ABSTRACT
BACKGROUND
A key objective of the Medicare program is to reduce risk of financial catastrophe due to out-of-pocket healthcare expenditures. Yet little is known about cumulative financial risks arising from out-of-pocket healthcare expenditures faced by older adults, particularly near the end of life.
DESIGN
Using the nationally representative Health and Retirement Study (HRS) cohort, we conducted retrospective analyses of Medicare beneficiaries’ total out-of-pocket healthcare expenditures over the last 5 years of life.
PARTICIPANTS
We identified HRS decedents between 2002 and 2008; defined a 5 year study period using each subject’s date of death; and excluded those without Medicare coverage at the beginning of this period (n = 3,209).
MAIN MEASURES
We examined total out-of-pocket healthcare expenditures in the last 5 years of life and expenditures as a percentage of baseline household assets. We then stratified results by marital status and cause of death. All measurements were adjusted for inflation to 2008 US dollars.
RESULTS
Average out-of-pocket expenditures in the 5 years prior to death were $38,688 (95 % Confidence Interval $36,868, $40,508) for individuals, and $51,030 (95 % CI $47,649, $54,412) for couples in which one spouse dies. Spending was highly skewed, with the median and 90th percentile equal to $22,885 and $89,106, respectively, for individuals, and $39,759 and $94,823, respectively, for couples. Overall, 25 % of subjects’ expenditures exceeded baseline total household assets, and 43 % of subjects’ spending surpassed their non-housing assets. Among those survived by a spouse, 10 % exceeded total baseline assets and 24 % exceeded non-housing assets. By cause of death, average spending ranged from $31,069 for gastrointestinal disease to $66,155 for Alzheimer’s disease.
CONCLUSION
Despite Medicare coverage, elderly households face considerable financial risk from out-of-pocket healthcare expenses at the end of life. Disease-related differences in this risk complicate efforts to anticipate or plan for health-related expenditures in the last 5 years of life.
KEY WORDS: Medicare, out-of-pocket spending, healthcare expenses, end-of-life
INTRODUCTION
A major goal of the Medicare legislation enacted in 1965 was to protect elderly citizens from financial risk. As Lyndon Johnson declared at the signing of the legislation, “No longer will illness crush and destroy the savings that [older Americans] have so carefully put away over a lifetime.”1 Since that time, healthcare costs have risen dramatically, as have Medicare expenditures. Some proposals seeking to rein in Medicare cost growth include provisions by which the elderly would pay a larger share of their healthcare costs out-of-pocket. While some prior research has suggested relatively little financial risk in the Medicare population on average,2,3 more recent studies point to a significant degree of financial risk in the last year of life.4,5 However, little is known about the extent of late life financial risk, particularly the risk associated with the death of a household head or spouse. Nor do we know how such spending varies by type of disease.
In this paper, we consider the financial risk faced by Medicare beneficiaries during the 5 years prior to death (or the death of a spouse), and how these risks vary by socioeconomic and marital status. Specifically, we examine the likelihood of spending all or more than half of one’s baseline assets on health-related expenses, and the extent to which these risks vary by marital status or type of disease. We use the Health and Retirement Study (HRS),6 a rich longitudinal cohort study of U.S. adults age 50 years and older, that includes detailed information on out-of-pocket spending as well as information about socioeconomic status, health and demographic characteristics and cause of death.
METHODS
We sampled all HRS decedents identified by a post-death, or “Exit”, interview, completed by a proxy between 2002 and 2008. Serial “Core” interviews are conducted every 2 years and response rates for each interview wave have exceeded 86 %. During each interview cycle, HRS identifies participants who died since the last Core interview and conducts Exit interviews with proxies knowledgeable about the deceased participant (response rate = 93 %). Both the Core and Exit interviews include the participant’s demographic, social, medical, functional and detailed financial characteristics. Prior analyses have found the validity of HRS wealth and spending data to be high.5,7–9 In total, there were 5,366 decedents identified across the 6 year time frame. In order to limit our study to those older adults with Medicare coverage during the last 5 years of life, we excluded respondents who were less than 70 years of age at time of death (n = 1,044) and those reporting no Medicare coverage at the first interview within the measurement period (n = 538). We also excluded those whose 5 year look-back period extended before 1998 (n = 405) and respondents missing at least one Core survey wave during the 5 years preceding death (n = 170), because we could not accurately measure out-of-pocket spending for these individuals. The final sample included 3,209 subjects. While the sample of end-of-life Medicare enrollees are older than the general population in the 1998 Medicare Current Beneficiary Study, other characteristics such as proportion female, race, education, income, Medicaid coverage, and burden of chronic disease were similar.10
The presence of a spouse and potential caregiver may attenuate out-of-pocket spending or exacerbate family burden if expenditures are positively correlated across spouses. Therefore, we considered subgroups by marital status: those who remained single (n = 1,750) or married (n = 713) throughout the 5 years prior to the death, and those who experienced a change in marital status during this period (n = 746).
Health-related out-of-pocket spending is measured every 2 years in the HRS Core interviews and again in the Exit interview, where it is reported by the decedent’s surviving spouse, family members or other knowledgeable proxy. Specific categories of spending include: insurance, hospital, physician, medication, nursing home, hired helpers, in-home medical care and other expenses. There were a few categories asked only in the Core, but not in the Exit interview (e.g., dental services), and, conversely, those asked in the Exit interview only (e.g., spending to improve home care, such as ramps or a handicap-accessible van and hospice care).
For some of the out-of-pocket expenditure questions in both the Core and Exit interviews, respondents provided incomplete answers or no answers at all. When respondents failed to provide a dollar amount, the HRS branched into more general questions, such as “Was it more than or less than $1,000?” By successively asking these questions, it became possible to bracket estimated spending, thereby allowing imputed values consistent with each bracket to be estimated, as described elsewhere.9
Total out-of-pocket expenses were summed across all categories and scaled to comprise a consistent 60-month (5 year) period. The study period was defined for each individual by the subject’s date of death and the 60 months preceding that date. In our sample, the Exit interviews reflected a time period ranging from 1 to 32 months (mean 14 months). Therefore, we included the Exit and Core interviews that captured a 60-month period counting back from the subject’s date of death. If the surveys including the Exit survey exceeded 60 months, the spending was adjusted to a 60-month period by prorating expenses reported in the earliest HRS interview, i.e. the time period farthest from death and thus likely to have the lowest cost. For example, based upon the subject’s date of death, the Exit survey may report spending for the last 10 months of life. This amount would be added to the spending reported in the preceding two Core interviews, and together account for 58 months of expenditures. The spending reported in the third preceding Core interview (the interview furthest from death) would then be prorated to augment the previous 58 months up to the common 60-month period. For subjects survived by a spouse, we also measured the spouse’s health-related out of pocket expenses during the same time period, and reported combined spending as the married couple’s total out-of-pocket burden. To capture spousal spending limited to the same length of time for which the decedent was alive, we prorated the spouse’s reported spending based upon the subject’s date of death. For example, if the subject died 8 months into a 24-month span between the spouse’s two HRS Core interviews, we allocated 8/24th of the spouse’s reported health care expenditures in that final survey period to the married couple’s total out-of-pocket burden.
We measured insurance status (Medicare, Medicaid, Medigap/Private/Retiree, Long term care, and Veterans Affairs (VA) policies) and total assets at the first Core interview within the study period, to correspond with the outset of our measurement of spending. Our measure of annual income was the average across the Core interviews within the study period. We used the Consumer Price Index (2008 US Dollars) to adjust all financial measures for inflation. As well, we obtained self-reported medical conditions, nursing home as primary residence, and ability to complete activities of daily living (ADLs)(e.g. bathing, dressing, etc.) from the last Core interview, completed on average approximately 12 months prior to death. The HRS obtains date and cause of death from the National Death Index.6
The introduction of Part D in Medicare has helped to limit the extent of very high expenses for pharmaceuticals. To approximate the benefit of this new source of insurance, we estimate adjusted spending as if there had been a Part D limit on overall spending during the entire period of analysis 1998–2006 by capping any drug spending at the amount ($3,600/year) that an individual would spend in 2008, after the standard “doughnut hole” out-of-pocket provision.
RESULTS
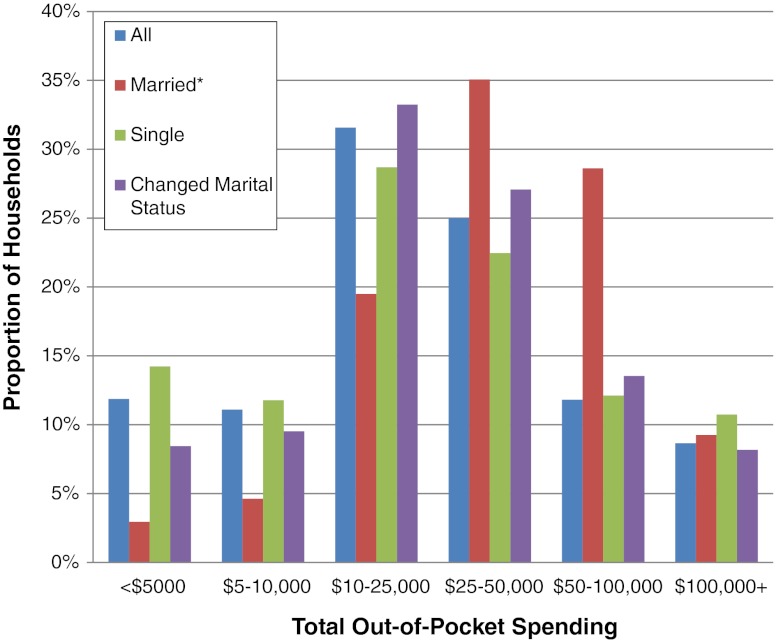
The mean out-of-pocket healthcare spending in the last 5 years was $38,688 (95 % CI $36,868, $40,508), with the median spending $22,885 (95 % CI $21,988, $23,732). The 5th percentile was $1,462, the 90th percentile was $89,106, and the 95th percentile was $139,077 (Range: 0 to $890,609). The distribution of spending is shown by subject group (all, married, single, and those who changed marital status) in Figure 1. More than three-fourths of households spent at least $10,000 during the 5-year period, while 11 % of single and 9 % of married households spent in excess of $100,000. Table 1 reports subjects’ characteristics across quartiles of total out-of-pocket spending. Table 1 also displays the characteristics of a subset of the top quartile: those in the top 10 % of total spending. Decedents in the lowest quartile of spending were more likely to belong to a racial or ethnic minority group (42 %), have Medicaid insurance coverage (44 %), have the lowest mean income and total assets ($22,208 and $106,121, respectively), and lack private insurance (84 %). Those in the highest quartile of spending were more likely to be older (mean age 86 years), Non-Hispanic white (91 %), a nursing home resident (41 %), require assistance with ADLs (61 %), and have dementia or a memory-related disease (32 %). The characteristics of those in the lowest quartile were all significantly different (p values < 0.05) from those in the highest quartile, except for congestive heart failure (p = 0.21), hypertension (p = 0.31), and lung disease (p = 0.08). The proportion spent on each sub-category of expenses varied across quartiles of total out-of-pocket expenses (data not shown). The lowest 75 % spent on average $17,662, with the greatest proportion of spending on insurance (45 %) and drugs (24 %). Among those in the top 25 %, average out-of-pocket spending was $101,791, and for the subset in the highest 10 %, out-of-pocket expenses averaged $163,121, with nursing home expenditures accounting for 48 % and 58 % of total spending, respectively.
Figure 1.
Distribution of out-of-pocket spending in the last 5 years of life. Legend: *Expenditures for married include expenses of both spouse and household head.
Table 1.
Total Out-of-Pocket Spending Over 5 Years by Quartile and Top 10 % of Spending
| Full sample (n = 3,209) | Q1 (n = 803) | Q2 (n = 802) | Q3 (n = 802) | Q4 (n = 802) | 90 % (n = 321) | |
|---|---|---|---|---|---|---|
| Total Out-of-Pocket, median (95 % CI) | $22,885 ($21,988, $23,732) | $5,286 ($4,810, $5,695) | $16,346 ($415,963, $17,091) | $30,015 ($39,352, $30,853) | $ 75,862 ($73,400, $79,994) | $ 139,077 ($129,521, $149,265) |
| Total Out-of-Pocket, mean (95 % CI) | $ 38,688 ($36,868, $40,508) | $5,163 ($4,929, $5,397) | $16,756 ($16,514, $16,998) | $ 31,084 ($30,687, $31,480) | $ 101,791 ($96,716, $106,866) | $ 163,121 ($154,034, $172,207) |
| Total Assets, median (95 % CI) | $106,555 ($99,731, $114,752) | $21,077 ($16,023, $29,364) | $113,120 ($103,234, $129,321) | $ 168,499 ($144,334, $192,434) | $ 185,501 ($160,460, $210,836) | $ 184,305 (140,798, $227,470) |
| Total Assets, mean (95 % CI) | $290,995 ($268,028,$313,961) | $106,121 ($89,275, $122,968) | $229,498 ($201,882, $257,114) | $ 380,885 ($332,101, $429,668) | $ 447,705 ($379,244, $516,165) | $ 440,430 ($340,388, $540,472) |
| Annual Income, median (95 % CI) | $22,024 ($21,200, $22,866) | $13,410 ($12,897, $13,995) | $21,645 ($20,591, $23,261) | $ 26,834 ($24,2984, $28,626) | $ 28,000 ($26,221, $29,357) | $ 26,185 ($22,487, $28,754) |
| Annual Income, mean (95 % CI) | $32,514 ($30,812, $34217) | $22,208 ($18,168, $26249) | $31,038 ($28,813, $33,263) | $ 38,476 ($34,448, $42,504) | $ 38,348 ($35,512, $41,183) | $ 35,941 ($32,458, $39,423) |
| Out-of-pocket (5 years) / Assets, median | 0.17 | 0.08 | 0.12 | 0.17 | 0.43 | 0.65 |
| Age at death, mean (SD) | 84.3 (7.6) | 83.7 (8.0) | 83.3 (7.4) | 83.9 (7.3) | 86.4 (7.3) | 88.7 (7.1) |
| Female, n (%) | 1830 (57.0) | 462 (57.5) | 418 (52.1) | 443 (55.2) | 507 (63.2) | 235 (73.2) |
| Race: | ||||||
| Non-Hispanic White, n (%) | 2528 (78.8) | 466 (58.0) | 622 (77.6) | 708 (88.3) | 732 (91.3) | 303 (94.4) |
| Black, n (%) | 415 (12.9) | 180 (22.4) | 121 ( 15.1) | 69 (8.6) | 45 (5.6) | 11 (3.4) |
| Hispanic, n (%) | 199 (6.2) | 115 (14.3) | 43 (5.4) | 22 (2.7) | 19 (2.4) | NA* |
| Other, n (%) | 67 (2.1) | 42 (5.2) | 16 (2.0) | NA* | 6 (0.7) | 7 (2.2) |
| Insurance: | ||||||
| Medicare, n (%) | 3209 (100) | 803 (100) | 802 (100) | 802 (100) | 802 (100) | 321 (100) |
| Medicaid, n (%) | 532 (16.6) | 351 (43.7) | 74 (9.2) | 54 (6.7) | 53 (6.6) | 18 (5.6) |
| Private/Medigap, n (%) | 1194 (37.2) | 131 (16.3) | 312 (38.9) | 380 (47.4) | 371 (46.3) | 133 (41.4) |
| Long-Term Care, n (%) | 252 (7.9) | 25 (3.1) | 33 (4.1) | 87 (10.9) | 107 (13.3) | 20 (6.2) |
| VA, n (%) | 104 (3.2) | 44 (5.5) | 22 (2.7) | 19 (2.4) | 19 (2.4) | NA* |
| Nursing Home Residence, n (%) | 679 (21.2) | 178 (22.2) | 82 (10.2) | 89 (11.1) | 330 (41.2) | 196 (61.1) |
| Independent ADLs, n (%) | 1784 (55.6) | 438 (54.6) | 533 (66.5) | 501 (62.5) | 312 (38.9) | 75 (23.4) |
| Medical Conditions (self/proxy report) | ||||||
| Diabetes, n (%) | 790 (24.6) | 239 (29.8) | 188 (23.4) | 187 (23.3) | 176 (22.0) | 65 (20.3) |
| Lung Disease, n (%) | 568 (17.7) | 153 (19.1) | 147 (18.3) | 149 (18.6) | 119 (14.8) | 42 (13.1) |
| Hypertension, n (%) | 1954 (60.9) | 508 (63.3) | 485 (60.5) | 483 (60.2) | 478 (59.6) | 179 (55.8) |
| Heart Disease, n (%) | 1477 (46.0) | 332 (41.3) | 364 (45.4) | 404 (50.4) | 377 (47.0) | 128 (39.9) |
| Congestive Heart Failure, n (%) | 425 (13.2) | 100 (12.5) | 98 (12.2) | 103 (12.8) | 124 (15.5) | 42 (13.1) |
| Cancer, n (%) | 756(23.6) | 150 (18.7) | 184 (22.9) | 228 (28.4) | 194 (24.2) | 73 (22.7) |
| Stroke, n (%) | 691 (21.5) | 176 (21.9) | 152 (19.0) | 152 (19.0) | 211 (26.3) | 92 (28.7) |
| Falls, n (%) | 1587 (49.5) | 373 (46.5) | 330 (41.2) | 399 (49.8) | 485 (60.5) | 206 (64.2) |
| Dementia/Memory disease, n(%) | 651 (20.3) | 167 (20.8) | 102 (12.7) | 127 (15.8) | 255 (31.8) | 136 (42.4) |
VA = Veterans Affairs, ADLs = Activities of daily living
P values for comparisons between 1st and 4th quartiles are all <0.05, except Congestive heart failure (p = 0.21), Hypertension (p = 0.31), and Lung disease (p = 0.08).
*Not able to report cell size with n <5 per HRS Restricted Data Use Agreement, therefore grouped with “Other”
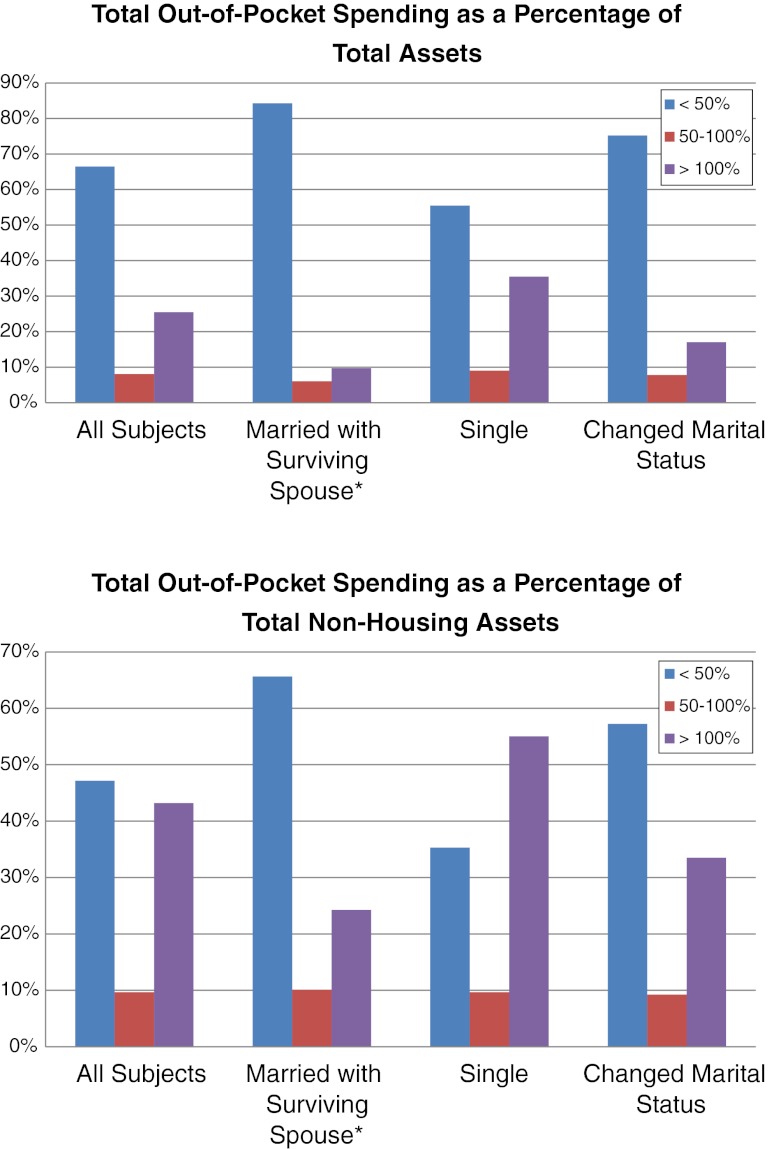
Considering out-of-pocket spending as a proportion of wealth, 817 (25 %) subjects experienced total out-of-pocket spending over the last 5 years of life that exceeded total household assets at the start of that period; and total spending among 1,386 (43 %) subjects surpassed their non-housing assets (Fig. 2). Stratified by marital status, 69 (10 %) of subjects survived by a spouse spent 100 % or more of their total household assets, while 621 (35 %) of unmarried subjects experienced this level of spending. One hundred seventy-three (24 %) of those with a surviving spouse accrued expenses greater than 100 % of non-housing assets, as compared to 963 (55 %) of those who were single during the study period.
Figure 2.
Out-of-pocket spending over 5 years prior to death as a percentage of household assets. Legend: *Considers only subject’s spending (not spousal out-of-pocket spending).
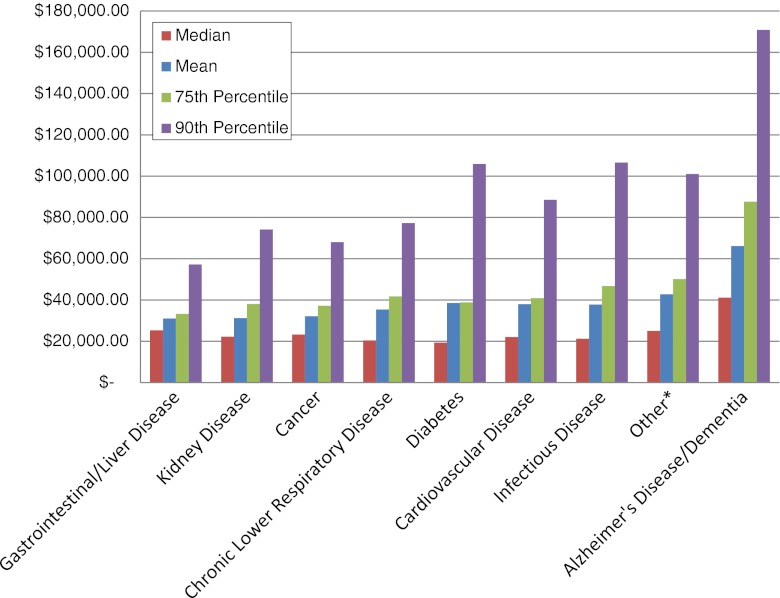
Finally, we examined total out-of-pocket spending by cause of death. Figure 3 shows median, mean, 75th percentile and 90th percentile spending by cause of death, ranging from gastrointestinal and liver disease $31,069 average spending (median $25,365), to Alzheimer’s disease $66,155 average spending (median $41,171). Nursing home expenses accounted for 56 % of average spending among those with Alzheimer’s disease.
Figure 3.
Out-of-pocket spending over 5 years prior to death, by cause of death. Legend: *Other causes of death (e.g., Accidents).
DISCUSSION
The Medicare program provides nearly universal health care coverage to the population ages 65 years or older. However, Medicare does not cover the full financial cost of poor health among the elderly population. Many enrollees must pay out-of-pocket for their copayments and deductibles and, more importantly, Medicare does not cover a variety of services particularly valuable for those with chronic diseases or a life-limiting illness, including most eye glasses, hearing aids, homecare services and equipment, and non-rehabilitative nursing home care. In this paper, we used the Health and Retirement Study to measure out-of-pocket health-related expenditures in the 5 years prior to the death of a household head or spouse. Even for the median household, spending over this time-period was $22,885, equivalent to 17 % of median household assets at the outset of the 5-year period, while one-in-four subjects spent more than their total baseline household assets. A breakdown by the components of spending indicates that nursing home costs comprise the largest fraction of expenditures for those with out-of-pocket costs in the upper quartile of spending. Expenditures also vary systematically with cause of death. Out-of-pocket spending for those with dementia is more than twice the average spending of those dying from gastrointestinal disease or cancer. Thus, advanced dementia represents an additional and unavoidable financial risk, creating further challenges for aging baby-boomers seeking to save against future health costs.
It is not entirely clear how the Patient Protection and Affordable Care Act (PPACA) will affect future out-of-pocket expenditures.11 The Community Living Assistance Services and Supports (CLASS) Act, originally a part of the PPACA, was designed to provide public voluntary long-term care insurance, and thus could have helped to shield the elderly from catastrophic out-of-pocket costs.12 However, this component of the legislation was dropped in 2011, owing to challenges surrounding financial viability. Other proposals designed as alternatives to the PPACA have focused on voucher plans with greater cost-sharing,13 but such plans would most likely increase, not decrease, out-of-pocket medical expenditures for the Medicare population.14
There are several limitations to this study. First, it is difficult to determine whether some sources of spending are medical necessities or “luxury” goods. For many of these expenditures, the line is difficult to draw, since we might expect better quality care in more expensive nursing homes that also feature higher staffing levels, better meals, more activities, and more pleasant accommodations.15–17 But the reverse of this question is equally important: whether those with less wealth are constrained from buying needed health care. There is evidence from one randomized trial suggesting better survival with specialized home nursing following cancer treatment,18 but those results may not be generalizable to all types of spending or to all diseases; nor would they be expected to hold indefinitely as spending on nursing homes increased.
These results are also descriptive and may be affected by sampling bias, whereby those with greater wealth enjoy better health, live longer and incur costs for long term care; while those with low wealth are more likely to die younger with chronic conditions, such as diabetes. Wealth may also be an incomplete measure of financial ability to pay, since households may also be able to draw on income to help pay out-of-pocket expenses. Also, this retrospective study does not allow us to predict future end-of-life health-related expenditures facing aging Baby Boomers. However, predicted increases in health care spending, along with fiscal pressures created by an aging population and increasing prevalence of debility and dementia, makes it likely that out-of-pocket expenditures will continue to rise.
There is also likely to be some measurement error in the reported out-of-pocket expenditures, particularly in the Exit interviews, where spending may be reported by a child or other individual who was not responsible for paying the bills. Additionally, because most questions ask about spending since the prior survey (approximately 2 years), but questions about insurance premiums ask respondents to report on a monthly basis, some respondents may misreport the amount. Finally, these data do not account for indirect costs, such as changes in labor market participation of a spouse or child or the implicit time costs incurred by other unpaid caregivers.19
Despite these limitations, the evidence from the HRS demonstrates a large and often persistent health-related financial shock that varies according to disease and with the largest average financial burden associated with dementia. Whether these increasing financial burdens—even among those with full Medicare coverage—will create renewed interest in a publicly sponsored long-term care program remains to be seen. Nonetheless, uninsured out-of-pocket expenditures are likely to continue their growth, whether because of secular growth in health care spending, or a greater reliance on copayments and deductibles to scale back Medicare cost growth. As more Baby Boomers retire, a new generation of widows or widowers could face a sharply diminished financial future as they confront their recently-depleted nest egg following the illness and death of a spouse.20,21
Acknowledgements
Funders
Amy Kelley receives support from the Hartford Foundation, Hartford Center of Excellence Scholars Award and the Claude D. Pepper Older Americans Independence Center at Mount Sinai (NIA-1P30AG28741-01). Sean Fahle is supported by (1 T32-AG033533). Jonathan Skinner is supported National Institute on Aging (PO1-AG19783). Funders did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Amy Kelley and Qingling Du had access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest
Jonathan Skinner lists several financial interests on his disclosure form, none of which he believes represents a conflict for this manuscript. The other authors have no conflicts of interest.
REFERENCES
- 1.Beschloss M. Our Documents: 100 Milestone Documents from the National Archives. New York, NY: Oxford University Press; 2006. [Google Scholar]
- 2.French E, Jones JB. On the distribution and dynamics of health care costs. J Appl Econometrics. 2004;19(6):705–721. doi: 10.1002/jae.790. [DOI] [Google Scholar]
- 3.De Nardi M, French E, Jones JB. Why do the elderly save? The role of medical expenses. J Polit Econ. 2010;118(1):39–75. doi: 10.1086/651674. [DOI] [Google Scholar]
- 4.Baicker K, Goldman D. Patient cost-sharing and health care spending growth. J Econ Perspect. 2011;25(2):47–68. doi: 10.1257/jep.25.2.47. [DOI] [PubMed] [Google Scholar]
- 5.Marshall S, McGarry K, Skinner J. The risk of out-of-pocket health care expenditures at the end of life. In: Explorations in the Economics of Aging. Chicago, IL: University of Chicago Press; 2011.
- 6.Health and Retirement Study. http://hrsonline.isr.umich.edu/ Accessed July 31, 2012.
- 7.Goldman DP, Zissimopoulos J, Lu Y. Medical Expenditure Measures in the Health and Retirement Study. Forum for Health Economics & Policy. 2011;14:3. doi: 10.2202/1558-9544.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venti S. Economic Measurement in the Health and Retirement Study. Report to the Data Monitoring Committee, Health and Retirement Study; National Institute on Aging; January, 2011.
- 9.Marshall S, McGarry KM, Skinner JS. The Risk of Out-of-Pocket Health Care Expenditure at End of Life. National Bureau of Economic Research, Working Paper 16170. July 2010. [PMC free article] [PubMed]
- 10.Medicare Current Beneficiaries Study: Details for Section: 1998 Characteristics and Perceptions of the Medicare Population. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/Data-Tables-Items/CMS1253269.html. Accessed July 31, 2012.
- 11.Patient Protection and Affordable Care Act. http://www.dol.gov/ebsa/healthreform/. Accessed July 31, 2012.
- 12.Title VIII. Community Living Assistance Services and Supports Act (CLASS act) | The White House http://www.whitehouse.gov/health-care-meeting/proposal/titleviii. Accessed July 31, 2012.
- 13.Paul Ryan: The GOP path to prosperity - WSJ.com http://online.wsj.com/article/SB10001424052748703806304576242612172357504.html. Published April 5, 2011. July 31, 2012.
- 14.Ryan’s Medicare voucher plan draws democrat opposition - AARP Bulletin. http://www.aarp.org/health/medicare-insurance/info-06-2011/paul-ryan-medicare-voucher-plan.html. Accessed July 31, 2012.
- 15.Anderson RA, Hsieh PC, Su HF. Resource allocation and resident outcomes in nursing homes: Comparisons between the best and worst. Res Nurs Health. 1998;21(4):297. doi: 10.1002/(SICI)1098-240X(199808)21:4<297::AID-NUR3>3.0.CO;2-A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castle NG, Engberg J. The influence of staffing characteristics on quality of care in nursing homes. Health Serv Res. 2007;42(5):1822–1847. doi: 10.1111/j.1475-6773.2007.00704.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castle NG, Anderson RA. Caregiver staffing in nursing homes and their influence on quality of care: Using dynamic panel estimation methods. Med Care. 2011;49(6):545–552. doi: 10.1097/MLR.0b013e31820fbca9. [DOI] [PubMed] [Google Scholar]
- 18.McCorkle R, Strumpf NE, Nuamah IF, et al. A specialized home care intervention improves survival among older post-surgical cancer patients. J Am Geriatr Soc. 2000. [DOI] [PubMed]
- 19.McGarry K. Does Caregiving Affect Work? Evidence Based on Prior Labor Force Experience. In: Wise D, ed. Health Care Issues in the United States and Japan. Chicago, IL: University of Chicago Press.
- 20.McGarry K, McGarry K. Medicare gaps and widow poverty. Soc Sec Bull. 2005;66:58. [PubMed] [Google Scholar]
- 21.McGarry K, Schoeni RF. Widow Poverty and Out-of-Pocket Medical Expenditures Near the End of Life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(3):S160. doi: 10.1093/geronb/60.3.S160. [DOI] [PubMed] [Google Scholar]