Abstract
Individuals with elevated anxiety sensitivity (AS; i.e., fear of somatic arousal) may binge eat to reduce emotional distress. Because physical activity reduces stress reactivity, we predicted that: (1) the relation between AS and binge eating would be moderated by physical activity and (2) coping motives for eating would mediate the association between AS and binge eating such that the relation would be stronger for those low in physical activity. Participants (N=167) completed online self-report measures. Regression analyses revealed that moderate-intensity physical activity (MPA) moderated the relation between AS and binge eating such that AS was not related to binge eating among those who frequently engaged in MPA but was related to binge eating among those who did not report engaging in MPA. Vigorous-intensity physical activity (VPA) moderated in the opposite direction such that the relation between AS and binge eating was significant among persons reporting high levels of VPA but less strong among persons reporting low levels of VPA. The mediation model was also significant, but was not moderated by MPA or VPA. Theoretical and clinical implications are discussed.
Keywords: Binge eating, Emotional eating, Anxiety sensitivity, Physical activity
1. Introduction
1.1. The problem of binge eating
Binge eating is defined by consuming an unusually large amount of food in a short period of time while experiencing a lack of control over eating. Binge eating is common, with lifetime prevalence estimates in United States (US) adults as high as 22.5% (American Psychiatric Association, 2000; Bushnell, Wells, Hornblow, Oakley-Browne, & Joyce, 1990). Approximately 2–5% of people in the US have a six-month or longer history of binge eating at least twice a week, thereby meeting criteria for binge eating disorder (BED; American Psychiatric Association, 2000; Hudson, Hiripi, Pope, & Kessler, 2007; Johnson, Spitzer, & Williams, 2001). Furthermore, BED tends to increase with age, with rates as high as 8% among women 46–55 years old (Johnson et al., 2001).
Regardless of whether it is frequent enough for a BED diagnosis, binge eating is associated with significant physical and psychological problems (Crow, Agras, Halmi, Mitchell, & Kraemer, 2002; Ricca et al., 2009; Striegel-Moore, Wilson, Wilfley, Elder, & Brownell, 1998; Striegel-Moore et al., 2000). For example, binge eating has been associated with higher body mass index (BMI) and thus greater obesity severity and increased risk for obesity-related chronic illnesses (Manson, Skerrett, Greenland, & VanItallie, 2004; Striegel-Moore et al., 2000; Wilfley, Wilson, & Agras, 2003). Additionally, BED is associated with greater prevalence of health problems, such as insomnia, gastrointestinal problems, shortness of breath, chest pain, and diabetes, as well as poorer physical, social, and role functioning (Johnson et al., 2001).
The psychological sequelae of binge eating include lower self-esteem and greater negative affect (Ricca et al., 2009; Striegel-Moore et al., 1998, 2000; Wilfley et al., 2003) as well as increased prevalence of anxiety disorders, alcohol use disorders, and major depressive disorder (Johnson et al., 2001). Similarly, individuals who binge eat report substantially more psychosocial stressors (e.g., lack of social support, relationship and sexual difficulties, financial problems) and greater overall psychiatric distress than those who do not binge eat (Johnson et al., 2001; Ricca et al., 2009; Striegel-Moore et al., 2000). Given the prevalence and psychological and physical toll associated with binge eating, it is important to identify factors that contribute to its development and maintenance. Indeed, such efforts can ultimately guide the prevention and treatment of binge eating.
1.2. Binge eating to reduce emotional distress
Early reinforcement theories (Conger, 1956) and Chapman's experiential avoidance model of deliberate self-harm (Chapman, Gratz, & Brown, 2006) posit that harmful behaviors are maintained through negative reinforcement in the form of avoidance or reduction of aversive emotions. Wedig and Nock (2010) have further described two dimensions along which the functions of self-injurious or maladaptive behaviors can vary, namely negative versus positive reinforcement and intrapersonal versus interpersonal focus. They found that binge eating served as intrapersonal negative reinforcement (i.e., behavior is maintained via removal of negative affect) significantly more than it served any of the other functions: intrapersonal positive reinforcement (i.e., behavior is maintained because it elicits a positive internal state), social negative reinforcement (i.e., behavior is engaged in to avoid social interactions or tasks), and social positive reinforcement (i.e., behavior is engaged in to gain attention from or communicate with others). This research suggests that, in addition to other important influences such as dietary restraint (see Racine, Burt, Iacono, McGue, & Klump, 2010; Stice, 2001), a primary reason people binge eat may be to reduce negative affective states (Wedig & Nock, 2010).
Consistent with this theory, studies accumulated over the past two decades have shown that individuals who binge eat often do so to reduce negative emotions (Arnow, Kenardy, & Agras, 1995; Hohlstein, Smith, & Atlas, 1998; Kenardy, Arnow, & Agras, 1996; Polivy & Herman, 1993; Ricca et al., 2009; Wedig & Nock, 2010). For example, individuals who expect eating to reduce their feelings of distress are more likely to report disinhibited eating patterns than those who do not associate eating with reductions in negative affect (Hohlstein et al., 1998). Similarly, the presence and severity of binge eating is positively correlated with eating in response to all three of the emotional categories assessed by the Emotional Eating Scale: anger/frustration, anxiety, and depression (Arnow et al., 1995; Ricca et al., 2009). Further, there is evidence that binge eating results in temporary relief from negative mood (Deaver, Miltenberger, Smyth, Meidinger, & Crosby, 2003), and Kenardy et al. (1996) found that binge eaters reported a “trade-off” of one aversive emotional state for a less aversive emotional state as a result of their binges. Interestingly, binge-eaters in this study reported a range of negative emotions as more distressing relative to non-binge eaters, suggesting that those who are particularly sensitive to negative affect may be even more likely to engage in binge eating in order to reduce their distress (Kenardy et al., 1996).
1.3. Anxiety sensitivity and binge eating
Anxiety sensitivity (AS) is an individual difference variable characterized by a fear of anxiety and related sensations, which is often fueled by catastrophic interpretations (Reiss & McNally, 1985). AS is distinct from trait anxiety (Taylor, Koch, & Crockett, 1991), and it plays a role in the development and maintenance of anxiety problems, particularly panic attacks and panic disorder (Brown, Smits, Powers, & Telch, 2003; Ehlers, 1995; Schmidt, Lerew, & Jackson, 1997; Smits, Powers, Cho, & Telch, 2004; Taylor, 1999), exacerbates preexisting anxiety (Reiss, 1991), and has also been associated with depression (Otto, Pollack, Fava, Uccello, & Rosenbaum, 1995; Schmidt et al., 1997) and substance use problems (Comeau, Stewart, & Loba, 2001; Stewart & Zeitlin, 1995). Because individuals with high AS experience increased levels of negative affect and are especially sensitive to this negative affect (Ehlers, 1995; Otto et al., 1995; Reiss, 1991; Schmidt et al., 1997; Taylor, 1999; Taylor, Koch, Woody, & McLean, 1996), they may be more likely to make behavioral attempts to reduce their negative affect relative to persons with normative or low AS levels.
Support for this hypothesis comes from the substance use literature. Specifically, a number of studies have demonstrated that people with high AS often turn to substance use in an effort to reduce their negative emotional states (Brown, Kahler, Zvolensky, Lejuez, & Ramsey, 2001; DeHaas, Calamari, Blair, & Martin, 2001; Lejuez, Paulson, Daughters, Bornovalova, & Zvolensky, 2006; Novak, Burgess, Clark, Zvolensky, & Brown, 2003; Stewart & Zeitlin, 1995; Zvolensky et al., 2004). For example, cigarette smokers with high AS are more likely than those with low AS to smoke as a means of decreasing negative affect, and they tend to relapse sooner after attempting to quit (Brown et al., 2001; Zvolensky et al., 2004). Additionally, individuals with high AS are more likely to use alcohol to cope with negative emotions than those less sensitive to anxiety (DeHaas et al., 2001; Novak et al., 2003; Stewart & Zeitlin, 1995), and high coping motives for drinking predict future problems with alcohol (Cooper, Russell, & George, 1988; Cooper, Russell, Skinner, & Windel, 1992). This relationship between AS and coping motives for substance use has also been observed for marijuana (Bonn-Miller, Zvolensky, & Bernstein, 2007; Comeau et al., 2001; Mitchell, Zvolensky, Marshall, Bonn-Miller, & Vujanovic, 2007; Smits, Bonn-Miller, Tart, Irons, & Zvolensky, 2011), suggesting that the relation is not specific to a particular substance and therefore indicates that a link may also exist between AS and coping motives for eating (i.e., the expectancy that eating can reduce negative affect).
There is some evidence suggesting that AS is implicated in binge eating. Specifically, a recent study showed that AS predicted bulimic symptoms (i.e., binge eating combined with inappropriate compensatory behaviors), even after accounting for the influence of other relevant variables, such as trait anxiety, depression, and impulsivity (Anestis, Holm-Denoma, Gordon, Schmidt, & Joiner, 2008). However, Anestis and colleagues only examined the relationship between AS and the bulimia subscale from the Eating Disorder Inventory (Garner, Olmstead, & Polivy, 1983). Because this subscale measures both binge eating and compensatory behaviors, these study findings do not speak to the AS–binge eating relation per se. The present study will extend this research by examining the relationship between AS and binge eating, with coping motives for eating as a potential mediator of this relationship.
1.4. Physical activity as a moderator of the AS-binge eating relation
Recent work indicates that that the strength of the AS–binge eating relation may vary as a function of physical activity (PA). Specifically, data from animal and human studies converge to suggest that individuals who are physically active show reduced physiological (i.e., blood pressure, heart rate) and psychological (e.g., anxiety, depressed mood) reactivity to stress relative to individuals who are inactive (Forcier et al., 2006; Sothmann, 2006). These data are consistent with the cross-stressor adaptation hypothesis, which posits that cardiovascular and neuroendocrine adaptations that have resulted from regular PA (a stress-or) also manifest themselves in an individual's responses to non-PA stressors, including psychosocial stressors (Sothmann, 2006). Accordingly, PA may serve as a buffer against stress, thereby protecting people from developing associated psychological problems (e.g., depression, anxiety, maladaptive behavioral action tendencies; Salmon, 2001). Indeed, PA has been linked to greater psychological wellbeing (Stathopoulou, Powers, Berry, Smits, & Otto, 2006) and reduced coping motives for substance use (Medina et al., 2011; Smits, Bonn-Miller, Tart, Irons, & Zvolensky, 2011).
Protection from stress is particularly relevant for individuals who are sensitive to stress or at risk to respond to stress with negative affect and associated maladaptive action tendencies. Accordingly, it is possible that the risk conferred by AS may be modulated by PA, such that individuals with elevated AS who are physically active experience fewer psychological problems relative to individuals with elevated AS who are physically inactive. Support for this hypothesis comes from a recent study (Smits, Tart, Rosenfield, & Zvolensky, 2011). In this study, higher levels of self-reported PA were related to significantly lower carbon dioxide (CO2) challenge reactivity (a predictor of the development of panic attacks) for those with elevated levels of AS, but not for those with low AS. Importantly, among participants with high levels of PA, there was no difference in CO2 challenge reactivity between those with high levels of AS and those with normal levels of AS. These results imply that regular PA may reduce the risk of developing problems associated with AS such as coping motives for both binge eating and other maladaptive behaviors.
Because of its negative affect-reducing effects (Salmon, 2001; Smits, Powers, Berry, & Otto, 2007; Smits & Zvolensky, 2006), regular PA may also weaken the relation between coping motives for eating and binge eating. Indeed, while physically active individuals may in fact maintain the belief that eating can be useful for coping with negative affect or stress, the reductions in negative affect brought on by PA may obviate actually turning to eating to cope (Rostad & Long, 1996).
1.5. Study aims and hypotheses
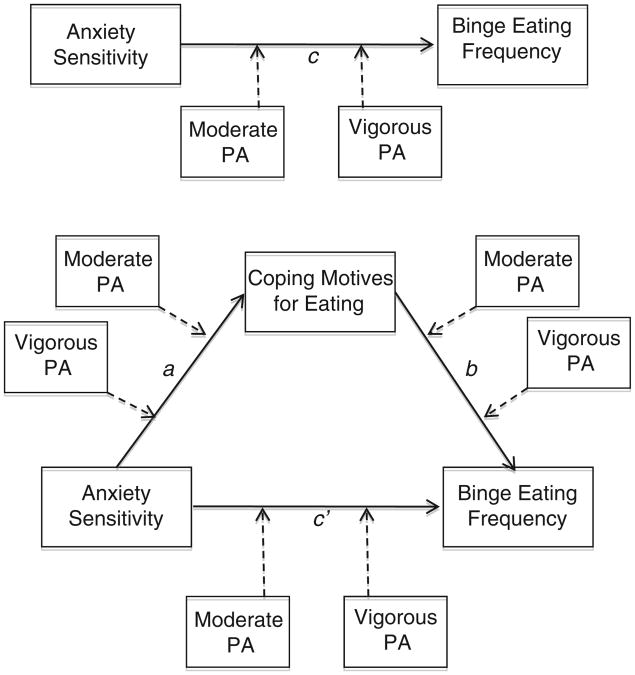
The present study sought to build on extant work by examining whether the protective effects of PA for individuals with AS extend from negative affect to maladaptive behavioral action strategies, in this case binge eating. On the basis of the available evidence, we hypothesized that (1) PA would moderate the association between AS and binge eating frequency, such that the association would be weaker among participants who were more physically active relative to individuals who are less physically active, and (2) that coping motives for eating would mediate the association between AS and binge eating frequency for those low in PA but not for those high in PA (i.e., PA would moderate the mediated pathway). For the moderated mediation analyses, we tested whether PA moderated both the association between AS and coping motives (i.e., the a path; see Fig. 1) and the association between coping motives and binge eating (i.e., the b path; see Fig. 1). Finally, because there is a dearth of work documenting dose–response relations between PA and the influence of AS on emotional responding to stress and corresponding coping behaviors, we examined both moderate-intensity (MPA)and vigorous-intensity physical activity (VPA) as moderators (simultaneously) of the association between AS and binge eating.
Fig. 1.
Study hypothesis.
2. Material and methods
2.1. Participants
Study participants were alumni from a private university in the US who participated in an internet-based study examining the relationship between mood and health behaviors. An email invitation, which included a link to an online survey, was sent to 497 potential participants. Of the 325 (65%) who responded, 180 completed the measures of interest. Following the recommendations of Tabachnick and Fidell (2001), we examined the residuals of the regression analyses for multivariate outliers and for the assumptions of regression and removed 13 outliers with standardized residuals greater than three. The final sample size was 167. Ages ranged from 31 to 81 years (M=51.02; SD=13.23), and 44.9% of the sample was female. Mean body mass index (BMI) ranged from 18.77 to 49.59 (M=26.36, SD=4.90). The racial breakdown of the sample was 90.2% White, 2.4% African American, 3.7% Asian, 1.8% American Indian or Alaska Native, and 1.8% listed their race as Other or Mixed Racial Heritage. Hispanic/Latino ethnicity was reported by 4.8% of participants.
2.2. Design and procedures
Cross-sectional data were obtained via an internet-based survey administered using SurveyMonkey, an online survey design program (http://www.surveymonkey.com). The first page of the survey provided a description of the study's purpose, its voluntary nature, data confidentiality, and contact information for the principal investigators and the Institutional Review Board. Participants clicked on a box indicating their consent and then proceeded to the assessments, which took approximately 15 min to complete.
2.3. Measures
2.3.1. Binge eating
Binge eating frequency was assessed using the Eating Disorder Diagnostic Scale (EDDS; Stice, Telch, & Rizvi, 2000). The EDDS consists of 22 items assessing DSM-IV diagnostic criteria for anorexia nervosa, bulimia nervosa, and binge eating disorder. The EDDS has demonstrated sound psychometric properties (Stice, Fisher, & Martinez, 2004; Stice et al., 2000). For the current study, item 8 (“How many times per week on average over the past 3 months have you eaten an unusually large amount of food and experienced a loss of control?”) was used as an index of DSM-IV defined binge eating frequency. This approach is similar to that employed in previous studies of binge eating (e.g., Stice, Presnell, Shaw, & Rhode, 2005; Stice, Presnell, & Spangler, 2002).
2.3.2. Coping motives for eating
The extent to which participants endorse coping motives for eating, or expect that eating can reduce negative affect, was assessed with the Eating Expectancies Inventory (EEI; Hohlstein et al., 1998). The EEI consists of 34 self-report questions assessing participants' expectancies about the function of eating. This measure utilizes a 7-point Likert scale format, and contains five subscales: eating as managing negative affect (EEI1), as pleasure/reward (EEI2), as leading to feelings of loss of control (EEI3), as enhancing cognitive competence (EEI4), and as alleviating boredom (EEI5).Higher scores indicate greater endorsement of expectancies about the function of eating. The EEI1 subscale, which consists of 16 items (e.g., “When I am feeling depressed or upset, eating can help me take my mind off my problems,” “When I am feeling anxious or tense, eating helps me relax”), was used to index emotional coping motives for eating. The EEI1 subscale has high internal consistency (α=.94 in the present sample), good construct validity (e.g., r=.48 for bulimic symptoms, r=.64 for disinhibited eating), convergent and discriminant validity (e.g., high EEI1 scores predict bulimia and not anorexia; Hohlstein et al., 1998).
2.3.3. Anxiety sensitivity
The Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986) was used to assess participants' AS. The ASI is a 16-item self-report questionnaire in which respondents indicate on a 5-point Likert-type scale (0=very little to 4=very much) the degree to which anxiety symptoms are distressing (e.g., “It scares me when my heart beats rapidly”) and the concern about negative consequences of anxiety symptoms (e.g., “When I cannot keep my mind on a task, I worry that I might be going crazy.”). The ASI has good internal consistency (ranging from .80 to .90; Peterson & Reiss, 1992; Taylor, Koch, & McNally, 1992; Telch, Shermis, & Lucas, 1989), construct validity (McNally & Lorenz, 1987; Taylor et al., 1991), and retest reliability (r ranging from .75 for 2-week periods to .71 for periods of over 3 years; Peterson & Reiss, 1992; Maller & Reiss, 1992). The alpha coefficient in the current sample was .88.
2.3.4. Physical activity
Frequency of participants' MPA and VPA was determined by responses to the first four items of the International Physical Activity Questionnaire-Short Form (IPAQ-SF; Craig et al., 2003). The IPAQ-SF is a 6-item questionnaire that assesses the amount of time spent in sedentary activity, walking, and in moderate- and vigorous-intensity activity. Participants provide the number of minutes and hours spent per day in each type of activity over the previous week. The IPAQ-SF defines vigorous-intensity exercise as “activities that take hard physical effort and make you breathe much harder than normal,” such as “heavy lifting, digging, aerobics, or fast bicycling.” Moderate-intensity activity is defined as “activities that take moderate physical effort and make you breathe somewhat harder than normal,” for example, “carrying light loads, bicycling at a regular pace, or doubles tennis.” This measure has demonstrated adequate psychometric properties, including good retest reliability (pooled p=.76), adequate concurrent validity with the IPAQ-Long Form (pooled p=.67), and adequate criterion validity of the self-report IPAQ-SF against accelerometers (pooled p=.30; Craig et al., 2003). As recommended in the IPAQ scoring manual, moderate and vigorous intensity time variables that exceeded an average of 180 min per day were truncated. Two cases exceeded this limit (i.e., 257 min per day VPA, 600 min per day MPA) and were therefore recoded as 180 min per day.
2.3.5. Negative affect
The Positive Affect Negative Affect Scale (PANAS; Watson & Clark, 1992) measures two global dimensions of mood: negative and positive. The 23-item negative affectivity scale was used to measure participants' experience of negative affective states (i.e., hostility, fear, sadness, guilt) during the “past few weeks.” The negative affectivity scale of the PANAS has demonstrated high levels of internal consistency across a range of populations, including cross-national samples (α ranges from .83 to .90; see Watson, 2000; α=.92 in the current sample). The PANAS has also demonstrated good retest reliability (r=.71; Watson, Clark, & Tellegen, 1988).
2.3.6. Body Mass Index (BMI)
BMI (weight (lbs)*703/height (inches)2) was calculated from participants' self-reported height and weight on a demographic questionnaire.
2.4. Data analytic procedure
2.4.1. Overview
The study hypotheses were evaluated using multiple regression analyses. As recommended by Aiken and West (1991), all continuous variables were standardized and centered at their means in order to reduce multicollinearity and to facilitate interpretation of the coefficients. Negative affect was included as a covariate in all analyses because of its associations with binge eating (Arnow et al., 1995; Kenardy et al., 1996; Polivy & Herman, 1993; Ricca et al., 2009; Wedig & Nock, 2010; Wegner et al., 2002), AS (Ehlers, 1995; Otto et al., 1995; Reiss, 1991; Schmidt et al., 1997; Taylor, 1999), and PA (Salmon, 2001; Stathopoulou et al., 2006). Thus, we controlled for negative affect to provide a more stringent test of the specific contribution of AS to risk for binge eating. BMI was also included as a covariate because it has been associated with binge eating (Striegel-Moore et al., 2000; Wilfley et al., 2003) and PA (Goldberg & King, 2007).
2.4.2. Hypothesis testing
In order to evaluate whether the relationship between AS and binge eating varied as a function of PA level (hypothesis 1; see c path in Fig. 1), we tested the following model:
Significant interactions were probed by testing the models with PA variables centered at zero PA and at 1.5 SD above the mean (Edwards & Lambert, 2007; Tein, Sandler, MacKinnon, & Wolchik, 2004). This procedure yielded regression coefficients for those who do not engage in MPA and VPA at all and those who engage in MPA and VPA at high levels, which aids understanding of the relations among the variables.
In order to test hypotheses that coping motives for eating mediated the association between AS and binge eating, and that this mediated pathway varied as a function of PA level (the moderated mediational model; see Fig. 1), we followed the guidelines put forth by MacKinnon, Fairchild, and Fritz (2007). Specifically, we tested the following models:
a path: Y (coping motives for eating)=(β0+β1(AS)+(β2(negative affect)+(β3(BMI)+(β4(MPA)+(β5(VPA)+(β6(AS*MPA)+(β7(AS*VPA)+ε
b and c′ paths: Y (binges per week)=(β0+β(AS)+(β2(NA)+(β3(BMI)+(β4(MPA)+(β5(VPA)+(β6(AS*MPA)+(β7(AS*VPA)+(β8(CM)+>(β9(CM*MPA)+(β10(CM*VPA)+ε
The significance of the mediated a*b pathway was tested using the distribution of products test (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; MacKinnon et al., 2007), which involves calculating the size of the joint mediated pathway by multiplying the regression coefficients of the two pieces of the mediated pathway (i.e., a*b) and then determining the 95% confidence interval (CI) for this product. CI's that do not include 0 indicate a significantly mediated pathway (MacKinnon, Lockwood, & Williams, 2004). Lastly, in order estimate the effect size of the mediated pathway, the proportion mediated (PM; Shrout & Bolger, 2002) was calculated using the formula (a*b)/c. The PM represents the proportion of the total effect of AS on binge eating (i.e., the c path) mediated by coping motives for eating.
3. Results
3.1. Preliminary analyses
Descriptive statistics and correlations among variables are presented in Table 1. The mean binge eating weekly frequency was relatively low (M=.29; SD=.63) with 13.8% reporting binge eating once weekly, 6.0% twice weekly, and 1.2% three times weekly. The mean PA levels were relatively high (MPA: M=196.11 min/week; SD=247.61; VPA: M=194.27 min/week; SD=222.78). Average levels of AS (M=14.47;SD=8.17) and negative affect (M=36.64; SD=11.04) were comparable to that observed in other community samples (Schmidt & Joiner, 2002; Watson & Clark, 1992).
Table 1.
Means, standard deviations, ranges, and correlations for study variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | Mean (SD) | Range |
|---|---|---|---|---|---|---|---|---|---|
| 1. Binges | 0.29 (0.63) | 0–3 | |||||||
| 2. ASI | 31 | 14.47 (8.17) | 1–46 | ||||||
| 3. EEI coping motives | .37*** | .46*** | 38.25 (19.61) | 16–99 | |||||
| 4. Moderate PA (min/week) | −.09 | .03 | .10 | 196.11 (247.61) | 0–1260 | ||||
| 5. Vigorous PA (min/week) | .01 | −.10 | −.07 | .40*** | 194.27 (222.78) | 0–1260 | |||
| 6. PANAS neg. affect | .11 | .49*** | .41*** | .02 | −.08 | 36.64 (11.04) | 23–110 | ||
| 7. BMI | .23** | −.06 | .33*** | −.06 | −.10 | −.05 | 26.36 (4.90) | 18.8–49.6 | |
| 8. Age | −.10 | −.15 | −.10 | .03 | .13 | −.16* | .15 | 51.02 (13.23) | 31–81 |
p≤.05.
p≤.01.
p≤.001.
3.2. Physical activity as a moderator of the association between AS and binge eating
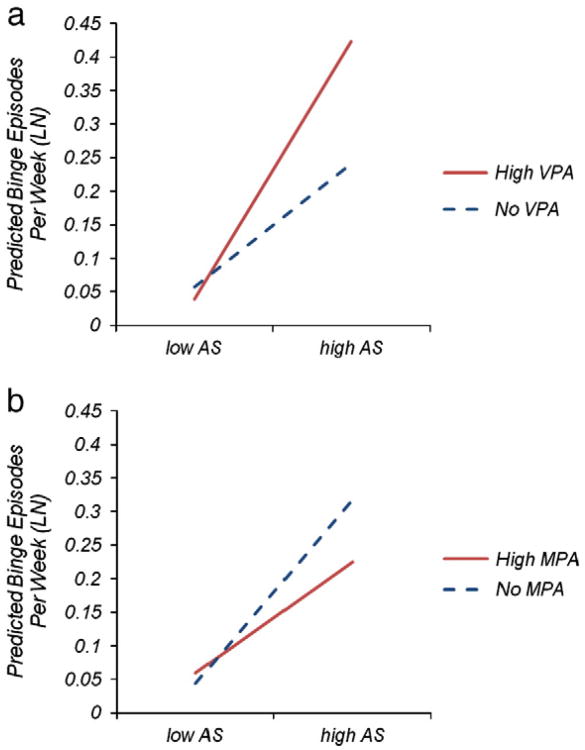
Regression analyses revealed that higher levels of AS were associated with more frequent binge eating (b=.137, p<.001), and that this association varied by MPA frequency (b=-.054, p=.036), such that AS was positively related to binge eating for those who did not engage in MPA (b=.095; p<.006), but AS was not related to binge eating for those who engaged in MPA at 1.5 SD above the mean (b=.054; p=.238; see Fig. 2a). VPA also moderated the relation between AS and binge eating, but in the opposite direction (b=.055; p=.038), such that AS-binge eating relation was stronger for those who engaged in VPA at 1.5 SD above the mean (b=.221; p<.001) than for those who did not engage in VPA (b=.185; p<.001; see Fig. 2b).1
Fig. 2.
The relation between AS and binge eating frequency for those with high levels (1.5 SD above mean; ∼567 min/week) of MPA versus those who do not engage in any MPA (a), and the relation between AS and binge eating for those with high levels (1.5 SD above mean; ∼528 min/week) of VPA versus those who do not engage in VPA (b).
3.3. Physical activity as a moderator of the meditational effect of coping motives
Contrary to prediction, neither MPA (b=−.082, p=.164) nor VPA (b=.053, p=.375) moderated the effect of AS on coping motives (i.e., a path). Also contrary to prediction, the coping motives by MPA (b=.035, p=.257) and coping motives by VPA (b=−.002, p=.956) interactions did not predict binge eating (i.e., b path). Because PA did not moderate the mediated pathway, we tested the model without the PA by AS interaction and PA terms. As is shown in Table 2, AS significantly predicted coping motives (b=.358, p<.001; a path), and coping motives significantly predicted binge eating (b=.085, p=.014; b path). The relation between AS and binge eating remained significant when accounting for coping motives (b=.105, p=.002). The distribution of products test revealed that this mediation model was significant [95% CI: .006, .060], and the proportion of the relationship between AS and binge eating that was mediated by coping motives (PM) was 22.0%.
Table 2.
Regression analysis testing the mediation model.
| Independent variables | β | t |
|---|---|---|
| c path | ||
| Anxiety sensitivity (ASI) | 14 | 4.34 |
| Negative affect (PANAS) | −.01 | −0.23 |
| Body mass index (BMI) | .09*** | 3.38 |
| Moderate PA min/week (IPAQ-SF) | −.04 | −.1.60 |
| Vigorous PA min/week (IPAQ-SF) | .05 | 1.59 |
| MPA×Anxiety sensitivity | −.05* | −.2.12 |
| VPA×Anxiety sensitivity | .06* | 2.10 |
| a path | ||
| Anxiety sensitivity (ASI) | .36*** | 5.07 |
| Negative affect (PANAS) | .27*** | 3.62 |
| Body mass index (BMI) | .35*** | 5.98 |
| b and c′ paths | ||
| Anxiety sensitivity (ASI) | .11** | 3.14 |
| Negative affect (PANAS) | −.03 | −0.91 |
| Body mass index (BMI) | .06* | 2.04 |
| MPA min/week (IPAQ-SF) | −.05 | −1.93 |
| VPA min/week (IPAQ-SF) | .05 | 1.67 |
| MPA×Anxiety sensitivity | −.05 | −1.87 |
| VPA× Anxiety sensitivity | −.05* | 1.95 |
| Coping motives (EEI-subscale 1) | .08** | 2.47 |
p≤.05.
p≤.01.
p≤.001.
4. Discussion
4.1. Overview of results
The present study sought to examine the hypothesis that PA would moderate the association between AS and binge eating frequency as well as the mediational effect of coping motives on the relation between AS and binge eating frequency. Our results were partially consistent with hypotheses. Specifically, AS was significantly associated with binge eating and this relationship was partially mediated by coping motives for eating. Further, there was evidence suggesting that PA may buffer the effect that AS has on binge eating. That is, the relation between AS and binge eating was significant among individuals who reported low levels of MPA, but not significant among individuals who reported high levels of MPA. Interestingly, however, VPA also moderated the AS-binge eating relation, but in the opposite direction, such that the relation between AS and binge eating was significant among persons reporting high levels of VPA but not among persons reporting low levels of VPA. Finally, neither VPA nor MPA influenced the meditational effects of coping motives for eating. This latter finding suggests that PA may influence the effects of AS on binge eating, but not because of reduced coping motives for eating.
4.2. Theoretical implications
Our findings add to the extant literature in a number of meaningful ways. First, we demonstrated that the maladaptive behavioral correlates of fearing somatic arousal are not limited to problematic use of substances (Bonn-Miller et al., 2007; Brown et al., 2001; Comeau et al., 2001; DeHaas et al., 2001; Lejuez et al., 2006; Mitchell et al., 2007; Novak et al., 2003; Stewart & Zeitlin, 1995; Zvolensky et al., 2004) and avoidance of phobic stimuli among those with anxiety disorders (Hayward & Wilson, 2007; Schmidt & Koselka, 2000). Thereby, these findings support previous research suggesting that AS may be implicated in the development or maintenance of bulimia nervosa (Anestis et al., 2008) or other conditions characterized by binge eating (e.g., BED, obesity). Second, we found evidence consistent with the account that, much like maladaptive substance use, binge eating when associated with AS may function as an emotion-regulation strategy (Arnow et al., 1995; Hohlstein et al., 1998; Kenardy et al., 1996; Polivy & Herman, 1993; Ricca et al., 2009; Wedig & Nock, 2010). Indeed, in our sample, AS was significantly related to coping motives for eating, which in turn was significantly associated with binge eating. Here, it is important to point out that the association between AS and coping motives for eating remained significant after controlling for the influence of negative affect, suggesting that it is not merely distress, but also the fear of distress and bodily sensations that may fuel beliefs about using eating as coping strategy. Together, these findings indicate that AS may be an important new target for intervention in conditions where emotional eating is prominent.
We hypothesized that such intervention work would be particularly important for individuals who are physically inactive. Our results show that the hypothesized protective effects of PA may only be apparent for MPA, and that VPA in fact may potentiate the negative influence of AS on binge eating. One possible explanation is that VPA can take on a different function – one that likely reinforces maladaptive coping behavior – in the context of binge eating, relative to other problem emotion-regulation strategies (e.g., cigarette smoking, cannabis use). For example, VPA may serve to counteract the effects of binge eating on weight gain, a pattern commonly observed among persons with bulimia nervosa (Meyer, Taranis, & Touyz, 2008). The hypothesis that the role of PA in binge eating may vary by intensity and eating disorder diagnosis (e.g., bulimia nervosa vs. BED or no diagnosis) as well as their interaction awaits testing in prospective experimental work.
What is the mechanism underlying the influence of MPA on the AS-binge eating link? We did not find evidence consistent with our hypothesis that PA would exert its protective effects for individuals with elevated AS through reduced psychological stress reactivity and corresponding decrease in negative affect, which in turn would result in reduced coping motives for eating and binge eating frequency. Research that involves the manipulation of PA and measurement of subsequent changes in constructs of interest (e.g., stress reactivity, negative affect, coping motives for eating, and binge eating) would provide a better test of this hypothesis with more meaningful findings. One possible alternative or complementary mediator that should be considered in the context of this research is perceived health. Indeed, individuals with elevated AS tend to have low perceived general health (McLeish, Zvolensky, Smits, Bonn-Miller, & Gregor, 2007), as do those who binge eat (Venditti, Wing, Jakicic, Butler, & Marcus, 2006). It is possible that the increases in perceived health conferred by PA (Kaleta, Makowiec-D(x00105)browska, Dziankowska-Zaborszczyk, & Jegier, 2006) protect those with high AS by decreasing the likelihood of engaging in behaviors inconsistent with their healthy conceptions of themselves, such as binge eating.
4.3. Clinical implications
If replicated and extended, the results of this study have implications for the treatment of binge eating. Specifically, it may be important to assess and treat AS and maladaptive beliefs regarding the usefulness of eating for managing distress in treatment for binge eating. Dialectical Behavior Therapy for Binge Eating (Safer, Telch, & Chen, 2009) may be particularly efficacious for individuals with elevated AS who binge eat. Indeed, this intervention targets distress intolerance (a construct related to AS; Simons & Gaher, 2005) by teaching adaptive skills to enhance emotion regulation capabilities and increase tolerance of negative affect. In addition, moderate-intensity PA programs (either alone or integrated with cognitive behavioral treatment) may be effective in reducing binge eating among individuals with high AS as exercise has been shown to reduce AS levels (Broman-Fulks, Berman, Rabian, & Webster, 2004; Broman-Fulks & Storey, 2008; Smits, Berry, Tart, & Powers, 2008; Smits et al., 2008), and, as the present research suggests, may buffer the negative consequences of AS. In addition, PA would likely lead to improvement in other domains of life functioning, given its established physical health benefits.
4.4. Limitations
The present study has several limitations, some of which provide suggestions for future research. First, over 90% were White and 70.5% held advanced degrees, limiting the generalizability of our findings. Second, the study's cross-sectional design precludes any conclusions regarding causality. It is possible that engaging in binge eating precedes and contributes to increases in AS and coping motives for eating. However, among those with comorbid anxiety and eating disorders, anxiety symptoms typically predate the onset of the eating disorder (Brewerton et al., 1995; Sihvola et al., 2009), suggesting that AS may operate earlier in the causal chain and serves as a risk factor for the development of binge eating as it does for anxiety-related disorders (Ehlers, 1995; Schmidt et al., 1997; Taylor, 1999). Third, the self-report assessment only captured PA over the previous week. Although this enhances accurate memory given the one-week time frame, it also leaves the possibility that this short period may not be representative of participants' usual activity level. Thus, future research may benefit by collecting activity data over a longer period of time.
Fourth, our sample was quite active on average, with MPA and VPA means of about 195 min/week. Given our finding that the AS-binge eating relation was no longer significant at 1.5 SDs above the mean for MPA (567 min/week), it may be that only a substantial amount of MPA is protective. Given the correlational nature of this study, however, we cannot draw strong conclusions about the amount of MPA needed to elicit a buffering effect. In order to examine the influence of (various doses of) PA on these relations, it is important to manipulate this variable and examine corresponding changes in AS, coping motives for eating, and binge eating as well as their interrelations.
We cannot rule out many possible third-variable explanations for the associations among the study variables. Future research should examine the influence of other risk factors, such as physiological differences (e.g., cortisol levels) and genetic vulnerability, on the observed associations. Finally, future research should include clinician ratings of binge eating symptoms to reduce shared method variance, and objective physiological measures of fitness (e.g., stress tests that yield VO2 max or MET scores) would be useful in determining if the relations among AS, coping motives, and binge eating vary by fitness level.
4.5. Conclusions
Despite these limitations, this study adds uniquely to the literature on cognitive risk or maintenance factors for binge eating and on AS and its association with maladaptive coping behaviors in showing that those with AS are more likely to engage in binge eating as an emotion regulation strategy. Additionally, we found that the risk conferred by AS is significantly reduced among those who engage in MPA, but not VPA. These findings highlight the potential benefit of incorporating moderate-intensity physical activity interventions, as well as addressing AS and maladaptive beliefs about the functions of food, into treatments for binge eating.
Acknowledgments
Role of funding source: This research is in part supported by National Institutes of Health (NIH) Grant R01DA027533 awarded to Dr. Smits.
Footnotes
We examined the possibility that the relations involving VPA would depend on the level of MPA and that the relations involving MPA would depend on the level of VPA. We accomplished this by adding a MPA by VPA interaction term and an AS by MPA by VPA interaction term to the regression equation, which already included the simultaneous entry of MPA and VPA terms. These interactions were not significant, and thus suggest that the observed relations involving MPA do not depend on the level of VPA and the relations involving VPA do not depend on the level of MPA.
Contributors: All authors contributed to the study design. Ms. DeBoer conducted statistical analyses and wrote the first draft of the manuscript; all authors contributed to and approved the final manuscript.
Conflict of interest: Ms. DeBoer, Ms. Tart, Dr. Presnell, Dr. Powers, and Dr. Baldwin report no financial relationships with commercial interests. Dr. Smits is currently supported by National Institutes of Health (NIH) Grants R01DA027533 and R34DA031038, and receives royalties from Oxford University Press. During the past 3 years, he has received grant support from Organon/Schering-Plough (now Merck). The content of this report is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse (NIDA) or the National Institutes of Health (NIH).
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Anestis MD, Holm-Denoma JM, Gordon KH, Schmidt NB, Joiner TE. The role of anxiety sensitivity in eating pathology. Cognitive Therapy Research. 2008;32:370–385. [Google Scholar]
- Arnow B, Kenardy J, Agras WS. The emotional eating scale: The development of a measure to assess coping with negative affect by eating. International Journal of Eating Disorders. 1995;18:79–90. doi: 10.1002/1098-108x(199507)18:1<79::aid-eat2260180109>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Bernstein A. Marijuana use motives: Concurrent relations to frequency of past 30-day use and anxiety sensitivity among young adult marijuana smokers. Addictive Behaviors. 2007;32:49–62. doi: 10.1016/j.addbeh.2006.03.018. [DOI] [PubMed] [Google Scholar]
- Brewerton TD, Lydiard RB, Herzog DB, Brotman AW, O'Neil P, Ballenger J. Comorbidity of Axis I psychiatric disorders in bulimia nervosa. Journal of Clinical Psychiatry. 1995;56:77–80. [PubMed] [Google Scholar]
- Broman-Fulks JJ, Storey KM. Evaluation of a brief exercise intervention for high anxiety sensitivity. Anxiety, Stress, and Coping. 2008;21:117–128. doi: 10.1080/10615800701762675. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Berman ME, Rabian BA, Webster MJ. Effects of aerobic exercise on anxiety sensitivity. Behavior Research and Therapy. 2004;42:125–136. doi: 10.1016/S0005-7967(03)00103-7. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addictive Behaviors. 2001;26:887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Brown M, Smits JAJ, Powers MB, Telch MJ. Differential sensitivity of the three ASI factors in predicting panic disorder patients’ subjective and behavioral response to hyperventilation challenge. Journal of Anxiety Disorders. 2003;17:583–591. doi: 10.1016/s0887-6185(02)00231-1. [DOI] [PubMed] [Google Scholar]
- Bushnell JA, Wells JE, Hornblow AR, Oakley-Browne MA, Joyce P. Prevalence of three bulimia syndromes in the general population. Psychological Medicine. 1990;20:671–680. doi: 10.1017/s0033291700017190. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm. The experiential avoidance model. Behaviour Research and Therapy. 2006;44:371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Comeau N, Stewart SH, Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors. 2001;26:803–825. doi: 10.1016/s0306-4603(01)00238-6. [DOI] [PubMed] [Google Scholar]
- Conger JJ. Alcoholism: Theory, problem, and challenge II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Cooper ML, Russell M, George WH. Coping, expectancies, and alcohol abuse: A test of social learning formulations. Journal of Abnormal Psychology. 1988;97:218–230. doi: 10.1037//0021-843x.97.2.218. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner KB, Windel M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4:123–132. [Google Scholar]
- Craig C, Marshall AL, Sjostrom M, Bauman A, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Crow SJ, Agras WS, Halmi K, Mitchell JE, Kraemer HC. Full syndromal versus subthreshold anorexia nervosa, bulimia nervosa, and binge eating disorder: A multicenter study. International Journal of Eating Disorders. 2002;32:309–318. doi: 10.1002/eat.10088. [DOI] [PubMed] [Google Scholar]
- Deaver CM, Miltenberger RG, Smyth J, Meidinger A, Crosby R. An evaluation of affect and binge eating. Behavior Modification. 2003;27(4):578–599. doi: 10.1177/0145445503255571. [DOI] [PubMed] [Google Scholar]
- DeHaas R, Calamari JE, Blair JP, Martin ED. Anxiety sensitivity and drug or alcohol use in individuals with anxiety and substance use disorders. Addictive Behaviors. 2001;26:787–801. doi: 10.1016/s0306-4603(01)00237-4. [DOI] [PubMed] [Google Scholar]
- Edwards JR, Lambert LS. Methods for integrating moderation and mediation: A general analytical framework using moderated path analysis. Psychological Methods. 2007;12:1–22. doi: 10.1037/1082-989X.12.1.1. [DOI] [PubMed] [Google Scholar]
- Ehlers A. A one-year prospective study of panic attacks: Clinical course and factors associated with maintenance. Journal of Abnormal Psychology. 1995;104:164–172. doi: 10.1037//0021-843x.104.1.164. [DOI] [PubMed] [Google Scholar]
- Forcier K, Stroud LR, Papandonatos GD, Hitsman B, Reiches M, Krishnamoorthy J, et al. Links between physical fitness and cardiovascular reactivity and recovery to psychological stressors: A meta-analysis. Health Psychology. 2006;25(6):723–739. doi: 10.1037/0278-6133.25.6.723. [DOI] [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–19. [Google Scholar]
- Goldberg J, King A. Physical activity and weight management across the lifespan. Annual Review of Public Health. 2007;28:145–170. doi: 10.1146/annurev.publhealth.28.021406.144105. [DOI] [PubMed] [Google Scholar]
- Hayward C, Wilson KA. Anxiety sensitivity: A missing piece to the agoraphobia-without-panic puzzle. Behavior Modification. 2007;31(2):162–173. doi: 10.1177/0145445506297015. [DOI] [PubMed] [Google Scholar]
- Hohlstein LA, Smith GT, Atlas JG. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment. 1998;10:49–58. [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Spitzer RL, Williams JB. Health problems, impairment and illness associated with bulimia nervosa and binge eating disorder among primary care and obstetric gynecology patients. Psychological Medicine. 2001;31:1455–1466. doi: 10.1017/s0033291701004640. [DOI] [PubMed] [Google Scholar]
- Kaleta D, Makowiec-Dąbrowska T, Dziankowska-Zaborszczyk E, Jegier A. Physical activity and self-perceived health status. International Journal of Occupational Medicine and Environmental Health. 2006;19(1):61–69. doi: 10.2478/v10001-006-0005-x. [DOI] [PubMed] [Google Scholar]
- Kenardy J, Arnow B, Agras WS. The aversiveness of specific emotional states associated with binge-eating in obese subjects. Australian and New Zealand Journal of Psychiatry. 1996;30:839–844. doi: 10.3109/00048679609065053. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Paulson A, Daughters SB, Bornovalova MA, Zvolensky MJ. The association between heroin use and anxiety sensitivity among inner-city individuals in residential drug use treatment. Behaviour Research and Therapy. 2006;44:667–677. doi: 10.1016/j.brat.2005.04.006. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Reviews in Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders. 1992;6:241–247. [Google Scholar]
- Manson JE, Skerrett PJ, Greenland P, VanItallie TB. The escalating pandemics of obesity and sedentary lifestyle: A call to action for clinicians. Archives of Internal Medicine. 2004;164:249–258. doi: 10.1001/archinte.164.3.249. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ, Smits JAJ, Bonn-Miller MO, Gregor KL. Concurrent associations between anxiety sensitivity and perceived health and health disability among young adult daily smokers. Cognitive Behaviour Therapy. 2007;36(1):1–11. doi: 10.1080/16506070600794653. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Lorenz M. Anxiety sensitivity in agoraphobics. Journal of Behavior Therapy and Experimental Psychiatry. 1987;18:3–11. doi: 10.1016/0005-7916(87)90065-6. [DOI] [PubMed] [Google Scholar]
- Medina JL, Vujanovic AA, Smits JAJ, Irons JG, Zvolensky MJ, Bonn-Miller MO. Exercise and coping-oriented alcohol use among a trauma-exposed sample. Addictive Behaviors. 2011;36(3):274–277. doi: 10.1016/j.addbeh.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer C, Taranis L, Touyz S. Excessive exercise in the eating disorders: A need for less activity from patients and more from researchers. European Eating Disorder Review. 2008;16:81–83. doi: 10.1002/erv.863. [DOI] [PubMed] [Google Scholar]
- Mitchell H, Zvolensky MJ, Marshall EC, Bonn-Miller MO, Vujanovic AA. Incremental validity of coping-oriented marijuana use motives in the prediction of affect-based psychological vulnerability. Journal of Psychopathology and Behavioral Assessment. 2007;29:277–288. [Google Scholar]
- Novak A, Burgess ES, Clark M, Zvolensky MJ, Brown RA. Anxiety sensitivity, self-reported motives for alcohol and nicotine use, and level of consumption. Journal of Anxiety Disorders. 2003;17:165–180. doi: 10.1016/s0887-6185(02)00175-5. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Fava M, Uccello R, Rosenbaum JF. Elevated anxiety sensitivity index scores in patients with major depression: Correlates and changes with antidepressant treatment. Journal of Anxiety Disorders. 1995;9:117–223. [Google Scholar]
- Peterson RA, Reiss S. Anxiety sensitivity index manual revised. Worthington, OH: International Diagnostic Systems; 1992. [Google Scholar]
- Polivy J, Herman CP. Etiology of binge eating: Psychological mechanisms. In: Fairburn CF, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. New York: Guilford Press; 1993. pp. 173–205. [Google Scholar]
- Racine SE, Burt SA, Iacono WG, McGue M, Klump KL. Dietary restraint moderates genetic risk for binge eating. Journal of Abnormal Psychology. 2010;120(1):119–128. doi: 10.1037/a0020895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S. Expectancy model of fear, anxiety, and panic. Clinical Psychology Review. 1991;11:141–153. [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. San Diego: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the predictions of fearfulness. Behavior Research and Therapy. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Ricca V, Castellini G, Lo Sauro C, Ravaldi C, Lapi F, Mannucci E, et al. Correlations between binge eating and emotional eating in a sample of overweight subjects. Appetite. 2009;53:418–421. doi: 10.1016/j.appet.2009.07.008. [DOI] [PubMed] [Google Scholar]
- Rostad FG, Long BC. Exercise as a coping strategy for stress: A review. International Journal of Sport Psychology. 1996;27(2):197–222. [Google Scholar]
- Safer DL, Telch CF, Chen EY. Dialectical behavior therapy for binge eating and bulimia. New York, NY: Guilford Press; 2009. [Google Scholar]
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress. Clinical Psychology Review. 2001;21:33–61. doi: 10.1016/s0272-7358(99)00032-x. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Koselka M. Gender differences in patients with panic disorder: Evaluating cognitive mediation of phobic avoidance. Cognitive Research and Therapy. 2000;24(5):533–550. [Google Scholar]
- Schmidt NB, Lerew DR, Jackson R. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Joiner TE. Structure of the Anxiety Sensitivity Index psycho-metrics and factor structure in a community sample. Journal of Anxiety Disorders. 2002;16:33–49. doi: 10.1016/s0887-6185(01)00087-1. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and non-experimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Sihvola E, Keski-Rahkonen A, Dick DM, Hoek HW, Raevuori A, Rose RJ, et al. Prospective associations of early onset Axis I disorders with developing eating disorders. Comprehensive Psychiatry. 2009;50(1):20–25. doi: 10.1016/j.comppsych.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- Smits JAJ, Zvolensky MJ. Emotional vulnerability as a function of physical activity among individuals with panic disorder. Depression & Anxiety. 2006;23:102–106. doi: 10.1002/da.20146. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Powers MB, Cho YC, Telch MJ. Mechanism of change in cognitive–behavioral treatment of panic disorder: Evidence for the fear of fear mediational hypothesis. Journal of Consulting & Clinical Psychology. 2004;72:646–652. doi: 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Powers MB, Berry AC, Otto MW. Translating empirically-supported strategies into accessible interventions: The potential utility of exercise for the treatment of panic disorder. Cognitive & Behavioral Practice. 2007;14:364–374. [Google Scholar]
- Smits JAJ, Berry AC, Rosenfield D, Powers MB, Behar E, Otto MW. Reducing anxiety sensitivity with exercise. Depression and Anxiety. 2008;25:689–699. doi: 10.1002/da.20411. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Berry AC, Tart CD, Powers MB. The efficacy of cognitive–behavioral interventions for reducing anxiety sensitivity: A meta-analytic review. Behaviour Research and Therapy. 2008;46:1047–1054. doi: 10.1016/j.brat.2008.06.010. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Bonn-Miller M, Tart CD, Irons JG, Zvolensky MJ. Anxiety sensitivity as a mediator of the relationship between moderate-intensity exercise and coping-oriented marijuana use motives. The American Journal on Addictions. 2011;20(2):113–119. doi: 10.1111/j.1521-0391.2010.00115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JAJ, Tart CD, Rosenfield D, Zvolensky MJ. The interplay between physical activity and anxiety sensitivity in fearful responding to CO2 challenge. Psychosomatic Medicine. 2011;73:498–503. doi: 10.1097/PSY.0b013e3182223b28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sothmann MS. The cross-stressor adaptation hypothesis and exercise training. In: Acevedo EO, Ekkekakis P, editors. Psychobiology of physical activity. Champaign, IL: Human Kinetics; 2006. pp. 149–160. [Google Scholar]
- Stathopoulou G, Powers MB, Berry AC, Smits JAJ, Otto MW. Exercise interventions for mental health: A quantitative and qualitative review. Clinical Psychology: Science and Practice. 2006;13:179–193. [Google Scholar]
- Stewart SH, Zeitlin SB. Anxiety sensitivity and alcohol use motives. Journal of Anxiety Disorders. 1995;9:229–240. [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology mediating effects of dieting and negative affect. Journal of Abnormal Psychology. 2001;110:124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E, Telch C, Rizvi S. Development and validation of the Eating Disorder Diagnostic Scale: A brief self-report measure for anorexia, bulimia, and binge eating disorder. Psychological Assessment. 2000;12:123–131. doi: 10.1037//1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychology. 2002;21(2):131–138. [PubMed] [Google Scholar]
- Stice E, Fisher M, Martinez E. Eating disorder diagnostic scale: Additional evidence of reliability and validity. Psychological Assessment. 2004;16:60–71. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Shaw H, Rhode P. Psychological and behavioral risk factors for obesity onset in adolescent girls: A prospective study. Journal of Consulting and Clinical Psychology. 2005;73(2):195–202. doi: 10.1037/0022-006X.73.2.195. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Wilson GT, Wilfley DE, Elder KA, Brownell KD. Binge eating in an obese community sample. International Journal of Eating Disorders. 1998;23:27–37. doi: 10.1002/(sici)1098-108x(199801)23:1<27::aid-eat4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm FA, Solomon EE, Fairburn CG, Pike KM, Wilfley DE. Subthreshold binge eating disorder. International Journal of Eating Disorders. 2000;27:270–278. doi: 10.1002/(sici)1098-108x(200004)27:3<270::aid-eat3>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 4th. Needham Heights, MA: Allyn&Bacon; 2001. [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ: Lawrence Erlbaum, Inc; 1999. [Google Scholar]
- Taylor S, Koch WJ, Crockett DJ. Anxiety sensitivity, trait anxiety, and the anxiety disorders. Journal of Anxiety Disorders. 1991;5:293–311. [Google Scholar]
- Taylor S, Koch WJ, McNally RJ. How does anxiety sensitivity vary across the anxiety disorders? Journal of Anxiety Disorders. 1992;6:249–259. [Google Scholar]
- Taylor S, Koch WJ, Woody S, McLean P. Anxiety sensitivity and depression: How are they related? Journal of Abnormal Psychology. 1996;105:474–479. doi: 10.1037//0021-843x.105.3.474. [DOI] [PubMed] [Google Scholar]
- Tein JY, Sandler IN, MacKinnon DP, Wolchik SA. How did it work? Who did it work for? Mediation in the context of a moderated prevention effect for children of divorce. Journal of Consulting and Clinical Psychology. 2004;72:617–624. doi: 10.1037/0022-006X.72.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch MJ, Shermis MD, Lucas JA. Anxiety sensitivity: Unitary personality trait or domain-specific appraisals? Journal of Anxiety Disorders. 1989;3:25–32. [Google Scholar]
- Venditti EM, Wing RR, Jakicic JM, Butler BA, Marcus MD. Weight cycling, psychological health, and binge eating in obese women. Journal of Consulting and Clinical Psychology. 2006;64(2):400–405. doi: 10.1037//0022-006x.64.2.400. [DOI] [PubMed] [Google Scholar]
- Watson D. Mood and temperament. New York: Guilford Press; 2000. [Google Scholar]
- Watson D, Clark L. Affects separable and inseparable: On the hierarchical arrangement of the negative affects. Journal of Personality and Social Psychology. 1992;62:489–505. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wedig MM, Nock MK. The functional assessment of maladaptive behaviors: A preliminary evaluation of binge eating and purging among women. Psychiatry Research. 2010;178:518–524. doi: 10.1016/j.psychres.2009.05.010. [DOI] [PubMed] [Google Scholar]
- Wegner KE, Smyth JM, Crosby RD, Wittrock D, Wonderlich SA, Mitchell JE. An evaluation of the relationship between mood and binge eating in the natural environment using ecological monetary assessment. International Journal of Eating Disorders. 2002;32:352–361. doi: 10.1002/eat.10086. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. International Journal of Eating Disorders. 2003;34:S96–S106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner E, Bonn-Miller MO, McLeish AC, Gregor K. Evaluating the role of anxiety sensitivity in smoking outcome expectancies among regular smokers. Cognitive Therapy and Research. 2004;28:473–486. [Google Scholar]