Summary
Background:
Multiloculated pleural effusion is a life-threatening condition that needs early recognition. Drainage by chest tube might be difficult which necessitates a surgical intervention. While x-ray typically does not show loculations, CT scan might not also identify the loculations. Ultrasound has a high sensitivity in detecting pleural diseases including multiloculated pleural effusion.
Case Report:
A 55-year-old female presented with dyspnea, cough and yellowish sputum for 3 days. Her heart rate was 136 bpm ,O2 saturation 88%, and WBC 21,000/mcL. Chest x-ray showed complete opacification of right lung. A chest tube insertion was unsuccessful. CT scan of the chest showed large pleural effusion occupying the right hemithorax with collapse of the right lung. Bedside ultra-sound showed a multiloculated pleural effusion with septations of different thickness. The patient subsequently underwent thoracotomy which showed multiple, fluid-filled loculations with significant adhesions. The loculations were dissected along with decortications of thick a pleural rind. Blood and pleural fluid cultures grew Streptococcus pneumoniae and the patient was treated successfully with Penicillin G.
Conclusions:
We advocate bedside ultrasound in patients with complete or near complete opacification of a hemithorax on chest x-ray. CT scan is less likely to show septations within pleural effusions compared to ultrasounnd. Therefore, CT scan and ultrasound are complementary for the diagnosis of empyema and multiloculated pleural effusion.
Keywords: empyema, ultrasonography, pleural effusion, chest tubes, thoracotomy
Background
Unilateral hemithorax opacification is a condition that is not uncommonly encountered in patients with respiratory distress. These patients can be critically-ill and early diagnosis is crucial for management. It can be caused by a paranchymal lung disease, pleural disease or chest wall disease.
Multiloculated pleural effusion is one of the causes of unilateral hemithorax opacification. It is usually due to an infectious process, but occasionally due to chylothorax or hemothorax. It is considered a complicated parapneumonic effusion by definition. Treatment with antibiotics and drainage is generally favored over antibiotics alone [1]. Initial attempts for drainage are usually by a chest tube. The importance of early recognition of the presence of multiloculations in patients with unilateral hemithorax opacification lies in the fact that drainage by chest tube alone might not be successful. Therefore, a more invasive method of drainage should be used. These include video-assisted thoracoscopic surgery (VATS), open decortication, and open thoracostomy.
The presence of pus in the pleural space or organisms seen on Gram stain defines the multiloculated pleural effusion as empyema. Empyema invariably requires drainage in addition to antibiotic therapy. Many of these patients will require thoracoscopic or open debridement and drainage [2].
While x-ray typically does not show loculations, CT scan might not also identify the loculations. Ultrasound has a high sensitivity in detecting pleural diseases including multiloculated pleural effusion. We present, herein, a case of complicated pleural effusion in which the multiloculations were detected only by a bedside ultrasound and not plain chest radiography or CT scan.
Case Report
A 55-year-old female presented with dyspnea, cough and yellowish sputum for 3 days. She is known to have Crohn’s disease and was started on prednisone and azathioprine one month prior. Her heart rate was 136 bpm, blood pressure 150/103, respiratory rate 37 bpm, O2 saturation 88% and temperature 36.2°C. She had a markedly diminished air sounds over the right lung. Her white cell count was 21,000/mcL, hemoglobin 8.9 g/dL, pH 7.11, pCO2 81 mmHg and HCO3 25 mmol/L. Chest x-ray showed complete opacification of right hemithorax (Figure 1).
Figure 1.
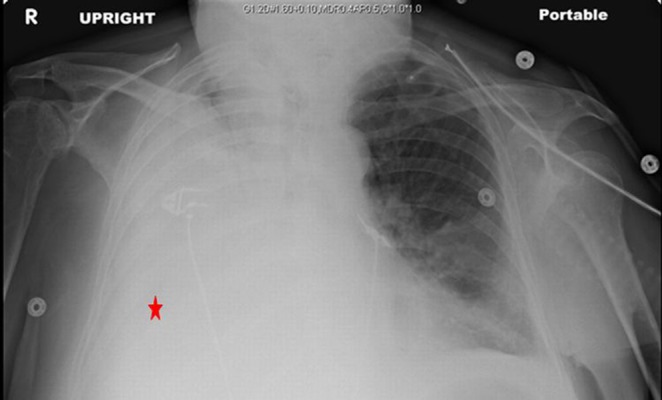
Plain chest x-ray showing a unilateral opacified right hemithorax.
She was put on BiPAP initially, but then required intubation. A bedside chest tube insertion was unsuccessful. CT scan of the chest (Figure 2) showed a large pleural effusion occupying the right hemithorax with collapse of the right lung in a bizarre fashion. Another attempt for drainage by chest tube yielded only 100 ml. Suspicion of loculations at this point was confirmed by a bedside ultrasound (Figure 3) which showed a multiloculated pleural effusion that was not clearly evident on CT scan.
Figure 2A.

Coronal chest CT showing an unusual appearance of collapsed right lung without evidence of loculations.
Figure 2B.

Axial chest CT showing lenticular collection.
Figure 3.
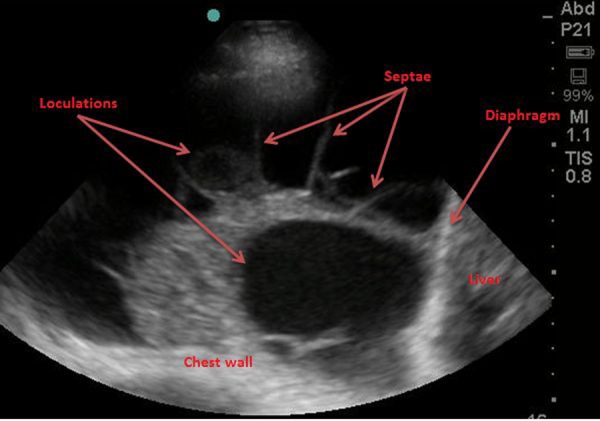
Bedside ultrasound of the right chest showing multiple collections with septations of different thickness.
She subsequently underwent thoracotomy which showed multiple, fluid-filled loculations mostly around the right lower lobe with significant adhesions to the diaphragm and along the major and minor fissures. The loculations were dissected along with decortications of thick a pleural rind. Two chest tubes were inserted. Blood and pleural fluid cultures grew Streptococcus pneumoniae and the patient was treated successfully with Penicillin G.
Discussion
Pleural fluid loculations develop secondary to the presence of visceral-to-paraietal adhesions that prevent fluid from falling to the dependent portion of the pleural cavity. Loculations can develop along any portion of the pleural cavity. The detection of loculations on plain chest radiography depends on the presence of surrounding aerated lung tissue that outlines the pleural opacity. A single loculated pocket of pleural effusion can be seen as an oval shape mass-like structure with a longitudinal orientation, a sharply demarcated convex margin at its interface with the lung and an indistinct margin where it contacts the chest wall [3]. However, in the setting of a massive pleural effusion and pneumonia with consolidation, multiloclations can not typically be seen on plain radiographs. Therefore, CT scan and/or ultrasound are required to visualize the multiloculations.
CT scan has many advantages over plain radiography for evaluation of patients with unilateral hemithorax opacification. It can potentially differentiate between pleural and paranchymal lung disease and provide visualization of underlying lung parenchymal processes that are obscured on the chest radiograph by a large pleural effusion. Loculated effusions have a lenticular configuration with smooth margins and relatively homogenous water attenuation. Loculations exert a mass effect, displace the lung and cause atelectasis of the adjacent lung tissue. These features can help differentiate empyema from lung abscess, which tend to be round rather than the lenticular shape of empyemas, and also have thick, irregular walls rarely displacing adjacent lung [4].
The attenuation of pleural fluid collections on CT scan does not allow definite distinction between infected and uninfected effusions, but can provide some diagnostic information. Infected pleural fluid collections have attenuation similar to water (i.e., 0 Hounsfield units), whereas collections with high protein content and bloody effusions may have attenuations of soft tissue (i.e., 30–50 Hounsfield units).
Pleural fluid on ultrasound can have one on the following patterns: echo free, complex septated, complex non-septated or hemogenously echogenic [5]. Although transudative pleural effusions are typically anechoic, 55% of proven transudative pleural effusions have a complex nonseptated appearance [6]. Conversely, although most complicated parapneumonic effusions and empyemas contain internal echoes or appear entirely echogenic, up to 27% of exudative effusions are anechoic [5]. Hemogenously echogenic collections typically contain blood or debris and almost invariably suggest the presence of empyema [7]. Large, discrete, primary loculations of pleural fluid indicate the presence of visceral to parietal pleural adhesions and suggest empyema [8].
Septae appear as thin, mobile, linear stuctures within a hypoechoic space [9]. Septae are essential fibrin strands that develop in protein-rich exudative effusions. Septations within an infected effusion are less readily imaged as compared with ultrasonography [10].
In a study by Himelman et al. radiographs demonstrated loculated fluid in 12 of the 17 (70%) loculated effusions. There were four cases in which ultrasound demonstrated loculations not seen on chest radiographs. CT scans demonstrated loculations not observed on radiograph or ultra-sound in only one case [11].
A study by Kearney et al. showed that there is no relationship between the presence of septated pleural fluid or pleural thickening on imaging, and the failure of aggressive management by chest tube drainage and intrapleural fibrinolytics. Therefore, it may be necessary to treat all patients with empyema by tube drainage in the first instance. The presence of apparent adverse CT and US features should not prevent a trial of drainage by tube as many of these patients will respond to tube drainage [10].
Our patient had a complex septated pleural effusion. This was not evident on CT scan. Bedside ultrasound was crucial in making the diagnosis and proceeding with surgical intervention following failure of drainage by a chest tube.
Conclusions
We advocate bedside ultrasound in patients with complete or near complete opacification of a hemithorax on chest x-ray. It helps identifying the nature of pleural disease, especially when CT does not show features of loculations or empyema. CT scan is less likely to show septations within pleural effusions compared to ultrasounnd. Therefore, CT scan and ultrasound are complementary for the diagnosis of empyema and multiloculated pleural effusion.
Refrences:
- 1.Colice GL, Curtis A, Deslauriers J, et al. Medical and surgical treatment of parapneumonic effusions: an evidence-based guideline. Chest. 2000;118:1158. doi: 10.1378/chest.118.4.1158. [DOI] [PubMed] [Google Scholar]
- 2.Wozniak CJ, Paull DE, Moezzi JE, et al. Choice of first intervention is related to outcomes in the management of empyema. AU Ann Thorac Surg. 2009;87:1525–30. 1530–31. doi: 10.1016/j.athoracsur.2009.01.028. discussion. [DOI] [PubMed] [Google Scholar]
- 3.Stark P. The pleura. In: Diagnosis Imaging, Intervention, Taveras, Ferrucci, editor. Radiology. Lippincott; Philadelphia: 2000. pp. 1–29. [Google Scholar]
- 4.Stark DD, Federle MP, Goodman PC. Differentiating lung abscess and empyema: Radiography and computed tomography. Am J Roentgenol. 1983;141(1):163–67. doi: 10.2214/ajr.141.1.163. [DOI] [PubMed] [Google Scholar]
- 5.Yang P-C, Luh K-T, Chang D-B, et al. Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. Am J Roentgenol. 1992;159(1):29–33. doi: 10.2214/ajr.159.1.1609716. [DOI] [PubMed] [Google Scholar]
- 6.Chen HJ, Tu CY, Ling SJ, et al. Sonographic appearances in transudative pleural effusions: not always an anechoic pattern. Ultrasound Med Biol. 2008;34(3):362–69. doi: 10.1016/j.ultrasmedbio.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Tu CY, Hsu WH, Hsia TC, et al. Pleural effusions in febrile medical ICU patients: chest ultrasound study. Chest. 2004;126(4):1274–80. doi: 10.1378/chest.126.4.1274. [DOI] [PubMed] [Google Scholar]
- 8.Lomas DJ, Padley SG, Flower CDR. The sonographic appearances of pleural fluid. Br J Radiol. 1993;66(787):619–24. doi: 10.1259/0007-1285-66-787-619. [DOI] [PubMed] [Google Scholar]
- 9.Marks WM, Filly RA, Callen PW. Real-time evaluation of pleural lesions: New observations regarding the probability of obtaining free fluid. Radiology. 1982;142(1):163–64. doi: 10.1148/radiology.142.1.7053526. [DOI] [PubMed] [Google Scholar]
- 10.Kearney SE, Davies CW, Davies RJ, Gleeson FV. Computed tomography and ultrasound in parapneumonic effusions and empyema. Clin Radiol. 2000;55(7):542–47. doi: 10.1053/crad.1999.0480. [DOI] [PubMed] [Google Scholar]
- 11.Himelman RB, Callen PW. The prognostic value of loculations in parapneumonic pleural effusions. Chest. 1986;90:852–56. doi: 10.1378/chest.90.6.852. [DOI] [PubMed] [Google Scholar]


