Abstract
Anisospondyly (irregularly shaped vertebral bodies) and enchondroma-like lesions in the metaphyseal and diaphyseal portions of the long tubular bones are the characteristic features in patients with dysspondyloenchondromatosis (DSC). Thoraco-lumbar scoliosis and windswept deformity of the lower limbs were the major abnormalities encountered in this patient. To the best of our knowledge this is the first case report delineating the spine pathology via reformatted CT scan and the correction of a windswept deformity by means of temporary hemiepiphysiodesis in a patient with (DSC).
Keywords: dysspondyloenchondromatosis, anisospondyly, windswept deformity, hemiepiphysiodesis
Abstract
Anisospondylie (irregular geformte Wirbelkörper) und Enchondrom-artige Läsionen im metaphysären und dipaphysären Bereich langer Röhrenknochen sind die charakteristischen Merkmale bei Patienten mit Dysspondyloenchondromatose (DSC). Bei dem von uns vorgestellten Patienten war eine thorako-lumbale Skoliose sowie eine Windschlag-Deformität der unteren Extremität ein wesentliches Merkmal. Unseres Wissens ist dies der erste Case-Report, welcher die Wirbelsäulen-Pathologie mittels CT-Untersuchung darstellt und die Korrektur der Windschlag-Deformität mit Hilfe einer Hemiepiphyseodese bei einem Patienten mit DSC beschreibt.
Introduction
Anisospondyly (irregularly shaped vertebral bodies) is a unique vertebral disorganization malformation complex encountered in a number of skeletally dysplastic patients [1].
The term “windswept deformity” describes the appearance of abnormal valgus deformity in one knee in association with varus in the other. It is commonly seen in young children in certain parts of Africa, and it develops secondary to metabolic bone diseases. Metabolic bone diseases frequently result in skeletal deformities, especially in the legs, due to physeal disturbances or defective mineralization in children before puberty. Among these disorders, hypophosphataemic rickets, hypophosphatasia, and renal osteodystrophy are the most frequent as well as some exceptional cases of bone dysplasias such as Shwartz-Jampel syndrome [2].
Dysspondyloenchondromatosis (DSC) is a rare skeletal dysplasia that has currently been classified into the group of spondylometaphyseal dysplasias. Distinctive features of DSC are anisospondyly and enchondroma-like lesions in the metaphyseal and diaphyseal portions of the long tubular bones. Patients with dysspondyloenchondromatosis are usually manifesting progressive kyphoscoliosis due to anisospondyly and asymmetric limb shortening at an early age. DSC was once considered to be a form of generalized enchondromatosis [3], [4], [5], [6], [7].
Clinical report
A 5-year-old-boy was referred to our department because of angular deformity of the limbs. He was the product of uneventful gestation at 38-weeks of gestation. Parents were unrelated. At birth his length was –3SD. His subsequent course of development has been of noticeable retardation particularly in acquiring the skills of motor development. Head control, sitting with no support, crawling and walking were markedly delayed. At the age of 3 he started to walk albeit with difficulty. Windswept deformities of the lower limbs were notable. There was no cleft lip and or palate. Hearing, vision, and neurological examinations were normal. No skin stigmata such as café-au-lait were seen. He had no history of pain, fatigue and or any other conditions, which could limit his activity. Limping was the most prominent abnormality in connection with windswept lower limb deformity.
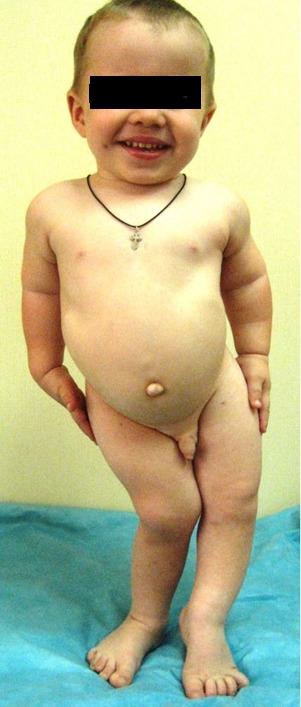
Clinical examination at the age of 5 years showed sparse skull hair, depressed nasal bridge, full cheeks, large nose, microdontia, and large ears. Ligamentous hyperlaxity, rhizomelia, barrel shaped chest, dysplastic nipples, umbilical hernia, and winswept lower limb deformity (genu valgum of 30º on the right side, genu varum of 10º on the left side) were evident (Figure 1 (Fig. 1)).
Figure 1. The child’s phenotype showed sparse skull hair, depressed nasal bridge, full cheeks, large nose, microdontia, and large ears. Ligamentous hyperlaxity, rhizomelia, barrel shaped chest, dysplastic nipples, umbilical hernia, and windswept lower limb deformity.
Hip movements were moderately reduced, with abduction of 35º, and internal rotation of 30º bilaterally. Full hematological tests, ESR, calcium, alkaline phosphatase, and urine mucopolysaccharides and a karyogram for the child and his parents were normal. No associated hyper functioning endocrinopathies, such as hyperthyroidism, or excess growth hormone have been encountered. We were unable to perform genetic testing on this patient because of logistical reasons.
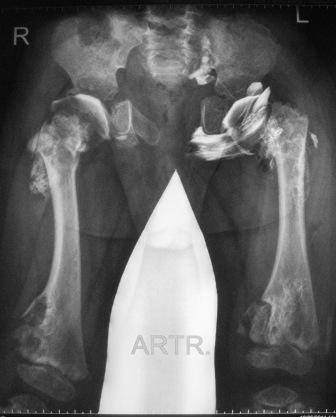
A skeletal survey at the age of 7 years, reformatted coronal spine CT scan showed thoracic scoliosis with significant vertebral disorganization associated with false image of butter-fly like vertebrae of the T8 and L1 and wedging of L2 because of irregular and defective ossification of the vertebral bodies which resembles segmentation defects overwhelmed by extensive enchondromatous lesions along the entire spine and the lacy-like appearance of the iliac crests (Figure 2 (Fig. 2)). Reformatted coronal spinal CT scan showed significant platyspondyly and anisospondyly (irregularly shaped vertebral bodies) in which a unique vertebral disorganization malformation complex is notable. Specific feature – chondromatose nodes in vertebral bodies (bony “defects” in anterior aspects, mostly – at thoracic level) (Figure 3 (Fig. 3)). Antero-posterior (AP) standing radiograph showed hypoplastic iliac bones associated with severe epiphyseal dysplasia and enchondroma-like lesions metaphyseal changes with significant metaphyseal expansion and radiolucency of the inferior femora. Note the windswept lower limb deformity (abnormal valgus deformity in one knee in association with varus in the other) (Figure 4 (Fig. 4)). Contrast arthgrography of the hips demonstrates spherical shape of the femoral heads with severe delayed ossification. Congruency of the hip joints is normal, cartilaginous acetabular coverage is sufficient. Short femoral necks (more severe on the left side with secondary decreased neck-shaft angle) are notable (Figure 5 (Fig. 5)). Contrast arthrography of the hips was done to assess cartilaginous components of the hip joints as a part of the previous pre-operative protocol which was standard in our clinic for children with severe hip instability. Now we believe that MRI would be less invasive and a more useful investigation in such a case. Nevertheless our data demonstrates spherical shape of the femoral heads with severe delayed ossification. Congruency of the hip joints is normal, cartilaginous acetabular coverage is sufficient.
Figure 2. Reformatted coronal Spine CT scan showed thoracic scoliosis with significant vertebral disorganization associated with false image of butter-fly like vertebrae of the T8 and L1 and wedging of L2 because of irregular and defective ossification of the vertebral bodies which resembles segmentation defects overwhelmed by extensive enchondromatous lesions along the entire spine and the lacy – like appearance of the iliac crests respectively.

Figure 3. Reformatted coronal spinal CT scan showed significant platyspondyly and anisospondyly (irregularly shaped vertebral bodies) in which a unique vertebral disorganization malformation complex is notable. Specific feature – chondromatose nodes in vertebral bodies (bony “defects” in anterior aspects, mostly – at thoracic level).

Figure 4. AP standing radiograph showed hypoplastic iliac bones associated with severe epiphyseal dysplasia and enchondroma-like metaphyseal changes with significant metaphyseal expansion and radiolucency of the inferior femora. Note the windswept lower limb deformity (abnormal valgus deformity in one knee in association with varus in the other).

Figure 5. Contrast arthrography of the hips demonstrates spherical shape of the femoral heads with severe delayed ossification. Congruency of the hip joints is normal, cartilaginous acetabular coverage is sufficient. Short femoral necks (more severe on the left side with secondary decreased neck-shaft angle) are notable.
Treatment
In order to guard against progression of the windswept deformity of the lower limbs, we decided to proceed by applying temporary hemiepiphysiodesis (plates were applied to the medial sides of the physes of right distal femur and right proximal tibia to correct the valgus deformity, with simultaneous application for the lateral aspect of the left proximal tibia to overcome the varus deformity) (Figure 6 (Fig. 6)).
Figure 6. Intraoperative radiographs of the knees. Plates for hemiepiphysiodesis applied to medial sides of the physes of right distal femur and right proximal tibia for correction of genu valgum and lateral aspect of left proximal tibia for correction of genu varum.

This technique might provide a guided growth of the long bones and has been used frequently in patients with skeletal dysplasia [8]. Ten months postoperative assessment revealed, satisfactory correction of 15º of genu valgum (left) and 5º of genu varum (right) was achieved.
Discussion
Enchondromas are common intraosseous, usually benign, cartilaginous tumors that develop in close proximity to growth plate cartilage. The lesions replace normal bone with mineralised or unmineralised hyaline cartilage thereby, generating a lytic area contain rings and arcs of chondroid calcifications. Moreover, it is characterised by an asymmetric distribution of the lesions and an extreme clinical variability. It is rarely observed at birth, although the lesions may be present. Enchondromas are metabolically active and may continue to grow and evolve throughout the patient’s lifetime, thus, progressive calcification over a period of years is not unusual. Radiographs typically show multiple, radiolucent, homogeneous lesions with an oval or elongated shape and well defined slightly thickened bony margins [9], [10].
Clinical abnormalities caused by enchondromas include limb length inequality, pathological fractures, and potential risk for malignant transformations, angular deformity, asymmetrical premature physeal arrest, and joint incongruity have been reported in connection with epi-metaphyseal enchondromatosis [11], [12], [13].
The distribution of the enchondromas, and other accompanying symptoms as well as the mode of inheritance define the different subtypes of enchondromatosis, which mainly includes Ollier disease, Maffucci syndrome, metachondromatosis, genochondromatosis, spondyloenchondrodysplasia, cheirospondyloenchondromatosis and dysspondyloenchondromatosis [1].
Spondyloenchondromatosis (Spranger type IV) is an autosomal recessive inherited disorder characterized by vertebral dysplasia combined with enchondroma like lesions in the pelvis or long tubular bones. The spinal aberrations include platyspondyly (flat, often rectangular vertebral bodies are seen at radiography with irregular areas of increased and decreased mineralization, and short broad ilia). Spondyloenchondrodysplasia can manifest itself from birth to later infancy. Patients usually have a short stature (short limbs), with increased lumbar lordosis, barrel chest and kyphoscoliosis, genu valga or vara, facial anomalies, and may show clumsy movements [1]. The clinical features of spondyloenchondrodysplasia are highly variable within and between the families (neurological and autoimmune manifestations were seen in different combinations within one single family suggesting remarkable pleiotropic manifestations of a single disease) [14].
Dysspondyloenchondromatosis (enchondromatosis with irregular vertebral lesions, enchondromatosis type V) is a non-hereditary disorder characterized by spondyloenchondromatosis combined with malformation of the spine. The irregularity of the vertebral anomalies differentiates dysspondyloenchondromatosis from other enchondromatosis with spinal involvement. Severe segmentation like abnormalities and secondary deformities of the vertebral column can be seen. Neonatal dwarfism, unequal limb length or asymmetric limb shortening, a flat midface with a frontal prominence, and progressive kyphoscoliosis can be found. Despite the existence of severe spinal deformity in our patient, surgical management was not recommended. The pathological distribution of the massive enchondromatous lesions within the spinal structures makes traditional approach potentially problematic and hazardous. Regular follow-up of this sort of spine pathology is the only line to be applied. Thereby, decisions for surgical repair and or intervention of the spine depend largely on the magnitude of deterioration. Furthermore, multiple enchondromas are present in the long tubular and flat bones while the bones of hands and feet are not or only mildly affected [1], [4], [5], [6]. Nakane et al. [15] identified a novel heterozygous COL2A1 missense mutation (p.Gly753Asp) in a 3-year-old boy.
Cheirospondyloenchondromatosis (Spranger type VI is characterized by generalized enchondromatosis with platyspondyly and enchondromatosis) combines symmetrically distributed multiple enchondromas with marked involvement of metacarpals and phalanges resulting in short hands and feet with mild platyspondyly. It occurs at very early age. There is mild to moderate dwarfism and joints, especially of the fingers, become enlarged. Mental retardation is frequently seen [1].
Halal and Azouz provisionally added three more subtypes to the Spranger classification including generalized enchondromatosis with irregular vertebral lesions (type VII), generalized enchondromatosis with mucopolysaccharides (type VIII) and enchondromatosis with concave vertebral bodies (type IX), all of which are non-hereditary [16].
In our current patient temporary hemiepiphysiodesis was applied as a minimally invasive and non-destructive approach. Hemiepiphysiodesis procedures have the advantage of producing unilateral physeal inhibition, thus achieving correction gradually and close to the joint, where correction of the deformity will be most effective. Hemiepiphysiodesis is a lesser surgical procedure than osteotomy and avoids the possible neurovascular complications of the latter, as well as the complications attendant on delayed union or malunion and surgical infection. Nevertheless, such patients are manifesting osteoporotic bones and staple extrusion is possible, therefore, strict follow-ups are mandatory [8]. In our current patient temporary epiphysiodesis with two-hole plates in contrast to Blount staples gives the possibility for more precise control of deformity correction. In children with unpleasant bone quality, the position of the screws can be chosen individually and independently. Particular consideration of the extent and the magnitude of the bone pathology should be taken into account. The bone pathology is variable among patients with skeletal dysplasias even if these patients are of the same diagnostic entity. The application of minimally invasive technique might be advantageous. Hypercorrection and or permanent closure of the growth plate should be avoided because of the unpredictable nature of the disease. In addition the screw can be replaced with minimal invasion in case recurrence was the outcome.
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Spranger JW, Brill PW, Poznanski AK. Bone dysplasias: An atlas of genetic disorders of skeletal development. 2nd ed. New York: Oxford University Press; 2002. [Google Scholar]
- 2.Al Kaissi A, Ganger R, Klaushofer K, Grill F. Windswept deformity in a patient with Schwartz-Jampel syndrome. Swiss Med Wkly. 2012 Mar 19;142:w13519. doi: 10.4414/smw.2012.13519. Available from: http://dx.doi.org/10.4414/smw.2012.13519. [DOI] [PubMed] [Google Scholar]
- 3.Haga N, Nakamura K, Taniguchi K, Nakamura S. Enchondromatosis with features of dysspondyloenchondromatosis and Maffucci syndrome. Clin Dysmorphol. 1998 Jan;7(1):65–68. doi: 10.1097/00019605-199801000-00014. Available from: http://dx.doi.org/10.1097/00019605-199801000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Freisinger P, Finidori G, Maroteaux P. Dysspondylochondromatosis. Am J Med Genet. 1993 Feb 15;45(4):460–464. doi: 10.1002/ajmg.1320450413. Available from: http://dx.doi.org/10.1002/ajmg.1320450413. [DOI] [PubMed] [Google Scholar]
- 5.Kozlowski K, Brostrom K, Kennedy J, Lange H, Morris L. Dysspondyloenchondromatosis in the newborn. Report of four cases. Pediatr Radiol. 1994;24(5):311–315. doi: 10.1007/BF02012112. Available from: http://dx.doi.org/10.1007/BF02012112. [DOI] [PubMed] [Google Scholar]
- 6.Reckling WC, Cheng EY. Dyssegmental dysplasia: short-trunk, short-limb dwarfism with anisospondyly. A case report. J Bone Joint Surg Am. 1994 Oct;76(10):1551–1556. [PubMed] [Google Scholar]
- 7.Warman ML, Cormier-Daire V, Hall C, Krakow D, Lachman R, LeMerrer M, Mortier G, Mundlos S, Nishimura G, Rimoin DL, Robertson S, Savarirayan R, Sillence D, Spranger J, Unger S, Zabel B, Superti-Furga A. Nosology and classification of genetic skeletal disorders: 2010 revision. Am J Med Genet A. 2011 May;155A(5):943–968. doi: 10.1002/ajmg.a.33909. Available from: http://dx.doi.org/10.1002/ajmg.a.33909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zuege RC, Kempken TG, Blount WP. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979 Apr;61(3):320–329. [PubMed] [Google Scholar]
- 9.Unni KK. Cartilaginous lesions of bone. J Orthop Sci. 2001;6(5):457–472. doi: 10.1007/s007760170015. Available from: http://dx.doi.org/10.1007/s007760170015. [DOI] [PubMed] [Google Scholar]
- 10.Kronenberg HM. Developmental regulation of the growth plate. Nature. 2003 May 15;423(6937):332–336. doi: 10.1038/nature01657. Available from: http://dx.doi.org/10.1038/nature01657. [DOI] [PubMed] [Google Scholar]
- 11.Mainzer F, Minagi H, Steinbach HL. The variable manifestations of multiple enchondromatosis. Radiology. 1971 May;99(2):377–388. doi: 10.1148/99.2.377. [DOI] [PubMed] [Google Scholar]
- 12.Gabos PG, Bowen JR. Epiphyseal-metaphyseal enchondromatosis. A new clinical entity. J Bone Joint Surg Am. 1998 Jun;80(6):782–792. doi: 10.2106/00004623-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz HS, Zimmerman NB, Simon MA, Wroble RR, Millar EA, Bonfiglio M. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987 Feb;69(2):269–274. [PubMed] [Google Scholar]
- 14.Renella R, Superti-Furga A. A new case of spondyloenchondrodysplasia with immune dysregulation confirms the pleiotropic nature of the disorder: comment on "A syndrome of immunodeficiency, autoimmunity, and spondylometaphyseal dysplasia" by M.L. Kulkarni, K. Baskar, and P.M. Kulkarni [2006] Am J Med Genet A. 2007 Jun 15;143A(12):1394–1395. doi: 10.1002/ajmg.a.31755. Available from: http://dx.doi.org/10.1002/ajmg.a.31755. [DOI] [PubMed] [Google Scholar]
- 15.Nakane T, Tando T, Aoyagi K, Hatakeyama K, Nishimura G, Coucke IP, Mortier G, Sugita K. Dysspondyloenchondromatosis: Another COL2A1-Related Skeletal Dysplasia? Mol Syndromol. 2011 Dec;2(1:21-6. DOI):10. doi: 10.1159/000333098. Available from: http://dx.doi.org/10.1159/000333098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halal F, Azouz EM. Generalized enchondromatosis in a boy with only platyspondyly in the father. Am J Med Genet. 1991 Mar 15;38(4):588–592. doi: 10.1002/ajmg.1320380418. Available from: http://dx.doi.org/10.1002/ajmg.1320380418. [DOI] [PubMed] [Google Scholar]


