ABSTRACT
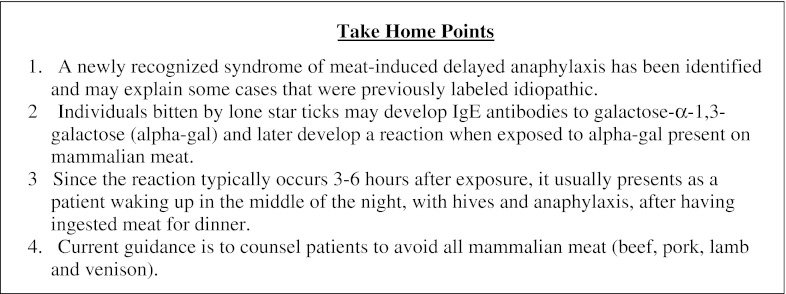
In recent years, a newly recognized allergic disease has been uncovered, and seemingly idiopathic causes of anaphylaxis now have an explanation. Individuals bitten by the lone star tick may develop IgE antibodies to the carbohydrate galactose-α-1,3-galactose (alpha-gal). Upon exposure of sensitized subjects to mammalian meat containing alpha-gal on glycoproteins or glycolipids, delayed anaphylaxis may ensue, often three to six hours after ingestion.1 Many of these individuals have negative allergy skin prick tests to meat, further obscuring the diagnosis. With the recent development of IgE alpha-gal tests, the clinical diagnosis can be confirmed in the laboratory.
KEY WORDS: allergy, anaphylaxis, immunology, tick, meat
INTRODUCTION
Delayed anaphylaxis linked to the ingestion of red meat is a newly recognized allergic disease. Previously, these cases might have been labeled idiopathic because the onset of signs and symptoms occurs three to six hours after exposure. However, research conducted at the University of Virginia by Platts–Mills and colleagues has uncovered a paradigm-changing new class of adult-onset mammalian meat-induced delayed anaphylaxis.2 Alpha-gal is a carbohydrate moiety found in mammalian meat. Humans can become sensitized to alpha-gal after tick bites, developing alpha-gal specific IgE that is detected commercially using a solid phase immunoassay.3 We present three clinical cases to illustrate this new syndrome. In addition, we review the discovery of alpha-gal specific IgE and how it impacts the current approach to anaphylaxis.
CASES
Case 1
An 82-year-old Caucasian man presented to clinic with a one-day history of a pruritic rash on his trunk and ankles. Past medical history was significant for hypertension, a transient ischemic attack, and polymyalgia rheumatica in remission. His wife thought the rash was an allergic reaction to amoxicillin which had been prescribed for a recent dental infection. The patient reported a history of occasional hives while playing golf, which he attributed to pesticide exposure. The last episode had been three years earlier. Physical exam revealed mild erythema and edema of his ankles and an urticarial rash on bilateral axillae and trunk. His wife also commented that ten days prior to the visit, she had removed a lone star tick from his back, which may have been attached for as long as 36 hours. Given the high prevalence of Lyme disease in central Virginia, he was prescribed a ten-day course of doxycycline.
The day after the clinic visit, the patient traveled to Canada. On the day before his return, he ate beef tenderloin at 6 PM, went to bed at 10 PM, and woke up around 11 PM covered with intensely pruritic hives and had the urge to urinate. He took 48 mg of liquid diphenhydramine and collapsed en route to the bathroom. He was unresponsive for 15 minutes. Emergency Medical Services (EMS) arrived and measured his supine blood pressure at 86/40 mmHg. He was treated with intravenous (IV) fluids and 50 mg of IV diphenhydramine, with complete resolution of his symptoms. Work-up in the Emergency Department (ED) was negative for myocardial infarction and stroke. Shortly after the trip, his wife incidentally read an article in a local newspaper regarding red meat ingestion causing anaphylaxis and discussed it with his primary care physician, who referred him to an allergist. The allergy/immunology work-up revealed IgE alpha gal >100 kU/L (Viracor-IBT, reference range <0.35 kU/L), specific IgE to beef 45 kU/L and to pork 53 kU/L (ImmunoCAP, Phadia, reference range <0.35 kU/L). Since the Canadian incident seven months prior, he has remained symptom-free while avoiding beef, pork and lamb. He continues to tolerate chicken, turkey, and fish without problem.
Case 2
A 54-year-old Caucasian man was seen in a tertiary allergy/immunology clinic for a history of anaphylaxis to insect stings. Notes from previous allergists indicated multiple episodes of “allergic reactions” without clear cause. Reactions involved pruritic hives, sensation of lip and tongue swelling, and occasional wheezing. He had multiple ED visits for these “allergic reactions” and has intermittently required epinephrine. On one occasion, he had prime rib for dinner and awoke at approximately 2 AM with hives on his thighs, which then became generalized. He took 25 mg of diphenhydramine and went back to bed. At 7:30 AM, he awoke with the progression of hives affecting his entire body, and with associated lip and tongue swelling. Despite additional diphenhydramine, he became dizzy and felt his throat closing. He gave himself an epinephrine injection and called 911. EMS administered another dose of epinephrine, which was repeated a third time in the ED. He was observed in the hospital for a day before he was discharged with a course of prednisone. His subsequent skin prick test was negative to beef and pork. His IgE alpha-gal was 3.94 IU/mL (University of Virginia, reference range <0.35 IU/mL), specific IgE to beef 1.5 kU/L and to pork 0.7 kU/L. He now avoids beef and pork, but has tolerated chicken, turkey and fish without incident for over a year.
Case 3
A 29-year-old Caucasian woman presented with a several year history of intermittent large hives. These occurred in the middle of the night and resolved two to three hours after taking diphenhydramine. They were often preceded by a prodrome of abdominal cramping. She recalled being bitten by ticks many years ago, but did not recall recent bites. She had two episodes in which the hives were accompanied by wheezing and resolved spontaneously after several hours. She works in a local ED, and on one occasion at work, developed abdominal cramps followed by pruritic hives on her arms five hours after eating a cheeseburger. Her coworkers noticed that her face and upper chest turned “beet red,” followed by coughing and wheezing. She was treated with albuterol nebulization, 125 mg IV solumedrol, and 0.3 mg of epinephrine IM with resolution of her symptoms. Laboratory tests showed IgE alpha-gal was 10.40 kU/L, and specific IgE to beef and pork were 5.50 kU/L and 5.10 kU/L, respectively. With abstinence from red meat, she has remained free from hives and wheezing for several months.
DISCUSSION
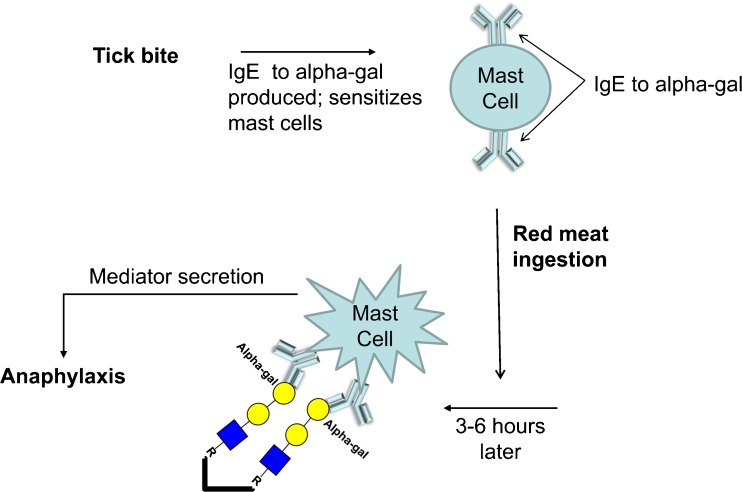
Delayed anaphylaxis to mammalian meat is a new syndrome, recognized initially in the southeastern United States. Patients present with hives and anaphylaxis three to six hours after ingestion of mammalian meat.1 This is due to circulating IgE antibody to the carbohydrate moiety alpha-gal. Individuals who are bitten by the lone star tick can become sensitized to alpha-gal. Alpha-gal is present in mammalian meat. When an alpha-gal sensitized individual eats mammalian meat, his/her IgE specific alpha-gal, attached to high affinity receptors on mast cells, binds the antigen, activating release of mediators such as histamine from mast cells that cause hives and anaphylaxis.3 (Fig. 1)
Figure 1.
Development of anaphylaxis to alpha-gal. Sensitization occurs after exposure to alpha-gal during tick bites. IgE to alpha-gal produced during sensitization binds to high affinity IgE receptors on mast cells and basophils, without causing symptoms. Re-exposure to alpha-gal in mammalian meat causes cross-linking of IgE:IgE receptor complexes on mast cells and basophils to induce secretion of various mediators that lead to anaphylaxis. (The oligosaccharide structures of the alpha-gal are shown in the symbolic depiction suggested by the Consortium of Functional Glycomics).
The journey to discovery of IgE alpha-gal started in 2005 when an oncology group in North Carolina noticed an increased incidence of anaphylaxis in patients receiving a newly developed chimeric mouse-human monoclonal antibody, cetuximab.2,4 Cetuximab is an antibody against epidermal growth factor receptor, and is used to treat colorectal, head and neck cancers. Patients who developed anaphylaxis did so within minutes of receiving their first intravenous infusion of cetuximab. The classic understanding of IgE-mediated anaphylaxis has been that prior sensitization with an allergen was a requirement for production of allergen-specific IgE. Upon re-exposure to that allergen, mast cells armed with this preformed allergen-specific IgE become activated, and release mediators that cause the signs and symptoms of immediate hypersensitivity. However, patients receiving cetuximab developed anaphylaxis after the first exposure.2
To explain the reaction after initial exposure, Chung, et al. found that IgE antibodies against cetuximab were present before the first exposure to the chimeric antibody.2 This IgE was specific for alpha-gal, an oligosaccharide present on the Fab portion of the cetuximab heavy chain.5 Alpha-gal is a carbohydrate found on non-primate mammal and tick glycoproteins, but is not made by humans. This foreign carbohydrate moiety is in part responsible for human rejection of animal xenografts; however, it had not been known to cause IgE-mediated anaphylaxis. During monoclonal antibody production using animal cell lines, oligosaccharides made by the animal cell attach to the antibody. In theory, foreign oligosaccharides such as alpha-gal can cause an allergic reaction; however, such reactions were thought to be uncommon because humans typically make IgE antibodies against protein, not carbohydrate, determinants. In classical food allergy, the IgE is directed against protein epitopes. Indeed, many of the major epitopes important in causing milk, egg, wheat, soy, peanut, tree nut, fish and shellfish allergies are known to be proteins. Alpha-gal is unique, as it is a carbohydrate recognized by IgE antibodies.
Cases of cetuximab-associated anaphylaxis have been shown to have a geographic predominance in the southeastern United States. Sensitization may be as high as 20 % in the five states of Tennessee, North Carolina, Arkansas, Missouri and Virginia, but <1 % in California and Massachusetts.6 Researchers have postulated that sensitization to alpha-gal in the Southeastern states has an association with tick bites, i.e., development of IgE alpha-gal seemed to follow tick bites in certain individuals. Thus, when a tick-bitten individual develops circulating IgE to alpha-gal, mast cells and basophils become sensitized. Later, when that individual is exposed for the first time to alpha-gal on cetuximab, a systemic allergic reaction ensues. In fact, the geographic distribution of the cetuximab-induced anaphylaxis correlates with the distribution of the lone star tick, Amblyomma americanum.3 The lone star tick differs from the blacklegged tick, Ixodes scapularis, known to cause Lyme disease, in that it is much more aggressive in both adult and larvae forms. The larvae ticks are also called seed ticks and their bites are often confused with chigger bites, which come from the larval form of the trombiculid mite.7 Bites from the lone star tick can cause severe pruritis. Long attachment, repeated attachments, and large numbers of larvae bites can all cause elevations of IgE alpha-gal to >100 kU/L.3
In addition to being a cause for cetuximab-induced anaphylaxis, IgE alpha-gal is now recognized as the cause for meat-induced delayed anaphylaxis. The connection between red meat ingestion and anaphylaxis remained elusive for several reasons: adult-onset food allergy is rare; anaphylaxis was delayed, and the commercially available skin prick test for mammalian meat was negative in the majority of cases. Of note, skin tests to fresh meat are often positive. Classic IgE-mediated anaphylaxis occurs within one hour of allergen exposure. However, anaphylaxis due to IgE antibody to alpha-gal, a carbohydrate, occurs on average three to six hours after ingestion of alpha-gal containing meat. Usually, patients have no immediate reaction to meat prior to developing delayed anaphylaxis. The delayed anaphylaxis is hypothesized to be related to the biochemistry, digestion and absorption of alpha-gal-containing glycolipids and glycoproteins.8 Carbohydrates released from digested meat are placed onto lipid particles such as chylomicrons or very low density lipoproteins.4 Some of these lipid particles, which take several hours to form, could be more potent in activating basophils or mast cells if alpha-gal moieties are presented on their surfaces.8 However, this hypothesis remains unproven. Since the article in 2009 linking IgE alpha-gal to anaphylaxis from mammalian meat,4 cases of meat-induced, delayed anaphylaxis have been reported in Texas, Georgia, South Carolina, Mississippi, Kentucky, Oklahoma, West Virginia and Spain, in addition to the original five southeast states.1,3,9
The alpha-gal story is truly a paradigm-shifting phenomenon for three distinct reasons. First, anaphylaxis occurred with the primary exposure to the glycoprotein cetuximab. Second, with regard to meat ingestion, anaphylaxis is delayed several hours rather than immediate. And third, meat-induced anaphylaxis is the first food-induced anaphylaxis due to a carbohydrate rather than a protein. Avoidance of all mammalian meat (including beef, pork, lamb, and venison) is the current recommendation for alpha-gal sensitized patients. Desensitization of alpha-gal sensitive patients has been done in the case of cancer patients requiring treatment with cetuximab, but not in the case of meat-allergic patients.
CONCLUSION
In summary, particularly in the southeastern United States where ticks are endemic, clinicians should be aware of this new syndrome when presented with a case of anaphylaxis. Exposure history beyond the traditional one-hour time frame, especially after red meat ingestion, should be obtained. Meat-induced delayed anaphylaxis usually presents as a patient waking up in the middle of the night with hives and anaphylaxis after having ingested red meat for dinner. Clinical history is key in solving these mystery cases, and a positive test for IgE against alpha-gal can help confirm the suspected diagnosis. Prevention of future life-threatening events requires dietary avoidance of all mammalian meat.
Acknowledgments
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Wolver and Sun contributed equally to this paper.
REFERENCES
- 1.Commins SP, Satinover SM, Hosen J, Mozena J, Borish L, Lewis BD, et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2009;123(2):426–33. doi: 10.1016/j.jaci.2008.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung CH, Mirakhur B, Chan E, Le QT, Berlin J, Morse M, et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-alpha-1,3-galactose. N Engl J Med. 2008;358(11):1109–17. doi: 10.1056/NEJMoa074943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Commins SP, James HR, Kelly LA, Pochan SL, Workman LJ, Perzanowski MS, et al. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2011;127(5):1286,93.e6. doi: 10.1016/j.jaci.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Commins SP, Platts-Mills TA. Anaphylaxis syndromes related to a new mammalian cross-reactive carbohydrate determinant. J Allergy Clin Immunol. 2009;124(4):652–7. doi: 10.1016/j.jaci.2009.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qian J, Liu T, Yang L, Daus A, Crowley R, Zhou Q. Structural characterization of N-linked oligosaccharides on monoclonal antibody cetuximab by the combination of orthogonal matrix-assisted laser desorption/ionization hybrid quadrupole-quadrupole time-of-flight tandem mass spectrometry and sequential enzymatic digestion. Anal Biochem. 2007;364(1):8–18. doi: 10.1016/j.ab.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 6.O’Neil BH, Allen R, Spigel DR, Stinchcombe TE, Moore DT, Berlin JD, et al. High incidence of cetuximab-related infusion reactions in Tennessee and North Carolina and the association with atopic history. J Clin Oncol. 2007;25(24):3644–8. doi: 10.1200/JCO.2007.11.7812. [DOI] [PubMed] [Google Scholar]
- 7.Chiggers, HYG-2100-98 [Internet]. Columbus, Ohio: Ohio State University Extension; 2007 [updated October 08, 2007; cited 4/30/2012]. Available from: http://ohioline.osu.edu/hyg-fact/2000/2100.html.
- 8.Commins SP, Platts-Mills TA. Allergenicity of carbohydrates and their role in anaphylactic events. Curr Allergy Asthma Rep. 2010;10(1):29–33. doi: 10.1007/s11882-009-0079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nunez R, Carballada F, Gonzalez-Quintela A, Gomez-Rial J, Boquete M, Vidal C. Delayed mammalian meat-induced anaphylaxis due to galactose-alpha-1,3-galactose in 5 european patients. J Allergy Clin Immunol. 2011;128(5):1122,4.e1. doi: 10.1016/j.jaci.2011.07.020. [DOI] [PubMed] [Google Scholar]