Abstract
The monomer of influenza haemagglutinin is synthesized as a single polypeptide precursor that during maturation is cleaved by proteases into two active subunits. Other studies have demonstrated that the human Transmembrane Protease Serine 2 (TMPRSS2) can cleave the HA of human seasonal influenza viruses. Consequently, we have investigated the use of human Transmembrane Protease Serine 2 to produce high titre influenza haemmagglutinin (HA) lentiviral pseudotypes from Group 2 influenza viruses. Such pseudotypes represent powerful and safe tools to study viral entry and immune responses. Influenza pseudotype particles are obtained by co-transfecting human embryonic kidney HEK293T/17 cells using plasmids coding for the influenza HA, HIV gag-pol and a lentiviral vector incorporating firefly luciferase. However, in order to produce Group 2 pseudotypes, it was necessary to co-transfect a plasmid expressing the TMPRSS2 endoprotease, to achieve the necessary HA cleavage for infective particle generation. These lentiviral pseudotypes were shown to transduce HEK293T/17 cells with high efficiency. This demonstrates that TMPRSS2 is necessary for the functional activation, in vitro, of both the HA of human seasonal influenza and other Group 2 HA influenza strains. Additionally, we show that the Group 2 influenza pseudotype particles can be used as surrogate antigens in neutralization assays and are efficiently neutralized by corresponding influenza virus reference sera. These data demonstrate that the viral pseudotype system is a powerful method for serological surveillance of a wide range of influenza viruses.
Keywords: Haemagglutinin, protease cleavage, antibody response, pseudotype serology
INTRODUCTION
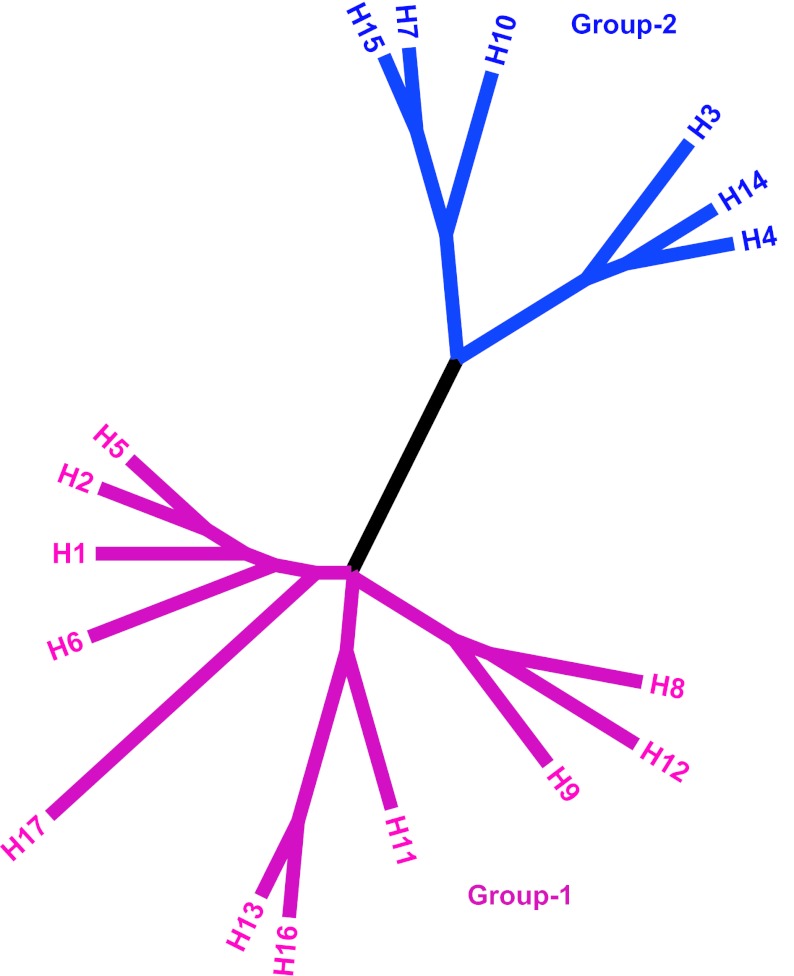
Influenza A viruses are disease-causing agents in humans and animals, which have a reservoir in wild birds, especially Charadriiformes and Anseriformes (Olsen et al, 2006). Influenza A viruses are classified using the antigenic characteristic of the envelope glycoproteins haemagglutinin (HA) and neuraminidase (NA). Currently, using antigenic characteristics and phylogenetic analysis, 17 different haemagglutinin subtypes are recognized and are divided into two lineages: Group-1 and Group-2 (Figure 1) (Röhm et al, 1996; Fouchier et al, 2005; Tong et al, 2012). Of the 17 haemagglutinin subtypes only two, H1 and H3, cause seasonal epidemics in the human population. However, viruses belonging to other subtypes have shown the capacity for avian-to-human transmission and their spread needs to be monitored in avian and mammalian populations for pandemic preparedness (Peiris, 2009). This can be achieved using serological and molecular biological diagnostic methods that permit the identification of haemagglutinin subtypes (Cattoli and Terregino, 2008). The haemagglutinin is the major target of antibody response against influenza viruses. It is the trimeric envelope glycoprotein necessary for entry into susceptible cells. Each HA monomer is produced as a single polypeptide precursor, HA0, that during maturation is cleaved into two subunits, HA1 and HA2. This process is a necessary step to acquire fusion activity and infectivity of influenza. When multiple basic amino acid residues (lysine and arginine) are situated immediately before the cleavage arginine, the haemagglutinin is cleaved by ubiquitously expressed subtilisin-like endoproteases, such as furin. This determines the virulence and lethality for several avian species observed in the high pathogenicity avian influenza (HPAI) strains H5 and H7 (Garten and Klenk, 2008). On the other hand, cleavage at the single arginine (or lysine) amino acid at the HA cleavage site of low pathogenicity avian influenza (LPAI) strains, human and mammalian influenza viruses is thought to be mediated by tissue-specific proteases. Recently, different human lung proteases belonging to the serine protease family that are able to cleave the haemagglutinin of human influenza strains were identified: Transmembrane Protease Serine 2 and 4 (TMPRSS2/4) and Human Airway Trypsin-like protease (HAT) (Böttcher et al, 2006; Bertram et al, 2010). To date, the proteases that cleave the haemagglutinin of LPAI strains are still unidentified. To study the HA cleavage of human seasonal strains (H1 and H3) by TMPRSS2, HAT and their avian and mammalian homologous proteases, pseudotype lentiviral particles are a suitable approach (Bertram et al, 2012). Influenza pseudotype particles (pp) represent powerful and safe tools to study both the antibody response directed against the influenza haemagglutinin and the viral entry mechanism (Garcia and Lai, 2011). In the present study, we use a pseudotype generation system to investigate human TMPRSS2 and its role in mediating the conversion of human and LPAI HA0s into their active forms, and we show that the pseudotypes produced can be efficiently used in a virus neutralization assay.
Figure 1.
Phylogenetic relationship of influenza A haemagglutinin subtypes. Evolutionary analysis involving 17 amino acid sequences representing HAs from each subtype was conducted in MEGA5 (Tamura et al, 2011). The evolutionary history was inferred using the Neighbor-Joining method, computing the evolutionary distances utilizing the Dayhoff matrix-based method. All positions with less than 100% site coverage were eliminated. Colours were added with FigTree software (http://tree.bio.ed.ac.uk/).
MATERIALS AND METHODS
Haemagglutinin expressing plasmids
The haemagglutinin of A/Udorn/307/1972 (H3N2) and of A/chicken/Italy/1082/1999 (H7N1) were cloned in the expression plasmid pI.18 using methodology described elsewhere (Temperton et al, 2007). The haemagglutinin of A/duck/Czechoslovakia/1956 (H4N6), A/chicken/Germany/N49 (H10N7), A/mallard/Astrakhan/263/1982 (H14N5), A/shearwater/West Australia/2576/1979 (H15N9) were custom synthesised and codon-optimized (Genscript), and cloned into the phCMV1 vector (Genlantis) as previously reported (Corti et al, 2011).
Reference sera
Reference sheep serum against A/England/427/1988 (H3N2) was provided by the National Institute for Biological Standards and Controls (NIBSC, United Kingdom). World Organisation for Animal Health (OIE) avian reference hyperimmune sera against H3N8, H4N8, H14N5, H10N1 and H15N9 were produced in specific pathogen-free chickens as described elsewhere (Cattoli et al, 2011). Reference avian sera against A/African starling/England/983/1979 (H7N1), A/chicken/Wales/1306/2007 (H7N2), A/chicken/England/4054/2006 (H7N3), A/England/268/1996 (H7N7) were provided by the Animal Health and Veterinary Laboratories Agency (AHVLA).
Cell line
Human embryonic kidney HEK293T/17 cells were cultured in Dulbecco's Modified Eagle Medium (DMEM) with Glutamax and high glucose (Gibco, Invitrogen, UK), supplemented with 10% (v/v) fetal bovine serum (Sigma) and 1% (v/v) penicillin/streptomycin (Fisher Bioreagents).
Pseudotype lentiviral particles production and titration
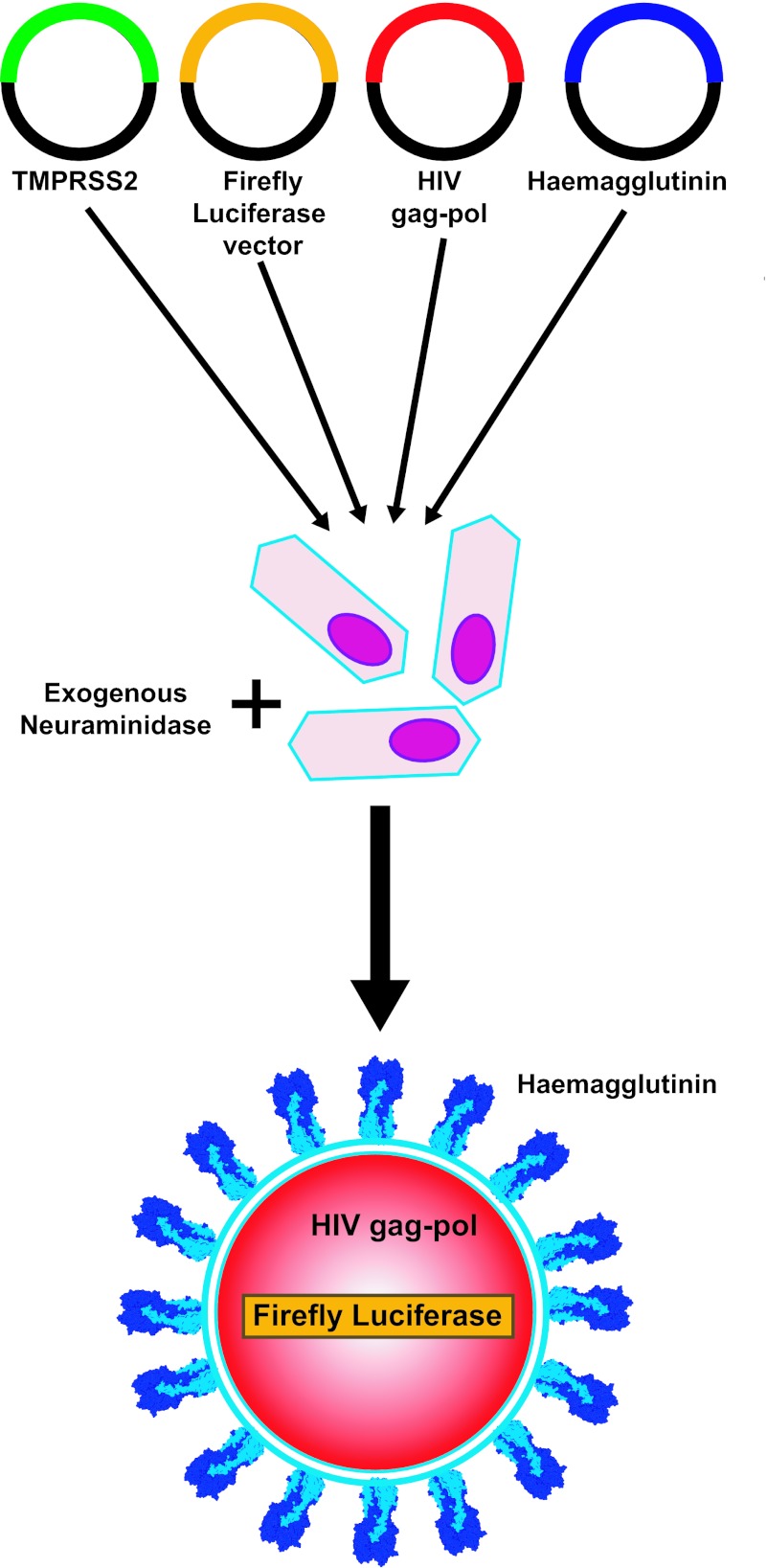
Lentiviral pseudotyped particles were produced as described previously (Temperton et al, 2007; Corti et al, 2011). Briefly, the HIV gag-pol plasmid p8.91, the firefly luciferase expressing plasmid pCSFLW, the HA expressing plasmid and the pCAGGS-TMPRSS2 (Böttcher et al, 2006) were co-transfected into human embryonic kidney HEK293T/17 cells using Fugene-6 transfection reagent (Roche, UK). After 24 hours incubation, 1U of recombinant neuraminidase from Clostridium perfringens (Sigma) was added (Figure 2) to facilitate pseudotype exit from the producer cells. Forty-eight hours post-transfection supernatant was harvested, filtered through 0.45 μm filters and stored at -80°C. Pseudotyped particles were also produced in the absence of pCAGGS-TMPRSS2 plasmid (ΔTMPRSS2). Titration of the pseudotype particles was performed by transducing HEK293T/17 cells (1 × 104 cells/well), with 50 μl of neat pseudotype supernatant and subsequent 1:2 serial dilutions.
Figure 2.
Schematic representation of Group-2 influenza pseudotype production. Plasmids encoding HIV gag pol, the specific HA, TMPRSS2 protease and a Firefly Luciferase encoding lentiviral vector are transfected into HEK293T/17 cells. 24 hr post-transfection, exogenous neuraminidase is added. 48hr post-transfection, influenza pseudotypes are harvested.
The ΔTMPRSS2 influenza pseudotypes were titrated in the absence or presence of TPCK-Trypsin to evaluate the effect of endogenous TMPRSS2 expression and to activate the haemagglutinin to obtain functional pseudotypes. TPCK-Trypsin (Sigma) was added to the pseudotypes to obtain the final concentration of 50 μg/ml and maintaining constant the TPCK-Trypsin concentration during the serial dilution. After 30 min at 37°C, 50 μl of trypsin neutralizing solution (Lonza) were added to each well. After 48 hrs, luminescence of cell cultures (in relative luminescence units or RLUs) was evaluated by luminometry using the Bright-Glo assay system (Promega, UK). Titres were expressed in RLU/ml.
Pseudotype particle neutralization assay with reference sera
Reference sera were tested against their respective pseudotypes by serially diluting 1:2 in culture media (from 1:80 to 1:5120) in white 96-well flat-bottomed tissue culture plates (Nunc) and 50 μl of pseudotype supernatant were added in each well, diluted to have a final concentration of 1 × 106 RLU/well. A ‘cell only’ control and a ‘pseudotype only’ (no sera) control were used in each assay. After 1 hr incubation of sera plus virus at 37°C, 1 × 104 HEK293T/17 cells were added to each well and the plates were incubated for a further 48 hrs at 37°C. Cell luminescence was measured as described above. The results were normalized and expressed as the percentage of inhibition of pseudotype virus entry (neutralization) using the cell only and pseudotype only control RLU values. The half maximal inhibitory concentration (IC50) and the 90% inhibitory concentration (IC90) were calculated with Prism version 6 (GraphPad Software).
RESULTS
The titres of Group-2 influenza pseudotype particles expressed in RLU/ml are shown in Figure 3. Through co-transfection with pCAGGS-TMPRSS2, we successfully obtained high-titre viral pseudotype particles harbouring the haemagglutinin of a human H3N2 virus (A/Udorn/307/1972), A/duck/Czechoslovakia/1956 (H4N6), A/chicken/Germany/N49 (H10N7), A/mallard/Astrakhan/263/1982 (H14N5), A/shearwater/West Australia/2576/1979 (H15N9) and H7 LPAI virus A/chicken/Italy/1082/1999 (H7N1). Notably, H3, H4 and H10 pseudotypes were produced with titres above 109 RLU/mL. The pseudotype particle titres obtained with TMPRSS2 transfection were compared to the controls: ΔTMPRSS2 influenza pseudotypes, ΔTMPRSS2 TPCK-Trypsin activated influenza pseudotypes and pseudotype particles produced without the HA envelope protein (Δenvelope). These data indicate that TMPRSS2 activates the haemagglutinin not only of human strains, such as A/Udorn/307/1972 (H3N2), but also the haemagglutinin of avian influenza strains (H4, H14, H15, H7 LPAI and H10 subtypes) in a similar manner to TPCK-Trypsin.
Figure 3.
Titres of Group-2 influenza pseudotype particles. Pseudotype transduction titres expressed in Relative Luminescence Units per ml (±SEM) are shown. The titres of influenza pseudotype particles produced after transfection of the pCAGGS-TMPRSS2 plasmid and the titre of ΔTMPRSS2 influenza pseudotype particles, before and after the TPCK-trypsin treatment, are reported. “∆envelope (pseudotype produced without the HA envelope protein) and cell only controls are also included.
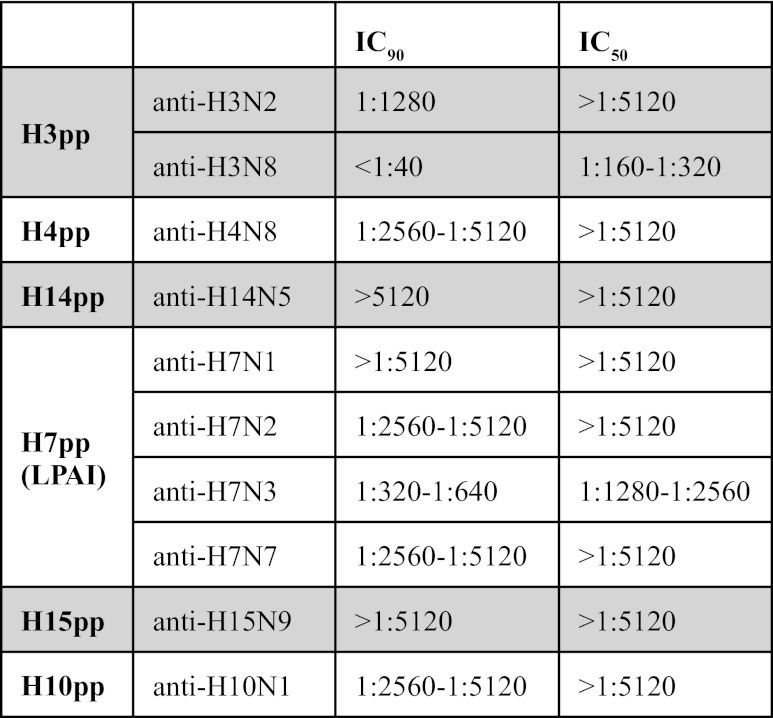
When tested in neutralization assays, the pseudotype particles were efficiently neutralized by their paired antisera (Table 1) using an IC50 cut-off dilution of 1:80. The only exception was for A/Udorn/307/1972 (H3N2) pseudotype that is efficiently neutralized (IC50 > 1:5120) by the anti-A/England/427/1988 (H3N2) sheep serum, but moderately neutralized by the anti-H3N8 sera of avian origin (IC50 = 1:160-1:320). Different neutralization profiles were also observed between the different H7 antisera, with the anti-A/chicken/England/4054/2006 (H7N3) exhibiting the least potent neutralization activity (IC50 = 1:1280-1:2560).
Table 1.
Half maximal inhibitory concentration (IC50) and the 90% inhibitory concentration (IC90) of reference antisera against Group-2 influenza pseudotype particles (pp). IC50 and IC90 were calculated with Graph Pad Prism version 6 and then were expressed as assay dilutions.
DISCUSSION
We have shown the essential role of TMPRSS2 in the production of high-titre Group-2 influenza pseudotype particles: the protease co-expression during virus production mediates the haemagglutinin activation of Group-2 human influenza and LPAI virus strains and enables functional pseudotype particles that have titres comparable to or higher than the ones that can be achieved with TPCK-Trypsin treatment. Since TMPRSS2 is a protease that is able to cleave human influenza haemagglutinins (Böttcher et al, 2006) and TPCK-Trypsin is able to activate haemagglutinin by proteolitic cleavage, we can assume that TMPRSS2 activates the HA on pseudotype particles by specific cleavage.
The fact that human TMPRSS2 is able to activate, most probably by cleavage, the HAs of different influenza A subtypes reinforces the concept that haemagglutinin cleavage is a conserved process between avian species and humans, which was highlighted by the observation that TMPRSS2 homologous proteins are able to cleave human influenza HA (Bertram et al, 2012). However further studies need to be performed to determine the function of TMPRSS2 and other proteases (e.g., HAT) in haemagglutinin activation and cleavage, to examine the cleavage kinetics and to understand the haemagglutinin amino acid residues involved in the haemagglutinin-protease interaction. Furthermore, it will be interesting to evaluate the ability of TMPRSS2 to activate LPAI Group-1 influenza haemagglutinin subtypes, since this protease is able to cleave the human H1 subtype (Böttcher et al, 2006) and similarly produced H1 pseudotypes have been reported in the literature (Wang et al, 2008; Corti et al, 2011). In the present study, we show that although human TMPRSS2 activates the haemagglutinin of different Group-2 subtypes, it is not clear if the difference in the titres observed between subtypes are dependent on differential HA expression and maturation (glycosylation, endoplasmic reticulum and Golgi apparatus trafficking) in the HEK293T/17 producer cell line (Ueda et al, 2008) or on differential TMPRSS2 recognition and cleavage of the different subtype haemagglutinins.
The Group-2 influenza haemagglutinins used in this study are characterized by the cleavage motif P[E,G][K,V,I]XX[K,R], with the numbers and physicochemical properties of the central aminoacidic residues between the proline and the cleavage arginine/lysine variable between subtypes (H3: PEKQTR; H4: PEKASR; H14: PGKQAK; H7: PEIPKGR; H15: PEKIRTR; H10: PEVVQGR). Recently the structure of an H16 subtype haemagglutinin was resolved and it was observed that some amino acid residues upstream of the cleavage site are important in determining the surface accessibility of the cleavage arginine (Lu et al, 2012). A similar process could explain the slightly lower titres observed in H14 and H15 pseudotypes: H14 haemagglutinin subtypes are characterized by a single lysine in their cleavage site (PGKQAK) (Kawaoka et al, 1990) and in H15 some amino acid residues upstream of the cleavage site (PEKIRTR) differ from the closely related H7 subtypes (PEIPKGR) (Röhm et al, 1996).
The resolving of the human TMPRSS2 protein structure and co-crystallization of TMPRSS2 with human and/or avian haemagglutinin could be valuable to delineate the amino acid residues involved in the cleavage process. This would not only enhance understanding of the haemagglutinin activation mechanism, but importantly may aid development of potential protease inhibitors (Zhirnov et al, 2011; Böttcher-Friebertshäuser et al, 2012), in a similar manner to neuraminidase inhibitor design, for treatment of severe influenza virus infections. The panel of Group-2 influenza pseudotypes described in this paper, in addition to those previously produced, could be utilized as tools to test the activity of these compounds in a pre-clinical screening phase.
The Group-2 influenza pseudotype particles could also be used to study the antibody response directed against haemagglutinin. Serological methods, such as haemagglutination inhibition and microneutralization, are cost-effective and widely-used methodologies to monitor the circulation and the prevalence of influenza viruses and are also employed in vaccine efficacy studies (Cattoli and Terregino, 2008). In this report, we have demonstrated that reference influenza antisera are able to efficiently neutralize their haemagglutinin-paired influenza pseudotype particles. It has been previously demonstrated that influenza pseudotype particle neutralization assays correlate with other classical serological assays (Temperton et al, 2007; Alberini et al, 2009; Garcia et al, 2010) and may become the technique of choice for HPAI H5 and H7 virus serology. Additionally, since the pseudotypes described are replication-defective, they offer a safe alternative to wild type virus methods that require biosafety level 3 containment, and the detection of antibody response is not influenced by the variability of blood-based reagents as observed in other assays (i.e. erythrocytes in haemagglutination inhibition) (Rowe et al, 1999). Furthermore, the pseudotype neutralization assay appears to be more effective than other functional assays to detect the antibody response directed against the HA2 haemagglutinin stalk (Corti et al, 2011). This is most likely due to the fact that, with the absence of neuraminidase on the pseudotype particle membrane surface, glycoprotein density is reduced and the HA stalk thus becomes more accessible to antibodies. Consequently, pseudotypes could be used to effectively study heterosubtypic antibody responses directed against the HA stalk region. In this study, with the production of Group-2 influenza pseudotypes we present a proof-of-principle for their use as surrogate antigens in antibody neutralization assays. We demonstrate that reference influenza antisera efficiently neutralize the matched pseudotypes. Interestingly, the human A/Udorn/307/1972 (H3N2) pseudotype is not efficiently neutralized by its paired (H3N8) avian antisera compared with the sheep H3N2 antisera. This is probably due to the fact that H3 avian viruses belong to a different lineage with respect to the human H3 (Zhang et al, 2007). Variation in the antisera neutralizing titres is also observed when the H7 antisera are tested. This is related to the origin of the antisera: they were generated against different H7 virus strains from the H7 pseudotype strain. This also may reflect intra-subtype antigenic differences among H7 strains. Furthermore the different antisera preparations probably have different neutralizing titres against their own viral strain.
Overall, the results presented here reinforce the greater sensitivity of the pseudotype particle neutralization assays described previously (Temperton et al, 2007; Garcia et al, 2010). These neutralization assays using Group-2 influenza pseudotype particles, provide additional impetus to optimise, standardise and validate this technology as a method to be used for the surveillance of influenza viruses in animals and humans.
CONCLUSIONS
In the present study we have shown that:
TMPRSS2 functions in effecting the activation, presumably by cleavage, of Group-2 influenza A virus haemagglutinins to produce high-titre influenza pseudotypes.
Influenza pseudotypes can be employed to determine which proteases are involved in haemagglutinin activation of individual subtypes.
Group-2 influenza pseudotype particles are neutralized by matched or related reference antisera.
The Group-2 influenza pseudotype particle neutralization assay could be used as an efficient serological surveillance assay, and for studying the antibody response against haemagglutinin elicited by vaccination or natural infection.
ACKNOWLEDGEMENTS
We thank the Animal Health and Veterinary Laboratories Agency for the reference antisera provided. This work was funded by the University of Kent.
LIST OF ABBREVIATIONS
- AHVLA
Animal Health and Veterinary Laboratories Agency
- HA
Haemagglutinin
- HAT
Human Airway-Trypsin-like protease
- HPAI
High pathogenicity avian influenza
- IC50
Half maximal inhibitory concentration
- IC90
90% inhibitory concentration
- LPAI
Low pathogenicity avian influenza
- NA
Neuraminidase
- NIBSC
National Institute for Biological Standards and Controls
- OIE
World Organisation for Animal Health
- Pp
Pseudotype particles
- RLU
Relative luminescence unit
- TMPRSS2
Transmembrane Protease Serine 2
COMPETING INTERESTS
None declared.
REFERENCES
- Alberini I, Del Tordello E, Fasolo A, et al. Pseudoparticle neutralization is a reliable assay to measure immunity and cross-reactivity to H5N1 influenza viruses. Vaccine. 2009;27:5998–6003. doi: 10.1016/j.vaccine.2009.07.079. [DOI] [PubMed] [Google Scholar]
- Bertram S, Glowacka I, Blazejewska P, et al. TMPRSS2 and TMPRSS4 facilitate trypsin-independent spread of influenza virus in Caco-2 cells. J Virol. 2010;84:10016–10025. doi: 10.1128/JVI.00239-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertram S, Heurich A, Lavender H, et al. Influenza and SARS-coronavirus activating proteases TMPRSS2 and HAT are expressed at multiple sites in human respiratory and gastrointestinal tracts. PLoS One. 2012;7:e35876. doi: 10.1371/journal.pone.0035876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böttcher E, Matrosovich T, Beyerle M, et al. Proteolytic activation of influenza viruses by serine proteases TMPRSS2 and HAT from human airway epithelium. J Virol. 2006;80:9896–9898. doi: 10.1128/JVI.01118-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böttcher-Friebertshäuser E, Lu Y, Meyer D, et al. Hemagglutinin activating host cell proteases provide promising drug targets for the treatment of influenza A and B virus infections. Vaccine. 2012;30:7374–7380. doi: 10.1016/j.vaccine.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Cattoli G, Milani A, Temperton N, et al. Antigenic drift in H5N1 avian influenza virus in poultry is driven by mutations in major antigenic sites of the hemagglutinin molecule analogous to those for human influenza virus. J Virol. 2011;85:8718–8724. doi: 10.1128/JVI.02403-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattoli G, Terregino C. New perspectives in avian influenza diagnosis. Zoonoses Public Health. 2008;55:24–28. doi: 10.1111/j.1863-2378.2007.01085.x. [DOI] [PubMed] [Google Scholar]
- Corti D, Voss J, Gamblin SJ, et al. A neutralizing antibody selected from plasma cells that binds to group 1 and group 2 influenza A hemagglutinins. Science. 2011;333:850–856. doi: 10.1126/science.1205669. [DOI] [PubMed] [Google Scholar]
- Fouchier RA, Munster V, Wallensten A, et al. Characterization of a novel influenza A virus hemagglutinin subtype (H16) obtained from black-headed gulls. J Virol. 2005;79:2814–2822. doi: 10.1128/JVI.79.5.2814-2822.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia JM, Lagarde N, Ma ES, et al. Optimization and evaluation of an influenza A (H5) pseudotyped lentiviral particle-based serological assay. J Clin Virol. 2010;47:29–33. doi: 10.1016/j.jcv.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Garcia JM, Lai JC. Production of influenza pseudotyped lentiviral particles and their use in influenza research and diagnosis: an update. Expert Rev Anti Infect Ther. 2011;9:443–455. doi: 10.1586/eri.11.25. [DOI] [PubMed] [Google Scholar]
- Garten W, Klenk H. Cleavage Activation of the Influenza Virus Hemagglutinin and Its Role in Pathogenesis. In: Klenk H, Garten W, Matrosovich M, editors. Avian Influenza; Karger, Basel, Switzerland: 2008. pp. 156–167. [Google Scholar]
- Kawaoka Y, Yamnikova S, Chambers TM, et al. Molecular characterization of a new hemagglutinin, subtype H14, of influenza A virus. Virology. 1990;179:759–767. doi: 10.1016/0042-6822(90)90143-f. [DOI] [PubMed] [Google Scholar]
- Lu X, Shi Y, Gao F, et al. Insights into avian influenza virus pathogenicity: the hemagglutinin precursor HA0 of H16 subtype has an α-helix structure in its cleavage site with an inefficient HA1/HA2 cleavage. J Virol. 2012;86:12861–12870. doi: 10.1128/JVI.01606-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen B, Munster VJ, Wallensten A, et al. Global patterns of influenza a virus in wild birds. Science. 2006;312:384–388. doi: 10.1126/science.1122438. [DOI] [PubMed] [Google Scholar]
- Peiris JSM. Avian influenza viruses in humans. Rev Sci Tech. 2009;28:161–173. doi: 10.20506/rst.28.1.1871. [DOI] [PubMed] [Google Scholar]
- Röhm C, Zhou N, Süss J, et al. Characterization of a novel influenza hemagglutinin, H15: criteria for determination of influenza A subtypes. Virology. 1996;217:508–516. doi: 10.1006/viro.1996.0145. [DOI] [PubMed] [Google Scholar]
- Rowe T, Abernathy RA, Hu-Primmer J, et al. Detection of antibody to avian influenza A (H5N1) virus in human serum by using a combination of serologic assays. J Clin Microbiol. 1999;37:937–943. doi: 10.1128/jcm.37.4.937-943.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamura K, Peterson D, Peterson N, et al. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011;28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temperton NJ, Hoschler K, Major D et al. A sensitive retroviral pseudotype assay for influenza H5N1-neutralizing antibodies. Influenza Other Respi Viruses. 2007;1:105–112. doi: 10.1111/j.1750-2659.2007.00016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S, Li Y, Rivailler P, et al. A distinct lineage of influenza A virus from bats. Proc Natl Acad Sci USA. 2012;109:4269–4274. doi: 10.1073/pnas.1116200109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda M, Yamate M, Du A, et al. Maturation efficiency of viral glycoproteins in the ER impacts the production of influenza A virus. Virus Res. 2008;136:91–97. doi: 10.1016/j.virusres.2008.04.028. [DOI] [PubMed] [Google Scholar]
- Wang W, Butler EN, Veguilla V, et al. Establishment of retroviral pseudotypes with influenza hemagglutinins from H1, H3, and H5 subtypes for sensitive and specific detection of neutralizing antibodies. J Virol Methods. 2008;153:111–119. doi: 10.1016/j.jviromet.2008.07.015. [DOI] [PubMed] [Google Scholar]
- Zhang W, Jiang Q and Chen Y. Evolution and variation of the H3 gene of influenza A virus and interaction among hosts. Intervirology. 2007;50:287–295. doi: 10.1159/000104788. [DOI] [PubMed] [Google Scholar]
- Zhirnov OP, Klenk HD and Wright PF. Aprotinin and similar protease inhibitors as drugs against influenza. Antiviral Res. 2011;92:27–36. doi: 10.1016/j.antiviral.2011.07.014. [DOI] [PubMed] [Google Scholar]