desmosomal plaque complexes at cell-cell borders. J Cell Sci. 2001;114(pt 4):727–738. doi: 10.1242/jcs.114.4.727. [DOI] [PubMed] [Google Scholar]
- 4.Korman NJ, Eyre RW, Klaus-Kovtun V, Stanley JR. Demonstration of an adhering-junction molecule (plakoglobin) in the autoantigens of pemphigus foliaceus and pemphigus vulgaris. N Engl J Med. 1989;321(10):631–635. doi: 10.1056/NEJM198909073211002. [DOI] [PubMed] [Google Scholar]
- 5.Kowalczyk AP, et al. The head domain of plakophilin-1 binds to desmoplakin and enhances its recruitment to desmosomes. Implications for cutaneous disease. J Biol Chem. 1999;274(26):18145–18148. doi: 10.1074/jbc.274.26.18145. [DOI] [PubMed] [Google Scholar]
- 6.Koch PJ, Franke WW. Desmosomal cadherins: another growing multigene family of adhesion molecules. Curr Opin Cell Biol. 1994;6(5):682–687. doi: 10.1016/0955-0674(94)90094-9. [DOI] [PubMed] [Google Scholar]
- 7.Harmon RM, et al. Desmoglein-1/Erbin interaction suppresses ERK activation to support epidermal differentiation. J Clin Invest. 2013;123(4):1556–1570. doi: 10.1172/JCI65220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stanley JR, Amagai M. Pemphigus, bullous impetigo, and staphylococcal scalded skin syndrome. N Engl J Med. 2006;355(17):1800–1810. doi: 10.1056/NEJMra061111. [DOI] [PubMed] [Google Scholar]
- 9.Ishii K, Lin C, Siegel DL, Stanley JR. Isolation of pathogenic monoclonal anti-desmoglein 1 human antibodies by phage display of pemphigus foliaceus autoantibodies. J Invest Dermatol. 2008;128(4):939–948. doi: 10.1038/sj.jid.5701132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu H, et al. Protection of neonates against pemphigus foliaceus by desmoglein 3. N Engl J Med. 2000;343(1):31–35. doi: 10.1056/NEJM200007063430105. [DOI] [PubMed] [Google Scholar]
- 11.Elias PM, et al. Desmoglein isoform distribution affects stratum corneum structure and function. J Cell Biol. 2001;153(2):243–249. doi: 10.1083/jcb.153.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brennan D, et al. Suprabasal Dsg2 expression in transgenic mouse skin confers a hyperproliferative and apoptosis-resistant phenotype to keratinocytes. J Cell Sci. 2007;120(pt 5):758–771. doi: 10.1242/jcs.03392. [DOI] [PubMed] [Google Scholar]
- 13.Getsios S, et al. Desmoglein 1-dependent suppression of EGFR signaling promotes epidermal differentiation and morphogenesis. J Cell Biol. 2009;185(7):1243–1258. doi: 10.1083/jcb.200809044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rickman L, et al. N-terminal deletion in a desmosomal cadherin causes the autosomal dominant skin disease striate palmoplantar keratoderma. Hum Mol Genet. 1999;8(6):971–976. doi: 10.1093/hmg/8.6.971. [DOI] [PubMed] [Google Scholar]
- 15.Wan H, et al. Striate palmoplantar keratoderma arising from desmoplakin and desmoglein 1 mutations is associated with contrasting perturbations of desmosomes and the keratin filament network. Br J Dermatol. 2004;150(5):878–891. doi: 10.1111/j.1365-2133.2004.05996.x. [DOI] [PubMed] [Google Scholar]
- 16.Lebeau S, et al. Comparative analysis of the expression of ERBIN and Erb-B2 in normal human skin and cutaneous carcinomas. Br J Dermatol. 2005;152(6):1248–1255. doi: 10.1111/j.1365-2133.2005.06687.x. [DOI] [PubMed] [Google Scholar]
- 17.Matsunaga-Udagawa R, et al. The scaffold protein Shoc2/SUR-8 accelerates the interaction of Ras and Raf. J Biol Chem. 2010;285(10):7818–7826. doi: 10.1074/jbc.M109.053975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siegel DH, Mann JA, Krol AL, Rauen KA. Dermatological phenotype in Costello syndrome: consequences of Ras dysregulation in development. Br J Dermatol. 2012;166(3):601–607. doi: 10.1111/j.1365-2133.2011.10744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nava C, et al. Cardio-facio-cutaneous and Noonan syndromes due to mutations in the RAS/MAPK signalling pathway: genotype-phenotype relationships and overlap with Costello syndrome. J Med Genet. 2007;44(12):763–771. doi: 10.1136/jmg.2007.050450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGrath JA. Inherited disorders of desmosomes. Australas J Dermatol. 2005;46(4):221–229. doi: 10.1111/j.1440-0960.2005.00188.x. [DOI] [PubMed] [Google Scholar]
- 21.Dusek RL, Attardi LD. Desmosomes: new perpetrators in tumour suppression. Nat Rev Cancer. 2011;11(5):317–323. doi: 10.1038/nrc3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tada H, Hatoko M, Tanaka A, Kuwahara M, Muramatsu T. Expression of desmoglein I and plakoglobin in skin carcinomas. J Cutan Pathol. 2000;27(1):24–29. doi: 10.1034/j.1600-0560.2000.027001024.x. [DOI] [PubMed] [Google Scholar]