Summary
SPICE, or K2, encompasses preparations of synthetic cannabinoids marketed as incense products, bath additives, and air fresheners and used for recreational purposes. These preparations are usually smoked for their cannabis-like effects and do not appear on routine urine toxicology screens. We report four cases of oliguric AKI associated with SPICE use in previously healthy men. All showed improvement in renal function without need for renal replacement therapy. Renal biopsy, performed in three of the patients, revealed acute tubular necrosis. The close temporal and geographic associations between the clinical presentation and the development of AKI strongly suggest an association between these SPICE preparations and AKI. Further investigations are required to identify the potential nephrotoxic agent(s). Nephrotoxicity from designer drugs should be included in the differential diagnosis of AKI, especially in young adults with negative urine drug screens.
Introduction
Synthetic cannabinoids have been marketed as various herbal mixtures over the past few years, often sold as incense products, bath additives, and air fresheners (1). Various terms have been used for these preparations, including SPICE, K2, and SPICE GOLD (1,2). These preparations are more potent and bind more avidly than cannabis to the cannabis receptors in the brain. They are distributed in the form of dried leaves, resin, or powder and are typically a mixture of synthetic cannabinoids and herbal additives. The mixture is typically smoked in a pipe or “hookah,” although inhalation and ingestion have also been described (1). Most users are young adults, with the desire to experience cannabis-like effects with a substance that cannot be detected on routine drug tests. The relatively low cost, about $20 USD per gram, is another reason for its popularity in the younger age group (2).
The use of these synthetic cannabinoid preparations has increased significantly in the United States over the past few years, with 567 cases being reported by poison control centers in 41 states during the first half of 2010 compared with a total of 13 calls in the whole year of 2009 (2). In another recent study, 1898 exposures to synthetic cannabinoids were reported to the National Poison Data System between January 1, 2010 and October 1, 2010 (3). In a survey of University of Florida students, 8% admitted to the use of K2 on at least one occasion (4). Well-recognized ill effects of these preparations of synthetic cannabinoids include impaired cognition in the immediate period after use, and long-term effects of dependence and withdrawal (2,5). Recently, three cases of acute coronary syndrome associated with spice use were reported in young participants (6). Tachycardia and seizures have also been reported (3). These adverse effects are not what would be anticipated with a pure synthetic cannabinoid. Given the nature of these synthetic drugs and how they are sold, it is likely that the preparations are adulterated with other compounds, which may have toxic effects. We report four cases of AKI associated with SPICE use (Table 1).
Table 1.
Clinical features and pertinent findings of the four patients
| Patient | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Age (yr) | 20 | 23 | 26 | 30 |
| Clinical features | Nausea, vomiting × 2 d | Nausea, vomiting × 2 d | Nausea, vomiting, diarrhea × 2 d | Nausea, vomiting, diarrhea × 3 d |
| Admission creatinine | 9.3 | 7.6 | 8.7 | 3.2 |
| Peak creatinine | 13.7 | 15.2 | 13.3 | 3.2 |
| Discharge creatinine | 2.9 | 11.5 | 8.6 | 2.4 |
| Renal biopsy | ATN | ATN | ATN | Not done |
| Proteinuria | 3.2a | 1.0a | 0.25b | None |
| Urine drug screen | Negative | Negative | Negative | Negative |
| White blood cell count (103/mm3) | 12.4 | 11.9 | 12.3 | 8.1 |
| Hemoglobin (g/dl) | 13.0 | 12.9 | 12.0 | 16.8 |
| Serum calcium (mg/dl) | 8.1 | 8.6 | 8.3 | 9.0 |
| Serum phosphorus (mg/dl) | 9.5 | 7.3 | 6.9 | 3.7 |
| Creatine phosphokinase (U/L) | 357 | 173 | Not done | 144 |
Serologies including antinuclear antibody, ANCA, anti-glomerular basement membrane, viral hepatitis panel, and HIV were negative in all four patients. ATN, acute tubular necrosis.
Proteinuria measured in grams/gram of creatinine on a spot urine collection.
Proteinuria measured in grams/gram of creatinine in a 24-hour collection.
Case 1
A 20-year-old man without prior medical problems presented to the University of Alabama at Birmingham (UAB) Hospital with nausea and vomiting for 2 days. His symptoms resolved within a few hours of admission. His BP was 130/66 without orthostatic changes; his pulse was 54 beats per minute. His physical examination was unremarkable. A serum chemistry panel showed the following results: sodium, 137 mEq/L; potassium, 3.1 mEq/L; bicarbonate, 25 mEq/L; urea nitrogen, 48 mg/dl; creatinine, 9.3 mg/dl; and albumin, 3.8 mg/dl. Other admission laboratory results are summarized in Table 1. Urinalysis (done by a nephrologist) showed specific gravity of 1.012, 3+ protein, trace glucose, and 6–10 white blood cells per high-power field with no red cells or eosinophils. Occasional muddy brown casts were observed. The spot urine protein/creatinine ratio was 3.2 g/g. A urine toxicology screen was negative. Antinuclear antibody (ANA), ANCA, anti-glomerular basement membrane (GBM) antibody, hepatitis screens, and HIV antibody screen were negative. The renal ultrasound was unremarkable.
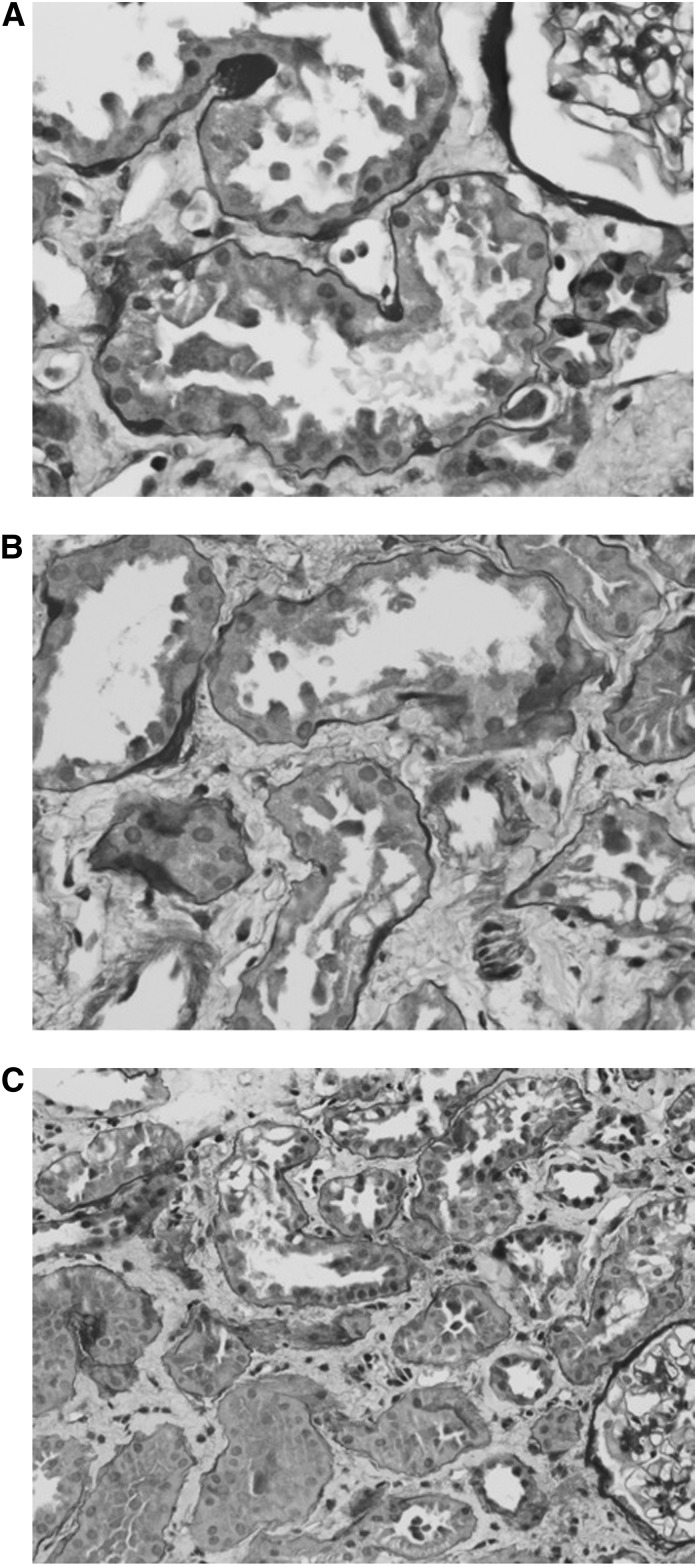
The patient denied use of any obvious nephrotoxic medications. There was no evidence of infection, and he was never hypotensive. Upon further questioning, the patient admitted to using SPICE over the prior few weeks. His renal function worsened, with a creatinine of 11.3 mg/dl despite aggressive volume repletion over the next 3 days. A renal biopsy revealed mild multifocal acute tubular injury, with tubular dilation, tubular epithelial cell vacuolization, sloughing, and apical blebbing (Figure 1A). There were rare nonspecific calcium oxalate crystals. The glomeruli and the blood vessels were unremarkable, and no immune complex deposits were identified. The patient had oliguric AKI, with a peak serum creatinine of 13.7 mg/dl. He did not require renal replacement therapy. He started to recover renal function and was discharged home with a serum creatinine of 2.9 mg/dl. Attempts to obtain a serum creatinine level after discharge have been unsuccessful.
Figure 1.
Pathologic features of AKI associated with SPICE. (A) Injured proximal tubular epithelial cells show apical blebbing from the surface and cytoplasmic vacuolization. Rare intraluminal detached necrotic tubular epithelial cells are also present. These findings are indicative of acute tubular injury. (B) Proximal tubular dilation with epithelial cell vacuolization and apical blebbing. Areas of denuded tubular basement membranes indicating focal epithelial cell loss are also identified. There is also accompanying interstitial edema. (C) The morphologic features of acute tubular injury are similar to the first two patients. All stained with periodic acid–Schiff. Original magnification, ×400 in A and B; ×200 in C.
Case 2
A 23-year-old man with no chronic medical illnesses presented to UAB Hospital with a 2-day history of nausea and vomiting. The patient had been consuming SPICE for a few years, and reported an increase in the amount and frequency of use over the few weeks prior to admission. On presentation, his BP was 125/73; his pulse was 52 beats per minute with no evidence of orthostasis. Admission laboratory tests revealed a BUN of 40 mg/dl and serum creatinine of 7.6 mg/dl. His serum phosphorus, calcium, creatine phosphokinase, and hemogram are summarized in Table 1. Liver function tests were within normal limits. His urinalysis showed 2+ protein, no white blood cells, and 25 red blood cells. Urinalysis, performed by the nephrology team, was unrevealing, with occasional granular casts, but no muddy brown casts or red cell casts. His spot urine protein/creatinine ratio was 1.0 g/g. Urine toxicology screen, viral hepatitis screen, HIV screen, ANCA, ANA, and dsDNA were negative, and serum complements were normal. His renal ultrasound was within normal limits. His urine output was 470 ml/24 h on the second day of hospitalization.
His renal function continued to worsen despite aggressive intravenous fluids. A kidney biopsy revealed mild acute tubular injury and few calcium oxalate crystals, features similar to those observed in case 1 (Figure 1B). The patient had oliguric AKI and his serum creatinine peaked at 15.2 mg/dl. He did not require dialysis and his renal function improved spontaneously. His serum creatinine was 11.5 mg/dl at discharge. A follow-up serum creatinine several weeks later was 0.8 mg/dl.
Case 3
A 26-year-old man with a past medical history of depression presented to a community hospital with complaints of nausea, vomiting, diarrhea, and lower abdominal pain for 2 days. He admitted to using SPICE over the past 2 years, but had used a “different supplier” over the previous week. His BP was 130/70; his pulse was 64 beats per minute, with no evidence of orthostasis. His initial serum creatinine was 2.1 mg/dl. He was transferred to UAB Hospital with a BUN of 34 mg/dl and serum creatinine of 8.7 mg/dl. Other laboratory results are summarized in Table 1. His urinalysis revealed 3+ blood, 3+ leukocyte esterase, 3+ protein, 26–50 white blood cells per high-power field, and >25 red blood cells per high-power field; no casts were seen. A 24-hour urine collection contained 245 mg of protein. His urine toxicology screen was negative. His viral hepatitis screen, HIV screen, ANCA, ANA, and dsDNA were negative and complements were normal. His renal ultrasound showed normal-sized kidneys and no hydronephrosis. Urine output was 200 ml/24 h on the first day of hospitalization at UAB.
A renal biopsy revealed acute tubular injury similar to biopsies in patients 1 and 2 (Figure 1C). He had oliguric AKI with a peak creatinine of 13.3 mg/dl. He did not require renal replacement therapy and his renal function improved spontaneously. His serum creatinine at discharge was 8.6 mg/dl. We have not been able to obtain the results of a serum creatinine after discharge.
Case 4
A 30-year-old man with hypertension presented to a local emergency room with a 3-day history of nausea, vomiting, diarrhea, and abdominal pain. He admitted to using SPICE over the past year, with a change in his supplier a few weeks earlier. He was transferred to UAB because of AKI that worsened despite intravenous fluids at the local hospital. His initial BP and pulse at our institution were 141/103 and 82 beats/min, respectively, with no evidence of orthostasis. His initial serum creatinine was 3.2 mg/dl; other laboratory data are summarized in Table 1. His urinalysis per the nephrology team was essentially normal with no evidence of casts or proteinuria. His urine toxicology screen, viral hepatitis screen, HIV screen, ANCA, ANA, and dsDNA were negative and serum complements were normal. A renal ultrasound revealed normal-sized kidneys with no hydronephrosis. Urine output was 2.6 L/24 h on day 1 of hospitalization at UAB. A kidney biopsy was not performed, because his renal function had improved within a day of admission. We have no follow-up serum creatinine.
Discussion
We present the cases of four young adults who presented to our institution with symptoms of nausea, vomiting, and abdominal pain after using SPICE. Three of the four patients had severe oliguric AKI. All four had improvement of renal function without specific treatment, and none required renal replacement therapy. The three patients who underwent renal biopsy had acute tubular necrosis (ATN). The fourth patient seemed to have prerenal AKI based on his clinical presentation and faster recovery after volume resuscitation. The common history of SPICE ingestion is suggestive but not conclusive evidence of a possible pathogenic role of the SPICE preparation in these patients’ AKI. All four patients were from the same community in Northeast Alabama and all were admitted to UAB within a 9-week period. The temporal and geographic clustering of the cases is consistent with a common toxic exposure.
An extensive electronic search of the medical literature failed to reveal previous reports of SPICE-associated AKI. However, an article in a local newspaper reported 30 cases of AKI among SPICE users from the same geographic area as our patients (7). Another newspaper reported a cluster of 14 cases of AKI among SPICE users in Casper, Wyoming (8). Because SPICE is not detected in routine urine drug screens, it is possible that similar “epidemics” in other geographic areas have gone undetected.
Unfortunately, we have not been able to obtain a sample of the SPICE involved, and the serum and urine of the patients had been discarded by the time of our review, precluding further analytical investigation. This is a major limitation in the interpretation of our observations. In addition, although there seems to be a suggestion for association between use of SPICE preparations and AKI based on our description of these four cases, it is hard to argue for a causative role of the SPICE preparations in AKI considering the small number of patients, the lack of specific biopsy findings, and the limited data available at this point in time.
The pathogenic mechanism of ATN in these patients remains elusive. The creatine phosphokinase levels were only mildly elevated, making rhabdomyolysis an unlikely etiology. Although serum uric acid levels were not measured, there was no evidence of acute uric acid nephropathy (i.e., no uric acid crystals were seen on urinalysis or in the biopsies). The oxalate crystals seen in two of the biopsies may be a nonspecific finding, or may represent a metabolic by-product of the nephrotoxin. Given that SPICE preparations are derived from products such as incense and air fresheners, they may be contaminated with heavy metals. The patchy nature of the tubular injury favors an ischemic related injury over toxin. The history of nausea, vomiting, and abdominal pain is most consistent with ischemic ATN secondary to hypovolemia, although this hypothesis is unsettling in that the patients did not appear to be severely hypovolemic on arrival at UAB. It is very likely that other compounds, including a possible nephrotoxin, adulterated the preparation used by our patients. There is very little information regarding the ingredients in SPICE and other synthetic cannabinoids that are sold on the streets, although it is known that additional compounds may be added in an attempt to enhance the euphoria.
Adebamiro and Perazella recently reported a case of recurrent AKI due to repeated use of “bath salts,” a pyrrolidineopropiophenone derivative designed to simulate the effects of amphetamines and cocaine, but undetectable by routine drug screens (9). The patient’s clinical course was thought to be consistent with ATN. As in our patients, no drug was available for analysis.
The last 5 years have seen a dramatic increase in the use of “designer drugs” such as SPICE, both globally and in the United States. The users are typically young adults, and the inability of routine drug tests to detect the synthetic cannabinoids adds to the appeal of these preparations. Despite legislation against the use of these preparations in 40 states, the use of these mixtures is increasing. This is partly because newer synthetic preparations that are not covered by legislation continue to be made and are available on the streets sometimes days after the legislation against prior preparations is introduced. It is important to include nephrotoxicity from designer drugs such as SPICE and bath salts in the differential diagnosis of AKI, especially in young patients with negative urine drug screens. Increased awareness may ultimately lead to identifications of the nephrotoxin(s).
Disclosures
None.
Acknowledgments
We acknowledge the UAB-UCSD O’Brien Center for Acute Kidney Injury Research (P30 DK079337) for helpful discussions.
Data from this article were published in abstract form at Kidney Week, San Diego, CA, October 30–November 4, 2012.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Fattore L, Fratta W: Beyond THC: The new generation of cannabinoid designer drugs. Front Behav Neurosci 5: 60, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson LA, Johnson RL, Alfonzo C: Spice: A legal marijuana equivalent. Mil Med 176: 718–720, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Hoyte CO, Jacob J, Monte AA, Al-Jumaan M, Bronstein AC, Heard KJ: A characterization of synthetic cannabinoid exposures reported to the National Poison Data System in 2010. Ann Emerg Med 60: 435–438, 2012 [DOI] [PubMed] [Google Scholar]
- 4.Hu X, Primack BA, Barnett TE, Cook RL: College students and use of K2: An emerging drug of abuse in young persons. Subst Abuse Treat Prev Policy 6: 16, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Müller H, Sperling W, Köhrmann M, Huttner HB, Kornhuber J, Maler J-M: The synthetic cannabinoid Spice as a trigger for an acute exacerbation of cannabis induced recurrent psychotic episodes. Schizophr Res 118: 309–310, 2010 [DOI] [PubMed] [Google Scholar]
- 6.Mir A, Obafemi A, Young A, Kane C: Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics 128: e1622–e1627, 2011 [DOI] [PubMed]
- 7.Rogers L: Spiked Spice sickening users in DeKalb County. The Gadsden Times May 11, 2012. Available at: http://www.gadsdentimes.com/article/20120511/NEWS/120519988 Accessed June 4, 2012
- 8.Morton T: Wyoming 'spice' smokers hospitalized with potential kidney failure. Casper Star-Tribune March 2, 2012. Available at: http://http://trib.com/news/local/casper/wyoming-spice-smokers-hospitalized-with-potential-kidney-failure/article_37639432-164f-52dc-9c58-c5f27b2b6224.html Accessed June 1, 2012
- 9.Adebamiro A, Perazella MA: Recurrent acute kidney injury following bath salts intoxication. Am J Kidney Dis 59: 273–275, 2012 [DOI] [PubMed] [Google Scholar]