Abstract
Objective
Black and Latino children with asthma have worse morbidity and receive less controller medication than their white peers. Scant information exists on racial/ethnic differences in parent perceptions of asthma. To compare parent perceptions among black, Latino, and white children with asthma in 4 domains: (1) expectations for functioning with asthma; (2) concerns about medications; (3) interactions with providers; and (4) competing family priorities.
Methods
In this cross-sectional study, we conducted telephone interviews with parents of children with persistent asthma in a Medicaid health plan and a multispecialty provider group in Massachusetts. To measure expectations for functioning and other domains, we adapted multi-item scales from past studies. Associations between race/ethnicity and these domains were evaluated in multivariate analyses that controlled for age, gender, household income, parental education, insurance, and language. The response rate was 72%.
Results
Of the 739 study children, 24% were black, 21% Latino, and 43% white. Parents of black and Latino children had lower expectations for their children’s functioning with asthma (P < .001), higher levels of worry about their children’s asthma (P < .001), and more competing family priorities (P = 004) compared with parents of white children. Parents of Latino children had higher levels of concern about medications for asthma than parents of black or white children (P = 002). There were no differences among racial/ethnic groups in reports of interactions with the provider of their children’s asthma care.
Conclusions
Efforts to eliminate disparities in childhood asthma may need to address variation in expectations and competing priorities between minority and white families.
Keywords: asthma, health care disparities, racial/ethnic variation
Minority children experience higher morbidity and mortality due to asthma than white children.1 Asthma, the most prevalent chronic illness in the United States, leads to 4 times as many hospitalizations and 5 times as many deaths in blacks than whites, and this gap has been increasing since 1980.1–4 Despite knowledge that inhaled corticosteroids prevent morbidity from asthma,5,6 well-defined national guidelines for asthma treatment,7 and numerous interventions designed to improve outcomes from asthma in the inner city,8 these disparities in outcomes continue to increase.1
Black and Latino children are less likely to use preventive medications for asthma compared with white children, even among populations with financial coverage through Medicaid.9,10 The reasons for this disparity are not well understood. A recent Institute of Medicine report identified both patient-level and system-level factors as potential causes of racial/ethnic variation in clinical decisions.11 Among the possible patient-level factors are social, economic, and cultural influences, as well as patient preferences and subjectivity in the perception of symptoms.12–15 For example, children with asthma may be under treated if their parents and/or providers underestimate the severity of their symptoms or are reluctant to have their children use daily controller medications for any of a number of reasons.
To reduce disparities in childhood asthma, clinicians and policy makers need to better understand how parental expectations and concerns may vary between minority and white families. Previous research suggests that 4 domains deserve special evaluation as potential drivers of racial/ ethnic disparities in asthma. The first 2 domains are lower expectations about treatment and control13 and parental concern about adverse effects from anti-inflammatory medications,16 which have been associated with lapses in appropriate use of asthma controller medications. The third domain is positive interactions with providers, which are important in self-management of chronic illness,17 and the fourth is competing family priorities that are common barriers to the use of preventive health care services for children.18 Although past studies suggest that these domains may play an important role in treatment decisions, they have not evaluated racial/ethnic variations in these domains. Past studies have described knowledge and attitudes about asthma in groups of black or Latino parents of children with asthma,12,19 but little is known about differences between minority and white parents.
This study’s goal was to compare parents of black, Latino, and white children with asthma in their perceptions in these 4 important domains. Specifically, we tested the hypotheses that parents of minority children would have (1) lower expectations for functioning with asthma; (2) more concerns about medications; (3) worse reports of interactions with providers; and (4) more competing family priorities.
METHODS
Design and Study Settings
This was a cross-sectional study based on telephone interviews in English or Spanish with parents of children with asthma in 2 health care systems: Neighborhood Health Plan (NHP), the largest Medicaid managed care plan in Massachusetts; and Harvard Vanguard Medical Associates (HVMA), a multispecialty provider group in the greater Boston area that serves privately insured patients as well as Medicaid patients. The study was approved by the institutional review board of Harvard Pilgrim Health Care.
Data Collection
We identified children likely to have persistent asthma by using computerized utilization data and criteria defined in the Health Employer Data Information Set (HEDIS)20 measure of the National Committee on Quality Assurance. We used claims records at NHP and electronic medical records at HVMA to identify children with diagnoses of asthma based on International Classification of Diseases, 9th edition, codes from any clinical encounter (hospitalization, emergency department visit, or outpatient visit) plus any of the following events during the year before baseline: 4 or more prescriptions for β2-agonists, 2 or more prescriptions for inhaled anti-inflammatory medications, 2 or more prescriptions for oral corticosteroids, or 2 or more hospital-based episodes (hospitalizations or emergency department visits). Patients could be eligible for the study by being insured by NHP and seen at HVMA; these patients were counted only once, in the NHP group. After obtaining verbal consent over the telephone, we conducted a second-stage screening at the beginning of each parent telephone interview to confirm that the child had been diagnosed with asthma.
The structured telephone interview consisted of closed-ended questions and took approximately 30 minutes. Interviews were conducted in English or Spanish, and parents who participated received a $20 gift card. Surveys with identical content in English and Spanish were mailed to families after 12 failed telephone interview attempts over 2 weeks.
Of 1594 parents we attempted to contact on the basis of computerized data, 449 (24%) were unreachable as a result of telephone numbers that were wrong, disconnected, or not in service. Thirty-six (2%) were ineligible because they did not speak English or Spanish or had moved out of state, and 62 (4%) did not have a child with asthma. Of the 1047 parents who were eligible for the study, 754 completed the survey. Children whose parents completed the interview did not differ from those whose parents did not, based on the number of hospitalizations, emergency department visits, and asthma medications they used in the preceding year (P = 13). The completion rate, figured on the basis of the standard formula from the American Association of Public Opinion Research, was 72%.21 Of the completed surveys, 668 (89%) were completed over the telephone in English, 22 (3%) over the phone in Spanish, and 64 (8%) via mailed survey.
Measures
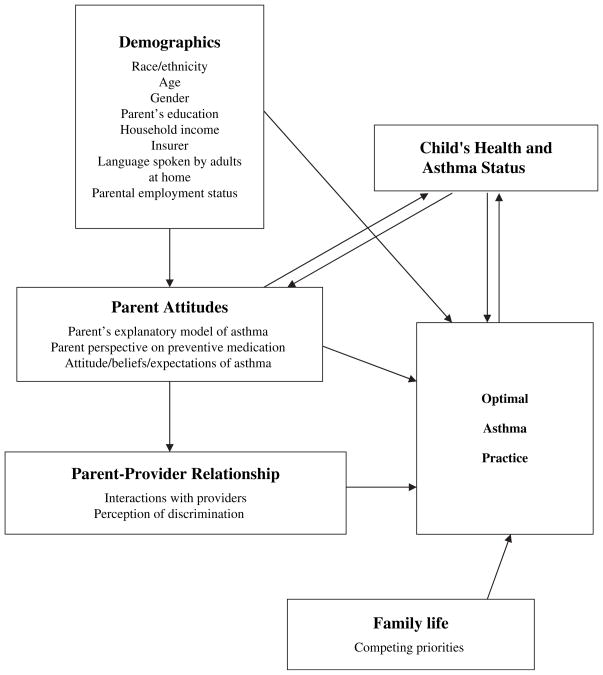
Our main outcome measures were parent expectations for asthma, parent concerns about medications, competing family priorities, and interactions with providers. These domains were chosen on the basis of our conceptual model (Figure), which we based on van Ryn’s model on race/ethnicity disparities in medical care.22 Factors that influence optimal asthma practice include family demographics, parental attitudes, the relationship between parent and provider, and family life.
Figure.
Conceptual model for factors involved in asthma practice. Main outcome measures—parent expectations for asthma, parent concerns about medications, competing family priorities, and interactions with providers—were based on these factors, which influence asthma practice.
If parents reported that their children were Spanish/ Hispanic/Latino, the children were included in the Latino subgroup for our analyses, regardless of description of race. Parents were also read a list of racial groups and asked which best described their children. Choices included black/African American, white/Caucasian, American Indian, Asian Indian, Chinese, Filipino, Japanese, and other race/ethnicities. Children with other race/ethnicities and mixed race/ethnicity were included in the “other” group. Statistical analyses compared the black, Latino, and white subgroups and did not include the “other” group. Children whose parents reported multiple races were also included in the “other” group.
The survey included questions that were based on published instruments as well as questions derived from qualitative analysis of interviews of parents of children with asthma. We used the Children’s Health Survey for Asthma (CHSA), which has high reliability and validity, to evaluate asthma physical status.23 Children with lower disease severity, measured by symptom activity, have higher CHSA scores than children with moderate to high disease severity.23 We chose 4 questions about parental expectations for symptoms from a reliable and valid 8-item measure developed by Yoos and colleagues.13 Each question posed a statement on expectations for asthma, eg, “I believe that my child can be symptom free most of the time.” Each question asked the parent to report on a 4-point Likert scale whether they agreed or disagreed with the statement (1 = strongly agree, 2 = agree, 3 = disagree, 4 = strongly disagree). The 4 questions on expectations for functioning with asthma had high interitem correlation (Cronbach’s alpha = 0.76) and were combined to form a summary measure with the possible scores ranging from 4 (lowest expectations) to 16 (highest expectations).
Questions on concerns about controller medications were created on the basis of a previous study of predictors of medication adherence.24 Each question posed a statement on concerns about controller medications, eg, “My child will become dependent on asthma medications if he/she takes them every day,” and parents were asked to agree or disagree (1 = strongly agree, 2 = agree, 3 = disagree, 4 = strongly disagree). We summed these 4 previously validated questions on concerns about medications24 to create a composite score that ranged from 4 (high concerns) to 16 (low concerns). This score had high reliability as measured by interitem correlation (Cronbach’s alpha = 0.72). The current research project included an earlier qualitative study of semistructured interviews with 37 parents of children with persistent asthma. The study explored the relationship between parents’ explanatory models of asthma and controller medication use. On the basis of the results of the qualitative analyses,25 we also asked whether parents worried about the long-term effects of corticosteroid use.
Interactions with the primary provider of asthma care were evaluated for the previous year by using subscales from instruments developed and validated by Safran and colleagues.26,27 Three questions assessed aspects of com- munication, and 2 questions assessed how well the provider knew the child and his or her medication history. This previously validated scale assessed how well providers listened carefully, how clear their instructions were, and how much time was spent in the clinical encounter.26,27
To assess whether parents experienced discrimination on the basis of their race/ethnicity, we asked 2 questions previously used in a survey by the Commonwealth Fund.28 These were, “Was there ever a time when doctors paid less attention to you or your child because of your race or ethnicity?” and “Was there ever a time when your child would have gotten better medical care if she or he had belonged to a different race/ethnic group?” We defined experiencing discrimination as answering “yes” to either of these 2 questions.
Questions that assessed competing family priorities were derived from unpublished work by A. Gurmankin and J. Baron that suggests that families have a finite “worry budget” to allocate to various domains of day-to-day living (e-mail communication, July 2004). We asked parents to rate their frequency of worry during the past 2 months for these domains: housing, home or neighborhood safety, job, personal/family relationships, income/making ends meet/keeping up with bills, parents’ own health/or other family member’s health. Parents were asked to answer on a 5-point Likert scale with responses 1 = “all the time” to 5 = “none of the time.” The individual questions on competing family priorities were summed to create the score for competing family priorities, with a range of 5 to 30.
Statistical Methods
Analyses were conducted in SAS version 9.1 (SAS Institute, Cary, NC). We evaluated demographic factors and measures of expectations and perceptions with univariate statistics. In bivariate analyses, we evaluated the association of each outcome with race/ethnicity and with other independent variables which included age, sex, respondent’s highest education attained, household income, insurer, language spoken by adults at home, parental employment status, and CHSA score. We estimated the unadjusted relative risk of each outcome, comparing the responses of black and Latino children’s parents to those of white children’s parents by using log-binomial regression. In multivariate analyses, we built iterative, forced-entry models based on our conceptual model in the Figure. The variables age, sex, and candidate variables significant at P ≤ .20 in the bivariate analyses were entered in the multivariate linear regression. Variables significant at P ≤ .10 were retained in the final multivariate models.
RESULTS
Population Characteristics
The study population included 739 children, of whom 24% were black, 21% Latino, 43% white, and 12% other (Table 1). The “other” category consisted of children who were Asian (n = 51), American Indian (n = 2), and multiracial/ethnic (n = 33).
Table 1.
Characteristics of Children by Race/Ethnicity*
| Characteristic | All† | Black | Latino | White | P |
|---|---|---|---|---|---|
| N | 739 | 177 | 156 | 320 | |
| Age, y, [SD] | 7.1 [3.1] | 7.0 [3.2] | 6.8 [3.2] | 7.5 [3.0] | .03 |
| Male sex, n (%) | 447 (60) | 115 (65) | 91 (58) | 193 (60) | (.54) |
| Respondent’s education, n (%) | <.0001 | ||||
| Less than high school | 189 (26) | 42 (24) | 67 (44) | 61 (19) | |
| High school graduate | 203 (28) | 64 (36) | 47 (31) | 72 (23) | |
| Some college | 197 (27) | 52 (29) | 26 (17) | 100 (31) | |
| College graduate or more | 146 (20) | 19 (11) | 14 (9) | 85 (27) | |
| Household income, n (%) | <.0001 | ||||
| <$15 000 | 82 (11) | 19 (11) | 31 (20) | 17 (5) | |
| $15 000–$30 000 | 127 (17) | 37 (21) | 50 (32) | 33 (10) | |
| $30 001–$50 000 | 38 (5) | 13 (7) | 14 (9) | 10 (3) | |
| >$50 000 | 443 (60) | 99 (56) | 52 (33) | 236 (74) | |
| Don’t know/refused | 49 (7) | 9 (5) | 9 (6) | 24 (8) | |
| Insurer, n (%) | <.0001 | ||||
| HPHC | 218 (30) | 48 (27) | 21 (13) | 131 (41) | |
| NHP | 249 (34) | 61 (34) | 87 (56) | 75 (23) | |
| Other | 272 (36) | 68 (38) | 48 (31) | 114 (36) | |
| Language spoken by adults at home, n (%) | <.0001 | ||||
| English | 654 (89) | 168 (96) | 111 (71) | 305 (97) | |
| Spanish | 46 (6) | 0 (0) | 45 (29) | 0 (0) | |
| Other | 31 (4) | 7 (4) | 0 (0) | 8 (3) | |
| Parental employment status, n (%) | <.0001 | ||||
| Unemployed | 254 (35) | 53 (30) | 46 (30) | 121 (38) | |
| Part time | 250 (34) | 42 (24) | 59 (39) | 122 (38) | |
| Full time | 227 (31) | 79 (45) | 48 (31) | 75 (24) | |
| CHSA score, mean [SD] | 84 [17] | 82 [18] | 78 [19] | 88 [14] | <.0001‡ |
HPHC indicates Harvard Pilgrim Health Care; NHP, Neighborhood Health Plan; and CHSA, Children’s Health Survey for Asthma.
All includes children of black (n = 177), Latino (n = 156), white (n = 320), and other (n = 86) race/ethnicity.
P value calculated with variable as a continuous variable.
Parents of black (11%) and Latino (9%) children were less likely to be college graduates compared with white (27%) parents (P < .0001). Black (56%) and Latino (33%) children were also less likely to have household incomes of greater than $50 000 compared with white (74%) children (P < .0001). Black (34%) and Latino (56%) children were more likely to be insured by NHP, whose patients are predominantly insured by Medicaid, than white (23%) children (P <.0001).
Expectations for Functioning With Asthma
Parents of black and Latino children had lower expectations for their children’s asthma than parents of white children (Table 2). For example, 84% of parents of black children, 75% of parents of Latino children, and 89% of parents of white children believed their children could be symptom-free most of the time (P = .0003). In addition, 44% of parents of black children, 43% of parents of Latino children, and 55% of parents of white children expected their children should have no emergency department visits or hospitalizations for asthma (P =.01). On the basis of our summary score for expectations, parents of black and Latino children had lower expectations than parents of white children even after controlling for age, gender, and household income (P =.01). Parents of Latino children were also more likely than other parents to say that they considered their children in good control if they had more than 2 days of symptoms per week (relative risk, 1.13; 95% confidence interval [95% CI], 1.05, 1.23]).
Table 2.
Expectations of Child’s Asthma Function by Race/Ethnicity
| Characteristic | All, n (%) | Black, n (%) | Latino, n (%) | White, n (%) | P | Relative Risk (95% Confidence Interval) Compared With White
|
|
|---|---|---|---|---|---|---|---|
| Black | Latino | ||||||
| N | 739 | 177 | 156 | 320 | – | – | – |
| Agreed to the following statements: | |||||||
| “I believe my child can be symptom free most of the time”* | 623 (87) | 149 (87) | 117 (79) | 284 (91) | .0003† | 0.69 (0.41, 1.16) | 0.43 (0.27, 0.69) |
| “I expect asthma will not affect school/daycare attendance”* | 443 (63) | 104 (62) | 74 (51) | 214 (69) | .0007† | 0.80 (0.62, 1.03) | 0.63 (0.50, 0.79) |
| “I expect child can fully participate in gym”* | 621 (86) | 154 (89) | 122 (81) | 271 (87) | .01† | 1.12 (0.68, 1.85) | 0.67 (0.43, 1.04) |
| “I expect child will have no ER visits or hospitalizations from asthma”* | 371 (55) | 78 (48) | 67 (47) | 177 (61) | .01† | 0.75 (0.61, 0.92) | 0.74 (0.59, 0.91) |
| Overall expectation score | <.01†‡ | 0.97 (0.87, 1.09) | 0.76 (0.59, 0.99) | ||||
| Low expectations (4–7) | 465 (67) | 109 (66) | 114 (80) | 191 (63) | – | – | |
| High expectations (8–16) | 227 (33) | 57 (34) | 29 (20) | 112 (37) | – | – | |
| Good control is __ days/week of symptoms§ | .0004† | 0.70 (0.37, 1.31) | 0.38 (0.22, 0.65) | ||||
| 0–2 days | 621 (90) | 148 (90) | 122 (82) | 273 (93) | – | – | |
| >2 days | 66 (10) | 16 (10) | 27 (18) | 20 (7) | – | – | |
| Rating of child’s asthma control in the last 14 days§ | <.0001† | 0.42 (0.26, 0.69) | 0.35 (0.21, 0.57) | ||||
| Excellent/Very Good/Good | 625 (86) | 144 (82) | 120 (78) | 288 (92) | – | – | |
| Fair/Poor/Very Poor | 102 (14) | 32 (18) | 34 (22) | 24 (8) | – | – | |
These 4 questions were summed to form the overall expectation score.
P values calculated with variables as continuous variables.
Controlled for age, gender, household income, parental education, health insurance, English fluency, and Children’s Health Survey for Asthma score.
Questions created as part of our study.
Concerns About Medications
Parents of black and Latino children had more medication concerns compared with parents of white children (Table 3). Parents of minority children were more likely to believe that their children would become dependent on medications if given every day, compared with parents of white children with a relative risk for parents of black children of 1.40 (95% CI, 1.18, 1.67) and 1.28 (95% CI, 1.08, 1.52) for Latino children. When asked whether their children did not need as much medicine as the doctor prescribed, 32% of parents of black children and 38% of parents of Latino children agreed, compared with 23% of parents of white children (P =.001). However, there were no differences in perception that their children’s asthma does not need medicine every day, in stopping the children’s medicines to give their bodies rests, or in concern about the long-term effects of corticosteroids in any of the groups. Parents of Latino children were more likely to have scores that indicated high concerns about asthma medications compared with parents of black or white children, even after controlling for other variables (Table 3, P =.002).
Table 3.
Concerns About Medications for Asthma Stratified by Race/Ethnicity
| Characteristic | All, n (%) | Black, n (%) | Latino, n (%) | White, n (%) | P | Relative Risk (95% Confidence Interval) Compared With White
|
|
|---|---|---|---|---|---|---|---|
| Black | Latino | ||||||
| N | 739 | 177 | 156 | 320 | |||
| Agreed to the following statements: | |||||||
| “Child’s asthma does not need medicine every day”* | 227 (45) | 62 (47) | 43 (45) | 96 (42) | (.26)† | 1.07 (0.88, 1.30) | 1.05 (0.85, 1.30) |
| “Child will become dependent on medicines if given every day”* | 177 (34) | 60 (45) | 43 (40) | 54 (24) | .0002† | 1.40 (1.18, 1.67) | 1.28 (1.08, 1.52) |
| “Child doesn’t need as much medicine as doctor prescribed”* | 159 (30) | 44 (32) | 39 (38) | 53 (23) | .001† | 1.14 (0.99, 1.30) | 1.24 (1.05, 1.46) |
| “Sometimes stop giving child medicine to give body rest”* | 170 (34) | 49 (37) | 34 (37) | 65 (29) | (.17)† | 1.13 (0.97, 1.32) | 1.12 (0.94, 1.34) |
| Worry about long-term effects of corticosteroids§ | 536 (76) | 127 (74) | 111 (76) | 235 (78) | (.71)† | 0.87 (0.63, 1.21) | 0.92 (0.64, 1.30) |
| Overall medication concern score | .002†‡ | 0.99 (0.89, 1.11) | 1.16 (1.01, 1.33) | ||||
| High concern (4–7) | 223 (30) | 47 (27) | 58 (37) | 87 (27) | – | – | |
| Low concern (8–16) | 516 (70) | 130 (73) | 98 (63) | 233 (73) | – | – | |
These 4 questions were summed to form the medication concern score. Medicine refers to controller medication such as inhaled corticosteroid or leukotriene inhibitor.
P values calculated with variables as continuous variables.
Controlled for age, gender, household income, education, English fluency, and Children’s Health Survey for Asthma score.
Question created as part of our study.
Interactions With Providers
Ninety-one percent of parents were highly satisfied with communication with their children’s providers.26,27 In addition, 93% of parents were satisfied with providers’ knowledge of their children based on a second previously validated scale.26,27 More specifically, parents felt their providers were knowledgeable about their children’s history and about their children. There were no significant differences among parents of black, Latino, and white children in any measure of satisfaction.
Parents of minority children were more likely to report that they had been discriminated against on the basis of race/ethnicity in a health care setting at some time in the past; 6% of black, 4% of Latino, and 0.6% of white parents reported experiencing discrimination. This variation was significantly different even after controlling for age, gender, income, education, and English fluency (P = .001).
Worries About Asthma and Competing Family Priorities
Nineteen percent of parents of black children and 33% of parents of Latino children rated their children’s asthma as 8 or higher on a scale where 10 represented the highest level of worry, compared with 9% of parents of white children (P <.0001). This variation persisted even after controlling for severity of asthma, as measured by the CHSA score.
Parents responded on a 5-point scale their degree of worry about each competing priority in the previous 2 months. The individual competing family priorities questions were added to make a summary score with a range from 5 (worries “none of the time” about any of the domains) to 30 (worries “all of the time” about all of the domains). This score had high interitem correlation (Cronbach’s alpha = 0.77).
Parents of black children (18%) and parents of Latino children (23%) were more likely to have competing family priorities “all of the time” or “most of the time” in addition to their children’s asthma compared with white (8%) parents, as assessed by our composite score for competing priorities on multivariate analysis (P = .004, Table 4), even after adjusting for age, gender, household income, education, and health insurance. Parents of black and Latino children were more likely to report that they worried all or most of the time about the following compared with white parents: housing, home and neighborhood safety, job, personal and family relationship, income/making ends meet, and personal or family health. For example, on bivariate analyses, 18% of black, 20% of Latino, and 3% of white parents worried all or most of the time about home or neighborhood safety (P < .0001), and 15% of parents of black children, 17% of parents of Latino children, and 8% of parents with white children worried about their job all or most of the time (P = .01).
Table 4.
Asthma Worries and Competing Family Priorities, by Race/Ethnicity
| Characteristic | All, n (%) | Black, n (%) | Latino, n (%) | White, n (%) | P | Relative Risk (95% Confidence Interval) Compared With White
|
|
|---|---|---|---|---|---|---|---|
| Black | Latino | ||||||
| N | 739 | 177 | 156 | 320 | – | – | – |
| Rating of child’s asthma on rating scale (−0, 10 = highest level of worry):* | <.0001†‡ | ||||||
| 1–3 | 199 (28) | 39 (23) | 24 (16) | 106 (34) | 0.85 (0.76, 0.95) | 0.78 (0.71, 0.88) | |
| 4–5 | 182 (25) | 48 (28) | 32 (22) | 82 (26) | 1.02 (0.91, 1.14) | 0.94 (0.84, 1.05) | |
| 6–7 | 214 (30) | 53 (31) | 43 (29) | 96 (31) | 0.93 (0.85, 1.01) | 0.93 (0.85, 1.02) | |
| 8–10 | 121 (17) | 33 (19) | 48 (33) | 27 (9) | 1.24 (1.10, 1.40) | 1.53 (1.30, 1.79) | |
| Worried about the following “all” or “most” of the time in the previous 2 months:* | |||||||
| Housing§ | 96 (13) | 34 (20) | 29 (19) | 17 (5) | <.0001† | 1.18 (1.09, 1.27) | 1.17 (1.08, 1.27) |
| Home/neighborhood safety§ | 82 (11) | 31 (18) | 30 (20) | 10 (3) | <.0001† | 1.18 (1.10, 1.27) | 1.21 (1.11, 1.31) |
| Job§ | 89 (13) | 25 (15) | 26 (18) | 26 (9) | .01† | 1.07 (0.99, 1.15) | 1.11 (1.02, 1.21) |
| Personal/family relationships§ | 77 (11) | 19 (11) | 23 (15) | 22 (7) | (.05)† | 1.05 (0.98, 1.11) | 1.10 (1.02, 1.18) |
| Income/making ends meet§ | 206 (29) | 51 (30) | 62 (41) | 63 (20) | <.0001† | 1.14 (1.02, 1.27) | 1.36 (1.18, 1.57) |
| Your own health/or other family member’s health§ | 149 (21) | 38 (22) | 54 (36) | 40 (13) | <.0001† | 1.12 (1.02, 1.23) | 1.37 (1.20, 1.55) |
| Score for competing family priorities*|| | .004† | ||||||
| Worries “all” or “most” of time (20–30) | 114 (15) | 32 (18) | 36 (23) | 27 (8) | 1.12 (1.04, 1.21) | 1.19 (1.09, 1.31) | |
| Worries “some” of the time (15–19) | 36 (5) | 9 (5) | 9 (6) | 15 (5) | 1.00 (0.96, 1.05) | 1.01 (0.97, 1.06) | |
| Worries “little” or “none” of the time (5–14) | 589 (80) | 136 (77) | 111 (71) | 278 (87) | 0.57 (0.38, 0.84) | 0.46 (0.31, 0.66) | |
Questions created as part of our study.
P values calculated with variables as continuous variables.
Controlled for age, gender, household income, education, health insurance, English-speaking ability, and Children’s Health Survey for Asthma score.
These questions were summed to form the score for competing priorities.
Range of scores 5–0, with 30 = worried “all of the time” about all of the domains and 5 = worried “none of the time” about any of the domains. Controlled for age, gender, household income, education, and health insurance.
DISCUSSION
This study suggests that parents of black and Latino children with asthma tend to have lower expectations for their children’s functioning compared with white parents. In addition, parents of minority children in this study had more concerns about medications and higher levels of worry about competing life issues such as housing, income, safety, jobs, and family relationships; this was true even after controlling for income and education. These differences may influence differences in asthma management and levels of asthma status among minority children.
Our findings lend support to the hypothesis that parental health beliefs are factors in racial/ethnic variation in asthma care. Racial/ethnic differences in patient expectations and perceptions appear to play a role in variation in clinical care observed in other medical areas including arthritis, knee replacement, renal transplantation, and depression.29–33 In our study, parents of minority children had lower expectations for functioning, and a previous study found that lower expectations are associated with fewer prescriptions for preventive medications.13 Our finding that Latino parents expressed greater concerns about medications than other patients is consistent with a previous study of minority patients.12 Concerns about medications may limit adherence.24,34,35
Our study is unique in that we were able to compare black, Latino, and white parents in the same populations. Previous studies have examined the perspectives of either black or Latino parents of children with asthma,12,19 but few studies, if any, have compared these groups with each other or with white parents. In addition to having different expectations and concerns, minority parents in our study tended to have more competing family priorities than white families. These competing priorities might present barriers to optimal asthma management in both the home and clinical settings.
Racial/ethnic variation in diagnosis, treatment, and outcomes have been documented in many health fields.30,36,37 Potential reasons for these differences include minority patients having worse access to health care, having providers that are less likely to provide appropriate care, or having cultural or other beliefs that lead to less appropriate care.12–14 Our study did not attempt to measure provider-level or health care system–level factors that might vary among children of different racial/ethnic groups. We did find that most parents were satisfied with their interpersonal relationships with their children’s asthma providers, regardless of the children’s race/ethnicity, even though minority parents were more likely to report having experienced discrimination in the health care system at some time in the past. Future research that evaluates the influence of provider-level and system-level factors relative to parent expectations and beliefs is warranted.
This study has several limitations. In this study, we did not attempt to evaluate whether racial/ethnic variation in parental beliefs was associated with variation in asthma control or medication use. Our response rate, 72%, was reasonably high compared with other studies that include Medicaid populations, but many families had to be excluded because of nonworking telephones.38 Most of the survey questions in our study have been previously validated in other studies, but on the basis of our analyses of qualitative data in a preceding phase of this project, we created several questions whose properties have not been fully evaluated. All patients in our study population had either Medicaid or private insurance and were from a single geographic region, so the results may not be generalizable to uninsured children. In addition, the inclusion criteria were based on asthma health services use, ie, hospital-based services and/or medications. Thus, the children in our target population were selected to have more symptomatic asthma and may have higher utilization rates of medical services than a more general population of asthmatics.
In this study, we treated Latinos as a single group, but we recognize that individual Latino subgroups may have different experiences and outcomes,39,40 and Puerto Rican children may have higher morbidity rates from asthma.41 Furthermore, our study did not specifically address language barriers, which may be an important driver of communication gaps, although our multivariate models did adjust for fluency in English.42,43 We administered our survey in Spanish and English, but limited sample size precluded our analyzing the Spanish responses in detail. Because our Latino population was predominantly fluent in English, our study population of Latinos may be more acculturated than some inner-city populations.
CONCLUSION
Our study suggests that parents of black and Latino children with asthma have lower expectations for functioning, more concerns about medications, and more competing family priorities than parents of white children. Our data suggest that in clinical interactions, providers may wish to adjust their communication patterns to account for the fact that patients of different racial/ethnic backgrounds may have different expectations and concerns about asthma. Providers could consider how best to partner with minority parents to raise their expectations for functioning with asthma. Efforts to eliminate disparities in childhood asthma may need to address these variations in parent perceptions to eliminate them as barriers to preventive treatment.
Acknowledgments
This work was supported by a grant from the National Institute of Child Health and Human Development (NICHD) (R01 HD044070). Dr Wu’s effort was supported by the Agency for Healthcare Research and Quality, grant T32 HS000063 to the Harvard Pediatric Health Services Research Fellowship Program. Dr Bokhour’s effort was supported in part by the Department of Veterans’ Affairs, Health Services Research & Development service. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. Dr Lieu’s effort was supported in part by a Mid-Career Investigator Award in Patient-Oriented Research from NICHD (K24 HD047667).
We are grateful to Charlene Gay for her assistance in coordinating this project, our research assistants, including Heather Brymer, Stephanie Love, Amarylis Perez, Tamaris Salerna, Patti Steele, Susan Swords, Elizabeth Suda, and Marlene Taveras, and our program officer, Lynn Haverkos, MD.
References
- 1.Gupta RS, Carrion-Carire V, Weiss KB. The widening black/white gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117:351–358. doi: 10.1016/j.jaci.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 2.Weiss KB, Wagener DK. Changing patterns of asthma mortality. Identifying target populations at high risk. JAMA. 1990;264:1683–1687. [PubMed] [Google Scholar]
- 3.Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma—United States, 1980–1999. MMWR Surveill Summ. 2002;51:1–13. [PubMed] [Google Scholar]
- 4.Mannino DM, Homa DM, Pertowski CA, et al. Surveillance for asthma—United States, 1960–1995. MMWR CDC Surveill Summ. 1998;47:1–27. [PubMed] [Google Scholar]
- 5.Adams RJ, Fuhlbrigge A, Finkelstein JA, et al. Impact of inhaled anti-inflammatory therapy on hospitalization and emergency department visits for children with asthma. Pediatrics. 2001;107:706–711. doi: 10.1542/peds.107.4.706. [DOI] [PubMed] [Google Scholar]
- 6.Donahue JG, Weiss ST, Livingston JM, Goetsch MA, Greineder DK, Platt R. Inhaled steroids and the risk of hospitalization for asthma. JAMA. 1997;277:887–891. [PubMed] [Google Scholar]
- 7.NAEPP Program. Expert Panel Report II: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Institutes of Health; 1997. [Google Scholar]
- 8.Quinn K, Shalowitz MU, Berry CA, Mijanovich T, Wolf RL. Racial and ethnic disparities in diagnosed and possible undiagnosed asthma among public-school children in Chicago. Am J Public Health. 2006;92:1599–1603. doi: 10.2105/AJPH.2005.071514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lieu TA, Lozano P, Finkelstein JA, et al. Racial/ethnic variation in asthma status and management practices among children in managed medicaid. Pediatrics. 2002;109:857–865. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 10.Finkelstein JA, Lozano P, Farber HJ, Miroshnik I, Lieu TA. Underuse of controller medications among Medicaid-insured children with asthma. Arch Pediatr Adolesc Med. 2002;156:562–567. doi: 10.1001/archpedi.156.6.562. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine; 2003. [Google Scholar]
- 12.Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: parent perspectives. Pediatrics. 2000;106:512–519. doi: 10.1542/peds.106.3.512. [DOI] [PubMed] [Google Scholar]
- 13.Yoos HL, Kitzman H, McMullen A. Barriers to anti-inflammatory medication use in childhood asthma. Ambul Pediatr. 2003;3:181–190. doi: 10.1367/1539-4409(2003)003<0181:btamui>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 14.Katz JN. Patient preferences and health disparities. JAMA. 2001;286:1506–1509. doi: 10.1001/jama.286.12.1506. [DOI] [PubMed] [Google Scholar]
- 15.Balsa AI, McGuire TG, Meredith LS. Testing for statistical discrimination in health care. Health Serv Res. 2005;40:227–252. doi: 10.1111/j.1475-6773.2005.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peterson-Sweeney K, McMullen A, Yoos HL, Kitzman H. Parental perceptions of their child’s asthma: management and medication use. J Pediatr Health Care. 2003;17:118–125. doi: 10.1067/mph.2003.31. [DOI] [PubMed] [Google Scholar]
- 17.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riportella-Muller R, Selby-Harrington ML, Richardson LA, Donat PL, Luchok KJ, Quade D. Barriers to the use of preventive health care services for children. Public Health Rep. 1996;111:71–77. [PMC free article] [PubMed] [Google Scholar]
- 19.Lara M, Duan N, Sherbourne C, et al. Differences between child and parent reports of symptoms among Latino children with asthma. Pediatrics. 1998;102:E68. doi: 10.1542/peds.102.6.e68. [DOI] [PubMed] [Google Scholar]
- 20.National Committee for Quality Assurance. HEDIS 2003 Technical Specifications. Washington, DC: National Committee for Quality Assurance; 2002. Health Employer Data Information Set (HEDIS) [Google Scholar]
- 21.American Association for Public Opinion Research. [Accessed November 28, 2007];Response rate calculator. Available at: http://www.aapor.org/responseratesoverview.
- 22.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 suppl):I140–I151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 23.Asmussen L, Olson LM, Grant EN, Fagan J, Weiss KB. Reliability and validity of the Children’s Health Survey for Asthma. Pediatrics. 1999;104:e71. doi: 10.1542/peds.104.6.e71. [DOI] [PubMed] [Google Scholar]
- 24.Riekert KA, Butz AM, Eggleston PA, Huss K, Winkelstein M, Rand CS. Caregiver-physician medication concordance and under-treatment of asthma among inner-city children. Pediatrics. 2003;111:e214–e220. doi: 10.1542/peds.111.3.e214. [DOI] [PubMed] [Google Scholar]
- 25.Bokhour BGCE, Cortes D, Yinusa-Nyahkoon LS, Smith L, Lieu T. Parents’ explanatory models and approaches to medications for childhood asthma. Presented at: American Public Health Association 134th Annual Meeting and Exposition; Boston, Mass. November 7, 2006. [Google Scholar]
- 26.Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–739. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Taira DA, Safran DG, Seto TB, et al. Do patient assessments of primary care differ by patient ethnicity? Health Serv Res. 2001;36:1059–1071. [PMC free article] [PubMed] [Google Scholar]
- 28.SteelFisher GK. Addressing Unequal Treatment: Disparities in Health Care. New York, NY: Commonwealth Fund; 2004. [PubMed] [Google Scholar]
- 29.Figaro MK, Williams-Russo P, Allegrante JP. Expectation and outlook: the impact of patient preference on arthritis care among African Americans. J Ambul Care Manage. 2005;28:41–48. doi: 10.1097/00004479-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Hebert PL, Frick KD, Kane RL, McBean AM. The causes of racial and ethnic differences in influenza vaccination rates among elderly Medicare beneficiaries. Health Serv Res. 2005;40:517–537. doi: 10.1111/j.1475-6773.2005.00370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Suarez-Almazor ME, Souchek J, Kelly PA, et al. Ethnic variation in knee replacement: patient preferences or uninformed disparity? Arch Intern Med. 2005;165:1117–1124. doi: 10.1001/archinte.165.10.1117. [DOI] [PubMed] [Google Scholar]
- 32.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 33.Mangione-Smith R, Elliott MN, Stivers T, McDonald L, Heritage J, McGlynn EA. Racial/ethnic variation in parent expectations for antibiotics: implications for public health campaigns. Pediatrics. 2004;113:e385–e394. doi: 10.1542/peds.113.5.e385. [DOI] [PubMed] [Google Scholar]
- 34.Chan PW, DeBruyne JA. Parental concern towards the use of inhaled therapy in children with chronic asthma. Pediatr Int. 2000;42:547–551. doi: 10.1046/j.1442-200x.2000.01278.x. [DOI] [PubMed] [Google Scholar]
- 35.Conn KM, Halterman JS, Fisher SG, Yoos HL, Chin NP, Szilagyi PG. Parental beliefs about medications and medication adherence among urban children with asthma. Ambul Pediatr. 2005;5:306–310. doi: 10.1367/A05-004R1.1. [DOI] [PubMed] [Google Scholar]
- 36.Wagner J, Tsimikas J, Abbott G, de Groot M, Heapy A. Racial and ethnic differences in diabetic patient-reported depression symptoms, diagnosis, and treatment. Diabetes Res Clin Pract. 200;71:119–122. doi: 10.1016/j.diabres.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation—clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343:1537–1544. doi: 10.1056/NEJM200011233432106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fredrickson DD, Jones TL, Molgaard CA, et al. Optimal design features for surveying low-income populations. J Health Care Poor Underserved. 2005;16:677–690. doi: 10.1353/hpu.2005.0096. [DOI] [PubMed] [Google Scholar]
- 39.Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Soc Sci Med. 2005;61:53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 40.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA. 2002;288:82–90. doi: 10.1001/jama.288.1.82. [DOI] [PubMed] [Google Scholar]
- 41.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 42.Cohen AL, Christakis DA. Primary language of parent is associated with disparities in pediatric preventive care. J Pediatr. 2006;148:254–258. doi: 10.1016/j.jpeds.2005.10.046. [DOI] [PubMed] [Google Scholar]
- 43.David RA, Rhee M. The impact of language as a barrier to effective health care in an underserved urban Hispanic community. Mt Sinai J Med. 1998;65:393–397. [PubMed] [Google Scholar]