Abstract
Humanitarian assistance standards require specific attention to address the reproductive health (RH) needs of conflict-affected populations. Despite these internationally recognised standards, access to RH services is still often compromised in war. We assessed the effectiveness of our programme in northern Uganda to provide family planning (FP) services through mobile outreach and public health centre strengthening. Baseline (n = 905) and endline (n = 873) cross-sectional surveys using a multistage cluster sampling design were conducted in the catchment areas of four public health centres in 2007 and 2010. Current use of any modern FP method increased from 7.1% to 22.6% (adjusted odds ratio [OR] 3.34 [95% confidence interval (CI) 2.27–4.92]); current use of long-acting and permanent methods increased from 1.2% to 9.8% (adjusted OR 9.45 [95%CI 3.99–22.39]). The proportion of women with unmet need for FP decreased from 52.1% to 35.7%. This study demonstrates that when comprehensive FP services are provided among conflict-affected populations, women will choose to use them. The combination of mobile teams and health systems strengthening can make a full range of methods quickly available while supporting the health system to continue to provide those services in challenging and resource-constrained settings.
Keywords: family planning, war, Uganda, humanitarian aid, reproductive health
Introduction
Complex humanitarian emergencies caused by armed conflict can devastate national health systems as health workers flee and infrastructure is destroyed (Kruk et al. 2010). The negative impact of war and displacement on women has long been recognised, compromising their right to reproductive health (RH) services (Al Gasseer et al. 2004, Austin et al. 2008). Although research indicates that fertility preferences among conflict-affected populations are mixed (McGinn 2000), studies show that demand for spacing or limiting births is present, as in any population (McGinn et al. 2004, 2011, Austin et al. 2008). The United Nations International Conference on Population and Development in 1994 specifically recognised the right to RH, including family planning (FP), of refugees and internally displaced people (IDP); humanitarian assistance standards now require specific attention to address RH needs of conflict-affected populations (Sphere Project 2011, United Nations 1994, 2011).
Despite this increased recognition of the importance of RH, 9 of the 10 countries with the highest maternal mortality ratios in the world are affected by conflict (WHO et al. 2010). Unmet need for contraception is a major contributing factor to maternal mortality. According to the Countdown to 2015 for Maternal, Newborn and Child Survival, a reduction in maternal mortality and morbidity requires, among other services, increased coverage of comprehensive FP programmes (Bhutta et al. 2010). In 2010, the UN Secretary General launched the Global Strategy for Women's and Children's Health (United Nations 2010). Since then, many donors, private companies, and technical and service delivery agencies – many of which identified FP as a key intervention – have made commitments to the campaign (United Nations 2011).
Nevertheless, funding for FP is under-prioritised when compared to competing issues in resource-poor settings, and even more neglected in conflict settings (Austin et al. 2008, Patel et al. 2009, Prata 2009). For example, a study published in 2009 showed that approximately 2% of official development assistance disbursements to the conflict-affected countries studied was allocated to RH, of which less than 2% was for FP (Patel et al. 2009). A 2004 global evaluation of 10 years of RH service provision to conflict-affected populations found that FP services were inadequate (Inter-Agency Working Group on Reproductive Health in Refugee Situations 2004). When available, FP services were generally limited to oral contraceptives and condoms, even though a broad choice of methods is an essential component of good FP programming (Cleland et al. 2006, Prata et al. 2009).
The protracted conflict in northern Uganda highlights the challenges of providing FP services in conflict settings (Orach et al. 2009). At the peak of the war, over 1.8 million people were displaced from their homes, nearly 90% of the population of northern Uganda (Internal Displacement Monitoring Centre 2008). Many of the displaced moved to ‘protected villages’ or IDP camps, often established near existing health centres (Orach et al. 2009). More than two-thirds of the displaced moved within their existing subcounty (Boas and Hatloy 2005). The Ministry of Health (MOH) and humanitarian aid organisations provided limited health services; in 2006, 25–60% of health facilities in the north were considered ‘non-functional’ (United Nations 2006). Furthermore, RH indicators were worse in the northern region compared with national figures, suggesting weak or inadequate services: modern contraceptive prevalence was 8.1% compared to 17.9% nationally; only 19.1% of the total demand for FP was satisfied in the north compared to 36.9% nationally (Uganda Bureau of Statistics and Macro International Inc. 2007).
To address this gap, Marie Stopes Uganda (MSU) partnered with the Reproductive Health Access, Information and Services in Emergencies (RAISE) Initiative to expand RH services in northern Uganda. The partnership employed a two-pronged approach, using mobile outreach teams in tandem with a long-term strategy of strengthening the capacity of four existing MOH health centres to provide RH services.
Beginning in 2007, six MSU mobile outreach teams visited MOH health centres in the four districts of Gulu, Lira, Pader and Kitgum every 1–2 months. After 18 months, the number of mobile teams was reduced to 4, resulting in a smaller number of sites (86) visited in order to maintain frequency of visits. The mobile teams, comprising one doctor and two nurses or midwives, provided primarily long-acting and permanent methods (LAPM): implants, intrauterine devices (IUDs), tubal ligations and vasectomies. The health centres provided short-acting methods (i.e. condoms, pills, injectables). Prior to the arrival of the mobile teams, MSU organised behaviour change communication (BCC) events targeting men, women and adolescents, including radio talk shows, drama shows, and community mobilisation by community health workers and village health teams to discuss the value of FP, the services available and the timing of the mobile team's visit. The mobile teams ensured adequate follow-up care by giving pre- and post-procedure counselling on how to deal with side effects, where and how to seek follow-up medical assistance if needed and when the mobile team would return to the health centre in case follow-up was required (Eva and Ngo 2010). In addition, clients could receive free treatment at Marie Stopes centres in Gulu and Lira.
As a second, complementary approach, MSU collaborated with the MOH and Canadian Physicians for Aid and Relief to strengthen the capacity of four MOH health centres (Awere, Mucwini, Purongo and Aromo), one in each of the four districts, to provide RH services. Once basic emergency obstetric care was established, long-acting FP methods were introduced in May-July 2010 in the four health centres which, according to MOH policy, are mandated to provide all short-and long-acting FP methods, but not permanent methods.
According to Bruce's quality of care framework, good-quality FP services enable women and couples to make an informed choice about using effective FP methods. Good-quality FP programmes have skilled providers who provide clients with information on a choice of methods available and have both the interpersonal communication skills required to communicate effectively and the technical competence to provide the selected method at the time (Bruce 1990). Support to the mobile teams and health centres included competency-based clinical and counselling training for providers with regular supportive supervision, provision of supplies and equipment to supplement government supplies (for the MOH facilities), and routine monitoring and evaluation. Mechanisms were in place to ensure continuation of use, and follow-up.
Little evidence is available for the effective provision of FP services in conflict-affected settings, and the challenges to collect data in these settings are well recognised (Thoms and Ron 2007, Ford et al. 2009). An evaluation using baseline (pre-intervention) and endline (post-intervention) surveys is appropriate when randomising clients is not due to the fundamental principle of client choice in FP programming (Habicht et al. 1999). In this paper, we discuss the results of population-based surveys conducted at baseline and endline to evaluate the effectiveness of the mobile outreach and health centre service provision of FP, and especially LAPM, in conflict-affected northern Uganda.
Methods
Survey design and sample
Baseline and endline population-based surveys were conducted in the catchment areas of the four MOH health centres that were also supported to provide RH services. Sampling at baseline was designed to permit independent parameter estimates for populations served by each health centre, as well as comparisons between urban and rural populations. Funding adjustments imposed a reduction on the survey sample size attainable at endline; specifically, urban populations were excluded from the second survey and the sample was not designed for independent estimates by region. Consequently, for this paper, rural populations surveyed at both baseline and endline are compared, while the single measures on urban populations are excluded. A multistage cluster sampling design was used within each of the four strata to ensure adequate representation of the four catchment areas. Using MOH population and household estimates for villages in the catchment areas, 45 clusters (10 each in Awere, Mucwini and Purongo and 15 in Aromo) were selected using probability proportional to size at baseline. Within each cluster, 25 households were systematically selected, except in Aromo where 17 households were selected in a larger number of clusters due to the low population density. At endline, a larger number of clusters (80) were selected using probability proportional to the population size in which a smaller number of households (11) were systematically selected to ensure adequate representation of the target areas. The number of clusters selected in each catchment area was proportional to the population size of that area: 28 clusters in Aromo, 22 in Awere, 23 in Mucwini and 7 in Purongo. For both surveys, in each household a single woman of reproductive age (15–49 years) was selected from all eligible women using a Kish table (Kish 1949). Anticipating an 80% response rate, a total of 1005 households were selected at baseline; a response rate of 90% was achieved resulting in a total of 905 respondents. At endline, a total of 880 households were selected; a response rate of 99% was achieved resulting in a total of 873 respondents.
Procedures
The questionnaire was adapted from the US Centers for Disease Control and Prevention's Reproductive health assessment toolkit for conflict-affected women (2007). The same questionnaire was used at baseline and endline with a few adaptations at endline to enhance clarity. The questionnaire covered various RH topics; this paper focuses on the FP findings. The questionnaire was translated and back-translated from English into the Langi and Acholi languages; the translations were reviewed and revised by the survey team.
All interviewers were female to ensure cultural appropriateness and increase the likelihood of accurate and valid data collection on RH topics. Consecutive trainings for supervisors and interviewers were held before baseline and endline data collection. The questionnaire was piloted in villages that were not sampled in the survey. Baseline data collection was carried out on 30 July – 2 September 2007; endline data collection occurred on 19 July – 5 August 2010.
Ethical considerations
Respondents were invited to participate in the survey through an oral informed consent process; names were not written on survey questionnaires ensuring anonymity. Ethical approvals for the survey were obtained from the Institutional Review Board of the Mailman School of Public Health, Columbia University and the Ugandan MOH.
Statistical analysis
Data were double-entered into CSPro Version 4.0 and subsequently exported to PASW (SPSS) Version 18 and STATA version 10.1 for cleaning and analysis. Data were initially weighted according to the number of eligible women of reproductive age in the household. Weights were scaled according to the number of households in the subcounty, so the final weighted population was representative of the distribution of households across the four subcounties. Weights were trimmed at 10 times the smallest weight. To incorporate the sample structure (strata, clusters and weights), analysis was conducted using the Stata survey functions. Logistic regression was used to calculate odds ratios (ORs) to compare key FP outcomes at baseline and endline, adjusting for differences in the distribution of key population demographics which may influence FP outcomes (age, marital status, number of children and education).
We have defined unmet need for FP among women in union (women who are married or living with a partner) and sexually active women not in union (defined as reporting sexual activity in the last 30 days). We considered women to have unmet need for FP if they reported wanting no more children or wanting to wait two years or more for their next child, or their current or recently delivered pregnancy was unwanted or mistimed; and they were not currently using a modern FP method nor were they using a modern method when they became pregnant.
Service statistics
Services statistics were collected monthly in 2008–2010 from the MSU mobile teams and the MOH health centres on numbers of clients who started LAPM.
Results
The samples of women at baseline and endline were similar with respect to age, religion, women in union, ability to read and having experienced an unwanted pregnancy (Table 1). Although the overall proportion of women in union was similar in the two surveys, a larger proportion of women reported being married and living with their husband at endline than at baseline (70.1% and 59.4%, respectively). More women reported having no living children at baseline (17.9% vs. 9.5% at endline). Over 80% of women at baseline and endline reported being able to read with difficulty or not at all; however, women reported less formal education at baseline (p = 0.005). Although 72.9% of women lived in IDP camps at baseline, 97.1% reported that they were local residents rather than displaced. No respondents lived in camps at endline.
Table 1.
Demographic characteristics of the population sampled at baseline and endline.
| Baseline (N = 905)a | Endline (N = 873)a | P-value | |
|---|---|---|---|
| Age (years) | .059 | ||
| 15–24 | 41.7% (370) | 34.8% (296) | |
| 25–34 | 30.8% (304) | 35.5% (331) | |
| 35–49 | 27.5% (231) | 29.7% (246) | |
| Mean age (SD), years | 28.12 (0.48) | 29.33 (0.37) | |
| Marital and cohabitation status | <.001 | ||
| Married and living with husband | 59.4% (557) | 70.1% (636) | |
| Married and not living with husband | 9.0% (75) | 6.5% (50) | |
| Not married, living with partner | 14.1% (140) | 4.0% (36) | |
| Not married, not living with partner | 17.5% (124) | 19.5% (151) | |
| Number of living children | <.001 | ||
| 0 | 17.9% (136) | 9.5% (74) | |
| 1–2 | 24.6% (224) | 26.7% (233) | |
| 3–4 | 27.0% (273) | 30.0% (275) | |
| 5 or more | 30.5% (271) | 33.8% (291) | |
| Religion | .089 | ||
| Catholic | 59.6% (570) | 58.3% (516) | |
| Protestant | 28.8% (229) | 27.9% (237) | |
| Pentecostal/Evangelical | 7.9% (74) | 12.2% (104) | |
| Other | 3.6% (31) | 1.6% (14) | |
| Formal education | .005 | ||
| None | 33.7% (328) | 24.4% (216) | |
| Did not complete primary school | 51.1% (455) | 59.0% (514) | |
| Completed primary school | 8.9% (76) | 9.0% (78) | |
| At least some secondary education | 6.4% (46) | 7.7% (65) | |
| Self-reported ability to read | .253 | ||
| With difficulty or not at all | 84.5% (786) | 81.6% (716) | |
| Easily | 15.6% (119) | 18.5% (157) | |
| Reported an unwanted pregnancy | .983 | ||
| No | 52.6% (435) | 52.7% (448) | |
| Yes | 47.4% (470) | 47.3% (425) | |
| Living in displaced persons camp | <.001 | ||
| No | 27.1% (205) | 100.0% (873) | |
| Yes | 72.9% (700) | 0.0% |
Note: Data are% of column weighted base (absolute counts), unless indicated. Bases are smaller for some variables due to missing data. Missing data are less than 0.5% for all variables except baseline marital and cohabitation status where data were missing for 10 women (1.1% weighted base).
aN = the weighted and unweighted base.
In Table 2, we show significant increases from baseline to endline in four categories of knowledge and use of modern FP, and particularly for LAPM. These increases persisted after adjusting for differences in sociodemographic characteristics of the baseline and endline samples. When asked to name any FP method, 43.4% (95%CI 37.7–49.2) of women at baseline spontaneously named at least one LAPM, compared to 83.1% (95%CI 79.9–85.8) at endline. The proportion of women who reported having received instruction on how to use at least one LAPM increased from 18.4% (95%CI 15.8–21.2) to 47.7% (95%CI 43.6–51.7). Reported ever use of any modern FP method increased from 27.6% (95%CI 23.5–32.2) to 47.3% (95%CI 43.6–51.1), and of LAPM from 3.1% (95%CI 1.9–5.0) to 12.1% (95%CI 9.5–15.3). Current use of any modern method of FP increased from 7.1% to 22.6% (adjusted OR 3.34 [95%CI 2.27–4.92]), while current use of LAPM increased from almost none (1.2%) to 9.8% at endline (adjusted OR 9.45 [95%CI 3.98–22.42]). Among modern FP methods, current use of implants and injectables showed the largest increases (Figure 1).
Table 2.
Reported knowledge and use of modern family planning methods at baseline and endline.
| Baseline (95%CI) (N = 905)a | Endline (95%CI) (N = 873)a | Unadjusted OR (95%CI) (N = 1768) | Adjusted OR (95%CI)b (N = 1768) | P-value, adjusted OR | |
|---|---|---|---|---|---|
| Spontaneous knowledge of modern FP methods | |||||
| Any modern method | 83.3 (79.6–86.4) | 94.0 (91.8–95.7) | 3.19 (2.09–4.88) | 3.00 (1.92–4.67) | <.001 |
| Any LAPMc | 43.4 (37.7–49.2) | 83.1 (79.9–85.8) | 6.39 (4.74–8.60) | 6.03 (4.47–8.13) | <.001 |
| Reported prior instruction on how to use modern FP method | |||||
| Any modern method | 51.0 (46.7–55.3) | 72.0 (68.1–75.6) | 2.48 (1.94–3.16) | 2.46 (1.92–3.16) | <.001 |
| Any LAPMc | 18.4 (15.8–21.2) | 47.7 (43.6–51.7) | 4.05 (3.22–5.09) | 4.13 (3.23–5.28) | <.001 |
| Reported ever use of modern FP method | |||||
| Any modern method | 27.6 (23.5–32.2) | 47.3 (43.6–51.1) | 2.34 (1.80–3.03) | 2.23 (1.70–2.92) | <.001 |
| Any LAPMc | 3.1 (1.9–5.0) | 12.1 (9.5–15.3) | 4.31 (2.46–7.56) | 4.14 (2.34–7.30) | <.001 |
| Reported current use of modern FP method | |||||
| Any modern method | 7.1 (5.2–9.6) | 22.6 (19.5–26.0) | 3.78 (2.59–5.52) | 3.44 (2.34–5.05) | <.001 |
| Any LAPMc | 1.2 (0.5–2.6) | 9.8 (7.4–12.9) | 9.10 (3.89–21.28) | 9.45 (3.98–22.42) | <.001 |
| Unmet need for family planning | |||||
| Unmet need for FP | 52.1 (48.5–55.6) | 35.7 (32.0–39.6) | 0.51 (0.41–0.63) | 0.47 (0.37–0.60). | <.001 |
Note: Bases are smaller for some variables due to missing data. Missing data are less than 0.5% for all variables. Any modern method includes emergency hormonal contraception for knowledge and ever use but not for current use.
aN = the weighted and unweighted base.
bAdjusted for age, marital status, number of children and education.
cLAPM are IUD, implant, tubal ligation and vasectomy.
Figure 1.
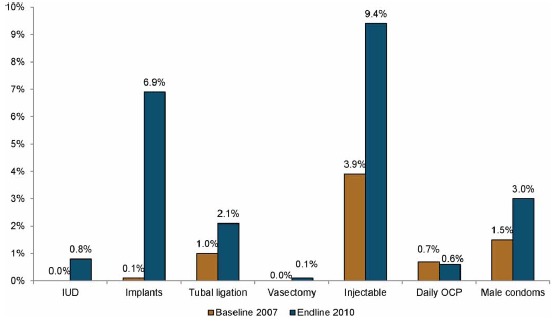
Current use of modern FP, by method, Northern Uganda, in 2007 and 2010.
The proportion of women with unmet need for FP decreased from 52.1% at baseline to 35.7% at endline (adjusted OR 0.47 [95%CI 0.37–0.60]). The demographic profiles were similar among women with met and unmet need for FP, with the exception of level of education (Table 3). Women currently using a modern method were more likely to have completed primary school or higher (25.2%) than women with unmet need (13.5%, p = 0.007).
Table 3.
Demographic characteristics of women with unmet and met need for family planning at endline.
| Unmet need for FP(95%CI) (N = 312,319)a | Met need for FPb (95%CI) (N = 197,200)a | P-value | |
|---|---|---|---|
| Age (years) | .788 | ||
| 15–24 | 33.1 (28.0–38.8) | 32.2 (26.1–39.0) | |
| 25–34 | 41.9 (35.0–49.2) | 39.9 (32.5–47.8) | |
| 35–49 | 24.9 (19.9–30.7) | 27.9 (21.4–35.5) | |
| Marital and cohabitation status | .082 | ||
| Married and living with partner | 82.0 (76.3–86.6) | 76.4 (67.7–83.4) | |
| Married and not living with Partner | 8.0 (5.3–11.7) | 7.6 (3.4–16.1) | |
| Not married, living with partner | 5.9 (3.3–10.4) | 4.2 (2.4–7.5) | |
| Not married, not living with Partner | 4.2 (2.1–8.0) | 11.7 (7.3–18.4) | |
| Number of living children | .844 | ||
| 0 | 2.7 (1.3–5.6) | 2.6 (1.0–7.0) | |
| 1–2 | 29.2 (24.0–35.0) | 25.5 (19.2–32.9) | |
| 3–4 | 29.9 (24.5–35.9) | 32.5 (26.0–39.8) | |
| 5 or more | 38.2 (33.4–43.3) | 39.4 (32.7–46.6) | |
| Religion | .183 | ||
| Catholic | 61.5 (54.6–67.9) | 52.8 (43.4–61.9) | |
| Protestant | 25.8 (20.2–32.2) | 33.9 (26.1–42.8) | |
| Pentecost/Evangelical | 11.9 (7.8–17.9) | 11.1 (7.2–16.5) | |
| Other | 0.8 (0.3–2.6) | 2.3 (0.6–7.8) | |
| Formal education | .007 | ||
| None | 27.7 (22.9–33.1) | 17.4 (12.4–23.9) | |
| Did not complete primary school | 58.8 (54.2–63.3) | 57.4 (49.2–65.3) | |
| Completed primary school | 7.7 (5.3–11.1) | 14.8 (9.6–22.1) | |
| At least some secondary Education | 5.8 (3.6–9.2) | 10.4 (6.3–16.6) | |
| Self-reported ability to read | .033 | ||
| With difficulty or not at all | 84.7 (79.5–88.8) | 76.4 (69.6–82.0) | |
| Easily | 15.3 (11.2–20.5) | 23.6 (18.0–30.4) |
Note: Bases are smaller for some variables due to missing data. Missing data are less than 0.5% for all variables.
aN = the weighted and unweighted bases.
bMet need for FP includes all women currently using any modern FP method.
Among women reporting current use of a modern FP method at endline, 54.7% (95%CI 47.6–61.7) reported a public health centre as the source of their method. Among women using an LAPM, more than half, 60.1% (95%CI 48.3–71.0), reported obtaining the method from a health centre, 20.7% (95%CI 11.7–33.9) from a hospital, 14.8% (95%CI 9.3–22.7) from MSU and 4.5% (95%CI 1.4–13.3) from a private health clinic.
In 2008–2010, the MSU mobile teams provided LAPM to 45,341 women and men at the 86 health centres in the 4 districts (Figure 2). By May 2010, the four supported health centres had staff trained to insert and remove long-acting methods as well as essential supplies. Service statistics showed that the 4 health centres provided 29 IUDs and 196 implants to clients between May and December 2010.
Figure 2.
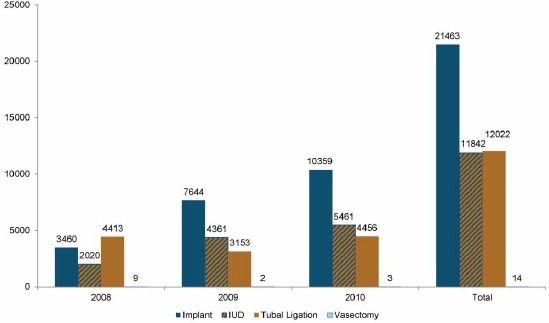
Number of clients who started each FP method, MSU mobile outreach teams in Kitgum, Lira, Pader and Gulu, Northern Uganda, in 2008–2010.
Discussion
Our results demonstrate the feasibility of meeting women's demands for FP in conflict settings. Substantive increases in the current use of modern methods from 7.1% to 22.6%, and especially of LAPM from 1.2% to 9.8%, were achieved in the areas of northern Uganda surveyed. Our findings demonstrate that women in conflict settings want and will use LAPM when they are available and clients are informed about them.
Demand for birth spacing or limiting exists in conflict-affected populations (McGinn et al. 2011). Our results concur with 52.1% of women at baseline reporting unmet need for FP. Where FP services are available in conflict settings, often only short-acting methods are provided (Inter-Agency Working Group on Reproductive Health in Refugee Situations 2004). Many humanitarian organisations have not expanded their expertise in delivering health services to prioritise FP, much less LAPM, provision while RH agencies rarely work in conflict settings (Austin et al. 2008). Our experience here and in other countries (Casey et al. 2009) demonstrated that a lack of provider training is one barrier to LAPM provision by humanitarian organisations. We addressed this by making competency-based training and supportive supervision a key aspect of our support. Our findings showed a decrease in unmet need for FP at endline when women who wanted to delay or avoid pregnancy chose to use FP, with many choosing an LAPM. This finding reinforces the need to ensure that the full range of FP methods is available to conflict-affected populations.
We believe that this programme provided the LAPM for most women who reported a public health centre as their source because the MSU mobile teams provided LAPM at the local health centres (before the facility staff were trained and supplied to provide them directly). Since the mobile teams provided the LAPM at the health centres, some women may have reported the location (health centre) while others reported the provider (MSU) even though they refer to the same source. However, it is possible that some women travelled further than the nearest health centre to obtain their method, for example to Gulu or Lira town, as was the likely case for those reporting FP use at baseline. A small number of organisations were providing LAPM in other areas of northern Uganda, though none were present in these four subcounties. According to the 2007 national service provision assessment, few facilities provided IUDs (4%) and implants (6%), suggesting that these methods are only rarely available (MOH [Uganda] and Macro International Inc. 2008).
Our baseline data showing low knowledge and use of LAPM are consistent with other FP data for northern Uganda at that time (Uganda Bureau of Statistics and Macro International Inc. 2007). We likely can attribute the increased knowledge and use primarily to the new availability of voluntary FP services, with a broad range of methods and appropriate information, given the apparent lack of other sources.
Our data show few inequities in access to the FP services. A larger proportion of current users of FP had completed primary school or higher education. This is consistent with other studies that show positive correlations between education and FP use (Ezeh et al. 2009, Ortayli and Malarcher 2010). Other sociodemographic characteristics such as age, marital status and number of living children were not significantly different among those with met and unmet need. Although evaluation of the BCC activities is beyond the scope of this study, this suggests that this community outreach and BCC model reached most women in the catchment areas, appearing to reduce inequity in access (Ortayli and Malarcher 2010).
During the intervention, the government policy of decongestion of the IDP camps was completed resulting in no participants living in IDP camps at endline. We believe that similar populations were surveyed despite the decongestion of the IDP camps because most people were displaced as village units, not far (often less than 10 km) from their original homes, and were served by the same health centres (Boas and Hatloy 2005). For example, at baseline, over 90% of the respondents self-reported that they were local residents rather than displaced within the country despite the fact that 72% of them lived in an IDP camp. Sociodemographic data from the surveys suggest that marriage prevalence, access to education, and the number of living children changed over time. The increases in educational attainment and proportion of married women are consistent with the data from 2006 and 2010 national surveys (Uganda Bureau of Statistics and Macro International Inc. 2007, Uganda Bureau of Statistics 2010). Despite the change in marriage prevalence, the proportion of women in union remained the same. The higher proportion of women with living children at endline is consistent with increased fertility that has been seen following a decline during war and that accompanies higher numbers of women living with their husbands or partners (Agadjanian and Prata 2002, Blanc 2004).
Our model made FP services available quickly through the mobile teams while the slower process to establish good-quality FP services through the MOH was implemented. Government agencies are often weakened during conflict. Supporting government health systems post-conflict is, therefore, an important component of recovery (Kruk et al. 2010). Our support to the health centres included essential components of good-quality FP services: competency-based training of providers; supportive supervision; essential equipment, supplies and medicines; and rigorous monitoring and evaluation (Bruce 1990). Health system strengthening can be a long-term process, a particular challenge when people who need these services await them. This process was enhanced by the mobile outreach teams’ service delivery as women started receiving LAPM immediately at the health centres in 2007. By mid-2010, the health centres had developed the capacity to provide LAPM and meet demand from women previously served by the mobile teams.
The mobile teams demonstrated to the MOH staff that demand for LAPM existed, increased awareness and knowledge among the population, and normalised these services at the health centres. When the MOH staff were trained to provide LAPM, demand had been generated and client load was present. MSU mobile staff further served as mentors while MOH staff gained confidence in their new skills post-training. Service statistics show that MOH staff at the four health centres, in addition to the mobile teams, provided long-acting methods during the last 6 months of 2010.
Limitations
It is important to recognise the limitations of our study. Data were collected in two cross-sectional surveys conducted at baseline and endline. There are strong ethical reasons for not having control communities in this situation, but in their absence we are unable to disentangle changes that would have occurred without this programme. However, the lack of LAPM provision in public health centres (MOH [Uganda] and Macro International Inc. 2008), the high numbers of LAPM provided by the mobile teams, and the data from cross-sectional surveys demonstrating increased knowledge of FP methods and increased ever and current use of FP provide strong evidence to support successful implementation of this programme (Habicht et al. 1999). The order of the FP questions changed at endline to prevent women who reported being infecund for invalid reasons from skipping questions about current use of FP. When calculating contraceptive prevalence at baseline, women who reported being physically unable to get pregnant were coded as not currently using FP unless they specifically reported use of a modern FP method as the reason they could not get pregnant. We may therefore have underestimated current FP use at baseline, but given the large increase in reported ever use of a modern FP method we believe the increase in current use to be robust.
This study did not directly measure the effectiveness of the BCC intervention. The BCC activities took place through a number of media outlets throughout the project period. However, the ongoing BCC activities which were intensified in the days before the mobile team arrived, along with routine service statistics and the increase in contraceptive prevalence, suggest a positive effect of the BCC intervention. We also did not explicitly evaluate the quality of the services. However, facility assessments at the end of the project illustrated that the essential supplies were available, and observation of providers during routine supervision visits over three years suggests that the mobile outreach teams provided good-quality FP services.
Conclusion
FP services are important to meet couples’ health needs. In conflict-affected countries, access to FP is often limited to short-acting methods or not available at all. This study demonstrates that when a full range of FP methods is provided among conflict-affected populations, women with unmet need will choose to use them. A dual approach of using mobile outreach teams and health system strengthening can make a full range of methods, including LAPM, quickly available in the short-term while strengthening the health system to continue to provide those services in the long-term. This model enables conflict-affected populations to exercise their right to prevent unwanted pregnancies while simultaneously improving the long-term sustainability of FP services as the country transitions from conflict to post-conflict development. It is imperative that international organisations, both humanitarian and RH agencies, prioritise FP services for these underserved populations, and offer the full range of short-acting, long-acting and permanent methods.
Acknowledgements
We thank the survey participants who shared their experiences as well as the field teams who conducted the interviews for their enthusiasm and dedication. We also acknowledge the contributions of James Onziga Geria, endline study coordinator, and Denis Okwar, project coordinator.
The RAISE Initiative was funded by an anonymous private foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
SEC and LLJ participated in the study conception and design; SEC, SEM, LLJ and JO participated in implementation of the study; SEC and CT participated in analysis of the data; SEC and SEM drafted the manuscript; LLJ, JO, CT and ACT contributed to the writing process; all authors reviewed and approved the final version of the manuscript. All authors had access to all the data; the corresponding author had final responsibility for the decision to submit for publication.
References
- Agadjanian V., Prata N. War, peace, and fertility in Angola. Demography. 2002;39(2):215–231. doi: 10.1353/dem.2002.0013. [DOI] [PubMed] [Google Scholar]
- Al Gasseer N., Dresden E., Keeney G., Warren N. Status of women and infants in complex humanitarian emergencies. Journal of Midwifery and Women's Health. 2004;49(4 Suppl 1):7–13. doi: 10.1016/j.jmwh.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Austin J., Guy S., Lee-Jones L., McGinn T., Schlecht J. Reproductive health: a right for refugees and internally displaced persons. Reproductive Health Matters. 2008;16(31):10–21. doi: 10.1016/S0968-8080(08)31351-2. [DOI] [PubMed] [Google Scholar]
- Bhutta Z.A., Chopra M., Axelson H., Berman P., Boerma T., Bryce J., Bustreo F., Cavagnero E., Cometto G., Daelmans B., De Francisco A., Fogstad H., Gupta N., Laski L., Lawn J., Maliqi B., Mason E., Pitt C., Requejo J., Starrs A., Victora C.G., Wardlaw T. Countdown to 2015 decade report (2000–10): taking stock of maternal, newborn, and child survival. The Lancet. 2010;375(9730):2032–2044. doi: 10.1016/S0140-6736(10)60678-2. [DOI] [PubMed] [Google Scholar]
- Blanc A.K. The role of conflict in the rapid fertility decline in Eritrea and prospects for the future. Studies in Family Planning. 2004;35(4):236–245. doi: 10.1111/j.0039-3665.2004.00028.x. [DOI] [PubMed] [Google Scholar]
- Boas M., Hatloy A. Northern Uganda internally displaced persons profiling study. 2005. [online]. Available from: http://www.fafo.no/ais/africa/uganda/IDP_uganda_2005.pdf [Accessed 10 August 2012]
- Bruce J. Fundamental elements of the quality of care: a simple framework. Studies in Family Planning. 1990;21(2):61–91. [PubMed] [Google Scholar]
- Casey S.E., Mitchell K.T., Amisi I.M., Haliza M.M., Aveledi B., Kalenga P., Austin J. Use of facility assessment data to improve reproductive health service delivery in the Democratic Republic of the Congo. Conflict and Health. 2009;3(1):12. doi: 10.1186/1752-1505-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleland J., Bernstein S., Ezeh A., Faundes A., Glasier A., Innis J. Family planning: the unfinished agenda. The Lancet. 2006;368(9549):1810–1827. doi: 10.1016/S0140-6736(06)69480-4. [DOI] [PubMed] [Google Scholar]
- Eva G, Ngo T.D. MSI mobile outreach services: retrospective evaluations from Ethiopia, Myanmar, Pakistan, Sierra Leone and Viet Nam. 2010. [online]. Available from: http://archive.k4health.org/system/files/outreach_web_1.pdf [Accessed 10 August 2012]
- Ezeh A.C., Mberu B.U., Emina J.O. Stall in fertility decline in eastern African countries: regional analysis of patterns, determinants and implications. Philosophical Transactions of the Royal Society B: Biological Sciences. 2009;364(1532):2991–3007. doi: 10.1098/rstb.2009.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford N., Mills E., Zachariah R., Upshur R. Ethics of conducting research in conflict settings. Conflict and Health. 2009;3(1):7. doi: 10.1186/1752-1505-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habicht J.P., Victora C.G, Vaughan J.P. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. International Journal of Epidemiology. 1999;28(1):10–18. doi: 10.1093/ije/28.1.10. [DOI] [PubMed] [Google Scholar]
- Inter-Agency Working Group on Reproductive Health in Refugee Situations. Report of an inter-agency global evaluation of reproductive health services for refugees and internally displaced persons. 2004. [online]. Available from: http://www.iawg.net/resources/2004_global_eval/ [Accessed 10 August 2012]
- Internal Displacement Monitoring Centre. Focus shifts to securing durable solutions for IDPS: a profile of the internal displacement situation. 2008. [online]. Available from: http://www.internal-displacement.org/8025708F004BE3B1/(httpInfoFiles)/B02A8784F26C9D6BC12574F6004BE252/$file/Uganda%20-November%202008.pdf [Accessed 10 August 2012]
- Kish L. A procedure for objective respondent selection within the household. Journal of the American Statistical Association. 1949;44(247):380–387. [Google Scholar]
- Kruk M.E., Freedman L.P., Anglin G.A., Waldman R.J. Rebuilding health systems to improve health and promote statebuilding in post-conflict countries: a theoretical framework and research agenda. Social Science and Medicine. 2010;70(1):89–97. doi: 10.1016/j.socscimed.2009.09.042. [DOI] [PubMed] [Google Scholar]
- McGinn T. Reproductive health of war-affected populations: what do we know? International Family Planning Perspectives. 2000;26(4):174–180. [Google Scholar]
- McGinn T., Austin J., Anfinson K., Amsalu R., Casey S., Fadulalmula S., Langston A., Lee-Jones L., Meyers J., Mubiru F., Schlecht J., Sharer M., Yetter M. Family planning in conflict: results of cross-sectional baseline surveys in three African countries. Conflict and Health. 2011;5(1):11. doi: 10.1186/1752-1505-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinn T., Casey S., Purdin S., Marsh M. Reproductive health for conflict-affected people: policies, research and programmes. 2004. London. Available from: http://www.odihpn.org/documents/networkpaper045.pdf [Accessed 10 August 2012]
- Ministry of Health (MOH) [Uganda] and Macro International Inc. Uganda service provision assessment survey 2007. 2008. [online]. Available from: http://www.measuredhs.com/pubs/pdf/SPA13/SPA13.pdf [Accessed 10 August 2012]
- Orach C.G., Musoba N., Byamukama N., Mutambi R., Aporomon J.F., Luyombo A., Rostedt A. Perceptions about human rights, sexual and reproductive health services by internally displaced persons in northern Uganda. African Health Sciences. 2009;9(Suppl 2):S72–80. [PMC free article] [PubMed] [Google Scholar]
- Ortayli N., Malarcher S. Equity analysis: identifying who benefits from family planning programs. Studies in Family Planning. 2010;41(2):101–108. doi: 10.1111/j.1728-4465.2010.00230.x. [DOI] [PubMed] [Google Scholar]
- Patel P., Roberts B., Guy S., Lee-Jones L., Conteh L. Tracking official development assistance for reproductive health in conflict-affected countries. Public Library of Science Medicine. 2009;6(6):e1000090. doi: 10.1371/journal.pmed.1000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata N. Making family planning accessible in resource-poor settings. Philosophical Transactions of the Royal Society of London Series B: Biological Sciences. 2009;364(1532):3093–3099. doi: 10.1098/rstb.2009.0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata N., Sreenivas A., Vahidnia F., Potts M. Saving maternal lives in resource-poor settings: facing reality. Health Policy. 2009;89(2):131–148. doi: 10.1016/j.healthpol.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Sphere Project. Sphere project: humanitarian charter and minimum standards in humanitarian response. 2011. [online]. Available from: http://www.sphereproject.org/handbook/ [Accessed 10 August 2012] [DOI] [PubMed]
- Thoms O., Ron J. Public health, conflict and human rights: toward a collaborative research agenda. Conflict and Health. 2007;1(1):11. doi: 10.1186/1752-1505-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uganda Bureau of Statistics. Uganda national household survey 2009/2010. 2010. [online]. Available from: http://www.ubos.org/UNHS0910/unhs200910.pdf [Accessed 10 August 2012]
- Uganda Bureau of Statistics and Macro International Inc. Uganda demographic and health survey 2006. 2007. [online]. Available from: http://www.measuredhs.com/pubs/pdf/FR194/FR194.pdf [Accessed 10 August 2012]
- United Nations. Programme of action of the international conference on population and development. 1994. [online]. Available from: http://www.un.org/ecosocdev/geninfo/populatin/icpd.htm#chapter10 [Accessed 10 August 2012]
- United Nations. Uganda 2006 revision consolidated appeal process. 2006. [online]. Available from: http://ochaonline.un.org/humanitarianappeal/webpage.asp?Page=1373 [Accessed 10 August 2012]
- United Nations. UN summit launches drive to save the lives of more than 16 million women and children (UN Press Release) 2010. [online]. Available from: http://www.unfpa.org/public/home/news/pid/6679 [Accessed 10 August 2012]
- United Nations. Every woman every child. 2011. Summary of commitments to advance the global strategy for women's and children's health 2011 [online]. Available from: http://everywomaneverychild.org/images/content/files/Every_Woman_Every_Child_2011_Commitments_9_28_11.pdf [Accessed 10 August 2012]
- US Centers for Disease Control and Prevention. Reproductive health assessment toolkit for conflict-affected women. 2007. [online]. Available from: http://www.cdc.gov/reproductivehealth/Global/CrisisSituations.htm [Accessed 10 August 2012]
- WHO, UNICEF, UNFPA and The World Bank. Trends in maternal mortality: 1990 to 2008: estimates developed by WHO, UNICEF, UNFPA and the World Bank. 2010. [online]. Available from: http://whqlibdoc.who.int/publications/2010/9789241500265_eng.pdf [Accessed 10 August 2012].


